Abstract
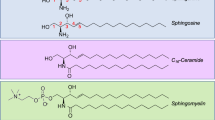
Sphingolipidoses is a cluster of genetic rare disorders regarding glycosphingolipid metabolism, classified as lysosomal storage disorders (LSD). Here, we focus on eight inheritable diseases, including GM1 gangliosidosis, GM2 gangliosidosis, Fabry disease, Gaucher’s disease, metachromatic leukodystrophy, Krabbe disease, Niemann–Pick disease A and B, and Farber disease. Mostly, pathogenic mutations in the key enzyme are loss-function, resulting in accumulation of substrates and deficiency of products. Thus, cellular overload of substrates causes lipotoxicity, which is deleterious to cellular and organ function. In the terms of clinical manifestations in sphingolipidoses, multiple systems and organs, especially central nervous system (CNS) are usually affected. As for diagnosis strategy, enzymatic activity assay and genetic sequencing are helpful. Up till now, limited treatment approaches have approved for treating sphingolipidoses, with some potential strategies for further evaluation. In general, enzyme replacement therapy (ERT), substrate reduction therapy (SRT), and molecular chaperones are feasible choices for enzyme deficiency disorders, but these therapies are limited to relieve CNS lesions and symptoms due to prevention from blood–brain barrier. Other possible treatments such as gene therapy, bone marrow transplantation (BMT), and hematopoietic stem cell transplantation (HSCT) need further evaluation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Glycosphingolipid
- Sphingolipidoses
- Lysosomal storage disorder
- GM1 gangliosidosis
- GM2 gangliosidosis
- Fabry disease
- Gaucher’s disease
- Metachromatic leukodystrophy
- Krabbe disease
- Niemann–Pick disease A and B
- Farber disease
13.1 GM1 Gangliosidosis
13.1.1 Condition and Genetic Defects
GM1 storage disorder termed GM1 gangliosidosis is a rare neurodegenerative lysosomal storage disease caused by β-galactosidase (β-Gal) deficiency due to mutation in the GLB1 gene [1, 2]. The GLB1 gene (MIM *611458) is located on the short arm of the chromosome 3 (3p22.3), comprising 16 exons. Up to now, about 293 different genetic variants associated with GM1 gangliosidosis have been reported and most of them are categorized as missense mutations [3].
The overall incidence of GM1 gangliosidosis has been estimated to be 1 in 100,000–200,000 live births wordwide [4], with elevated incidence in some certain populations, which may be biased by the founder’s effect [4,5,6,7]. For instance, increased prevalence was previously reported in Porto Alegre city at south Brazil (1:1700) [5, 6], in Malta (1:3700) [7], which may be closely related with a higher frequency of disease carriers, around 8.3% at the village of Pelendri in Cyprus [8] and 1:30 in Malta [7].
β-Gal is the first enzyme in the catabolism of complex glycosphingolipids, responsible for the degradation of glycoproteins, glycolipids, and keratan sulfate, all of which perform essential roles in cellular signaling and structure [9]. This deficiency results in abnormal deposition of GM1 gangliosides in neuronal organs and glycosaminoglycans or glycopeptides in visceral tissues [10, 11].
13.1.2 Lab Findings
Definitive diagnosis of GM1 gangliosidosis mainly relies on assaying the enzyme activity of β-Gal and genetic testing of GLB1 gene. Residual β-Gal activity in fibroblasts isolated from patients, measured using the artificial 4-methylumbelliferyl β-galactopyranoside substrate, varied in different disease subtypes, namely 0.07% to 1.3% of control values in infantile patients, 0.3% to 4.8% in the juvenile form, and up to 9% in adults [12].
Several objective biomarkers can reflect disease diversity of GM1 patients and would be useful for evaluating disease status and therapeutic response to clinical trials, including GM1 ganglioside concentration, aspartate aminotransferase (AST), lactate dehydrogenase (LDH), neuron-specific enolase, myelin basic protein and brain proton magnetic spectroscopy indexes [13, 14].
Targeted lipidomic is used to measure the storage of GM1 gangliosides in cerebrospinal fluid (CSF) samples. Although valuable, lipidomics analysis requires a liquid chromatography-tandem mass spectrometry (LC-MS/MS) assay only available in specialized laboratories. By contrast, AST and LDH are more commonly applied to monitor disease severity and treatment responses. It has been demonstrated that AST and LDH levels were obviously increased in the CSF samples collected from late-infantile patients, but not in most juvenile patients. Thus, AST and LDH could be ideal candidates for indicating disease severity [15, 16]. Furthermore, in peripheral blood samples from GM1 gangliosidosis patients, AST levels were correlated with disease severity, but LDH remained unchanged [13]. As a result, AST was emphasized to be a potential biomarker for clinical application [13]. Furthermore, recent studies have shown that patients with the infantile form showed a tenfold higher plasma chitotriosidase activity than those with the late-infantile form, indicating a correlation between chitotriosidase activity and clinical phenotype [17].
Except for the biochemical indicators in CSF and peripheral blood, brain proton magnetic spectroscopy indexes, such as N-acetylaspartate and myoinositol, have been proposed to monitor investigational approaches for GM1 gangliosidosis [18, 19]. Electroencephalography, 7T magnetic resonance imaging (MRI), and magnetic resonance spectroscopy were used to evaluate lesions in the brain of GM1 patients. Besides, pathologists have demonstrated that the brain is sometimes slightly infiltrated with inflammatory cells in GM1 gangliosidosis patients, which considered as pathophysiological responses to the lipid overloading in neurons and the abundance of antigenically acting gangliosides [20]. It is necessary to examine the expression of a panel of inflammatory markers in the CNS.
Overall, tracking of disease progression through clinical assessment will remain critically important, sensitive biomarkers are important tools for monitoring disease progression and evaluating the efficacy of treatment strategies.
13.1.3 Clinical Features and Diagnosis
The clinical manifestations of GM1 gangliosides results from the massive storage of GM1 gangliosides and related glycoconjugates in various tissues, especially in the CNS [21]. GM1 gangliosides in the gray matter of GM1 gangliosides patients could accumulate as much as threefolds more than that of healthy individuals [22]. Besides, GM1 gangliosides also accumulates in the viscera, producing complications such as hepatomegaly, cardiomegaly, skeletal deformities, joint stiffness, and muscle weakness.
Cognitive decline, muscular hypotonia, and seizures were the most frequent neurologic symptoms. Based on the age of onset and severity of symptoms, GM1 gangliosidosis has been classified into three major phenotypes: type I (infantile, MIM #230500), type II (late infantile/juvenile, MIM #230600), and type III (adult, MIM #230650). (1) The type I infantile form is the most severe, with life expectancy less than 3 years [21, 23], characterized by early onset between birth and 6 months with psychomotor regression, cherry-red spot, visceromegaly, and facial and skeletal abnormalities. (2) The type II form usually starts between 7 months and 3 years of age with slowly progressive neurological signs, such as early locomotor problems, seizures, strabismus, lethargy, muscle weakness, and terminal bronchopneumonia. Comparing to type I, dysmorphisms and skeletal changes are less severe [24]. (3) The adult form, also known as type III, the mildest phenotype of the disease, with onset between 3 and 30 years of age, is featured by cerebellar dysfunction, slurred speech, dystonia, mild vertebral deformities, and short stature [21]. Overall, the diagnosis of GM1 gangliosidosis is often delayed, particularly in the patients with milder forms or unclassical characteristics.
The residual activity of the mutant β-Gal directly linked with disease severity, as the enzymatic activity nearly absent in type I-associated mutations, but a small amount of residual activity in type II and type III patients [21, 25].
In rare cases, patients present with peripheral manifestations of β-Gal deficiency but without CNS involvement, for instance, one type of such disease termed as Morquio B disease, also called mucopolysaccharidosis IVB. The deficiency of β-Gal enzymatic activity, in combination with neuraminidase deficiency, is also present in a different disorder named galactosialidosis [26], due to a defect in the protective protein/cathepsin A [27], which stabilizes the β-galactosidase/neuraminidase complex [28]. Meanwhile, it should be pointed out that the predominant clinical symptoms of galactosialidosis are mainly resulted from severe neuraminidase deficiency, instead of the partial β-Gal enzyme deficiency [21].
Diagnosis of all subtypes of GM1 gangliosidosis is often achieved by β-Gal enzyme activity assay [1] and genetic testing through whole-genome sequencing or -exome sequencing of the GLB1 gene [29]. Furthermore, prenatal diagnosis is possible via amniocentesis especially for those candidates with GM1 gangliosidosis family history, or for those from both parents are carriers of a pathogenic allele [30].
At the same time, the detection of biochemical markers and neuroimaging changes are playing important roles during diagnosis and treatment.
13.1.4 Treatment and Advances
At present, there is no current effective FDA-approved treatment for GM1 gangliosidosis yet, only symptomatic and supportive therapy is available for these patients. Several therapeutic approaches have been explored by reducing substrate accumulation and promoting GM1 ganglioside catabolism. Targeted restoration of GM1 ganglioside catabolism occurs through gene therapy [31], stem cell transplantation [32], enzyme replacement therapy [33], and pharmacological chaperones [34] to increase the β-Gal activity, reduce neuronal lysosomal storage lesions, prevent the onset of neurological signs gait abnormalities, and extend the lifespan.
To date, the gene therapy based on adeno-associated virus (AAV) serotype 9 has been developed for GM1 gangliosidosis [35]. Related studies exhibited extraordinary efficacy in animal models, which demonstrated that AAV-mediated gene transferred to the brain can restore β-Gal expression in CNS and prevent the onset of neurological signs. Moreover, a phase I/II clinical trials is ongoing to evaluate the safety and efficacy of AAV-mediated GLB1 delivery by intravenous injection [30].
SRT is another alternative possible approach, which relies on residual β-Gal activity to remove ganglioside that has already accumulated. Therefore, it would not be effective enough for those symptomatic infantile GM1 patients with scarce or no residual β-Gal enzyme activity.
Hopefully, it has recently been reported that N-butyldeoxygalactonojirimycin (NB-DGJ), which functions as pharmacological chaperone that binds directly to misfold protein, improving its folding to increase its stability and promote its proper trafficking, showed favorable outcomes in infantile GM1 patients. NB-DGJ enhanced the activity of β-Gal up to ~4.5% of control activity within the first 24 h, and further significantly increased to ~10% within 6 days [36].
Besides, previous research has demonstrated that microglia/Mϕ activation plays a central role in the pathological process of GM1 gangliosides [20]. In this case, anti-inflammatory drugs might be an effective choice for the GM1 gangliosides, along with other proven therapies such as SRT [37] and bone marrow transplantation [38].
In the perspective of future available therapies, we are expecting more effective therapeutic methods that can be applied to clinical treatment for GM1 ganglioside patients.
13.2 GM2 Gangliosidosis
13.2.1 Condition
GM2 gangliosidosis is rare autosomal recessive LSD resulted from the deficiency of β-hexosaminidase (Hex) or GM2 activator protein (GM2-AP) activity, leading to the accumulation of GM2 ganglioside in the lysosome in neurons [39, 40]. GM2 gangliosides can be catabolized by the lysosomal hydrolases Hex through the hydrolysis of the N-acetylgalactosamine residues in normal conditions [41]. Hex are formed by the dimerization of α (HEXA, MIM *606869) and β (HEXB, MIM *6068732) subunits. Additionally, GM2-AP plays an important role in GM2 gangliosides degradation by presenting the gangliosides to α subunit of Hex [42].
GM2 gangliosidosis is caused by inherited enzyme deficiency, so that the accumulation of GM2 gangliosides deposits in the brain and surrounding organs, resulting in a series of clinical manifestations.
13.2.2 Genetic Defects
The GM2 gangliosidosis can be divided into Tay–Sachs disease (TSD, MIM #272800), Sandhoff disease (SD, MIM #268800), or GM2-AP deficiency (AB variant, MIM #27750), caused by the mutations in the genes of HEXA, GM2A, and double mutations of HEXA and HEXB (MIM *613109) [41]. Very few GM2A mutations have been reported in GM2 gangliosidosis [40].
