Abstract
The outlook for children with newly diagnosed Wilms tumors (WT) has improved dramatically with the advent of multimodal therapy, which includes surgery, chemotherapy, and for some, radiation therapy, with survival rates currently approaching 90 % (Lemerle et al. 1983; D’Angio et al. 1981, 1976). Although the overall relapse rate for children with WT has decreased to less than 15 %, the overall long-term survival for patients with recurrent disease remains at approximately 50 % (Grundy et al. 1989; Pinkerton et al. 1991; Pein et al. 1998; Kremens et al. 2002; Tannous et al. 2000). Due to the small numbers of relapsed patients, advancements in the treatment of these patients have remained a challenge. Investigators from different cooperative groups have evaluated the role of different therapeutic strategies in an attempt to improve the outcomes of patients with recurrent WT. Therapy for these patients depends on characteristics of their primary disease, extent of previous therapy, and time from initial diagnosis to relapse.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Overall Survival
- Autologous Stem Cell Rescue
- Anaplastic Histology
- United Kingdom Child
- Vascular Endothelial Growth Factor Tyrosine
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
7.1 Introduction
The outlook for children with newly diagnosed Wilms tumors (WT) has improved dramatically with the advent of multimodal therapy, which includes surgery, chemotherapy, and for some, radiation therapy, with survival rates currently approaching 90 % (Lemerle et al. 1983; D’Angio et al. 1981, 1976). Although the overall relapse rate for children with WT has decreased to less than 15 %, the overall long-term survival for patients with recurrent disease remains at approximately 50 % (Grundy et al. 1989; Pinkerton et al. 1991; Pein et al. 1998; Kremens et al. 2002; Tannous et al. 2000). Due to the small numbers of relapsed patients, advancements in the treatment of these patients have remained a challenge. Investigators from different cooperative groups have evaluated the role of different therapeutic strategies in an attempt to improve the outcomes of patients with recurrent WT. Therapy for these patients depends on characteristics of their primary disease, extent of previous therapy, and time from initial diagnosis to relapse.

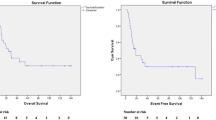
Fig. 7.1

Fig. 7.2

Fig. 7.3
7.2 Risk Stratification
A number of potential prognostic features influencing outcome post-recurrence have been analyzed, but it is difficult to separate whether these factors are independent of each other. Moreover, the prognostic factors appear to be changing over time as therapy for primary and recurrent WT evolves.
Grundy and coworkers provided a comprehensive analysis of prognostic indicators after relapse on National Wilms Tumor Studies (NWTS)-2 and NWTS-3 (Grundy et al. 1989). The time to recurrence was strongly predictive of survival, with those patients who relapsed early (0–5 months from nephrectomy) having worse outcome than those who relapsed later than 6 months. Other adverse factors were anaplastic histology, advanced tumor stage, and relapse outside the lung. Interestingly, the more recent experience from NWTS-5 showed that time to recurrence and site of recurrence were no longer prognostically significant (Malogolowkin et al. 2008; Green et al. 2007). Gender was predictive of outcome, with males faring worse than females. In addition, the group of patients treated initially with two drugs fared better than patients treated initially with three drugs, indicating that initial treatment remains a powerful prognostic factor.
The International Society of Pediatric Oncology (SIOP) identified adverse factors for relapsed WT including initial stage 4 disease, unfavorable histology, time to recurrence 6 months or less after diagnosis, and recurrence in multiple organs or a previously irradiated field (Pein et al. 1999). The German group analyzed a cohort of 170 relapsed patients and in accordance with the previous studies initial stage III or IV, high-risk histology (according to the SIOP classification (Vujanic et al. 2002)), early event, and combined site of relapse emerged as relevant prognostic indicators (Reinhard et al. 2008).
The explanation for the different prognosis between pulmonary and abdominal relapses may be that many of the abdominal recurrences occur in irradiated fields, whereas most lung recurrences developed in nonirradiated sites. Furthermore, it is sometimes difficult to extrapolate the precise recurrence site in the published reports, with “lung relapses” category including not only pulmonary parenchymal relapses but also those involving the mediastinum. Abdominal recurrence generally involves the original tumor bed (kidney area), but can correspond to retroperitoneal lymph nodes, liver, peritoneum, or contralateral kidney disease. Most “recurrences” in the contralateral kidney probably represent second primary tumors rather than true relapses. For these reasons, the site of relapse should deserve more analysis before being definitively considered for patient risk grouping.
However, it is likely that factors originally identified as predictors of survival, like combined site of relapse or recurrence-free interval, can lose their significance when more aggressive and effective regimens, like the ones adopted in recent years, are applied at relapse. Furthermore, the changes in initial disease therapy, now evolving towards less intense treatment, may influence outcome at recurrence. The more conservative upfront use of radiation in the recent era may have allowed for increased use at relapse, contributing to the improved patient outcome. Worthy of note is the fact that some stage I or II tumors also received radiation therapy in past years.
In conclusion, features that seem clearly associated with a worse outcome after relapse are anaplastic or SIOP high-risk histology and initial chemotherapy including doxorubicin. On the other hand, it is less clear whether time to recurrence remains prognostically significant with contemporary therapy.
Based on current data, three risk categories for recurrent Wilms tumor can be schematically identified:
-
1.
