Abstract
Sphingolipids are biomolecules with diverse physiological functions in signaling as well as plasma membrane structure. They are associated with either cellular membranes or plasma lipoproteins and any changes in their levels may contribute to certain metabolic diseases. Sphingolipids are evenly distributed in lipoproteins and may be used as prognostic and diagnostic markers. Mechanisms involved in the transport of sphingolipids have been recently explored and here we discuss the most recent advances in the molecular mechanisms of sphingolipids transport by lipoproteins. It has been shown that microsomal triglyceride transfer protein (MTP) and ATP-binding cassette transporter family A protein 1 (ABCA1) play an important role in plasma sphingolipid homeostasis. However, the exact mechanisms are not well known. Though much research has already been done to emphasize the impact of sphingolipids changes in many pathological disorders, understanding mechanisms by which circulating lipoproteins assist in transporting sphingolipids may provide novel information that may help in devising strategies to therapeutically target these pathways to treat various metabolic disorders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- ABCA1
- Abetalipoproteinemia
- Ceramides
- Hexosylceramides
- Lipoproteins
- MTP
- Sphingolipids
- Sphingomyelin
- Sphingosine-1-phosphate
- Tangier disease
5.1 Introduction
Sphingolipids are not only involved in membrane organization as structural lipids but also act as essential signaling biomolecules [1]. The homeostasis of sphingolipids is maintained by regulating their synthesis and degradation in the cells. Ceramides (Cer) act as key precursors in the de novo synthesis of other sphingolipids such as glycosphingolipids, sphingomyelin (SM), sphingosine-1-phosphate (S1P), etc. [1]. Sphingolipids can also be synthesized through salvage pathway by the re-acylation of sphingosine in the lysosomes to form Cer or its derivatives [2]. Newly synthesized sphingolipids are secreted and transported by lipoproteins or remain associated within cells as structural lipids. In recent years new knowledge has been gained in understanding intracellular transport and secretion of different sphingolipids. Here, we summarize an overview of the most recent advances that have been made to understand pathways involved in the intracellular transport of sphingolipids by lipoproteins and highlight deficiencies that need to be resolved in future research.
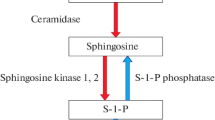
5.2 Biosynthesis of Sphingolipids
Biosynthesis of sphingolipids involves either de novo synthesis in the endoplasmic reticulum (ER) or catabolism of other sphingolipids via the salvage pathway [1, 2]. Cer acts as central precursor molecules in the synthesis of other sphingolipids. They are transported from the ER to Golgi via either transport vesicles or ceramide transfer protein (CERT) [3]. The mode of transport from the ER to Golgi may determine the fate of Cer as a precursor molecule for biosynthesis of different sphingolipids [3]. CERT dependent transport of Cer from the ER to Golgi appears to be necessary for the synthesis of SM [4, 5] as dysfunctional CERT in cells reduces the levels of SM but not glucosylceramides (GluCer) [5]. Sphingomyelin synthase 1 (SMS1) inside the Golgi lumen helps in the synthesis of SM from Cer by transferring a phosphorylcholine group from phosphatidylcholine onto Cer [6, 7]. The synthesized SM is then transported to the plasma membrane to form lipid rafts with cholesterol [7]. Synthesis of GluCer from Cer that are transported via transport vesicles from ER to Golgi occurs on the cytoplasmic side of the cis Golgi. Translocation of Cer from the lumenal side to cytoplasmic side for the biosynthesis of GluCer involves possibly unidentified transporters. These glycosylated Cer can be translocated back to the Golgi lumen and transferred to the trans Golgi network by both vesicular and non-vesicular transport for the biosynthesis of lactosylceramides (LactCer) which are precursors for more complex glycosphingolipids [3]. Besides SM and GluCer, Cer can also be de-acylated in the ER to form sphingosine, which is further phosphorylated to form S1P. They can also be phosphorylated in the Golgi to form ceramide 1-phosphate (C1P) [8].
