Abstract
The COVID-19 pandemic has caused large regions to be locked down for extended periods, severely impacting global economies and straining healthcare systems. Such pandemics require swift and appropriate responses to slow the rate of infections and reduce stress on healthcare systems. Hence, there is an urgent need to analyse government responses to combat future epidemics more efficiently. In this project, we study non-pharmaceutical interventions (NPIs) in particular: we adapt Imperial College’s COVID-19 model (Flaxman et al. in Report 13: estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries (2020), [1]; Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe (2020), [2]), by challenging their assumption that the effectiveness of NPIs are shared across all 14 European countries. We introduce two new semi-mechanistic Bayesian hierarchical models to investigate this problem from different perspectives. While this further elevates model complexity, we can now compare NPIs’ effectiveness across countries. Additionally, we have fine-tuned intervention input quality by introducing more interventions and modifying the model to account for interventions only affecting a fraction of a country. Based on the analysis of government responses in specific countries, we conclude that governments should respond proactively instead of reactively to emerging pandemics and implement strict restrictions especially during the early stages. This is so that infections start slowing down, and NPIs will not need to be implemented for extended times.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
3.1 Introduction
-
A.
COVID-19
On 31 December 2019, a cluster of pneumonia cases in Wuhan, China, marked the beginning of the COVID-19 pandemic. As of 30 November 2020, there have been 63,087,137 infections, with over 1,465,368 deaths reported worldwide [3]. Several European countries, in particular, experienced large epidemics in the past few months, with daily cases increasing significantly day by day. The situation in these European countries has highlighted the severity of the COVID-19 pandemic and its impact on national health systems, the country’s economy and the daily lives of its people.
The last time the world experienced a pandemic of comparable scale was the 1918 H1N1 influenza pandemic. With the help of multiple NPIs, many countries eventually managed to keep the virus under control. Measures adopted included closing schools, churches, bars and other social venues. Cities which implemented NPIs early in the epidemic were largely successful in reducing infections and mortality rates. However, an increase in cases was also observed after measures were lifted, indicating transmission resurfaced. While understanding of infectious diseases and their prevention has changed since 1918, most countries across the globe face a similar challenge today with COVID-19.
-
B.
Non-Pharmaceutical Interventions
In response, multiple countries have implemented, or are implementing various NPIs to flatten the curve, maintain their healthcare systems and treat as many as possible [4]. These NPIs follow the fundamental strategy of suppressing this infectious disease, with the main aim of reducing the reproduction number (average number of secondary cases each case generates, or rate of transmission) \({R}_{t}\) to below 1, hence reducing transmission rates and case numbers to low levels. This reduces stress on the nation’s healthcare systems, resulting in lower mortality rates.
However, there remain limitations to estimating reproduction numbers for SARS-CoV-2 based on case data. Due to high proportion of undetected and asymptomatic cases, real-world infection numbers are largely unreliable. Additionally, regular changes in testing policies produce huge spikes in daily cases and, at times, negative reported cases. Hence, we studied an alternative way to estimate the course of the epidemic—using observed deaths to model infections [5, 6]. Imperial College’s model does so, while accounting for NPIs implemented, resulting in a time-varying transmission rate. This is much more realistic than the constant transmission rate most models assume.
In this project, we adapt Imperial College’s model [1, 2] to allow comparison of NPIs’ effectiveness across countries. We introduce two new semi-mechanistic Bayesian hierarchical models to investigate this problem from different perspectives. Additionally, we have fine-tuned intervention input quality by introducing more interventions and modifying the model to account for interventions only affecting a fraction of a country.
-
C.
Motivation
The main aim of our study is to gain more insights into individual countries, where the original model [1, 2] did not inform us about individual intervention effectiveness for each country. We would like to compare multiple countries and conclude which interventions were effective in which countries—and for what reasons, as well as comparing the overall effectiveness of all interventions among different countries. This would give more insight into how to better manage future pandemics, or how to improve management of COVID-19 for the near future before vaccines become widely available.