13.2.3 Clinical Features
GM2 gangliosidosis are autosomal recessive, progressive neurodegenerative disorders.
TSD can be divided into three subtypes: classic infantile, juvenile, and adult late onset according to when symptoms appear. The incidence is approximately 1 in 320,000 newborns. Classic infantile is the most common and severe phenotype, losing the ability to turn over, sit, or crawl in 6 months old [43]. Seizures, axial hypotonia, cherry-red spot, regression in developmental milestones, and exaggerated startle response are the clinical features of TSD. Neuroimaging may implicate bilateral thalamic involvement, brain atrophy, and hypomyelination [40].
SD can also be divided into three subtypes and is clinically almost indistinguishable from TSD in neurodegenerative disorders, with infantile cases presenting as the most severe and rapidly progressing condition [22]. Ataxia, myoclonus, motor regression, psychotic episodes, intellectual disability, and progressive clumsiness are the clinical features of SD. Cerebellar atrophy can be discovered by neuroimaging [40].
GM2-AP deficiency is featured with dysphagia, muscle atrophy, cerebellar ataxia, dysarthric speech, manic depression, muscle weakness, psychotic episodes, and severe cerebellar atrophy, which are similar to those of TSD and SD [22].
The classical infantile form, with severely defective Hex enzyme activity, develops in infancy with developmental retardation, paralysis, dementia, blindness, and death usually by 2 or 3 years of age [40, 44]. Juvenile and adult types of late onset have a late onset with milder symptoms [45].
13.2.4 Diagnosis
In addition to the clinical characteristics, diagnosis is also supported by neuroimaging characterized by hyperdensity of basal ganglia, which can be accompanied by other changes in white matter and sometimes prominent, but non-specific, cerebellar atrophy [44].
Detection of Hex enzyme activity in peripheral blood can confirm the diagnosis [41]. At least, genetic testing of the HEXA, HEXB, and GM2A genes allows confirmation of all GM2 gangliosidosis subtypes [40].
13.2.5 Treatment
There is no proven treatment for TSD/SD and only supportive care is suggested for patients [22]. Several approaches have been explored for new treatments for GM2 gangliosidosis, including ERT, HSCT and BMT, SRT, pharmacological chaperone therapy, gene therapy, and gene editing approaches with AAV or CRISPR system [46].
ERT is a therapeutic alternative conceived in 1964 in which the lysosomal enzymes can be uptake through endocytosis and delivered to the lysosomes [47]. However, IDEAMLD phase I/II clinical trial (NCT01510028) showed that ERT may not be a definitive treatment for GM2 gangliosidosis with limited enzyme spread to the neuraxis [41]. Maegawa et al. found that pyrimethamine was the most prospective pharmacological chaperone for HexA because it can induce a threefold increase in enzyme activity on TSD fibroblasts [48, 49]. However, clinical trials with pyrimethamine showed an increase in enzyme activity but with little effect on the CNS manifestations [41, 50, 51]. What’s more, the intraperitoneal administration of EtDO-PIP2 can reduce the content of brain and liver gangliosides in SD mice, suggesting a potential treatment for ganglioside storage diseases with CNS manifestations [52]. HSCT can offer a potential alternative approach by delivering WT HexA and HexB with a patient’s own blood cells [46]. Additionally, gene therapy with AAV or CRISPR has been proved a 56% extension of the lifespan, a significant improvement motor function, and a slight therapeutic effect on the CNS in SD mice [53, 54]. It is possible that the co-administration of different therapies for GM2 gangliosidosis patients may be required.
13.3 Fabry Disease
13.3.1 Condition and Genetic Defects
Fabry disease (FD, MIM #301500) is a rare X-linked lysosomal storage disease caused by mutations in the GLA gene (Xq22; MIM *300644) resulting from deficient or absent activity of the lysosomal enzyme α-galactosidase A (α-Gal A) and glycolipid accumulation in many tissues [55], mainly in the form of globotriaosylceramide (Gb3). In 1898, Johann Fabry [56] and William Anderson [57] reported the skin lesion of Fabry disease, termed as angiokeratoma corporis diffusum. Nowadays, more than 1000 mutations in patients with Fabry disease have been identified [58]. According to individual genotype, the range of α-Gal A mutation phenotypes can vary widely [59]. In fact, the impacts of most reported α-Gal A mutations remain unclear [60]. Furthermore, an accurate estimation of the prevalence is complicated by the great phenotypic heterogeneity. The estimated incidence of FD is 1 in 117,000 live male births [61]. Because the atypic variant of the disease is underdiagnosed, the incidence might be underestimated in previous newborn screening surveys, and it may be much higher. The actual incidence of the disease may be approximately 1 in 8800 individuals in European [62,63,64]. In Asia, even higher frequencies have been noted, approximately 1 in 1600 males [65].
13.3.2 Clinical Features
The early-onset Type 1 “Classic” and Type 2 “Later-Onset” phenotypes are two major subtypes. Type 1 “Classic” is a classic variant subtype with systemic symptoms that begin in childhood and Type 2 “Later-Onset” is a late-onset variant subtype that develop in adulthood [66]. As FD is an X-linked disease, clinical manifestations are generally more severe and its progress is more rapid in males than in females. Some representative manifestations include periodic crisis of severe pain in the distal extremities, chronic neuropathic pain, sweating abnormalities (anhidrosis and hypohidrosis), angiokeratomas distributed in groin, hip and periumbilical areas, corneal (cornea verticillate) and lenticular opacities [67]. While in females, these symptoms present 5–10 years later and some even may be asymptomatic [68]. Besides multiple organs can be suffered, renal failure, left ventricular hypertrophy, gastrointestinal symptoms, strokes, and myocardial fibrosis often appear after 30 years old. In some cases, left ventricular hypertrophy might be the only manifestation [69].
13.3.3 Diagnosis
Within a detailed family history and physical examination, α-Gal A activity should be measured. α-Gal A activity <1% is highly suggestive for the diagnosis of classic FD [70]. Biopsy of the affected organ and “zebra bodies” are the distinctive characteristics [71, 72]. Elevated lyso-Gb3 in plasma and in urine is helpful for both initial diagnosis and long-term monitoring. Obviously, genetic testing of GLA is the golden criteria. Recently, some new methods have been explored to further elevate the accuracy, such as sensitive LC-MS method [73], dried blood spots (DBS), peripheral blood mononuclear cells measurement [74], and the proteomics approach [75]. Besides, calnexin, g-enolase, galectin-1 and relative miRNAs are new markers that have shown promising potential.
The chronic pain of FD should be discerned from fibromyalgia or rheumatologic pain diseases [76]. Systematic abnormities such as unexplained left ventricular hypertrophy, stroke, and renal failure should be screened and other diseases that also have the similar symptoms should be excluded [77].
13.3.4 Treatment
Current two treatment methods are intravenous administered ERT with agalsidase-α or agalsidase-β, and oral pharmacological chaperone therapy (Migalastat) or enzyme stabilizers along with other symptomatic remedies. Bone marrow transplantations may preferably be performed on young FD patients. Despite the above methods have achieved definite clinical effects, drawbacks like infusion-associated reactions, limited tissue penetration, and the formation of neutralizing antidrug antibodies cannot be negligible [78, 79]. Fortunately, there have been relative remedies to mitigate these effects [80, 81]. Nowadays, ERT, SRT, messenger RNA (mRNA), and gene therapy are novel methods [82]. Pegunigalsidase-alfa (PRX-102, Protalix Biotherapeutics) and Moss-αGal (Greenovation biopharmaceuticals) are two new forms of ERT [83]. Novel developed SRT molecules, like venglustat/ibiglustat [84] and lucerastat [85], aim to reduce production of Gb3 by inhibiting glucosylceramide synthase [86]. The mRNA therapy is a new class of therapy, and the administration of α-Gal mRNA can help stimulate the production of α-Gal [82]. For gene therapy, several different vectors (retroviral, lentiviral, adenoviral, adeno-associated viral and non-viral vectors) have been explored and may be an effective treatment option [87]. Additionally, Judit [88] explored α-Gal-loaded nanovesicles to treat FD and showed improved efficacy and good safety profile.
13.4 Gaucher’s Disease
13.4.1 Condition
Gaucher’s disease (GD) is a rare autosomal recessive disease characterized by a variety of clinical phenotypes, and yet it is the most common type in LSD. In 1882, Philippe Gaucher observed unusual cells in a patient’s spleen with splenomegaly and reported the disease for the first time. The prevalence of GD is about 1/40,000 to 1/50,000 worldwide, while it rises to approximately 1/600 in Jews of Ashkenazi population [89].
13.4.2 Genetic Defects
The GBA1 gene (MIM *606463) is located on chromosome 1 (1q22) and encodes glucocerebrosidase (GCase), one of the lysosomal enzymes. Homozygous or compound heterozygous pathogenic mutations in GBA1 gene damage the function of glucocerebrosidase in hydrolyzing its substrate, glucosylceramide, into β-glucose and ceremide, thus leading to the abnormal accumulations of glucosylceramide in macrophages [90]. More than 400 mutations in GBA1 gene have been discovered until recently, of which N370S, L444P, 84GG, and IVS2(+1) are most prevalent [91, 92]. The dominant mutations in Jews of Ashkenazi population are N370S, 84GG, IVS2(+1), and R496H [93, 94].
13.4.3 Lab Findings
Detection of GBA1 gene mutations based on genetic sequencing is necessary to establish the diagnosis of GD, which becomes a common diagnostic method due to the development in molecular science [95].
The measurement of GCase activity in patients is a requisite for diagnosing GD. Usually, the residual activity of GCase in GD patients is approximately between 10% and 15% compared to the normal standard [96].
The accumulation of glucosylceramide transforms macrophages into the typical “Gaucher cells” characterized with a “crumpled tissue paper” appearance. Those pathological cells deposit in several organs (such as liver, bone marrow, and spleen) and are the cause of most symptoms in GD. The presence of Gaucher cells in bone marrow aspiration helps to confirm the diagnosis of GD, but it’s not regarded as a routine examination [92].
About 90% of GD patients have thrombocytopenia with a different extent, meanwhile anemia and leukopenia are comparatively rare [97].
Chitotriosidase, CCL18, glucosylsphingosine, and ferritin are biomarkers of GD. Gaucher cells can produce a considerable amount of chitotriosidase and CCL18, resulting in high levels of these types of substances in plasma [98, 99]. Glucosylsphingosine, a newly found biomarker, is more sensitive than chitotriosidase and CCL18 regarding condition monitoring and is elevated in GD patient’s plasma as well [100]. The concentration of ferritin often elevates in GD, and excess iron in plasma is likely to accumulate in the liver and bone marrow, which may indicate the appearance of bone complications [101].
In imaging examinations, magnetic resonance imaging is recommended to evaluate the lesion in the liver, the spleen, and bone marrow in GD, because it is not radioactive and is suitable for monitoring the disease in repeated examinations [102].
13.4.4 Clinical Features and Diagnosis
According to the presence of neurological manifestations, GD is divided into 3 types, including non-neuronopathic GD (GD1, MIM #230800), acute neuronopathic GD (GD2, MIM #230900), and chronic neuronopathic GD (GD3, MIM #231000). The common phenotypes include splenomegaly, hepatomegaly, abnormal hemogram and, in some cases, impairments in bones. In neuronopathic GD, clinical features related to the central nervous system are important to identify patients in the early onset of disease. However, the correlation of phenotype and genotype remains uncertain as GD patients’ clinical manifestations are of high heterogeneity [103].