5.3 Lipoproteins as Lipid Transporters
Since lipids are insoluble in water, they need to associate with proteins in order to transport in the circulation [9, 10]. Lipoproteins are complex particles containing both polar and non-polar lipids along with apolipoproteins. Classification of lipoproteins is based on their size and flotation densities [9]. They are mainly classified into four major entities from low density to high density as chylomicrons, very low density lipoproteins (VLDL), low density lipoproteins (LDL), and high density lipoproteins (HDLs) [9]. Liver and intestine are the main two organs that produce these lipoproteins. Chylomicrons are the largest size triglyceride rich particles which share a common structural apolipoprotein, apolipoprotein B (apoB), with VLDL and LDL. Conversely, HDL lacks this protein and contains apolipoprotein A1 (apoA1) as the core structural protein. Assembly of chylomicrons and VLDL takes place in the intestine and liver, respectively, and essentially requires the presence of MTP for the lipidation of apoB [11, 12]. Formation of LDL occurs after the hydrolysis of triglycerides on VLDL by the lipases. These LDL are then taken up by the peripheral tissues as a source of fatty acids through LDL receptors.
Unlike chylomicrons and VLDL, HDL is synthesized extracellularly after the secretion of apoA1 by the enterocytes and hepatocytes. ApoA1 from intestine and liver interact with the membrane bound ABCA1 and accept phospholipids and unesterified cholesterol to form discoidal pre-β HDL which is then converted to HDL in the plasma after the esterification of cholesterol by lecithin–cholesterol acyltransferase (LCAT) [13, 14]. HDL accepts more cholesterol from these peripheral tissues through ABCA1 and ABCG1 cholesterol efflux which is then delivered to the liver and steroidogenic tissues after the interaction with the scavenger receptor B1 (SR-B1) [15].
Lipoproteins play an important role in the absorption and transport of dietary lipids in the circulation to peripheral tissues. Any abnormality in the functioning of MTP or ABCA1 leads to conditions that affect the lipoprotein levels in the circulation. Abetalipoproteinemia is one of the rare diseases characterized by a defect in the assembly or secretion of plasma VLDL and chylomicrons due to mutations in MTP [16]. Similarly, mutation in ABCA1 leads to a condition called Tangier disease which is characterized by low HDL levels in the plasma [17].
5.4 Secretion and Transport of Sphingolipids
Plasma sphingolipids may be used as potential biomarkers for several metabolic disorders [6, 18,19,20,21,22,23,24,25]. However, there is not much information known about the mechanisms that regulate plasma sphingolipids. It was recently shown that the pathways involved in the transport of sphingolipids from the intestine and liver are more complex than those involved in other lipids [26, 27]. Like other lipids, sphingolipids also need apolipoproteins for their transport in the circulation. There are around 200 species of sphingolipids that are distributed on chylomicrons, VLDL, LDL, HDL, and albumin in the circulation [28,29,30]. These sphingolipids may be secreted from the cells and associated intracellularly with apoA1 or apoB-containing lipoproteins or effluxed to extracellular acceptors such as HDL or albumin from the plasma membrane. Here, we summarize the recent advances that have been made to understand the molecular mechanisms that are involved in the transport of sphingolipids.
5.4.1 Transport of Ceramides
Ceramides which constitute around 3% of plasma sphingolipids are equally distributed in apoB- (~49%) and apoA1-containing (~41%) lipoproteins (Table 5.1) [30]. However, similar to triglycerides, transport of Cer to the plasma is critically dependent on the presence of MTP in the liver and intestine. We have previously shown that mutation in MTTP gene in abetalipoproteinemia subjects or mice lacking hepatic and intestinal MTP (L,I-Mttp−/−) resulted in ~82–95% decrease in plasma Cer compared to controls (Tables 5.2 and 5.3). Furthermore, tissue-specific ablation of MTP suggests that liver and intestine are both important in regulating the levels of Cer in the plasma [27]. This observation points to significant role MTP plays in Cer transfer to apoB-containing lipoproteins for their transport to plasma [26]. It is possible that other unknown proteins and mechanisms may exist to enrich lipoproteins with Cer. We have also shown that deficiency of ABCA1 in the intestine and liver tends to associate with lower plasma Cer levels (Table 5.4) [27], but the decrease was not as significant as that shown in MTP deficiency (Table 5.3) [26]. Similar findings were observed in Tangier subjects where the decrease in the plasma Cer level was only 35% as opposed to an 82% decrease in abetalipoproteinemia subjects compared to controls (Table 5.2). Interestingly, only hepatic ABCA1 and not intestinal ABCA1 play a major role in regulating the plasma Cer level (Table 5.4). Although ABCA1 may be involved in determining the plasma levels of Cer to some extent, but the data points towards MTP as being the major determinant of plasma Cer.