Standard risk: defined as patients with favorable histology WT with relapse after therapy with only vincristine and/or actinomycin D. These patients are expected to have event-free survival (EFS) estimates in the 70–80 % range, as the results reported for the NWTS-5 or United Kingdom Children’s Cancer and Leukemia Group (UKCCLG) recurrent protocols (Green et al. 2007; Hale et al. 2008). These situations account for 30 % of recurrences.
-
2.
High risk: defined as patients with favorable histology WT with relapse after therapy with three or more agents (at least including doxorubicin). These patients, accounting for 45–50 % of the children with WT who relapse, are expected to have survival rates in the 40–50 % range (Malogolowkin et al. 2008).
-
3.
Very high risk: defined as patients with recurrent anaplastic – regardless of adoption of primary chemotherapy or primary surgery- or post-chemotherapy blastemal-type WT. These patients are expected to have survival rates in the 10 % range (Reinhard et al. 2008; Dome et al. 2006). This group accounts for 10–15 % of all WT relapses.
7.3 Principles of Treatment
7.3.1 Surgery
In general, the discussion on indications, timing, and modality of surgery in children with recurrent WT has been rarely addressed, and it is more difficult to standardize a surgical approach for recurrent tumor. Most of the information we gather on surgery and radiation are extrapolated from unselected groups of patients or case discussions. Surgical removal of operable recurrent tumors is probably helpful, but has not been examined prospectively.
The lack of data on surgical excision of lung metastases in relapsed patients precludes precise interpretation of its potential role. Because the lungs are the most frequent site of first recurrence, more information on the therapeutic role of surgical resection of pulmonary metastases, and on which techniques to adopt, might be important. The only systematic evaluation – retrospectively acquired – is the one by the NWTS group, which suggested that surgical removal of all pulmonary metastases is unlikely to improve post-relapse survival compared with treatment with whole-lung radiation therapy and chemotherapy (Green et al. 1991). However, in the retrospective analysis by Dome et al., patients who underwent a complete surgical resection of recurrent tumor had a higher probability of survival than did patients who had a partial resection or no surgery (Dome et al. 2002).
The German data on surgical aspects for liver metastases or recurrences suggested that complete surgical resection of liver recurrences improves survival. Fuchs et al. reported that in children with a recurrence in the liver, those with a complete resection survived, whereas the patients with an incomplete resection all died (Fuchs et al. 2008). Patients who achieved a complete remission following chemotherapy and/or hepatic resection did not receive radiation therapy to the liver. Overall, it is tempting to speculate that surgery plays an important role in treating recurrent disease, but we cannot exclude the possibility that patients who underwent a complete surgical resection had less aggressive disease.
7.3.2 Radiation Therapy
The radiosensitivity of WT has been well documented since 1950, when Gross and Neuhauser (Gross and Neuhauser 1950) demonstrated the benefits of routine postoperative radiation to the renal fossa in patients with WT. Since then the cooperative groups (NWTS, SIOP, and UKCCG) have defined the interrelationship between adjuvant radiation therapy and chemotherapy, progressively limiting the indications for and intensity of radiation without negatively impacting survival rates. Differently then for newly diagnosed patients, the indication and doses of radiation for children with relapsed WT have not been investigated in a uniform fashion. The administration of radiation to a previously unirradiated field is less controversial and is frequently associated with a higher probability of survival.
Uniform guidelines for radiation therapy were developed for the NWTS-5 relapse study and included higher doses when compared with those used at initial diagnoses, even if the primary therapy did not include radiotherapy (Malogolowkin et al. 2008; Green et al. 2007). Although the outcomes of patients entered onto this study improved in comparison to the historical controls, due to the non-randomized design of this study, the role of radiation therapy for the treatment of relapse remained undetermined. The indication for the use of radiotherapy and the appropriate doses to be delivered for patients with relapsed WT who previously received radiation therapy remains controversial. Treatment plans for these patients should be done in conjunction with the radiation oncologist and taking into consideration the response to chemotherapy, extent of surgical resection, and consideration for the use of high-dose chemotherapy with stem cell rescue.
7.3.3 Chemotherapy
A general principle for the treatment of relapsed WT is to use agents not used for primary therapy. Phase 2 trials demonstrated efficacy of ifosfamide (52 % objective responses) (Tournade et al. 1988), etoposide (42 % responses) (Pein et al. 1993), and carboplatin (52 % responses) (De Camargo et al. 1994) either as single agents or as combinations (Pinkerton et al. 1991; Pein et al. 1994). More recently, investigators at St. Jude Children’s Research Hospital (Memphis) documented the activity of topotecan (48 %) responses in favorable histology WT (Metzger et al. 2007).
The treatment of recurrent WT has improved dramatically during the past two decades. In a review of 54 cases involved in consecutive trials at St. Jude Children’s Hospital, Dome et al. underline that outcome has improved noticeably since around the mid-1980s, when cyclophosphamide, ifosfamide, platinum compounds, and etoposide became available (Dome et al. 2002). The introduction of these drugs led to disease-free survival (DFS) rates for children with recurrent WT ranging between 50 and 70 %. Nevertheless, the best combination, dose intensity, and duration of chemotherapy agents remain poorly explored.