GD1, the most common type of GD, accounts for 90% to 95% of GD patients in Europe and North America [92]. Since the appearance and extent of clinical symptoms vary in different individuals, GD1 can be diagnosed at any age with a median age from 10 to 20 years old [104]. Most GD1 patients have enlarged or even massive spleen and sometimes have enlarged liver as well. Hematological disorders can be observed in part of patients in the forms of mucocutaneous bleeding and postoperative hemorrhage resulting from thrombocytopenia mainly [105]. Bone manifestation, like acute or chronic bone pain, is another typical symptom in GD1 patients, especially in children, and has a relationship with bone deformities, lesions and mass decline [106, 107]. With the progression of the disease, the respiratory system can be affected by the infiltration of Gaucher cells in lung presented with the interstitial disease [108]. Furthermore, about 35% of children diagnosed with GD1 had growth retardation and delayed puberty in a past cohort study [109].
GD2 is often characterized by early and severe clinical symptoms within the first year of life. Although patients also exhibit splenomegaly, thrombocytopenia, and growth retardation, the diagnosis of GD2 relies on distinguishing the feature of neurological impairment from non-neurological GD. Typical signs include rigidity of neck and trunk, difficulty in swallowing, laryngeal stridor, trismus, and oculomotor paralysis [110]. Central apnea accounts for about 50% of death in GD2, as Gaucher cells infiltrate lung leading to dysfunction of the respiratory system [111]. Of note, perinatal lethal form of GD2, also known as fetal GD, is the rarest, while at the same time, the most severe type exhibits hydrops fetalis, ichthyosis, facial dysmorphia, and central nervous system degeneration, resulting in fetal death in utero or soon after birth [111, 112]. This emphasizes the importance of carrying out newborn screening, next-generation sequencing, and carrier testing among high-risk populations to achieve early diagnosis of GD and minimize negative consequences.
Apart from observing visceral involvements which is similar to GD1, the identification of oculomotor nerve impairment, a slowed or absent horizontal saccadic eye movement, is necessary in diagnosing GD3 patients [113]. This can be the only neurological sign in some cases. GD3 patients may develop other severe neurological manifestations such as myoclonic seizures, cerebellar ataxia or spasticity and dementia [114, 115]. GD3a, GD3b, and GD3c are classical subtypes of GD3. Progressive myoclonic epilepsy constitutes the clinical feature in GD3a patients, and the symptom is less severe in type 3b comparatively [95, 114]. GD3c, the cardiac phenotype of GD3, is described with cardiac manifestations, of which calcification of the aortic and mitral valves and calcification of the aorta are the most typical characteristics [116].
Taken together, diagnosis of GD is mainly based on GBA1 gene sequencing mutations and the measurement of remaining GCase activity as mentioned above. The identification of Gaucher cells in biopsy of bone marrow and enlarged spleen can help confirm the diagnosis when GD patient has no obvious symptom, shows unexplained worsening blood count or displays no response to enzyme treatment [117].
13.4.5 Treatment
Two well-established treatments of GD are ERT and SRT.
ERT applies recombinant GCase via intravenous injection to compensate for the lack of GCase in cells. ERT for GD first appeared in the 1990s [118], and three types of ERT drugs, including imiglucerase, velaglucerase, and taliglucerase, have been applied in clinical use under marketing authorizations. These drugs can alleviate visceral and hematological involvements effectively. However, none of them improves neurological symptoms without the ability to cross the blood–brain barrier [95].
In SRT, the partial inhibitor restrains the function of the enzyme that synthesizes glucosylceramide to reduce the substrate of GCase. Miglustat and Eliglustat are two oral SRT drugs that have been approved officially to treat GD. Miglustat can be a replacement drug therapy when patients are intolerant of ERT [117]. Even though Miglustat can cross the blood–brain barrier, it exerts a subtle influence on neurological manifestations [119]. Given that Eliglustat, a ceramide analog, is a more potent drug and has fewer side effects than Miglustat and ERT drugs, it is now recommended as first-line therapy in the treatment of adult GD1 patients [120]. Patients are required to have CYP2D6 genotyping before using Miglustat, which is decomposed by cytochrome P450, to prevent certain drug–drug interactions [92]. Still, Eliglustat is unable to get into the central nervous system to ease neurological symptoms [121].
Splenectomy, orthopedic surgery, liver transplantation, and other symptomatic treatments are not regarded as routine therapies after the appliance of ERT and SRT, unless severe visceral complications exist, such as splenic rupture and pathological bone fractures.
As new emerging therapies, both gene therapies and the usage of molecular chaperones need further investigation and clinical trials [122, 123].
13.5 Metachromatic Leukodystrophy
13.5.1 Condition
Metachromatic leukodystrophy (MLD, MIM #250100) is an extremely rare autosomal recessive lysosomal storage disease and the estimated birth prevalence rate is 1.4–1.8 per 100,000 [124]. Most patients were of Caucasian ethnicity, followed by Asian [125]. Based on the age of onset, MLD is divided into three subtypes, namely late-infantile form (before 30 months), juvenile form (between 2.5–16 years), and adult form (after 16 years) [126]. Late-infantile patients account for the largest proportion of all clinical types of MLD patients [125].
13.5.2 Genetic Defects
MLD is an auto-recessive hereditary disorder characterized by arylsulfatase A (ASA) deficiency or, more rarely, defective sphingolipid activator protein B, saposin B (Sap-B) [125]. ASA plays an important role in the degradation of sulfatides which are mainly found in the myelin membranes and Sap-B assists this process by solubilizing the hydrophobic lipid [127]. Patients with MLD often show increased levels of 3-O-sulfogalactosylceramide (sulfatide) and 1-(3-O-sulfo-beta-d-galactosyl) sphingosine (lyso-sulfatide) [128, 129]. Sulfatides accumulate in several tissues, such as kidney, gallbladder, or bile ducts [130], but the progressive accumulation especially affects oligodendrocytes and Schwann cells, and leads to demyelination and axon loss, causing neurological symptoms [128, 130].
ASA is encoded by ARSA gene (22q13.33, MIM *607574), with 8 exons [125, 131]. Now more than 250 mutations of the ARSA gene have been reported [132], while the most common disease-causing variants are splice donor site variant c.465 + 1G > A, missense variants c.1283C > T (p.Pro428Leu) and c.542 T > G (p.Ile181Ser) [125, 133]. The splice donor site variant c.465 + 1G > A is regularly identified in the most severe late-infantile form [125, 133, 134]. However, missense mutations are the most common mutations observed in the late-infantile form, which leads to misfolding of ASA in the endoplasmic reticulum and subsequent proteasomal degradation, thus no functional enzyme can reach lysosome, subsequently causing sulfatides accumulation [134]. The other two missense variants mentioned above are usually detected in adult or juvenile patients [125, 133].
Sap-B is encoded by PSAP gene (MIM #176801), which is mapped to chromosome 10q22.1 and with 15 exons [125]. ASA activity is usually normal in patients with MLD due to Sap-B deficiency.
13.5.3 Clinical Features and Diagnosis
The clinical features of MLD are heterogeneous according to the subtypes. In patients with late-infantile form, impaired gross motor function is usually the first manifestation, such as abnormal movement patterns, walking difficulties, affected gait, and motor regression [134,135,136]. Motor function completely lost in late-infantile patients occurs no later than 40 months [135]. In late-infantile form, peripheral neuropathy symptoms usually appear before the central neuropathy symptoms and the symptoms usually manifest as clumsiness, muscle weakness, sensory deficits, and areflexia [126]. As the disease progresses, patients can develop other symptoms, such as mental regression, spastic tetraparesis, visual and auditory impairment, bulbar palsy, and seizures [126].
In juvenile patients, MLD is usually characterized by cognitive impairment and behavioral changes, which usually manifests as academic performance deterioration, attention difficulties, and disruptive behavior, followed by motor regression, such as slowness of movements, gait disturbances and balance impairment, and epilepsy [136, 137].
Adult patients often have symptoms of mental deterioration and behavioral abnormalities firstly [138]. Adult patients can also have neurological symptoms including pyramidal and cerebellar symptoms, usually accompanied by modification of speech [138]. The mean survival of adult patients is longer than the two other types [139]. In addition to nervous system, gallbladder is usually involved, such as polyp, gallstone, and increased thickness, and MLD patients is prone to neoplastic gallbladder abnormalities [140].
Whole-exome sequencing or whole-genome sequencing can be used to detect mutations to help genetic diagnosis [141,142,143,144]. To measure ARSA enzyme activity, samples from leukocyte lysate, or rarely, fibroblast lysate, can be incubated with synthetic chromogenic substrate p-nitrocatecholsulfate [145], and the assay can be conducted at 0 °C to reduce the interference of arylsulfatase B (ARSB) which can also hydrolyze the substrate [146]. To further improve accuracy, AgNO3 can be added to inhibit ARSB [146]. This assay can be read out photometrically [145]. A novel detection method using deuterated natural sulfatide substrate to measure ARSA enzyme activity in leukocytes or DBfS by LC-MS/MS is developed, which has high specificity and sensitivity [147]. Measuring blood sulfatides or sulfatides excretion in urine by LC-MS/MS is helpful for diagnosis in MLD [148, 149].
MRI is an important tool in the diagnosis of MLD. On proton density and T2-weighted images, diffuse and symmetric hyperintensities within the white matter can be seen, which is consistent with demyelination [150]. The corpus callosum is usually the initial area to be involved and abnormalities then spread to the periventricular white matter, while the subcortical fibers are spared at the early stage [137]. Within the abnormal white matter, there are hypointense signal abnormalities which can be divided into two appearances on T2I: tigroid stripes extending radially [134, 150] and dots like leopard-skin appearance [150, 151]. Proton magnetic resonance spectroscopy can evaluate motor and cognitive function by measuring the neuronal metabolite N-acetylaspartate levels which is a biomarker for neuronal and axonal loss [152]. Nerve conduction studies can detect decline of the peripheral nerve conduction velocity which is an early symptom to help diagnosis [138, 153].
Adult patients with MLD might be misdiagnosed with Alzheimer disease for early-onset progressive dementia [154]. Besides, the similar psychiatric symptoms of the adult MLD might lead to wrong diagnosis, such as manic depression, schizophrenia, organic disorders, or alcoholism [155].
Some ARSA gene alterations known as polymorphisms lead to an 10%–15% of normal ASA enzymatic activity, which is enough to prevent symptoms of disease, and these alleles are called pseudodeficiency alleles [156]. Sulfatide excretion in a 24-h urine sample helps distinguish ASA pseudodeficiency from MLD, in which MLD patients exhibit a large amount of sulfatide excretion [134].
Multiple sulfatase deficiency (MSD) is a rare disorder characterized by the deficiency of multiple sulfatases and combines the clinical features of diseases caused by deficiencies of individual sulfatases [157]. Some MSD patients with similar neuropathy symptoms, high protein in cerebrospinal fluid, and high sulfatide excretion in urine might be misdiagnosed as MLD, which can be distinguished by detecting other or total sulfatases, and specific manifestations including facial dysmorphia, skeletal deformities, and ichthyosis [134].
13.5.4 Treatment and Advances
HSCT can improve ASA enzyme activity and limit disease progression by halting further demyelination and immunomodulation [158,159,160]. Because of slow replacement of ASA deficient resident tissue, HSCT is only suitable for asymptomatic juvenile and adult patients, or patients with mild nervous system involvement, while the beneficial effects may be temporary and restricted to CNS symptoms [126, 137, 161, 162].
Gene therapy of MLD can be divided into bone marrow stem cell gene therapy and in vivo gene therapy [163]. Genetically modified autologous HSC by retrovirus and lentivirus transplantation can provide more functional enzyme for effected tissues and reduce the risk of graft-versus host disease, while it is only suitable for those who are identified at pre-symptomatic stage, which limits the application of this strategy [156, 164, 165]. In vivo gene therapy has developed three vectors: optimized adeno virus, adeno-associated virus, and lentivirus vectors [163]. AAV-based gene therapy is believed to be a promising way to transmit the gene message for ARSA gene directly to the CNS for sustained metabolic correction within the body [164, 166].