It is intriguing to see that transport and plasma levels of Cer are completely dependent on the presence of MTP and apoB-containing lipoproteins since Cer are synthesized by other cells also, apart from enterocytes and hepatocytes, that do not synthesize and assemble apoB-lipoproteins. Whereas hepatocytes and enterocytes may synthesize Cer for delivery to other tissues, it is possible that the non-apoB synthesizing cells may use Cer not for secretion but to synthesize other sphingolipids. Although the presence of MTP may be critical in determining the levels of plasma Cer, significant amounts of Cer are also found on HDL particles [30]. Not much is known about the mechanisms of incorporation of Cer onto HDL particles. It is likely that other plasma lipid transfer proteins such as phospholipid transfer protein (PLTP) which transfers phospholipids between HDL particles and cholesteryl ester transfer protein (CETP) which transfers cholesteryl ester from HDL to apoB-containing lipoproteins in exchange for triglycerides may transfer Cer from apoB-lipoproteins to HDL. Additionally, the degradation of SM by sphingomyelinases or direct efflux of Cer from plasma membranes may also contribute to HDL Cer. Further studies are needed to investigate all potential possibilities.
5.4.2 Transport of Sphingomyelin
Sphingomyelin constitutes around 20% of total phospholipids [31] and 87% of total sphingolipids [30] in the plasma. It is the most abundant sphingolipid in lipoproteins and is distributed around ~36% in VLDL/LDL and ~64% in HDL (Table 5.1) [30]. SM uses both apoB-dependent and apoB-independent pathways to reach circulation. Absence of MTP in abetalipoproteinemia subjects and liver and intestine (L,I-Mttp−/−) mice was associated with a decrease of ~41% and ~59% (Tables 5.2 and 5.3), respectively, in plasma SM levels compared to controls [26]. Conversely, absence of ABCA1 in Tangier subjects and mice was associated with a reduction of about 40% and 86% (Tables 5.2 and 5.4), respectively, in plasma SM levels [27]. These data suggest that MTP and ABCA1 could play a major role in modulating plasma SM levels in both humans and mice. Interestingly, liver specific ablation of MTP or ABCA1 in mice decreased the plasma SM levels by ~69% and ~88% (Tables 5.3 and 5.4), respectively [27], suggesting that liver may be the major contributor of SM in the plasma.
Neither MTP nor ABCA1 is involved in the synthesis of Cer or SM. However, MTP has been shown to transfer both Cer and SM between vesicles in vitro, suggesting that it can add Cer and SM during apoB-lipoprotein synthesis [26]. Similar to its role in cholesterol efflux, we predicted that ABCA1 might also be involved in SM efflux. However, ablation, downregulation, or overexpression of ABCA1 gene did not affect SM efflux to HDL suggesting that it may not directly participate in SM efflux [27]. These studies suggest that ABCA1 is indirectly involved in bringing SM to plasma compartment. It is possible that reduction of HDL due to absence of ABCA1 in Tangier subjects or ABCA1 ablated mice may indirectly diminish SM efflux to plasma HDL via an unknown membrane-embedded protein. Reduction in plasma SM in SMS2 knockout mice suggest that synthesis of SM by SMS2 on the plasma membrane may also contribute to HDL SM [32]. Furthermore, ability of PLTP to transfer SM between vesicles in vitro suggests that it may be involved in the transfer of SM from VLDL to HDL [33]. Further studies are needed to evaluate the possibility of other transporters in SM efflux.