7.4 Standard-Risk Recurrent Patients
Children with low-stage favorable histology WT have an excellent survival with minimal therapy; therefore, the number of patients matching the criteria for the definition of standard-risk recurrent tumors is very small accounting for approximately 30 % of all recurrences, making the study of these patients a challenge. There is a paucity of reports focusing on this patient population. Recently, Green et al. reported on the outcome of 58 patients who relapsed after immediate nephrectomy (stages I and II), initial chemotherapy with vincristine and actinomycin D, and no radiation therapy (low-risk) and were registered on stratum B of the NWTS-5 relapse protocol (Green et al. 2007). Relapsed treatment included surgical excision, when feasible; radiation therapy; and alternating courses of vincristine-doxorubicin-cyclophosphamide and etoposide-cyclophosphamide. For 31 patients, the lung was the only site of relapse. The 4-year event-free survival and overall survival were 71.1 and 81.8 %, respectively, for all patients and 67.8 and 81.0 % for those who relapsed only to their lungs. The most frequent toxicities were hematological. This survival rate appears to be improved compared to a crude survival rate of 57.9 % among 19 children with stage I or II, favorable histology WT who relapsed after treatment on the United Kingdom Children’s Cancer Study Group Wilms Tumor 1 protocol (Dome et al. 2002), or to the 47.8 % 5-year overall survival rate for children with relapsed stage I or II favorable or anaplastic histology reported by investigators from Saint Jude Children’s Research Hospital (Malogolowkin et al. 2008).
7.5 High-Risk Relapsed Wilms Tumors
More recent experiences on high-risk recurrent WT, in series ranging between 11 and 60 cases, seem to support the rationale for dose-intense strategies, though there is not yet consensus on whether or not high-dose chemotherapy with autologous stem cell rescue (ASCR) can account for the improvement in outcome. Table 7.1 summarizes the results of these studies.
7.6 Conventional-Dose Chemotherapy
Abu-Gosh et al. reported on 11 cases treated with ifosfamide, carboplatin, and etoposide (ICE) chemotherapy, obtaining a 63.6 % EFS and OS at 3 years, although almost all received additional therapies, including surgery, radiation, or other chemotherapy drugs (Kung et al. 1995). Doses for ifosfamide were 1,800 mg/m2/day × 5 days, carboplatin 400 mg/m2/day × 2 days, and etoposide 100 mg/m2/day × 5 days. The ICE regimen was demonstrated to be extremely efficacious in determining second responses (82 % objective response rate). It is significant that persistent nephrotoxicity was moderate, as remarked also by other groups (Dome et al. 2002; Malogolowkin et al. 1994).
Malogolowkin et al. reported for the NWTS-5 Relapse protocol on 60 homogeneously treated children who relapsed after initial therapy with vincristine, actinomycin D, and doxorubicin plus radiotherapy (Abu-Ghosh et al. 2002). The 4-year EFS and OS were 42.3 and 48 %, respectively, for all patients and were 48.9 and 52.8 % for those with relapse to the lungs only. These results were obtained using alternate courses of the drug pairs cyclophosphamide/etoposide and carboplatin/etoposide; this regimen was 90 weeks long, and many children had discontinuation of therapy due to prolonged hematological toxicity. In a previous experience, Malogolowkin et al. treated 27 patients with alternating carboplatin/etoposide and ifosfamide/doxorubicin. The 3-year event-free survival and overall survival for these patients were 58 % (Malogolowkin et al. 1994).
7.7 High-Dose Chemotherapy and Autologous Stem Cell Rescue (ASCR)
The role of high-dose chemotherapy and ASCR in patients with high-risk recurrent WT is not fully defined. High-dose chemotherapy with ASCR has been used worldwide and mostly outside controlled clinical trials. Since the first European Bone Marrow Transplant report (Garaventa et al. 1994), the number of WT patients registered in the EBMT registry has grown to more than 300 cases (Dallorso et al. 2008).
Overall, trials with high-dose chemotherapy and ASCR seemed to obtain a better outcome than historical controls, with 3- or 4-year overall survival (OS) rates ranging from 60 to 73 % (Pein et al. 1998; Kremens et al. 2002; Hale et al. 2008; Spreafico et al. 2008; Campbell et al. 2004). Pein et al. reported on 28 high-risk chemotherapy-responsive patients transplanted, and the 3-year OS and DFS were 60 and 50 %, respectively (Pein et al. 1998). Conditioning chemotherapy consisted of melphalan, etoposide, and carboplatin (MEC) in all the cases. Kremens et al. described 23 cases treated with high-dose chemotherapy and ASCR (18 children had the MEC conditioning course), after various reinduction regimens; the OS was 60.9 %, and the EFS 48.2 % (Kremens et al. 2002). Campbell et al. showed 4-year EFS and OS rates of 60 and 73 %, respectively, in 13 patients who underwent single or double ASCR after various conditioning regimens (Campbell et al. 2004). Spreafico et al. reported on 20 consecutive patients with high-risk features at recurrence: all patients received an intense-dose chemotherapy induction, most of them adopting ICE-based therapy and 15/20 receiving high-dose chemotherapy and ASCR as consolidation (Spreafico et al. 2008). This group electively reduced the drug dosage of the ICE and MEC associations vis-à-vis the doses used by others, in an attempt to reduce the expected toxicity without jeopardizing outcome; ICE consisted of ifosfamide 1,500 mg/m2/day × 4 days, carboplatin 600 mg/m2/day × 1 day, and etoposide 100 mg/m2/day × 4 days. Three-year DFS and OS rates were 56 and 55 %, respectively.