ERT has showed success in the treatment of many other LSDs, while the effectiveness of ERT in treating MLD is challenged by blood–brain barrier which is considered a powerful barrier preventing high molecular weight substances from reaching brain tissue [156, 167]. To solve this problem, intracerebroventricular and intrathecal ERT agent delivery are developed [156, 167].
13.6 Krabbe Disease
13.6.1 Condition
Krabbe Disease (KD, MIM #245200) was first described in 1916 by the Danish neurologist, Knud Krabbe [168]. It is a rare autosomal recessive lysosomal disorder due to deficiency of β-galactocerebrosidase, affecting primarily cerebral white matter and peripheral nerves [169]. The incidence of KD is about 1:100,000–1:250,000, and more than 90% of cases are proved as severe forms which often start during the infant time. Meanwhile, the adult-onset form of KD probably leads to the disability [170]. KD is a long-term disease that can be life-threatening especially in the early-onset form which can lead to death in early infancy [171].
13.6.2 Genetic Defects
KD is an autosomal recessive neurodegenerative disorder typically caused by a deficiency of the lysosomal enzyme galactocerebrosidase (GALC), encoded by gene GALC (14q31, MIM *606890). Up to date, more than 140 disease-causing mutations and polymorphisms have been reported, including missense, deletion nonsense, insertion, and deletion insertion variants. The effects of mutations are complicated due to the concomitant presence of polymorphisms [172]. Besides, a child at 3.5-month-old was reported as atypical KD with mutation in the prosaposin gene (PSAP, 10q22.1, MIM *176801), leading to saposin A deficiency, which functions as a kind of sphingolipid activator protein [173]. Another pathogenic mutation in PSAP was reported in a 7-month-old girl strongly suggested KD, but without enzymatic evidence nor genetic findings in GALC [174].
13.6.3 Clinical Features
Galactosylceramide, direct substrate of GALC, is the major lipid species in myelin, kidney, and epithelial cells of the small intestine and colon. Owing to this biology property, GALC loss-of-function mutations mainly lead to defects in nervous system, urinary system, and digestive system. The classifications for KD can be various. The classic one divides KD into five forms which is based on the age at onset of neurological symptoms: early-infantile (0 to 6 months), late-infantile (7 to 12 months), later onset (13 months to 10 years), adolescent (11 to 20 years) and adult (from 21 years on) [169]. The first two forms account for most of cases while the adult form is very rare [175]. In the terms of central neuropathy, Krabbe’s leukodystrophy is the outcome of demyelination in the brain, also known as globoid cell leukodystrophy.
The early-onset infantile KD is a severe rapidly progressing, demyelinating disease, and has typical clinical features including hyper-irritability, feeding difficulties, stiffness, elevated temperature, psychomotor regression, convulsive seizures, and vision loss. The other form of KD is late onset, the symptoms of which can be very various. Blindness, muscle weakness, and arrest of intellectual development are always evident. Other symptoms include behavioral problems, ataxia, and spastic paraparesis [176, 177].
13.6.4 Diagnosis
GALC activity measurement, genetic analysis, and psychosine measurement are the main diagnostic criteria which are performed only when the symptoms occur. Some early clinical evidence should be discovered to distinguish the KD in an early time [178].
Magnetic resonance imaging is one of the important diagnostic features and biomarkers for the description of the CNS pathology of KD [169]. The features differ according to the age of disease onset. The infantile onset form often presented with white matter hyperintensities which involve the dentate nuclei and cerebellar white matter. For the juvenile form, the parieto-occipital white matter is affected while the cerebellum is always normal. But the data for adult-onset patients is quite limited [179].
Shoko Komatsuzaki’s study showed the earlier onset of disease was strongly associated with a higher cerebrospinal fluid protein concentration which means it may be considered as a diagnostic biomarker in the appropriate clinical background of KD. However, since other diseases such as CNS infections and demyelinating diseases also have the similar laboratory findings, cerebrospinal fluid protein concentration can be very limited to specifically distinguish KD from other differential conditions [177].
The first-tier measurement of GALC enzymatic activity in DBS of the newborn alone can be unreliable due to common pseudodeficiency GALC gene variants. The psychosine has emerged as a valuable biomarker for diagnosis and prognosis of KD [180]. As for atypical KD with PSAP mutations, genetic sequencing supplemented with functional validation may be the proper practice at current status.
13.6.5 Treatment and Advances
KD is a long-term debilitating disease that can be life-threatening. Treatment options for KD include HSCT, gene therapy, bone marrow cell transplant, substrate reduction therapy, ERT, and the use of small molecules “chemical chaperones,” but some of which haven’t been conducted on human [181].
Currently, there is no FDA or EMA approved treatment for KD. Two investigational compounds, recombinant human GALC and ibudilast were granted orphan drug designation by the FDA. The former one produced by a method known as “recombinant DNA technology,” was also assigned orphan drug designation by the EMA in 2011 [171].
Some experimental therapeutic approaches are also focused on hematopoietic stem cells which can replace the missing enzyme. However, it is risky, expensive, and of uncertain efficacy [175].
Recent information reported by a group of public health and medical professionals showed that the diagnosis and prompt initiation of HSCT conducted before 30 days of life can improve the future symptoms considerably. Several states of America have begun considering about the necessity of KD newborn screening [182]. Inversely, some people question the efficacy of newborn screening for KD due to the false positives of the tests, and the efficacy of early HSCT [183].
However, prenatal diagnosis should be performed with measurement of GALC enzyme activity or molecular genetic testing if the family member was diagnosed of KD. Carriers testing of the family members is useful to prevent the risk for future pregnancies with potential disease [172].
13.7 Niemann–Pick Disease A and B
13.7.1 Condition
Niemann–Pick disease (NPD) is a genetic lipid storage disease, inherited in autosomal recessive mode, and characterized by developing hepatosplenomegaly, neuropathic symptoms, and recurrent lung infections close to birth. The first NPD patient reported by German pediatrician Albert Niemann in 1914 was an Ashkenazi Jewish infant. In 1961, Allen C. Crocker described four subtypes of NPD, type A to type D. Later, two more types, type E and F were delineated. Nevertheless, NPD-A (MIM #257200) and NPD-B (MIM #607616) are two classic forms with the majority, with frequency suggested to be 1 in 250,000 individuals [184]. From a worldwide perspective, approximately 1200 cases have been diagnosed as NPD-A or NPD-B. NPD-A is also known as the classic infantile form or the intermediate protracted neurovisceral form, while NPD-B is recognized as the visceral form [185], mainly based on clinical manifestations. The signs and symptoms of NPD-B are similar with NPD-A, but not as severe as NPD-A, thus NPD-B patients usually survive into adulthood.
13.7.2 Genetic Defects
NPD-A and NPD-B are caused by homozygous or compound heterozygous mutation of SMPD1 gene (MIM *607608), which is located on human chromosome 11 (11p15.4), encoding a lysosomal enzymatic protein termed acid sphingomyelinase (ASM). This 631-amino acid protein mainly functions in the hydrolysis of sphingomyelin to ceramide and phosphorylcholine [186, 187]. Respectively, ASM activity is completely absent in NPD-A, but is residual remaining in NPD-B. Pathogenic mutations in SMPD1 result in deficiency of acid sphingomyelinase, which leads to reduced degradation of sphingomyelin. Over time, the buildup of sphingomyelin causes lipotoxicity, further arouses cellular dysfunction or even apoptosis. Cell death further non-selectively impairs fundamental function of organs including the brain, lungs, the spleen, and the liver.
13.7.3 Clinical Features and Diagnosis
Symptoms of NPD are closely related with the tissues and organs where sphingomyelin abnormally accumulates, including peripheral symptoms (hepatosplenomegaly) and central symptoms (dementia, dysarthria, dysphagia, and ataxia). NPD-A is distinguished from NPD-B with impaired neurological function [188]. Most NPD-A patients show severe neuropathic symptoms and shorter lifespan compared to NPD-B subjects [185]. Moreover, typical cherry-red spots of the retina macula are common in NPD-A affected infants, and often combined with fatal interstitial lung diseases [189]. An early-stage diagnosis of NPD is established in observing the deficiency of acid sphingomyelinase activity in white blood cells or cultured skin fibroblasts. Prenatal diagnosis is anticipated via measuring sphingomyelinase enzymatic activity, or the neonatal screening panel based on the gene sequencing technique on uncultured or cultured chorionic villus sampling, or cultured amniocytes [190].
13.7.4 Treatment and Advances
Liver transplantation might be efficient for NPD individuals with severe liver and pulmonary dysfunction [191]. On the one hand, ERT, especially in NPD-B patients, has been proven worked in previous clinical trials [192]. On the other hand, no curable treatment is available for NPD-A so far. Meanwhile, recent study [193] has revealed that cerebellomedullary cistern injection of AAV serotype 9 encoding human ASM can effectively restore ASM activity in ASM knockout mice, which indicates the possibility of genetic therapy in clinical trials in NPD-A as well as other lysosomal storage brain disorders. Enzyme replacement therapy or gene therapy for treating NPD and other human sphingolipid disorders might be promising in the foreseeable future.
13.8 Farber Disease
13.8.1 Condition
Farber disease, also known as Farber’s lipogranulomatosis (MIM #228000), is an extremely rare autosomal recessive lysosomal storage disorder caused by mutations in the ASAH1 gene (MIM *613468). The first case was referred as “disseminated lipogranulomatosis” by Sidney Farber in 1952 [194]. Meanwhile, the mutated ASAH1 gene contributes to another disorder known as spinal muscular atrophy with progressive myoclonic epilepsy (SMA-PME) [195]. It was originally believed that Farber disease and SMA-PME were two independent diseases. However, there is an overlap in their clinical phenotypes with the appearance of more case reports. To date, less than 200 reported cases of Farber disease or SMA-PME have been identified worldwide based on literature search and the true incidence of this disease remains unknown.
13.8.2 Genetic Defects
The ASAH1 gene is mapped to chromosome 8p21.3-p22 and encodes human acid ceramidase enzyme (ACDase), which is a lysosomal hydrolase that degrades bioactive lipid ceramide into sphingosine and fatty acid [196, 197]. Mutations in ASAH1 lead to deficiency in ACDase and abnormal accumulation of ceramides in various tissues of the body, such as joints, bones, brain, liver, and spleen, and ultimately cause various clinical features.
13.8.3 Lab Findings
The ACDase activity assay measured in cultured skin fibroblasts and leukocytes, which is generally reduced to less than 10% of control cells, could provide valuable evidence for the diagnosis of Farber disease [198, 199]. Moreover, the significantly decreased enzyme activity in amniocytes and fetal fibroblasts is also employed in prenatal diagnosis [200].
In addition, excess ceramide concentrations could be detected in cultured cells as mentioned above or in biopsy specimens and body fluid samples from Farber disease patients [201,202,203]. In the recent decades, the fundamentally development of liquid chromatography and mass spectrometry allowed for detailed detection and quantification of ceramide species and their derivatives, which has been applied to demonstrating increased amount of ceramide species in tissues and cells and provided novel insights into the pathologic mechanism of Farber disease [204]. Based on this technique, C26:0 ceramide has been reported as a potential sensitive biomarker candidate for early detection and intervention [205].
The morphological change of subcutaneous nodules or other tissues from Farber disease patients mainly includes granulomas and lipid-laden macrophages (foam cells) infiltration. Ultrastructural analysis revealed the presence of characteristic comma-shaped curvilinear tubular Farber bodies, spindle-shaped bodies, and zebra-like bodies among different cell types [206,207,208].
Recent studies also found that monocyte chemoattractant protein 1 (MCP-1) was increased in plasma of Farber disease patients and animal models, which is consistent with the phenotype of inflammatory infiltration in tissues [204, 209]. It was suggested that MCP-1 could be a sensitive cytokine biomarker for differential diagnosis of Farber disease.
13.8.4 Clinical Features and Diagnosis
The clinical symptoms of Farber disease patients are varied and complicated. The most classic three phenotypes consist of subcutaneous nodules near joints, progressive immobilization and deformation of joints and hoarseness due to nodules formation within the larynx. Moreover, Farber disease is characterized as seven types via different clinical manifestations, age of onset, and the severity of this disorder. The following Table 13.1 summarized the main phenotypes of Farber disease and SMA-PME.