(Our analysis focuses on modelling the infection and death rate. We do not study the economic impact of the NPIs.)
3.2 Imperial College’s Original Model
The summary of Imperial College’s model is presented in the form of a flow chart, as shown in Fig. 3.1. In the original model, Bayesian inference is used to fit modelled deaths to observed deaths of every country. This is informed by several prior distributions, “Symptoms to Death Distribution” and “Infection to Symptoms Distribution”, both of which accounts for the time lag between infection and death, as well as “Infection Fatality Ratio”. The daily infections are informed by the time-varying reproduction number \({R}_{t,m}\) and the Serial Interval Distribution. The model calculates backwards from observed deaths to modelled deaths, which is then used to calculate modelled infections and estimate \({R}_{t,m}\). In Imperial College’s model, \({R}_{t,m}\) is assumed to obey Eq. (3.1).
The effectiveness of the \(k{\text{th}}\) NPI, \(\alpha_{k}\), is then fit to best follow the predicted real-world \(R_{t,m}\).
-
A.
Limitations
As Imperial College published their report in March 2020, there was little real-world infection and fatality data available. As such, they decided to treat all countries as a single data set, assuming \({\alpha }_{k}\) is similar across all counties. While this decreases idiosyncrasy and variance, several months later, the assumption that countries have similar NPI effectiveness is no longer true, with countries such as Belgium having much larger death rates than their European counterparts Norway.
3.3 Methodology
Our model was written with the probabilistic programming language Stan [7], and ran with Stan’s Hamiltonian Monte Carlo sampler, on top of R programming language. Both models ran with six chains and 600 iterations, 300 of which is for warm-up. JavaScript was used to extract intervention data, while Python was used to process intervention data to input into the models.Footnote 1
-
A.
Country and Data set
We challenge Imperial College’s main assumption by introducing two models, A and B, which treat each of the 14 European countries as distinct data sets, different from the original model’s unique pooling of information from multiple countries at once.
With more real-world data, we need not worry about increased idiosyncrasy and variance.
The added advantage is increased flexibility. Due to Imperial College’s key assumption, countries had to be carefully chosen to have similar circumstances, resulting in Imperial College choosing all 14 countries from Europe. However, our models are unconstrained by this and can model any country with enough reported deaths.
-
B.
Model A
Model A assumes NPI’s effectiveness varies with country and considers the effectiveness of the seven NPIs for each country, denoted by variable \({\alpha }_{k,m}\), representing the effectiveness of intervention \(k\) in country \(m\). The reproduction number for country \(m\) on day t is given in Eq. (3.2), where \({I}_{k,m,t}\) represents active interventions on day \(t\) for each country (Fig. 3.2).
However, if a country implements multiple interventions in the same time period, they would be statistically indistinguishable from one another, increasing the variance of \(\alpha\) of those interventions. For example, Austria and France implemented both social distancing and self-isolation from 16 March, which thus would be indistinguishable from one another. Additionally, with more variables to fit, more epochs are required for model convergence to occur.
-
C.
Model B
Model A has multiple limitations involving increased variance. Hence, we counter these limitations with model B, which considers the overall impact of all seven NPIs for each country, denoted by variable \({\alpha }_{m}\), representing the overall effectiveness of all interventions in country \(m\). The reproduction number is given in Eq. (3.3)\(.\) This allows us to directly compare two countries, even if they execute entirely different interventions, while controlling variance (Fig. 3.3).
However, Model B assumes all interventions of a country have similar effectiveness, which would increase variance of \({\alpha }_{m}\) and decrease convergence rate. Additionally, from the results of this model, one would be unable to conclude the effectiveness of individual interventions of a country and cannot compare between different interventions.
-
D.
Interventions
Intervention data was taken until 2 December 2020. During this period, the countries have implemented more NPIs, including “Mask Wearing” and “Border Closure”. We have updated the list of interventions to include them, while removing “First Intervention”, which would have little effect in the long run. The comparison between the interventions considered in the original and updated model is shown in Fig. 3.4.