The UK CCLG’s strategy for patients with recurrent high-risk disease was based on reinduction dose-intense regimen and a consolidation with high-dose chemotherapy and ASCR (Hale et al. 2008). The reinduction chemotherapy alternated carboplatin and etoposide with cyclophosphamide and etoposide. After six chemotherapy courses, responding patients received high-dose single-agent melphalan with ASCR.
There are no randomized trials comparing conventional-dose to high-dose chemotherapy. However, the North American colleagues reported on a series of children who underwent one or the other strategy according to the quality of tumor response to induction chemotherapy. This Children’s Cancer Group study of 66 patients with recurrent high-risk WT used cyclophosphamide (440 mg/m2/day × 5 days) and etoposide (100 mg/m2/day × 5 days) alternating with carboplatin (500 mg/m2/day × 2 days) and etoposide (100 mg/m2/day × 3 days) and gave a response rate of 78 % (42 % complete response and 36 % partial response after two courses) (Tannous et al. 2000). Patients who achieved complete tumor remission received maintenance therapy with a further five identical course pairs, while those with partial response or stable disease received ablative chemotherapy followed by ASCR. The 3-year EFS were 59 and 40 % for the maintenance and ASCR subgroups, while the 3-year OS were 64 and 42 %, respectively. Although the maintenance chemotherapy group had better outcomes than the ASCR group, there was a selection bias such that patients who were disease-free after induction therapy received standard-dose chemotherapy, whereas patients with residual disease received ASCR.
The abovementioned reports dealt with diverse inclusion criteria for patient selection (responding or not to miscellaneous reinduction chemotherapy, different disease status at the time of transplant, different histological types of renal tumors) and various conditioning regimens (single or tandem transplant, different agents). Direct comparisons are limited by these differences. It is not clear which preparative regimen is superior, but it does seem that there is a survival advantage in patients whose recurrent disease was chemosensitive and those without disease evidence prior to transplant.
Taken together, all these studies seem to suggest a role for dose-intensive strategies to treat children with relapsing high-risk WT, though there is no consensus on whether or not high-dose chemotherapy with ASCR accounts for the improvement in post-relapse outcome compared to historical published data.
In an effort to improve evidence on the role of high-dose chemotherapy and ASCR, an international analysis has attempted a synthesis of relevant published information, following a Bayesian framework, however remaining conscious of constraints that the underlined heterogeneity imposes on conclusions drawn (Ha et al. 2013). The authors have summarized EFS and OS experience of patients with relapsed or refractory WT with the objective of comparing patients who received high-dose therapy with those that did not. A total of 19 publications concerning 1,226 patients were identified (5 reporting on patients treated with high-dose chemotherapy, 6 reporting on patients treated without high-dose chemotherapy, and 8 including both categories of patients). The EFS and OS rates were combined in a weighted manner to derive hazard ratios. Pooling all studies suggested an advantage to high-dose therapy with a hazard ratio for EFS of 0.87 and 0.94 for OS. Further, analyses of those patients classified as high-risk suggested a hazard ratio of 0.90 (95 % CI 0.62 to 1.31), and for the very-high-risk patients 0.50 (CI 0.31 to 0.82). The authors concluded that the evidence was suggestive of the value of a high-dose option, particularly in the highest risk relapse group.
7.8 Topoisomerase Inhibitors
Topotecan, a camptothecin analogue that interacts with DNA topoisomerase I, demonstrated antitumor activity in different childhood cancers including WT (Nitschke et al. 1998). The schedule of administration was probably important in determining its activity, with the protracted schedule being more effective than an intermittent high-dose regimen. Investigators at St. Jude Children’s Research Hospital studied its activity specifically on WT, both in preclinical models and in clinical phase I and II trials (Dome et al. 2005; Tubergen et al. 1996). In the WILTOP, a St. Jude-based phase II study, a response rate of 48 % was obtained in 25 evaluable heavily pretreated favorable histology WT patients (12 patients had partial remission, 6 patients had stable disease, and 7 patients had progression) (Metzger et al. 2007). Importantly, topotecan seemed to be less effective in anaplastic tumors. The encouraging results obtained in the WILTOP study differed from previous topotecan trials (Nitschke et al. 1998; Tubergen et al. 1996) and were ascribed to the protracted topotecan schedule (the action of poisons during S phase is optimized by longer exposure). Based on the St. Jude’s experience, topotecan has been variably included into salvage strategies for high-risk recurrent WT patients in the past few years, but outside controlled clinical trials.
Prolonged and short schedules, as well as single infusions of irinotecan, a potent topoisomerase I inhibitor, alone or in combination with other agents, have been investigated in the traditional phase II setting in various pediatric tumors such as neuroblastoma, Ewing sarcoma, WT, and certain malignant brain tumors (Bomgaars et al. 2007; Vassal et al. 2008; Kushner et al. 2006; Turner et al. 2002; Wagner et al. 2007; Casey et al. 2009; Pappo et al. 2007). A recent Children’s Oncology Group (COG) trial on rhabdomyosarcoma revealed no differences in response rates between two different schedules of irinotecan (prolonged versus short: daily for 5 days versus daily for 5 days, 2 days off, and then an additional 5 days, respectively), disproving the preclinical prediction of superior activity with a prolonged schedule (Mascarenhas et al. 2010).