The primary clinical diagnosis of Farber disease is based on the classic triad as mentioned above. Generally, Farber disease might be initially misdiagnosed as juvenile idiopathic arthritis, rheumatoid arthritis, and juvenile hyaline fibromatosis due to its rarity and similar manifestations in joints and subcutaneous nodules [197, 213]. Therefore, further biochemical and genetic analyses are required. Enzyme activity assay and quantitation of excess ceramides described above are the two most methods assisting in definite diagnosis of Farber disease. Gene testing provides a conclusive diagnosis, especially for those with mild or non-classical symptoms, and SMA-PME patients.
13.8.5 Treatment and Advances
As for the management of this disease, there is no effective therapeutic method to date. The basic treatment are anti-inflammatory medications and physical therapy to relieve pain and related symptoms. HSCT was reported for the first time to treat a classic Farber disease case in 1989 [214]. Recently, a follow-up study evaluated the effects on 10 Farber disease patients who underwent HSCT within 15 years [215]. All the data revealed that abnormal inflammatory response could be corrected after HSCT, while neurological symptoms and signs could not be relieved. Therefore, for Farber disease patients without nervous system involvement, HSCT might be effective.
ERT has been commonly applied to clinical treatment of lysosomal storage disease such as Gaucher disease [216]. A recent study demonstrated that human recombinant acid ceramidase (rhACDase) derived from Chinese hamster ovary cells overexpressing ACDase significantly reduced ceramide in fibroblast from a Farber disease patient [217]. Meanwhile, the researchers administered rhACDase to the asah1P361R/P361R mutant mice (Farber disease mice) and found that the treatment improved their survival rate, normalized spleen size, decreased plasma MCP-1 levels, reduced macrophage infiltration in liver and spleen, and ceramide accumulation in tissues [217]. It was suggested that ERT might be promising treatment for Farber disease and further investigations are urgently required for clinical translation.
13.9 Summary
In this chapter, we give a brief review about these eight diseases belonging to sphingolipidoses. To further compare similarities and differences between them, Table 13.2 including genetic characteristics, molecular changes, clinical manifestations, and treatments is attached as follows. Overall, limited effective choices have been approved for treating sphingolipidoses, especially for those patients affected with CNS. Thus, further investigations are indeed warranted for better understanding and managing these life-threatening disorders.
Abbreviations
- AAV:
-
Adeno-associated virus
- ACDase:
-
Acid ceramidase enzyme
- ASA:
-
Arylsulfatase A
- AST:
-
Aspartate aminotransferase
- BMT:
-
Bone marrow transplantation
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- DBS:
-
Dried blood spots
- ERT:
-
Enzyme replacement therapy
- FD:
-
Fabry disease
- FDA:
-
Food and Drug Administration
- GALC:
-
Galactocerebrosidase
- Gb3:
-
Globotriaosylceramide
- GCase:
-
Glucocerebrosidase
- GD:
-
Gaucher’s disease
- GM2-AP:
-
GM2 activator protein
- Hex:
-
β-hexosaminidase
- HSCT:
-
Hematopoietic stem cell transplantation
- KD:
-
Krabbe disease
- LC-MS/MS:
-
Liquid chromatography-tandem mass spectrometry
- LDH:
-
Lactate dehydrogenase
- LSD:
-
Lysosomal storage disorders
- MCP-1:
-
Monocyte chemoattractant protein 1
- MLD:
-
Metachromatic leukodystrophy
- MRI:
-
Magnetic resonance imaging
- mRNA:
-
messenger RNA
- MSD:
-
Multiple sulfatase deficiency
- NB-DGJ:
-
N-butyldeoxygalactonojirimycin
- NPD:
-
Niemann–Pick disease
- Sap-B:
-
Saposin B
- SD:
-
Sandhoff disease
- SMA-PME:
-
Spinal muscular atrophy with progressive myoclonic epilepsy
- SRT:
-
Substrate reduction therapy
- TSD:
-
Tay–Sachs disease
- α-Gal A:
-
α-galactosidase A
- β-Gal:
-
β-galactosidase
References
Ferreira, C. R., & Gahl, W. A. (2017). Lysosomal storage diseases. Translational Science of Rare Diseases, 2, 1–71.
Caciotti, A., et al. (2011). GM1 gangliosidosis and Morquio B disease: An update on genetic alterations and clinical findings. Biochimica et Biophysica Acta, 1812, 782–790.
Stenson, P. D., et al. (2014). The human gene mutation database: Building a comprehensive mutation repository for clinical and molecular genetics, diagnostic testing and personalized genomic medicine. Human Genetics, 133, 1–9.
Sinigerska, I., et al. (2006). Founder mutation causing infantile GM1-gangliosidosis in the gypsy population. Molecular Genetics and Metabolism, 88, 93–95.
Coelho, J. C., Wajner, M., Burin, M. G., Vargas, C. R., & Giugliani, R. (1997). Selective screening of 10,000 high-risk Brazilian patients for the detection of inborn errors of metabolism. European Journal of Pediatrics, 156, 650–654.
Severini, M. H., Silva, C. D., Sopelsa, A., Coelho, J. C., & Giugliani, R. (1999). High frequency of type 1 GM1 gangliosidosis in southern Brazil. Clinical Genetics, 56, 168–169.
Lenicker, H. M., Vassallo Agius, P., Young, E. P., & Attard Montalto, S. P. (1997). Infantile generalized GM1 gangliosidosis: High incidence in the Maltese Islands. Journal of Inherited Metabolic Disease, 20, 723–724.
Georgiou, T., et al. (2005). The Arg482His mutation in the beta-galactosidase gene is responsible for a high frequency of GM1 gangliosidosis carriers in a Cypriot village. Genetic Testing, 9, 126–132.
Regier, D. S., et al. (2016). MRI/MRS as a surrogate marker for clinical progression in GM1 Gangliosidosis. American Journal of Medical Genetics. Part A, 170, 634–644.
Alniemi, S. T., Amin, S. R., Sculley, L., & Bakri, S. J. (2018). Ultrasound biomicroscopy in pseudophakic patients with unexplained recurrent hyphema or vitreous hemorrhage. Seminars in Ophthalmology, 33, 260–264.
Morrone, A., et al. (2000). Beta-galactosidase gene mutations affecting the lysosomal enzyme and the elastin-binding protein in GM1-gangliosidosis patients with cardiac involvement. Human Mutation, 15, 354–366.
Okumiya, T., Sakuraba, H., Kase, R., & Sugiura, T. (2003). Imbalanced substrate specificity of mutant beta-galactosidase in patients with Morquio B disease. Molecular Genetics and Metabolism, 78, 51–58.
Gray-Edwards, H. L., et al. (2017). Novel biomarkers of human GM1 Gangliosidosis reflect the clinical efficacy of gene therapy in a feline model. Molecular Therapy, 25, 892–903.
Satoh, H., et al. (2007). Cerebrospinal fluid biomarkers showing neurodegeneration in dogs with GM1 gangliosidosis: Possible use for assessment of a therapeutic regimen. Brain Research, 1133, 200–208.
Parakh, N., Gupta, H. L., & Jain, A. (2002). Evaluation of enzymes in serum and cerebrospinal fluid in cases of stroke. Neurology India, 50, 518–519.
Osuna, E., Perez-Carceles, M. D., Luna, A., & Pounder, D. J. (1992). Efficacy of cerebro-spinal fluid biochemistry in the diagnosis of brain insult. Forensic Science International, 52, 193–198.
Arash-Kaps, L., et al. (2019). The clinical and molecular spectrum of GM1 gangliosidosis. The Journal of Pediatrics, 215, 152–157e153.
Satoh, H., Yamato, O., Asano, T., Yamasaki, M., & Maede, Y. (2004). Increased concentration of GM1-ganglioside in cerebrospinal fluid in dogs with GM1- and GM2-gangliosidoses and its clinical application for diagnosis. Journal of Veterinary Diagnostic Investigation, 16, 223–226.
Brunetti-Pierri, N., et al. (2008). Brain proton magnetic resonance spectroscopy and neuromuscular pathology in a patient with GM1 gangliosidosis. Journal of Child Neurology, 23, 73–78.
Jeyakumar, M., et al. (2003). Central nervous system inflammation is a hallmark of pathogenesis in mouse models of GM1 and GM2 gangliosidosis. Brain, 126, 974–987.
Brunetti-Pierri, N., & Scaglia, F. (2008). GM1 gangliosidosis: Review of clinical, molecular, and therapeutic aspects. Molecular Genetics and Metabolism, 94, 391–396.
Ryckman, A. E., Brockhausen, I., & Walia, J. S. (2020). Metabolism of glycosphingolipids and their role in the pathophysiology of lysosomal storage disorders. International Journal of Molecular Sciences, 21, 6881.
Utz, J. R. J., et al. (2017). Infantile gangliosidoses: Mapping a timeline of clinical changes. Molecular Genetics and Metabolism, 121, 170–179.
Karimzadeh, P., et al. (2017). Case reports of juvenile GM1 gangliosidosisis type II caused by mutation in GLB1 gene. BMC Medical Genetics, 18, 73.
Yang, C. F., Wu, J. Y., & Tsai, F. J. (2010). Three novel beta-galactosidase gene mutations in Han Chinese patients with GM1 gangliosidosis are correlated with disease severity. Journal of Biomedical Science, 17, 79.
Wenger, D. A., Tarby, T. J., & Wharton, C. (1978). Macular cherry-red spots and myoclonus with dementia: Coexistent neuraminidase and beta-galactosidase deficiencies. Biochemical and Biophysical Research Communications, 82, 589–595.
Galjart, N. J., et al. (1988). Expression of cDNA encoding the human “protective protein” associated with lysosomal beta-galactosidase and neuraminidase: Homology to yeast proteases. Cell, 54, 755–764.
D’Azzo, A., Hoogeveen, A., Reuser, A. J., Robinson, D., & Galjaard, H. (1982). Molecular defect in combined beta-galactosidase and neuraminidase deficiency in man. Proceedings of the National Academy of Sciences of the United States of America, 79, 4535–4539.
Pierson, T. M., et al. (2012). Exome sequencing as a diagnostic tool in a case of undiagnosed juvenile-onset GM1-gangliosidosis. Neurology, 79, 123–126.
Rha, A. K., Maguire, A. S., & Martin, D. R. (2021). GM1 Gangliosidosis: Mechanisms and management. The Application of Clinical Genetics, 14, 209–233.
McCurdy, V. J., et al. (2014). Sustained normalization of neurological disease after intracranial gene therapy in a feline model. Science Translational Medicine, 6, 231ra248.
Sawada, T., et al. (2009). Intracerebral cell transplantation therapy for murine GM1 gangliosidosis. Brain Dev, 31, 717–724.
Condori, J., et al. (2016). Enzyme replacement for GM1-gangliosidosis: Uptake, lysosomal activation, and cellular disease correction using a novel beta-galactosidase:RTB lectin fusion. Molecular Genetics and Metabolism, 117, 199–209.
Front, S., et al. (2017). (5aR)-5a-C-Pentyl-4-epi-isofagomine: A powerful inhibitor of lysosomal beta-galactosidase and a remarkable chaperone for mutations associated with GM1-gangliosidosis and Morquio disease type B. European Journal of Medicinal Chemistry, 126, 160–170.
Latour, Y. L., et al. (2019). Human GLB1 knockout cerebral organoids: A model system for testing AAV9-mediated GLB1 gene therapy for reducing GM1 ganglioside storage in GM1 gangliosidosis. Molecular Genetics and Metabolism Reports, 21, 100513.
Mohamed, F. E., et al. (2020). The pharmacological chaperone N-n-butyl-deoxygalactonojirimycin enhances β-galactosidase processing and activity in fibroblasts of a patient with infantile GM1-gangliosidosis. Human Genetics, 139, 657–673.