5.4.3 Transport of Glycosphingolipids
Out of more than 50 species of complex glycosphingolipids that make up about 9–10% of plasma sphingolipids, the most abundant are GluCer and LactCer. They are mostly distributed on VLDL/LDL (~54–57%) and HDL (~42–44%) (Table 5.1) [30, 34]. Although reduction in plasma glycosphingolipid levels ameliorates atherosclerosis [35], very little is known about their origin in plasma lipoproteins. Unlike SM and Cer, MTP neither transfers glycosphingolipids between vesicles in vitro nor does its deficiency in humans and mice have any effect on plasma glycosphingolipids concentrations [26]. It is possible that glycosphingolipids may be effluxed to HDL in the plasma through yet unidentified protein(s) or mechanisms. ABCC1 and ABCA12 have been shown to transport GluCer in vitro [36] and in keratinocytes [37]. However, their role to efflux glycosphingolipids to apoA1 or HDL in plasma is still unknown. We have recently shown for the first time that ABCA1 is a critical determinant of plasma glycosphingolipids [27]. Deficiency of ABCA1 in humans and mice was associated with reduced plasma hexosylceramides (HexCer) levels. A reduction of ~69–89% in the levels of HexCer in Tangier subjects and liver and intestine ABCA1 knockout (L,I-Abca1−/−) mice (Tables 5.2 and 5.4) possibly suggest the existence of additional mechanisms in their transport from tissues to the plasma compartment. Hepatic ABCA1 plays a crucial role in determining plasma HexCer level since tissue-specific ABCA1 ablation in mice had predominant effect on their plasma levels (Table 5.4) [27]. In contrast, ablation or chemical modification of ABCA1 in Huh7 cells had no effect on GluCer efflux to HDL suggesting that ABCA1 may not be directly involved in their efflux [27]. These data may implicate that the reductions in plasma HexCer in ABCA1 deficient humans or mice may be secondary to low levels of HDL which may be needed to interact with different transporter proteins on plasma membranes for the efflux of HexCer. Further studies are needed to identify possible transporters that are involved in this process.
We have previously shown that plasma concentrations of LactCer in humans and mice differ significantly with humans containing higher concentrations of LactCer than mice [26, 27]. Furthermore, deficiency of ABCA1 reduces LactCer only in mice but not in humans (Tables 5.2 and 5.4) [27] suggesting that their levels may be regulated by different mechanisms. Conversely, studies have shown that deficiency of MTP in mice and humans has no effect on plasma LactCer (Tables 5.2 and 5.3) [26]. One plausible explanation is that ABCA1 and MTP probably do not play a significant role in regulating plasma LactCer level. Further studies are needed to determine potential proteins that are involved in this process.
5.4.4 Transport of Sphingosine 1-Phosphate
Sphingosine 1-phosphate is a bioactive signaling molecule abundant in plasma [38] and found mainly on HDL and albumin [29, 39]. Among all the lipoproteins, about 95% of S1P is present on HDL (Table 5.1). Majority of plasma S1P comes from erythrocytes, platelets, and endothelial cells [39, 40] with some contribution from liver [41]. In our recent studies, we have shown that abetalipoproteinemia or Tangier subjects have no significant difference in the levels of S1P compared with controls suggesting that neither MTP nor ABCA1 may be involved in the transport of S1P in humans (Table 5.2) [26, 27]. Even though we observed a decrease of around 43–55% in the plasma SIP levels in MTP and ABCA1 deficient mice (Tables 5.3 and 5.4), this difference was not statistically significant [26, 27]. These data suggest that MTP and ABCA1 may not play a significant role in S1P transport from the cells to the circulation. Several proteins have been implicated in regulating the levels of plasma S1P. Cell surface membrane protein, spinster2, exports S1P to plasma [42]. Apolipoprotein M (apoM) plays an important role in the transport of S1P to plasma [43, 44]. Besides apoM, PLTP has also been shown to play a role in regulating plasma S1P levels [45].