Despite there were no response to single-agent irinotecan in previous early phase clinical trials, in a recent report four patients with multiply relapsing WT were treated with a combination of vincristine, irinotecan, temozolomide, and bevacizumab. Two had a complete response, and two had a partial response to treatment (Venkatramani et al. 2014). The respective dose-limiting toxicities were myelosuppression and diarrhea.
The Children’s Oncology Group (COG) AREN0321 renal tumour study investigated the response to irinotecan in combination with vincristine (VI regimen) in patients with newly diagnosed stage IV diffuse anaplastic measurable WT in a upfront window (Perlman 2005; Daw et al. 2014). Preliminary data seem to support the use of the VI combination in diffuse anaplastic tumors at relapse, since 11/14 (79 %) patients treated with VI window displayed partial remission.
7.9 Very-High-Risk Relapsed Wilms Tumors
Patients with relapsed diffuse anaplastic tumors have dismal long-term survival rate regardless of the site of relapse (Dome et al. 2002, 2006; Green et al. 1994). Blastemal-type WT after primary chemotherapy has been identified by the SIOP colleagues as a poor prognosis group at diagnosis; patients bearing this histological type of WT who relapse displayed a dismal prognosis after recurrence, comparable to diffuse anaplastic tumors (Reinhard et al. 2008).
Overall, very poor responses to any drug or combination have been reported in these patients. In the analysis by Pinkerton et al., one out of seven patients with unfavorable histology responded to second-line chemotherapy (Pinkerton et al. 1991); in the WILTOP study two partial responses to topotecan were observed out of 11 diffuse anaplastic recurrent tumors (Metzger et al. 2007); no survivors were registered among nine anaplastic WT who relapsed, in the retrospective analysis of the S. Jude Hospital’s survey (Dome et al. 2002).
Differently than for standard- or some high-risk patients with relapsed WT, the major cause of initial treatment failure was relative under treatment as opposed to the development of drug resistance, and we can speculate that for very-high-risk children, the intrinsic resistance to drugs is the main cause of failure, both at diagnosis and at relapse. Because very-high-risk patients will have received most conventional active agents in their initial therapy, inclusion into trials of novel agents is justified for these patients.
In general, these children should be referred to centers that are conducting research trials on novel agents in the treatment of children with solid tumors.
7.10 International Cooperative Trials
As a result of the success of the multidisciplinary approach for the therapy of these rare tumors, most of the reported trials on the treatment of relapsed WT are based on small cohorts of patients treated in a non-randomized fashion and compared to historical controls. Due to the small numbers of patients with relapsed WT investigators from the Children’s Oncology Group, the International Society of Pediatric Oncology and the United Kingdom Children’s Cancer and Leukemia Group have been working together to develop a cooperative trial to study important questions about the treatment of these patients. A trial for the treatment of high-risk relapsed WT patients was proposed to determine if treatment with conventional intensive chemotherapy or with high-dose chemotherapy followed by autologous stem cell transplantation (ASCT) would be associated with a better outcome. This study would also estimate the differences in resource utilization between these two therapeutic approaches by collecting data on the number of hospital days and the extent of transfusion support, as well as quality of life measurements associated with each therapeutic approach. Despite the international collaboration, this study would require a long period of patient accrual and follow-up and a large investment of time and effort to accomplish the study goals. With the decrease in financial support for pediatric cancer trials, this study was not opened and therefore the question of the role of ASCT will remain unanswered.
In spite of recognizing the importance of the development of an international cooperation, these groups decide to proceed with the development of studies to determine the feasibility and toxicity of a chemotherapy regimen including either ifosfamide or cyclophosphamide, carboplatin, etoposide, with or without topotecan for the treatment of high-risk favorable histology WT patients. This studies will potentially serve as the template for future studies that may explore the combination of chemotherapy with novel biologic agents.
7.11 New Agents, Novel Approaches
Since the number of relapsed WT cases is limited, there have been few WT children entered in phase I or II studies for relapsed pediatric solid tumors. Apart from isolated case reports on single promising agents, like taxane (Italiano et al. 2005; Ramanathan et al. 2000), scanty data come from controlled clinical trials.
Oxaliplatin has a broad antitumor activity including tumors resistant to carboplatin. However, since the data available is from two patients enrolled on two different phase I pediatric trials (oxaliplatin alone (Spunt et al. 2007) and oxaliplatin/etoposide (McGregor et al. 2009)), with no documented response, no conclusion can be made about the potential efficacy of this agent for the treatment of recurrent WT.
Antiangiogenic strategies have been investigated, concentrating on the activity of vascular endothelial growth factor (VEGF) as a potential target (Ghanem et al. 2003). However, what emerged was that the pathways regulating angiogenesis in WT are very complex, and single-drug therapy is likely to be unsuccessful due to the early onset of resistance. Bevacizumab, a monoclonal antibody directed against the VEGF, was administered in a phase I study conducted by the Children’s Oncology Group (COG) that included two patients with WT. Neither patient had an objective response. Bevacizumab was also administered to two children with WT on a compassionate basis (no information on their histology is available) (Benesch et al. 2008). Temporary disease stabilization was achieved in both patients, the second case being treated in combination with topotecan. Instead of targeting the ligand, some of the newer agents inhibit the VEGF tyrosine kinase-signaling receptors, VEGFR-1 and VEGFR-2. As a group, the tyrosine-kinase inhibitors are less specific and may affect signaling at varying degrees through parallel angiogenic pathways platelet-derived growth factor receptor (PDGFR) and FGFR. In the more recent studies in adults, antiangiogenic agents have been tested in combination with cytotoxic chemotherapy, with a potential additive or even synergistic effect.