Jeyakumar, M., et al. (1999). Delayed symptom onset and increased life expectancy in Sandhoff disease mice treated with N-butyldeoxynojirimycin. Proceedings of the National Academy of Sciences of the United States of America, 96, 6388–6393.
Norflus, F., et al. (1998). Bone marrow transplantation prolongs life span and ameliorates neurologic manifestations in Sandhoff disease mice. The Journal of Clinical Investigation, 101, 1881–1888.
Myerowitz, R., et al. (2002). Molecular pathophysiology in Tay-Sachs and Sandhoff diseases as revealed by gene expression profiling. Human Molecular Genetics, 11, 1343–1350.
Leal, A. F., et al. (2020). GM2 Gangliosidoses: Clinical features, pathophysiological aspects, and current therapies. International Journal of Molecular Sciences, 21, 6213.
Cachon-Gonzalez, M. B., Zaccariotto, E., & Cox, T. M. (2018). Genetics and therapies for GM2 Gangliosidosis. Current Gene Therapy, 18, 68–89.
Sandhoff, K., & Harzer, K. (2013). Gangliosides and gangliosidoses: Principles of molecular and metabolic pathogenesis. The Journal of Neuroscience, 33, 10195–10208.
Breiden, B., & Sandhoff, K. (2020). Mechanism of secondary ganglioside and lipid accumulation in lysosomal disease. International Journal of Molecular Sciences, 21, 2566.
Hall, P., Minnich, S., Teigen, C., & Raymond, K. (2014). Diagnosing lysosomal storage disorders: The GM2 Gangliosidoses. Current Protocols in Human Genetics, 83, 17.16.11–17.16.18.
Gort, L., de Olano, N., Macias-Vidal, J., Coll, M. A., & Spanish, G. M. W. G. (2012). GM2 gangliosidoses in Spain: Analysis of the HEXA and HEXB genes in 34 Tay-Sachs and 14 Sandhoff patients. Gene, 506, 25–30.
Beegle, J., Hendrix, K., Maciel, H., Nolta, J. A., & Anderson, J. S. (2020). Improvement of motor and behavioral activity in Sandhoff mice transplanted with human CD34+ cells transduced with a HexA/HexB expressing lentiviral vector. The Journal of Gene Medicine, 22, e3205.
Giugliani, R., et al. (2018). Neurological manifestations of lysosomal disorders and emerging therapies targeting the CNS. The Lancet Child & Adolescent Health, 2, 56–68.
Maegawa, G. H., et al. (2007). Pyrimethamine as a potential pharmacological chaperone for late-onset forms of GM2 gangliosidosis. The Journal of Biological Chemistry, 282, 9150–9161.
Bateman, K. S., Cherney, M. M., Mahuran, D. J., Tropak, M., & James, M. N. (2011). Crystal structure of beta-hexosaminidase B in complex with pyrimethamine, a potential pharmacological chaperone. Journal of Medicinal Chemistry, 54, 1421–1429.
Clarke, J. T., et al. (2011). An open-label phase I/II clinical trial of pyrimethamine for the treatment of patients affected with chronic GM2 gangliosidosis (Tay-Sachs or Sandhoff variants). Molecular Genetics and Metabolism, 102, 6–12.
Osher, E., et al. (2015). Effect of cyclic, low dose pyrimethamine treatment in patients with late onset Tay Sachs: An open label, extended pilot study. Orphanet Journal of Rare Diseases, 10, 45.
Arthur, J. R., et al. (2013). Ethylenedioxy-PIP2 oxalate reduces ganglioside storage in juvenile Sandhoff disease mice. Neurochemical Research, 38, 866–875.
Woodley, E., et al. (2019). Efficacy of a Bicistronic vector for correction of Sandhoff disease in a mouse model. Molecular Therapy—Methods & Clinical Development, 12, 47–57.
Ou, L., et al. (2020). A novel gene editing system to treat both Tay-Sachs and Sandhoff diseases. Gene Therapy, 27, 226–236.
Schiffmann, R. (2009). Fabry disease. Pharmacology & Therapeutics, 122, 65–77.
Fabry, J. (1898). Ein Beitrag zur Kenntniss der Purpura haemorrhagica nodularis (Purpura papulosa haemorrhagica Hebrae). Archiv für Dermatologie und Syphilis, 43, 187–200.
Anderson, W. (1898). A case of “Angeio-Keratoma”*. British Journal of Dermatology, 10, 113–117.
International Fabry Disease Genotype-Phenotype Database (dbFGP). Retrieved from http://www.dbfgp.org/dbFgp/fabry/FabryGP.html.
Čerkauskaitė, A., et al. (2019). Genotype-phenotype correlation in a new Fabry-disease-causing mutation. Medicina (Kaunas, Lithuania), 55, 122.
Smid, B. E., et al. (2015). Diagnostic dilemmas in Fabry disease: A case series study on GLA mutations of unknown clinical significance. Clinical Genetics, 88, 161–166.
Meikle, P. J., Hopwood, J. J., Clague, A. E., & Carey, W. F. (1999). Prevalence of lysosomal storage disorders. The Journal of the American Medical Association, 281, 249–254.
Hopkins, P. V., et al. (2015). Lysosomal storage disorder screening implementation: Findings from the first six months of full population pilot testing in Missouri. The Journal of Pediatrics, 166, 172–177.
Colon, C., et al. (2017). Newborn screening for Fabry disease in the north-west of Spain. European Journal of Pediatrics, 176, 1075–1081.
Burlina, A. B., et al. (2019). Implementation of second-tier tests in newborn screening for lysosomal disorders in north eastern Italy. International Journal of Neonatal Screening, 5, 24.
Lin, H. Y., et al. (2009). High incidence of the cardiac variant of Fabry disease revealed by newborn screening in the Taiwan Chinese population. Circulation. Cardiovascular Genetics, 2, 450–456.
Eng, C. M., Resnick-Silverman, L. A., Niehaus, D. J., Astrin, K. H., & Desnick, R. J. (1993). Nature and frequency of mutations in the alpha-galactosidase a gene that cause Fabry disease. American Journal of Human Genetics, 53, 1186–1197.
Miller, J. J., Kanack, A. J., & Dahms, N. M. (2020). Progress in the understanding and treatment of Fabry disease. Biochimica et Biophysica Acta - General Subjects, 1864, 129437.
Beck, M. (2006). In A. Mehta, M. Beck, & G. Sunder-Plassmann (Eds.), Fabry disease: Perspectives from 5 years of FOS. Oxford PharmaGenesis.
Platt, F. M., d'Azzo, A., Davidson, B. L., Neufeld, E. F., & Tifft, C. J. (2018). Lysosomal storage diseases. Nature Reviews. Disease Primers, 4, 27.
Clarke, J. T. (2007). Narrative review: Fabry disease. Annals of Internal Medicine, 146, 425–433.
Smid, B. E., et al. (2014). Uncertain diagnosis of Fabry disease: Consensus recommendation on diagnosis in adults with left ventricular hypertrophy and genetic variants of unknown significance. International Journal of Cardiology, 177, 400–408.
Biegstraaten, M., et al. (2015). Recommendations for initiation and cessation of enzyme replacement therapy in patients with Fabry disease: The European Fabry working group consensus document. Orphanet Journal of Rare Diseases, 10, 36.
Mirzaian, M., et al. (2017). Simultaneous quantitation of sphingoid bases by UPLC-ESI-MS/MS with identical (13)C-encoded internal standards. Clinica Chimica Acta, 466, 178–184.
Cairns, T., et al. (2018). Hot topics in Fabry disease. Postgraduate Medical Journal, 94, 709–713.
Simonetta, I., Tuttolomondo, A., Daidone, M., & Pinto, A. (2020). Biomarkers in Anderson-Fabry disease. International Journal of Molecular Sciences, 21, 8080.
MacDermot, K. D., Holmes, A., & Miners, A. H. (2001). Anderson-Fabry disease: Clinical manifestations and impact of disease in a cohort of 60 obligate carrier females. Journal of Medical Genetics, 38, 769–775.
Vardarli, I., Rischpler, C., Herrmann, K., & Weidemann, F. (2020). Diagnosis and screening of patients with Fabry disease. Therapeutics and Clinical Risk Management, 16, 551–558.
Eng, C. M., et al. (2001). Safety and efficacy of recombinant human alpha-galactosidase a replacement therapy in Fabry’s disease. The New England Journal of Medicine, 345, 9–16.
Lenders, M., et al. (2016). Serum-mediated inhibition of enzyme replacement therapy in Fabry disease. The Journal of the American Society of Nephrology, 27, 256–264.
Garman, R. D., Munroe, K., & Richards, S. M. (2004). Methotrexate reduces antibody responses to recombinant human alpha-galactosidase a therapy in a mouse model of Fabry disease. Clinical and Experimental Immunology, 137, 496–502.
Sato, Y., Ida, H., & Ohashi, T. (2017). Anti-BlyS antibody reduces the immune reaction against enzyme and enhances the efficacy of enzyme replacement therapy in Fabry disease model mice. Clinical Immunology, 178, 56–63.
Kok, K., et al. (2021). Fabry disease: Molecular basis, pathophysiology, diagnostics and potential therapeutic directions. Biomolecules, 11, 271.
van der Veen, S. J., Hollak, C. E. M., van Kuilenburg, A. B. P., & Langeveld, M. (2020). Developments in the treatment of Fabry disease. Journal of Inherited Metabolic Disease, 43, 908–921.
Peterschmitt, M. J., et al. (2021). Pharmacokinetics, pharmacodynamics, safety, and tolerability of Oral Venglustat in healthy volunteers. Clinical Pharmacology in Drug Development, 10, 86–98.
Guerard, N., Morand, O., & Dingemanse, J. (2017). Lucerastat, an iminosugar with potential as substrate reduction therapy for glycolipid storage disorders: Safety, tolerability, and pharmacokinetics in healthy subjects. Orphanet Journal of Rare Diseases, 12, 9.
Ashe, K. M., et al. (2015). Efficacy of enzyme and substrate reduction therapy with a novel antagonist of glucosylceramide synthase for Fabry disease. Molecular Medicine, 21, 389–399.
Ruiz de Garibay, A. P., Solinis, M. A., & Rodriguez-Gascon, A. (2013). Gene therapy for fabry disease: A review of the literature. BioDrugs, 27, 237–246.
Tomsen-Melero, J., et al. (2021). Impact of chemical composition on the nanostructure and biological activity of alpha-galactosidase-loaded nanovesicles for Fabry disease treatment. ACS Applied Materials & Interfaces, 13, 7825–7838.
Grabowski, G. A. (2008). Phenotype, diagnosis, and treatment of Gaucher’s disease. The Lancet, 372, 1263–1271.
Lieberman, R. L., et al. (2007). Structure of acid beta-glucosidase with pharmacological chaperone provides insight into Gaucher disease. Nature Chemical Biology, 3, 101–107.
Huang, W. J., Zhang, X., & Chen, W. W. (2015). Gaucher disease: A lysosomal neurodegenerative disorder. European Review for Medical and Pharmacological Sciences, 19, 1219–1226.
Stirnemann, J., et al. (2017). A review of Gaucher disease pathophysiology, clinical presentation and treatments. International Journal of Molecular Sciences, 18, 441.
Aharon-Peretz, J., Rosenbaum, H., & Gershoni-Baruch, R. (2004). Mutations in the glucocerebrosidase gene and Parkinson’s disease in Ashkenazi Jews. New England Journal of Medicine, 351, 1972–1977.
Beutler, E., Gelbart, T., & Scott, C. R. (2005). Hematologically important mutations: Gaucher disease. Blood Cells, Molecules & Diseases, 35, 355–364.
Daykin, E. C., Ryan, E., & Sidransky, E. (2021). Diagnosing neuronopathic Gaucher disease: New considerations and challenges in assigning Gaucher phenotypes. Molecular Genetics and Metabolism, 132, 49–58.