5.5 Conclusion
In conclusion, we have summarized here that dependence of sphingolipids on lipoproteins as transporters is different among sphingolipids family. Sphingolipids utilize different mechanisms and carriers for their transport from cell membrane to plasma. Although MTP and ABCA1 seem to play an important role in regulating the levels of plasma sphingolipids (Fig. 5.1), their transport involve more complex and diverse mechanisms than are known for glycerolipids and sterol transport through apoB-lipoproteins or HDL. ABCA1- and MTP-dependent pathways may not be universal for all sphingolipids. Some of the sphingolipids such as LactCer, sphingosine, S1P, dihydrosphingosine, dihdyrosphigosine-1P, and dihydroceramide may reach circulation independently of these pathways [26, 27].
Impact of MTP and ABCA1 deficiencies on plasma sphingolipids transport. MTP and ABCA1 play an important role in the regulation of sphingolipids in the plasma mainly through their transport to apoB-lipoproteins or HDL. Presence of MTP and ABCA1 is critical for the transport of Cer and SM to plasma in humans and mice (a–d). Levels of Cer in the plasma are changed by both hepatic (e) and intestinal (g) MTP activity. Conversely, only hepatic (f) and not intestinal (h) ABCA1 regulates Cer level in the plasma. Furthermore, levels of SM in the plasma are modulated by the presence of MTP and ABCA1 in the liver only (e, f) and not in the intestine (g, h). In contrast to SM which is regulated by both hepatic MTP and ABCA1, only hepatic and not intestinal ABCA1 regulates the levels of HexCer, LactCer, and S1P in the plasma (f)
Our recent findings suggest that transport of sphingolipids apparently involves at least three different mechanisms (Fig. 5.1). First, MTP may contribute to plasma levels of sphingolipids by directly transferring Cer and SM to apoB-containing lipoproteins [26]. Second, HDL may act as an acceptor for Cer, HexCer, and SM from cells [27]. Third, some of the sphingolipids such as LactCer and S1P may reach circulation via different pathways independently of apoB-containing lipoproteins and HDL [26, 27]. The reason why sphingolipids use different mechanisms for their transport might be related to their diverse functions. These new findings highlight the importance of plasma lipoproteins in transporting sphingolipids and provide novel insights into mechanisms of sphingolipids secretion and transport. Further studies are warranted to unravel the existence of multiple mechanisms involved in the sphingolipids transport pathways.
Abbreviations
- ABCA1:
-
ATP-binding cassette transporter A1
- apoA1:
-
Apolipoprotein A1
- apoB:
-
Apolipoprotein B
- apoM:
-
Apolipoprotein M
- Cer:
-
Ceramides
- CERT:
-
Ceramide transfer protein
- CETP:
-
Cholesteryl ester transfer protein
- C1P:
-
Ceramide 1-phosphate
- ER:
-
Endoplasmic reticulum
- GluCer:
-
Glucosylceramides
- HDL:
-
High density lipoproteins
- HexCer:
-
Hexosylceramides
- LactCer:
-
Lactosylceramides
- LCAT:
-
Lecithin–cholesterol acyltransferase
- LDL:
-
Low density lipoproteins
- MTP:
-
Microsomal triglyceride transfer protein
- PLTP:
-
Phospholipid transfer protein
- SR-B1:
-
Scavenger receptor B1
- SM:
-
Sphingomyelin
- SMS1:
-
Sphingomyelin synthase 1
- S1P:
-
Sphingosine-1-phosphate
- VLDL:
-
Very low density lipoproteins
References
Borodzicz, S., Czarzasta, K., Kuch, M., & Cudnoch-Jedrzejewska, A. (2015). Sphingolipids in cardiovascular diseases and metabolic disorders. Lipids in Health and Disease, 14, 55.