A phase II trial by the COG testing the differentiation effect of all-trans-retinoic acid and interferon-α2A enrolled 14 evaluable WT patients, and no responses were registered (Adamson et al. 2007). Despite this, a recent case report by Witt et al. of a patient with a chemotherapy-resistant refractory bilateral nephroblastomatosis showed an excellent response to 13-cis retinoic acid in combination with vincristine and dactinomycin (Witt et al. 2009).
7.12 Biology
Although there are increasing data on molecular genetic factors present in the tumor at diagnosis, there is little information regarding the molecular genetic events acquired between primary tumors and subsequent relapse, to gain insights into the molecular basis of tumor progression or relapse, or the mechanisms through which tumor cells home into different sites of relapse.
There are only scanty data on the specific cellular pathways involved in tumor progression or metastasis, mainly relating to presence of TP53 mutations (Bardeesy et al. 1995). Whether anaplasia and/or 17p/TP53 acquired mutation also confers an additional higher attitude to disseminate is not clear. Natrajan et al. revealed that the most significant abnormality acquired between paired primary and recurrent tumors was loss of 17p, the locus of the TP53 gene (Natrajan et al. 2007).
There is an urgent clinical need to define the involvement of pathways for which targeted therapies already exist in the progression or relapse of WT. Natrajan et al. interestingly documented an acquired gain at 15q, to which the IGF1R gene maps. IGF1R copy number gain and overexpression may be seen as steps leading to relapse, opening to a possible role for anti-IGF1R in the therapy for recurrent Wilms tumor.
7.13 Future Directions
Advancements in the treatment of relapsed WT resulting in improvement in the outcomes of high-risk patients and in the decrease in the morbidity of relapse therapy for those who currently have a very good outcome with respect to disease control will only be feasible through the development of well-designed clinical trials and international cooperation.
These studies should include biologic evaluation of the recurrent tumors that may provide insights into the genetic mechanisms of drug resistance, tumor progression, and relapse. The identification of these molecular events may provide new targets for novel therapeutic approaches to be used in future trials for the treatment of these patients.
References
Abu-Ghosh AM, Krailo MD, Goldman SC et al (2002) Ifosfamide, carboplatin and etoposide in children with poor-risk relapsed Wilms’ tumor: a Children’s Cancer Group report. Ann Oncol 13:460–469
Adamson PC, Matthay KK, O’Brien M, Reaman GH, Sato JK, Balis FM (2007) A phase 2 trial of all-trans-retinoic acid in combination with interferon-alpha2a in children with recurrent neuroblastoma or Wilms tumor: a Pediatric Oncology Branch, NCI and Children’s Oncology Group Study. Pediatr Blood Cancer 49:661–665
Bardeesy N, Beckwith JB, Pelletier J (1995) Clonal expansion and attenuated apoptosis in Wilms’ tumors are associated with p53 gene mutations. Cancer Res 55:215–219
Benesch M, Windelberg M, Sauseng W et al (2008) Compassionate use of bevacizumab (Avastin) in children and young adults with refractory or recurrent solid tumors. Ann Oncol 19:807–813
Bomgaars LR, Bernstein M, Krailo M et al (2007) Phase II trial of irinotecan in children with refractory solid tumors: a Children’s Oncology Group Study. J Clin Oncol 25:4622–4627
Campbell AD, Cohn SL, Reynolds M et al (2004) Treatment of relapsed Wilms’ tumor with high-dose therapy and autologous hematopoietic stem-cell rescue: the experience at Children’s Memorial Hospital. J Clin Oncol 22:2885–2890
Casey DA, Wexler LH, Merchant MS et al (2009) Irinotecan and temozolomide for Ewing sarcoma: the Memorial Sloan-Kettering experience. Pediatr Blood Cancer 53:1029–1034
D’Angio GJ, Evans AE, Breslow N et al (1976) The treatment of Wilms’ tumor: results of the national Wilms’ tumor study. Cancer 38:633–646
D’Angio GJ, Evans A, Breslow N et al (1981) The treatment of Wilms’ tumor: results of the Second National Wilms’ Tumor Study. Cancer 47:2302–2311
Dallorso S, Dini G, Faraci M, Spreafico F (2008) SCT for Wilms’ tumour. Bone Marrow Transplant 41(Suppl 2):S128–S130
Daw NC, Anderson JR, Hoffer FA et al (2014) A phase 2 study of vincristine and irinotecan in mestastatic diffuse anaplastic Wilms tumor: results from Children’s Oncology Group Study AREN0321. J Clin Oncol 32 (5s) suppl abstr 10032.