Neufeld, E. F. (1991). Lysosomal storage diseases. Annual Review of Biochemistry, 60, 257–280.
Charrow, J., Andersson, H. C., Kaplan, P., Kolodny, E. H., Mistry, P., Pastores, G., Rosenbloom, B. E., Scott, C. R., Wappner, R. S., Weinreb, N. J., & Zimran, A. (2000). The Gaucher registry: Demographics and disease characteristics of 1698 patients with Gaucher disease. Archives of Internal Medicine, 160, 2835–2843.
Boot, R. G., et al. (2004). Marked elevation of the chemokine CCL18/PARC in Gaucher disease: A novel surrogate marker for assessing therapeutic intervention. Blood, 103, 33–39.
Hollak, C. E., van Weely, S., van Oers, M. H., & Aerts, J. M. (1994). Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. Journal of Clinical Investigation, 93, 1288–1292.
Dekker, N., et al. (2011). Elevated plasma glucosylsphingosine in Gaucher disease: Relation to phenotype, storage cell markers, and therapeutic response. Blood, 118, e118–e127.
Mekinian, A., et al. (2012). Ferritinemia during type 1 Gaucher disease: Mechanisms and progression under treatment. Blood Cells, Molecules & Diseases, 49, 53–57.
Vom Dahl, S., et al. (2006). Evidence-based recommendations for monitoring bone disease and the response to enzyme replacement therapy in Gaucher patients. Current Medical Research and Opinion, 22, 1045–1064.
Sidransky, E. (2004). Gaucher disease: Complexity in a ‘simple’ disorder. Molecular Genetics and Metabolism, 83, 6–15.
Stirnemann, J., et al. (2012). The French Gaucher’s disease registry: Clinical characteristics, complications and treatment of 562 patients. Orphanet Journal of Rare Diseases, 7, 77.
Rosenbaum, H. (2014). Hemorrhagic aspects of Gaucher disease. Rambam Maimonides Medical Journal, 5, e0039.
Pastores, G. M., Wallenstein, S., Desnick, R. J., & Luckey, M. M. (1996). Bone density in type 1 Gaucher disease. Journal of Bone and Mineral Research, 11, 1801–1807.
Wenstrup, R. J., Roca-Espiau, M., Weinreb, N. J., & Bembi, B. (2002). Skeletal aspects of Gaucher disease: A review. The British Journal of Radiology, 75, A2–A12.
Mistry, P. K., et al. (2002). Pulmonary hypertension in type 1 Gaucher’s disease: Genetic and epigenetic determinants of phenotype and response to therapy. Molecular Genetics and Metabolism, 77, 91–98.
Kaplan, P., Andersson, H. C., Kacena, K. A., & Yee, J. D. (2006). The clinical and demographic characteristics of nonneuronopathic Gaucher disease in 887 children at diagnosis. Archives of Pediatrics and Adolescent Medicine, 160, 603–608.
Gupta, N., Oppenheim, I. M., Kauvar, E. F., Tayebi, N., & Sidransky, E. (2011). Type 2 Gaucher disease: Phenotypic variation and genotypic heterogeneity. Blood Cells, Molecules, and Diseases, 46, 75–84.
Mignot, C., Doummar, D., Maire, I., & De Villemeur, T. B. (2006). & French type 2 Gaucher disease study, G. type 2 Gaucher disease: 15 new cases and review of the literature. Brain Dev, 28, 39–48.
Mignot, C., et al. (2003). Perinatal-lethal Gaucher disease. American Journal of Medical Genetics. Part A, 120A, 338–344.
Roshan Lal, T., & Sidransky, E. (2017). The Spectrum of neurological manifestations associated with Gaucher disease. Diseases, 5, 10.
Gary, S. E., Ryan, E., Steward, A. M., & Sidransky, E. (2018). Recent advances in the diagnosis and management of Gaucher disease. Expert Review of Endocrinology and Metabolism, 13, 107–118.
Kraoua, I., et al. (2011). A French experience of type 3 Gaucher disease: Phenotypic diversity and neurological outcome of 10 patients. Brain Dev, 33, 131–139.
George, R., McMahon, J., Lytle, B., Clark, B., & Lichtin, A. (2001). Severe valvular and aortic arch calcification in a patient with Gaucher’s disease homozygous for the D409H mutation. Clinical Genetics, 59, 360–363.
Zimran, A. (2011). How I treat Gaucher disease. Blood, 118, 1463–1471.
Barton, N. W., et al. (1991). Replacement therapy for inherited enzyme deficiency—macrophage-targeted glucocerebrosidase for Gaucher’s disease. The New England Journal of Medicine, 324, 1464–1470.
Schiffmann, R., et al. (2008). Randomized, controlled trial of miglustat in Gaucher’s disease type 3. Annals of Neurology, 64, 514–522.
Cox, T. M., et al. (2015). Eliglustat compared with imiglucerase in patients with Gaucher’s disease type 1 stabilised on enzyme replacement therapy: A phase 3, randomised, open-label, non-inferiority trial. The Lancet, 385, 2355–2362.
Weinreb, N. J. (2017). Encore! Oral therapy for type 1 Gaucher disease. Blood, 129, 2337–2338.
Han, T. U., Sam, R., & Sidransky, E. (2020). Small molecule chaperones for the treatment of Gaucher disease and GBA1-associated Parkinson disease. Frontiers in Cell and Development Biology, 8, 271.
Wood, H. (2018). Fetal gene therapy could be feasible for neuronopathic Gaucher disease. Nature Reviews. Neurology, 14, 507.
Biffi, A., Lucchini, G., Rovelli, A., & Sessa, M. (2008). Metachromatic leukodystrophy: An overview of current and prospective treatments. Bone Marrow Transplantation, 42(Suppl 2), S2–S6.
Cesani, M., et al. (2016). Mutation update of ARSA and PSAP genes causing metachromatic leukodystrophy. Human Mutation, 37, 16–27.
Beerepoot, S., et al. (2019). Peripheral neuropathy in metachromatic leukodystrophy: Current status and future perspective. Orphanet Journal of Rare Diseases, 14, 240.
Gieselmann, V., Polten, A., Kreysing, J., & von Figura, K. (1994). Molecular genetics of metachromatic leukodystrophy. Journal of Inherited Metabolic Disease, 17, 500–509.
van Eijk, M., Ferraz, M. J., Boot, R. G., & Aerts, J. (2020). Lyso-glycosphingolipids: Presence and consequences. Essays in Biochemistry, 64, 565–578.
Von Figura, K. (2001). Metachromatic leukodystrophy. In The metabolic and molecular basis of inherited disease. McGraw-Hill.
Gieselmann, V., et al. (1998). Metachromatic leukodystrophy: Molecular genetics and an animal model. Journal of Inherited Metabolic Disease, 21, 564–574.
Kreysing, J., von Figura, K., & Gieselmann, V. (1990). Structure of the arylsulfatase a gene. European Journal of Biochemistry, 191, 627–631.
Elgun, S., et al. (2019). Phenotypic variation between siblings with metachromatic Leukodystrophy. Orphanet Journal of Rare Diseases, 14, 136.
Lugowska, A., et al. (2005). Mutations c.459+1G>a and p.P426L in the ARSA gene: Prevalence in metachromatic leukodystrophy patients from European countries. Molecular Genetics and Metabolism, 86, 353–359.
Gieselmann, V., & Krageloh-Mann, I. (2010). Metachromatic leukodystrophy—An update. Neuropediatrics, 41, 1–6.
Kehrer, C., Blumenstock, G., Gieselmann, V., Krageloh-Mann, I., & German, L. (2011). The natural course of gross motor deterioration in metachromatic leukodystrophy. Developmental Medicine and Child Neurology, 53, 850–855.
Harrington, M., et al. (2019). Insights into the natural history of metachromatic leukodystrophy from interviews with caregivers. Orphanet Journal of Rare Diseases, 14, 89.
van der Knaap, M. S., & Bugiani, M. (2017). Leukodystrophies: A proposed classification system based on pathological changes and pathogenetic mechanisms. Acta Neuropathologica, 134, 351–382.
Baumann, N., et al. (1991). Adult forms of metachromatic leukodystrophy: Clinical and biochemical approach. Developmental Neuroscience, 13, 211–215.
Hageman, A. T., et al. (1995). Clinical symptoms of adult metachromatic leukodystrophy and arylsulfatase a pseudodeficiency. Archives of Neurology, 52, 408–413.
van Rappard, D. F., et al. (2016). Gallbladder and the risk of polyps and carcinoma in metachromatic leukodystrophy. Neurology, 87, 103–111.
Wang, Y., et al. (2019). Metachromatic leukodystrophy: Characterization of two (p.Leu433Val, p.Gly449Arg) arylsulfatase a mutations. Experimental and Therapeutic Medicine, 18, 1738–1744.
Froukh, T. (2019). First record mutations in the genes ASPA and ARSA causing leukodystrophy in Jordan. BioMed Research International, 2019, 7235914.
Mahdieh, N., et al. (2021). Novel disease-causing variants in a cohort of Iranian patients with metachromatic leukodystrophy and in silico analysis of their pathogenicity. Clinical Neurology and Neurosurgery, 201, 106448.
Ashrafi, M. R., et al. (2020). An update on clinical, pathological, diagnostic, and therapeutic perspectives of childhood leukodystrophies. Expert Review of Neurotherapeutics, 20, 65–84.
Pajarola, S., et al. (2019). Measurement of recombinant human arylsulfatase a and leukocyte sulfatase activities by analytical isotachophoresis. Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences, 1124, 109–113.
Lee-Vaupel, M., & Conzelmann, E. (1987). A simple chromogenic assay for arylsulfatase A. Clinica Chimica Acta: International Journal of Clinical Chemistry, 164, 171–180.
Hong, X., et al. (2020). Leukocyte and dried blood spot arylsulfatase a assay by tandem mass spectrometry. Analytical Chemistry, 92, 6341–6348.
Mirzaian, M., Kramer, G., & Poorthuis, B. J. (2015). Quantification of sulfatides and lysosulfatides in tissues and body fluids by liquid chromatography-tandem mass spectrometry. Journal of Lipid Research, 56, 936–943.
Spacil, Z., et al. (2016). Sulfatide analysis by mass spectrometry for screening of metachromatic leukodystrophy in dried blood and urine samples. Clinical Chemistry, 62, 279–286.
Faerber, E. N., Melvin, J., & Smergel, E. M. (1999). MRI appearances of metachromatic leukodystrophy. Pediatric Radiology, 29, 669–672.
Nandhagopal, R., & Krishnamoorthy, S. G. (2006). Neurological picture. Tigroid and leopard skin pattern of dysmyelination in metachromatic leucodystrophy. Journal of Neurology, Neurosurgery, and Psychiatry, 77, 344.
i Dali, C., et al. (2010). Brain N-acetylaspartate levels correlate with motor function in metachromatic leukodystrophy. Neurology, 75, 1896–1903.
Shaimardanova, A. A., et al. (2020). Metachromatic leukodystrophy: Diagnosis, modeling, and treatment approaches. Frontiers in Medicine, 7, 576221.
Sadovnick, A. D., et al. (1993). The differential diagnosis of adult onset metachromatic leukodystrophy and early onset familial Alzheimer disease in an Alzheimer clinic population. The Canadian Journal of Neurological Sciences, 20, 312–318.
Mahon-Haft, H., Stone, R. K., Johnson, R., & Shah, S. (1981). Biochemical abnormalities of metachromatic leukodystrophy in an adult psychiatric population. The American Journal of Psychiatry, 138, 1372–1374.
Patil, S. A., & Maegawa, G. H. (2013). Developing therapeutic approaches for metachromatic leukodystrophy. Drug Design, Development and Therapy, 7, 729–745.
Cosma, M. P., et al. (2003). The multiple sulfatase deficiency gene encodes an essential and limiting factor for the activity of sulfatases. Cell, 113, 445–456.