In the original model, all countries are treated as a single data set, thus there is multiple “First Intervention” for the model to fit its effectiveness. However, as both models A and B treat each country as distinct data sets, “First Intervention” only appears once in each data set, resulting in high variance of α of “First Intervention”.
The original model assumed interventions affected the entire country and would never end once started. As many European countries only implemented interventions in highly affected regions of the country, we have collected intervention data down to individual states and towns. A Python program was used to process such data, producing a sequence of numbers between 0 and 1 (inclusive) for every intervention in every country, each representing how active a country’s intervention is on a given date (\({I}_{k,m,t}\)). 0 represents an inactive intervention, while 0.5 and 1 represent an intervention affecting half the population and the whole country, respectively. This allows interventions fed into the model to better depict the real world.
-
E.
Serial Interval
Serial interval models the time between successive infections in the same chain of transmission. Serial interval data from Imperial College’s model is taken from multiple studies [8, 9] based on real-world contact tracing data. However, to extend it to longer durations, we perform gamma regression, getting our new serial interval to be \({\text{Gamma}}\left( {k = 1.8365,{\uptheta } = 0.4071} \right)\), quantised to each day \(t\) with: \(g_{t} = \int_{\tau = t - 0.5}^{t + 0.5} {\frac{{\tau^{k - 1} e^{ - \tau /\theta } }}{{\Gamma \left( k \right)\theta^{k} }}{\text{d}}\tau }\). The updated serial interval plot is shown in Fig. 3.5.
3.4 Results
-
A.
Norway
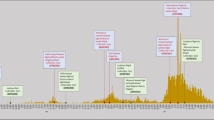
From Figs. 3.6 and 3.7, Norway was observed to have the largest per cent reduction in \({R}_{t}\) for majority of its interventions and the lowest final \({R}_{t}\). With the help of European news articles, we analyse the situation in Norway to understand why its interventions were significantly more effective than the other European countries.
Compared to other countries such as Sweden, Norway has done an impressive job of strictly enforcing interventions when the virus first emerged in the country. On 12 March, when the reproduction number in Norway was at 2.5, the Norwegian Government immediately imposed the strictest emergency measures at that time—all schools, bars and parlours were closed and those entering the country were put in a 2-week quarantine. This was a key step in combatting the virus, as Norway was able to prevent large-scale community transmission at heavily populated areas. Norway’s quick and effective response to the growing pandemic allowed its reproduction number to drop from 2.5 on 12 March to 0.5 by early April.
During the resurgence period, Norway was also quick to identify the more affected regions, implementing a lockdown and enforcing mask wearing in Oslo. While less-affected regions were still able to keep up the country’s economy, the lockdown in affected regions again effectively reduced transmission of the virus. As its neighbours were hit hard by the second wave of the pandemic, Norway kept its borders closed, keeping infection numbers low.
-
B.
Spain
We also analyse the interventions in Spain, particularly “Border Closure” measures, which was observed to be more effective than the other interventions in Spain and result in the largest per cent reduction in \({R}_{t}\) among all 14 countries (as observed from Fig. 3.8).
COVID-19 first hit Europe in Italy, one of Spain’s neighbouring countries. The Spanish government responded quickly, being the first European country to start closing its borders to Italy on 10 March, heavily reducing the number of imported cases. When it spread to other parts of Europe, Spain imposed travel restrictions on all non-residents from 16 March.
Unlike other countries, Spain kept its borders closed until infection numbers were brought down, and the virus was kept under control. This was certainly more effective than the 14-day quarantine implemented in some other countries as they eased border restrictions.
During the resurgence period, with improved testing policies, Spain was able to keep its borders open while requesting all travellers to have a negative COVID-19 test and 14-day quarantine to enter the country. As infection rates increase towards end October, Spain was also one of the few countries to implement border closures again.