De Camargo B, Melarango R, Saba e Silva N et al (1994) Phase II study of carboplatin as a single drug for relapsed Wilms’ tumor: experience of the Brazilian Wilms’ Tumor Study Group. Med Pediatr Oncol 22:258–260
Dome JS, Liu T, Krasin M et al (2002) Improved survival for patients with recurrent Wilms tumor: the experience at St. Jude Children’s Research Hospital. J Pediatr Hematol Oncol 24:192–198
Dome JS, Neale G, Hill DA et al (2005) Anti-tumor activity of topotecan against Wilms’ tumor: translation of a xenograft model to phase II study. Pediatr Blood Cancer 45:432–433
Dome JS, Cotton CA, Perlman EJ et al (2006) Treatment of anaplastic histology Wilms’ tumor: results from the fifth National Wilms’ Tumor Study. J Clin Oncol 24:2352–2358
Fuchs J, Szavay P, Luithle T, Furtwangler R, Graf N (2008) Surgical implications for liver metastases in nephroblastoma–data from the SIOP/GPOH study. Surg Oncol 17:33–40
Garaventa A, Hartmann O, Bernard JL et al (1994) Autologous bone marrow transplantation for pediatric Wilms’ tumor: the experience of the European Bone Marrow Transplantation Solid Tumor Registry. Med Pediatr Oncol 22:11–14
Ghanem MA, van Steenbrugge GJ, Sudaryo MK, Mathoera RB, Nijman JM, van der Kwast TH (2003) Expression and prognostic relevance of vascular endothelial growth factor (VEGF) and its receptor (FLT-1) in nephroblastoma. J Clin Pathol 56:107–113
Green DM, Breslow NE, Ii Y et al (1991) The role of surgical excision in the management of relapsed Wilms’ tumor patients with pulmonary metastases: a report from the National Wilms’ Tumor Study. J Pediatr Surg 26:728–733
Green DM, Beckwith JB, Breslow NE et al (1994) Treatment of children with stages II to IV anaplastic Wilms’ tumor: a report from the National Wilms’ Tumor Study Group. J Clin Oncol 12:2126–2131
Green DM, Cotton CA, Malogolowkin M et al (2007) Treatment of Wilms tumor relapsing after initial treatment with vincristine and actinomycin D: a report from the National Wilms Tumor Study Group. Pediatr Blood Cancer 48:493–499
Gross RE, Neuhauser EB (1950) Treatment of mixed tumors of the kidney in childhood. Pediatrics 6:843–852
Grundy P, Breslow N, Green DM, Sharples K, Evans A, D’Angio GJ (1989) Prognostic factors for children with recurrent Wilms’ tumor: results from the Second and Third National Wilms’ Tumor Study. J Clin Oncol 7:638–647
Ha TC, Spreafico F, Graf N, Dallorso S, Dome JS, Malogolowkin M, Furtwängler R, Hale JP, Moroz V, Machin D, Pritchard-Jones K (2013) An international strategy to determine the role of high dose therapy in recurrent Wilms’ tumour. Eur J Cancer 49(1):194–210. doi:10.1016/j.ejca.2012.07.010
Hale J, Hobson R, Moroz V, Satori P (2008) Results of UK Children’s Cancer and Leukemia Group (CCLG) protocol for relapsed Wilms tumor (UKWR): unified relapse strategy improves outcome. In: 40th meeting of International Society of Paediatric Oncology, p 62
Italiano A, Sirvent N, Michiels JF, Peyrade F, Otto J, Thyss A (2005) Tumour response to paclitaxel in an adult with relapsed nephroblastoma. Lancet Oncol 6:252–253
Kremens B, Gruhn B, Klingebiel T et al (2002) High-dose chemotherapy with autologous stem cell rescue in children with nephroblastoma. Bone Marrow Transplant 30:893–898
Kung FH, Desai SJ, Dickerman JD et al (1995) Ifosfamide/carboplatin/etoposide (ICE) for recurrent malignant solid tumors of childhood: a Pediatric Oncology Group Phase I/II study. J Pediatr Hematol Oncol 17:265–269
Kushner BH, Kramer K, Modak S et al (2006) Irinotecan plus temozolomide for relapsed or refractory neuroblastoma. J Clin Oncol 24:5271–5276
Lemerle J, Voute PA, Tournade MF et al (1983) Effectiveness of preoperative chemotherapy in Wilms’ tumor: results of an International Society of Paediatric Oncology (SIOP) clinical trial. J Clin Oncol 1:604–609
Malogolowkin MH, Casak SJ, Feusner J et al (1994) Carboplatin and etoposide alternating with ifosfamide and doxorubicin for the treatment of children with recurrent Wilms’ tumors. Proc Am Soc Clin Oncol 13:424, (abstract no. 1453)
Malogolowkin M, Cotton CA, Green DM et al (2008) Treatment of Wilms tumor relapsing after initial treatment with vincristine, actinomycin D, and doxorubicin. A report from the National Wilms Tumor Study Group. Pediatr Blood Cancer 50:236–241
Mascarenhas L, Lyden ER, Breitfel PP et al (2010) Randomized phase II window trial of two schedules of irinotecan with vincristine in patients with first relapse or progression of rhabdomyosarcoma: a report from the Children’s Oncology Group. J Clin Oncol 28:4658
McGregor LM, Spunt SL, Santana VM et al (2009) Phase 1 study of an oxaliplatin and etoposide regimen in pediatric patients with recurrent solid tumors. Cancer 115:655–664
Metzger ML, Stewart CF, Freeman BB 3rd et al (2007) Topotecan is active against Wilms’ tumor: results of a multi-institutional phase II study. J Clin Oncol 25:3130–3136