Wolf, N. I., et al. (2020). Metachromatic leukodystrophy and transplantation: Remyelination, no cross-correction. Annals of Clinical Translational Neurology, 7, 169–180.
Sessa, M., et al. (2016). Lentiviral haemopoietic stem-cell gene therapy in early-onset metachromatic leukodystrophy: An ad-hoc analysis of a non-randomised, open-label, phase 1/2 trial. The Lancet, 388, 476–487.
Biffi, A., et al. (2013). Lentiviral hematopoietic stem cell gene therapy benefits metachromatic leukodystrophy. Science, 341, 1233158.
Berger, J., Moser, H. W., & Forss-Petter, S. (2001). Leukodystrophies: Recent developments in genetics, molecular biology, pathogenesis and treatment. Current Opinion in Neurology, 14, 305–312.
Martin, H. R., et al. (2013). Neurodevelopmental outcomes of umbilical cord blood transplantation in metachromatic leukodystrophy. Biology of Blood and Marrow Transplantation, 19, 616–624.
Matzner, U., & Gieselmann, V. (2005). Gene therapy of metachromatic leukodystrophy. Expert Opinion on Biological Therapy, 5, 55–65.
Rosenberg, J. B., Kaminsky, S. M., Aubourg, P., Crystal, R. G., & Sondhi, D. (2016). Gene therapy for metachromatic leukodystrophy. Journal of Neuroscience Research, 94, 1169–1179.
Kohler, W. (2010). Leukodystrophies with late disease onset: An update. Current Opinion in Neurology, 23, 234–241.
Penati, R., Fumagalli, F., Calbi, V., Bernardo, M. E., & Aiuti, A. (2017). Gene therapy for lysosomal storage disorders: Recent advances for metachromatic leukodystrophy and mucopolysaccaridosis I. Journal of Inherited Metabolic Disease, 40, 543–554.
Batzios, S. P., & Zafeiriou, D. I. (2012). Developing treatment options for metachromatic leukodystrophy. Molecular Genetics and Metabolism, 105, 56–63.
Compston, A. (2013). A new familial infantile form of diffuse brain-sclerosis. Brain, 136, 2649–2651.
Krieg, S. I., et al. (2020). Natural history of Krabbe disease—A nationwide study in Germany using clinical and MRI data. Orphanet Journal of Rare Diseases, 15, 243.
Zhong, J., et al. (2020). Novel GALC mutations cause adult-onset Krabbe disease with myelopathy in two Chinese families: Case reports and literature review. Frontiers in Neurology, 11, 830.
Agency, E. M. Public summary of opinion on orphan designation. (2011).
Pannuzzo, G., Graziano, A. C. E., Avola, R., Drago, F., & Cardile, V. (2019). Screening for Krabbe disease: The first 2 years’ experience. Acta Neurologica Scandinavica, 140, 359–365.
Spiegel, R., et al. (2005). A mutation in the saposin a coding region of the prosaposin gene in an infant presenting as Krabbe disease: First report of saposin a deficiency in humans. Molecular Genetics and Metabolism, 84, 160–166.
Kose, M., et al. (2019). The second case of Saposin a deficiency and altered autophagy. JIMD Reports, 44, 43–54.
Meng, X., et al. (2020). A new compound heterozygous mutation in adult-onset Krabbe disease. The International Journal of Neuroscience, 130, 1267–1271.
Szymańska, K., et al. (2012). Diagnostic difficulties in Krabbe disease: A report of two cases and review of literature. Folia Neuropathologica, 50, 346–356.
Komatsuzaki, S., et al. (2019). Clinical characteristics of 248 patients with Krabbe disease: Quantitative natural history modeling based on published cases. Genetics in Medicine, 21, 2208–2215.
Duffner, P. K., et al. (2009). Newborn screening for Krabbe disease: The New York state model. Pediatric Neurology, 40, 245–252.; discussion 253-245.
Cousyn, L., et al. (2019). Brain MRI features and scoring of leukodystrophy in adult-onset Krabbe disease. Neurology, 93, e647–e652.
Herbst, Z., et al. (2020). Achieving congruence among reference laboratories for absolute abundance measurement of analytes for rare diseases: Psychosine for diagnosis and prognosis of Krabbe disease. International Journal of Neonatal Screening, 6, 29.
Graziano, A. C., & Cardile, V. (2015). History, genetic, and recent advances on Krabbe disease. Gene, 555, 2–13.
Kwon, J. M., et al. (2018). Consensus guidelines for newborn screening, diagnosis and treatment of infantile Krabbe disease. Orphanet Journal of Rare Diseases, 13, 30.
Ehmann, P., & Lantos, J. D. (2019). Ethical issues with testing and treatment for Krabbe disease. Developmental Medicine and Child Neurology, 61, 1358–1361.
Patiño-Escobar, B., Solano, M. H., Zarabanda, L., Casas, C. P., & Castro, C. (2019). Niemann-pick disease: An approach for diagnosis in adulthood. Cureus, 11, e4767.
Schuchman, E. H., & Wasserstein, M. P. (2015). Types A and B Niemann-Pick disease. Best Practice & Research. Clinical Endocrinology & Metabolism, 29, 237–247.
Crocker, A. C., & Mays, V. B. (1961). Sphingomyelin synthesis in Niemann-Pick disease. The American Journal of Clinical Nutrition, 9, 63–67.
Jenkins, R. W., Canals, D., & Hannun, Y. A. (2009). Roles and regulation of secretory and lysosomal acid sphingomyelinase. Cellular Signalling, 21, 836–846.
Baskfield, A., et al. (2019). An induced pluripotent stem cell line (TRNDi009-C) from a Niemann-Pick disease type a patient carrying a heterozygous p.L302P (c.905 T>C) mutation in the SMPD1 gene. Stem Cell Research, 38, 101461.
Wasserstein, M. P., & Schuchman, E. H. (1993). In M. P. Adam, H. H. Ardinger, R. A. Pagon, et al. (Eds.), GeneReviews® [Internet]. University of Washington, Seattle.
Irun, P., et al. (2013). Identification of seven novel SMPD1 mutations causing Niemann-Pick disease types a and B. Clinical Genetics, 84, 356–361.
Liu, Y., et al. (2019). The effects of liver transplantation in children with Niemann-Pick disease type B. Liver Transplantation, 25, 1233–1240.
Schuchman, E. H., & Desnick, R. J. (2017). Types a and B Niemann-Pick disease. Molecular Genetics and Metabolism, 120, 27–33.
Samaranch, L., et al. (2019). Adeno-associated viral vector serotype 9-based gene therapy for Niemann-Pick disease type A. Science Translational Medicine, 11, 1–15.
Farber, S. (1952). A lipid metabolic disorder: Disseminated lipogranulomatosis; a syndrome with similarity to, and important difference from, Niemann-Pick and hand-Schüller-Christian disease. American Journal of Diseases of Children, 84, 499–500.
Zhou, J., et al. (2012). Spinal muscular atrophy associated with progressive myoclonic epilepsy is caused by mutations in ASAH1. American Journal of Human Genetics, 91, 5–14.
Li, C. M., et al. (1999). The human acid ceramidase gene (ASAH): Structure, chromosomal location, mutation analysis, and expression. Genomics, 62, 223–231.
Yu, F. P. S., Amintas, S., Levade, T., & Medin, J. A. (2018). Acid ceramidase deficiency: Farber disease and SMA-PME. Orphanet Journal of Rare Diseases, 13, 121.
Dulaney, J. T., Milunsky, A., Sidbury, J. B., Hobolth, N., & Moser, H. W. (1976). Diagnosis of lipogranulomatosis (Farber disease) by use of cultured fibroblasts. The Journal of Pediatrics, 89, 59–61.
Ben-Yoseph, Y., Gagné, R., Parvathy, M. R., Mitchell, D. A., & Momoi, T. (1989). Leukocyte and plasma N-laurylsphingosine deacylase (ceramidase) in Farber disease. Clinical Genetics, 36, 38–42.
Fensom, A. H., et al. (1979). Prenatal diagnosis of Farber’s disease. Lancet (London, England), 2, 990–992.
Chatelut, M., et al. (1996). A simple method for screening for Farber disease on cultured skin fibroblasts. Clinica Chimica Acta; International Journal of Clinical Chemistry, 245, 61–71.
Moser, H. W., Prensky, A. L., Wolfe, H. J., & Rosman, N. P. (1969). Farber’s lipogranulomatosis. Report of a case and demonstration of an excess of free ceramide and ganglioside. The American Journal of Medicine, 47, 869–890.
Iwamori, M., & Moser, H. W. (1975). Above-normal urinary excretion of urinary ceramides in Farber’s disease, and characterization of their components by high-performance liquid chromatography. Clinical Chemistry, 21, 725–729.
Dworski, S., et al. (2017). Acid ceramidase deficiency is characterized by a unique plasma cytokine and ceramide profile that is altered by therapy. Biochimica et Biophysica Acta: Molecular Basis of Disease, 1863, 386–394.
Cozma, C., et al. (2017). C26-ceramide as highly sensitive biomarker for the diagnosis of Farber disease. Scientific Reports, 7, 6149.
Schmoeckel, C., & Hohlfed, M. (1979). A specific ultrastructural marker for disseminated lipogranulomatosis (Faber). Archives of Dermatological Research, 266, 187–196.
Zappatini-Tommasi, L., Dumontel, C., Guibaud, P., & Girod, C. (1992). Farber disease: An ultrastructural study. Report of a case and review of the literature. Virchows Archiv A Pathological Anatomy and Histopathology, 420, 281–290.
Zarbin, M. A., Green, W. R., Moser, H. W., & Morton, S. J. (1985). Farber’s disease. Light and electron microscopic study of the eye. Archives of Ophthalmology, 103, 73–80.
Alayoubi, A. M., et al. (2013). Systemic ceramide accumulation leads to severe and varied pathological consequences. EMBO Molecular Medicine, 5, 827–842.
Fusch, C., et al. (1989). A case of combined Farber and Sandhoff disease. European Journal of Pediatrics, 148, 558–562.
Harzer, K., et al. (1989). Sphingolipid activator protein deficiency in a 16-week-old atypical Gaucher disease patient and his fetal sibling: Biochemical signs of combined sphingolipidoses. European Journal of Pediatrics, 149, 31–39.
Hulková, H., et al. (2001). A novel mutation in the coding region of the prosaposin gene leads to a complete deficiency of prosaposin and saposins, and is associated with a complex sphingolipidosis dominated by lactosylceramide accumulation. Human Molecular Genetics, 10, 927–940.
Kostik, M. M., et al. (2013). Farber lipogranulomatosis with predominant joint involvement mimicking juvenile idiopathic arthritis. Journal of Inherited Metabolic Disease, 36, 1079–1080.
Souillet, G., Guiband, P., Fensom, A., Maire, I., & Zabot, M. (1989). Outcome of displacement bone marrow transplantation in Farber’s disease: A report of a case. In Correction of certain genetic diseases by transplantation (pp. 137–141). COGENT.
Ehlert, K., et al. (2019). Allogeneic hematopoietic cell transplantation in Farber disease. Journal of Inherited Metabolic Disease, 42, 286–294.
Weinreb, N. J., et al. (2002). Effectiveness of enzyme replacement therapy in 1028 patients with type 1 Gaucher disease after 2 to 5 years of treatment: A report from the Gaucher registry. The American Journal of Medicine, 113, 112–119.
He, X., et al. (2017). Enzyme replacement therapy for Farber disease: Proof-of-concept studies in cells and mice. BBA Clinical, 7, 85–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive licence to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Zhou, H. et al. (2022). Rare Diseases in Glycosphingolipid Metabolism. In: Jiang, XC. (eds) Sphingolipid Metabolism and Metabolic Disease. Advances in Experimental Medicine and Biology, vol 1372. Springer, Singapore. https://doi.org/10.1007/978-981-19-0394-6_13
Download citation
DOI: https://doi.org/10.1007/978-981-19-0394-6_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-0393-9
Online ISBN: 978-981-19-0394-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)