Kitatani, K., Idkowiak-Baldys, J., & Hannun, Y. A. (2008). The sphingolipid salvage pathway in ceramide metabolism and signaling. Cellular Signalling, 20(6), 1010–1018.
D’Angelo, G., Uemura, T., Chuang, C. C., Polishchuk, E., Santoro, M., Ohvo-Rekila, H., et al. (2013). Vesicular and non-vesicular transport feed distinct glycosylation pathways in the Golgi. Nature, 501(7465), 116–120.
Wang, X., Rao, R. P., Kosakowska-Cholody, T., Masood, M. A., Southon, E., Zhang, H., et al. (2009). Mitochondrial degeneration and not apoptosis is the primary cause of embryonic lethality in ceramide transfer protein mutant mice. The Journal of Cell Biology, 184(1), 143–158.
Hanada, K., Kumagai, K., Yasuda, S., Miura, Y., Kawano, M., Fukasawa, M., et al. (2003). Molecular machinery for non-vesicular trafficking of ceramide. Nature, 426(6968), 803–809.
Iqbal, J., Walsh, M. T., Hammad, S. M., & Hussain, M. M. (2017). Sphingolipids and lipoproteins in health and metabolic disorders. Trends in Endocrinology and Metabolism, 28(7), 506–518.
Deng, Y., Rivera-Molina, F. E., Toomre, D. K., & Burd, C. G. (2016). Sphingomyelin is sorted at the trans Golgi network into a distinct class of secretory vesicle. Proceedings of the National Academy of Sciences of the United States of America, 113(24), 6677–6682.
Simanshu, D. K., Kamlekar, R. K., Wijesinghe, D. S., Zou, X., Zhai, X., Mishra, S. K., et al. (2013). Non-vesicular trafficking by a ceramide-1-phosphate transfer protein regulates eicosanoids. Nature, 500(7463), 463–467.
Hussain, M. M. (2014). Intestinal lipid absorption and lipoprotein formation. Current Opinion in Lipidology, 25(3), 200–206.
Hammad, S. M. (2011). Blood sphingolipids in homeostasis and pathobiology. Advances in Experimental Medicine and Biology, 721, 57–66.
Hussain, M. M., Shi, J., & Dreizen, P. (2003). Microsomal triglyceride transfer protein and its role in apoB-lipoprotein assembly. Journal of Lipid Research, 44(1), 22–32.
Hussain, M. M., Rava, P., Walsh, M., Rana, M., & Iqbal, J. (2012). Multiple functions of microsomal triglyceride transfer protein. Nutrition & Metabolism (London), 9, 14.
Yancey, P. G., Bortnick, A. E., Kellner-Weibel, G., de la Llera-Moya, M., Phillips, M. C., & Rothblat, G. H. (2003). Importance of different pathways of cellular cholesterol efflux. Arteriosclerosis, Thrombosis, and Vascular Biology, 23(5), 712–719.
Rousset, X., Vaisman, B., Amar, M., Sethi, A. A., & Remaley, A. T. (2009). Lecithin: cholesterol acyltransferase—From biochemistry to role in cardiovascular disease. Current Opinion in Endocrinology, Diabetes, and Obesity, 16(2), 163–171.
Wang, X., Collins, H. L., Ranalletta, M., Fuki, I. V., Billheimer, J. T., Rothblat, G. H., et al. (2007). Macrophage ABCA1 and ABCG1, but not SR-BI, promote macrophage reverse cholesterol transport in vivo. The Journal of Clinical Investigation, 117(8), 2216–2224.
Wetterau, J. R., Aggerbeck, L. P., Bouma, M. E., Eisenberg, C., Munck, A., Hermier, M., et al. (1992). Absence of microsomal triglyceride transfer protein in individuals with abetalipoproteinemia. Science, 258(5084), 999–1001.
Oram, J. F. (2000). Tangier disease and ABCA1. Biochimica et Biophysica Acta, 1529(1–3), 321–330.
Hussain, M. M., Jin, W., & Jiang, X. C. (2012). Mechanisms involved in cellular ceramide homeostasis. Nutrition & Metabolism (London), 9(1), 71.