Natrajan R, Little SE, Sodha N et al (2007) Analysis by array CGH of genomic changes associated with the progression or relapse of Wilms’ tumour. J Pathol 211:52–59
Nitschke R, Parkhurst J, Sullivan J, Harris MB, Bernstein M, Pratt C (1998) Topotecan in pediatric patients with recurrent and progressive solid tumors: a Pediatric Oncology Group phase II study. J Pediatr Hematol Oncol 20:315–318
Pappo AS, Lyden E, Breitfeld P et al (2007) Two consecutive phase II window trials of irinotecan alone or in combination with vincristine for the treatment of metastatic rhabdomyosarcoma: the Children’s Oncology Group. J Clin Oncol 25:362–9
Pein F, Pinkerton R, Tournade MF et al (1993) Etoposide in relapsed or refractory Wilms’ tumor: a phase II study by the French Society of Pediatric Oncology and the United Kingdom Children’s Cancer Study Group. J Clin Oncol 11:1478–1481
Pein F, Tournade MF, Zucker JM et al (1994) Etoposide and carboplatin: a highly effective combination in relapsed or refractory Wilms’ tumor–a phase II study by the French Society of Pediatric Oncology. J Clin Oncol 12:931–936
Pein F, Michon J, Valteau-Couanet D et al (1998) High-dose melphalan, etoposide, and carboplatin followed by autologous stem-cell rescue in pediatric high-risk recurrent Wilms’ tumor: a French Society of Pediatric Oncology study. J Clin Oncol 16:3295–3301
Pein F, Rey A, de Kraker J et al (1999) Multivariate analysis of adverse prognostic factors (APF) in children with recurrent (Rec) Wilms’ tumor (WT) after initial treatment according to SIOP-6 or SIOP-9 strategies. Med Pediatr Oncol 33:170, (abstract no. 11)
Perlman EJ (2005) Pediatric renal tumors: practical updates for the pathologist. Pediatr Dev Pathol 8:320–338
Pinkerton CR, Groot-Loonen JJ, Morris-Jones PH, Pritchard J (1991) Response rates in relapsed Wilms’ tumor. A need for new effective agents. Cancer 67:567–571
Ramanathan RK, Rubin JT, Ohori NP, Belani CP (2000) Dramatic response of adult wilms tumor to paclitaxel and cisplatin. Med Pediatr Oncol 34:296–298
Reinhard H, Schmidt A, Furtwangler R et al (2008) Outcome of relapses of nephroblastoma in patients registered in the SIOP/GPOH trials and studies. Oncol Rep 20:463–467
Spreafico F, Bisogno G, Collini P et al (2008) Treatment of high-risk relapsed Wilms tumor with dose-intensive chemotherapy, marrow-ablative chemotherapy, and autologous hematopoietic stem cell support: experience by the Italian Association of Pediatric Hematology and Oncology. Pediatr Blood Cancer 51:23–28
Spunt SL, Freeman BB 3rd, Billups CA et al (2007) Phase I clinical trial of oxaliplatin in children and adolescents with refractory solid tumors. J Clin Oncol 25:2274–2280
Tannous R, Giller R, Holmes E et al (2000) Intensive therapy for high risk (HR) relapsed Wilms’ tumor (WT). A CCG-4921/POG-9445 study report. In: Proceeding of ASCO, p 588a, (abstract no. 2315)
Tournade MF, Lemerle J, Brunat-Mentigny M et al (1988) Ifosfamide is an active drug in Wilms’ tumor: a phase II study conducted by the French Society of Pediatric Oncology. J Clin Oncol 6:793–796
Tubergen DG, Stewart CF, Pratt CB et al (1996) Phase I trial and pharmacokinetic (PK) and pharmacodynamics (PD) study of topotecan using a five-day course in children with refractory solid tumors: a pediatric oncology group study. J Pediatr Hematol Oncol 18:352–361
Turner CD, Gururangan S, Eastwood J et al (2002) Phase II study of irinotecan (CPT-11) in children with high-risk malignant brain tumors: the Duke experience. Neuro Oncol 4:102–108
Vassal G, Giammarile F, Brooks M et al (2008) A phase II study of irinotecan in children with relapsed or refractory neuroblastoma: a European cooperation of the Société Française d’Oncologie Pédiatrique (SFOP) and the United Kingdom Children Cancer Study Group (UKCCSG). Eur J Cancer 44:2453–2460
Venkatramani R, Malogolowkin MH, Mascarenhas L (2014) Treatment of multiply relapsed wilms tumor with vincristine, irinotecan, temozolomide and bevacizumab. Pediatr Blood Cancer 61:756–9
Vujanic GM, Sandstedt B, Harms D, Kelsey A, Leuschner I, de Kraker J (2002) Revised International Society of Paediatric Oncology (SIOP) working classification of renal tumors of childhood. Med Pediatr Oncol 38:79–82
Wagner LM, McAllister N, Goldsby RE et al (2007) Temozolomide and intravenous irinotecan for treatment of advanced Ewing sarcoma. Pediatr Blood Cancer 48:132–139
Witt O, Hammerling S, Stockklausner C et al (2009) 13-cis retinoic acid treatment of a patient with chemotherapy refractory nephroblastomatosis. J Pediatr Hematol Oncol 31:296–299
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Spreafico, F., Malogolowkin, M.H. (2014). Treatment of Relapsed Wilms Tumor. In: Pritchard-Jones, K., Dome, J. (eds) Renal Tumors of Childhood. Pediatric Oncology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-44003-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-662-44003-2_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-44002-5
Online ISBN: 978-3-662-44003-2
eBook Packages: MedicineMedicine (R0)