Hannun, Y. A., & Obeid, L. M. (2008). Principles of bioactive lipid signalling: Lessons from sphingolipids. Nature Reviews. Molecular Cell Biology, 9(2), 139–150.
Futerman, A. H., & Hannun, Y. A. (2004). The complex life of simple sphingolipids. EMBO Reports, 5(8), 777–782.
Gault, C. R., Obeid, L. M., & Hannun, Y. A. (2010). An overview of sphingolipid metabolism: From synthesis to breakdown. Advances in Experimental Medicine and Biology, 688, 1–23.
Lucki, N. C., & Sewer, M. B. (2012). Nuclear sphingolipid metabolism. Annual Review of Physiology, 74, 131–151.
Hannun, Y. A., & Obeid, L. M. (2018). Sphingolipids and their metabolism in physiology and disease. Nature Reviews. Molecular Cell Biology, 19(3), 175–191.
Sabourdy, F., Kedjouar, B., Sorli, S. C., Colie, S., Milhas, D., Salma, Y., et al. (2008). Functions of sphingolipid metabolism in mammals—Lessons from genetic defects. Biochimica et Biophysica Acta, 1781(4), 145–183.
Jahangir, Z., Bakillah, A., & Iqbal, J. (2018). Regulation of sphingolipid metabolism by MicroRNAs: A potential approach to alleviate atherosclerosis. Diseases (Basel, Switzerland), 6(3), 82.
Iqbal, J., Walsh, M. T., Hammad, S. M., Cuchel, M., Tarugi, P., Hegele, R. A., et al. (2015). Microsomal triglyceride transfer protein transfers and determines plasma concentrations of ceramide and sphingomyelin but not glycosylceramide. The Journal of Biological Chemistry, 290(43), 25863–25875.
Iqbal, J., Walsh, M. T., Hammad, S. M., Cuchel, M., Rader, D. J., & Hussain, M. M. (2018). ATP binding cassette family A protein 1 determines hexosylceramide and sphingomyelin levels in human and mouse plasma. Journal of Lipid Research, 59(11), 2084–2097.
Quehenberger, O., Armando, A. M., Brown, A. H., Milne, S. B., Myers, D. S., Merrill, A. H., et al. (2010). Lipidomics reveals a remarkable diversity of lipids in human plasma. Journal of Lipid Research, 51(11), 3299–3305.
Hammad, S. M., Al Gadban, M. M., Semler, A. J., & Klein, R. L. (2012). Sphingosine 1-phosphate distribution in human plasma: Associations with lipid profiles. Journal of Lipids, 2012, 180705.
Hammad, S. M., Pierce, J. S., Soodavar, F., Smith, K. J., Al Gadban, M. M., Rembiesa, B., et al. (2010). Blood sphingolipidomics in healthy humans: Impact of sample collection methodology. Journal of Lipid Research, 51(10), 3074–3087.
Nilsson, A., & Duan, R. D. (2006). Absorption and lipoprotein transport of sphingomyelin. Journal of Lipid Research, 47(1), 154–171.
Liu, J., Zhang, H., Li, Z., Hailemariam, T. K., Chakraborty, M., Jiang, K., et al. (2009). Sphingomyelin synthase 2 is one of the determinants for plasma and liver sphingomyelin levels in mice. Arteriosclerosis, Thrombosis, and Vascular Biology, 29(6), 850–856.
Jiang, X. C., Bruce, C., Mar, J., Lin, M., Ji, Y., Francone, O. L., et al. (1999). Targeted mutation of plasma phospholipid transfer protein gene markedly reduces high-density lipoprotein levels. The Journal of Clinical Investigation, 103(6), 907–914.
Scherer, M., Bottcher, A., Schmitz, G., & Liebisch, G. (2011). Sphingolipid profiling of human plasma and FPLC-separated lipoprotein fractions by hydrophilic interaction chromatography tandem mass spectrometry. Biochimica et Biophysica Acta, 1811(2), 68–75.
Chatterjee, S., Bedja, D., Mishra, S., Amuzie, C., Avolio, A., Kass, D. A., et al. (2014). Inhibition of glycosphingolipid synthesis ameliorates atherosclerosis and arterial stiffness in apolipoprotein E−/− mice and rabbits fed a high-fat and -cholesterol diet. Circulation, 129(23), 2403–2413.
Raggers, R. J., van Helvoort, A., Evers, R., & van Meer, G. (1999). The human multidrug resistance protein MRP1 translocates sphingolipid analogs across the plasma membrane. Journal of Cell Science, 112(Pt 3), 415–422.
Ishibashi, Y., Kohyama-Koganeya, A., & Hirabayashi, Y. (2013). New insights on glucosylated lipids: Metabolism and functions. Biochimica et Biophysica Acta, 1831(9), 1475–1485.
Proia, R. L., & Hla, T. (2015). Emerging biology of sphingosine-1-phosphate: Its role in pathogenesis and therapy. The Journal of Clinical Investigation, 125(4), 1379–1387.
Ksiazek, M., Chacinska, M., Chabowski, A., & Baranowski, M. (2015). Sources, metabolism, and regulation of circulating sphingosine-1-phosphate. Journal of Lipid Research, 56(7), 1271–1281.
Pappu, R., Schwab, S. R., Cornelissen, I., Pereira, J. P., Regard, J. B., Xu, Y., et al. (2007). Promotion of lymphocyte egress into blood and lymph by distinct sources of sphingosine-1-phosphate. Science, 316(5822), 295–298.
Ikeda, H., Ohkawa, R., Watanabe, N., Nakamura, K., Kume, Y., Nakagawa, H., et al. (2010). Plasma concentration of bioactive lipid mediator sphingosine 1-phosphate is reduced in patients with chronic hepatitis C. Clinica Chimica Acta, 411(9–10), 765–770.
Nagahashi, M., Kim, E. Y., Yamada, A., Ramachandran, S., Allegood, J. C., Hait, N. C., et al. (2013). Spns2, a transporter of phosphorylated sphingoid bases, regulates their blood and lymph levels, and the lymphatic network. The FASEB Journal, 27(3), 1001–1011.
Kurano, M., Tsukamoto, K., Ohkawa, R., Hara, M., Iino, J., Kageyama, Y., et al. (2013). Liver involvement in sphingosine 1-phosphate dynamism revealed by adenoviral hepatic overexpression of apolipoprotein M. Atherosclerosis, 229(1), 102–109.
Liu, M., Seo, J., Allegood, J., Bi, X., Zhu, X., Boudyguina, E., et al. (2014). Hepatic apolipoprotein M (apoM) overexpression stimulates formation of larger apoM/sphingosine 1-phosphate-enriched plasma high density lipoprotein. The Journal of Biological Chemistry, 289(5), 2801–2814.
Yu, Y., Guo, S., Feng, Y., Feng, L., Cui, Y., Song, G., et al. (2014). Phospholipid transfer protein deficiency decreases the content of S1P in HDL via the loss of its transfer capability. Lipids, 49(2), 183–190.
Acknowledgments
Not applicable.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Availability of data and materials: Not applicable.
Competing interests: The authors declare that they have no competing interests.
Funding: This review was written with support from the KAIMRC grants (RA16–024-A and RA17–013-A) and the International Collaboration Initiative grant from the Ministry of Education, Saudi Arabia (RA20–005-A, Project #230) to JI.
Author’s contributions: Not applicable.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive licence to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Iqbal, J., Al Qarni, A., Bakillah, A. (2022). Molecular Mechanisms of Sphingolipid Transport on Plasma Lipoproteins. In: Jiang, XC. (eds) Sphingolipid Metabolism and Metabolic Disease. Advances in Experimental Medicine and Biology, vol 1372. Springer, Singapore. https://doi.org/10.1007/978-981-19-0394-6_5
Download citation
DOI: https://doi.org/10.1007/978-981-19-0394-6_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-0393-9
Online ISBN: 978-981-19-0394-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)