These border closures were essential in ensuring no carriers of the virus entered the country, assisting the government in contact tracing efforts and for the government to be able to focus on reducing community transmission, bringing the reproduction number down significantly over time. The government responded quickly and kept borders closed for an appropriate amount of time, hence resulting in a significantly higher per cent reduction in \({R}_{t}\) as compared to other interventions.
-
C.
Belgium
From Fig. 3.6, Belgium was observed to have one of the lowest per cent reductions in \({R}_{t}\) for majority of its interventions and the highest final \({R}_{t}\) value. Back in April, Belgium was also already observed to have one of the highest mortality rates in the world. We study the possible reasons that led Belgium to become one of Europe’s most hardly hit countries by the coronavirus.
First, Belgium is one of the smallest yet most densely populated countries in Europe. This results in a higher initial reproduction number, which was estimated to be at 3.4 before strict measures were implemented in Belgium. It also puts a strain on “Social Distancing” measures, accounting for a considerably low per cent reduction in \({R}_{t}\) (as observed in Fig. 3.9).
Second, Belgium’s location in Europe also makes it more vulnerable to imported cases. At the heart of Europe, Belgium is well connected to neighbouring countries, and Europeans are able to travel in and out of Belgium by train or car. Since “Border Closure” measures were focused more on international flights and entry-checks which were more concentrated in airports, Belgium was unable to account for several imported cases at other entry-points of the country early on during the pandemic. Hence, despite the strict travel flight restrictions implemented in Belgium, “Border Closure” measures were ineffective in reducing \({R}_{t}\) (as observed in Fig. 3.9).
Third, Belgium’s multi-layered government applied a regional approach to COVID-19 measures, throwing citizens into confusion. As some regions imposed stricter restrictions compared to neighbouring regions, it sparked outrage in its citizens, severely affecting the government’s efforts in enforcing the NPIs implemented. Anti-coronavirus protest gatherings also resulted in more congested areas for large-scale community transmission, further increasing the reproduction number in Belgium.
-
D.
Intervention-specific
Our results from Model A for all 14 countries imply that major NPIs such as “School Closure”, “Lockdown” and “Border Closure” substantially reduced reproduction numbers.
-
E.
Model-specific
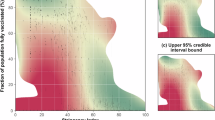
3.5 Model A
As different interventions have wildly different \({\alpha }_{k,m}\) compared to others, this model allows us to gain additional insights into the effectiveness of different interventions by each country. For example, in the Netherlands, School Closure has an \({\alpha }_{k,m}\) of around 90%, which is much higher than the other interventions in the Netherlands, which are mostly < 25%.
3.6 Model B
Certain countries have extremely small error bars in \({\alpha }_{m}\) while others have error bars which stretch close to the full range, meaning Model B has a tendency of “hit and miss”. Notably, if all interventions have similar effectiveness in Model A, the \({\alpha }_{m}\) of Model B would have an extremely low variance. However, the same is not true for its inverse (Fig. 3.10).
3.7 Future Studies
3.7.1 Unresolved Limitations
First, the model assumes \({R}_{t,m}\) is constant throughout the country. There tends to be higher urban density in cities than rural areas, thus this is not true. Second, the model assumes \({R}_{t,m}\) varies only with a change of interventions implemented. However, movement of people throughout the country would change urban densities of different regions and consequently \({R}_{t,m}\). While this can be controlled to some extent by interventions such as lockdowns and border closures, it still varies significantly. Third, the model assumes α is constant throughout time. For example, people might comply to lockdown rules initially, but when it is extended, some may get restless and protest, defeating the purpose of the lockdown. Additionally, if a second lockdown order is issued, our model will assume both lockdowns have the same α, which is not always the case. Fourth, prior distributions such as Serial Interval Distribution, Infection-to-onset Distribution and Onset-to-death Distribution vary throughout country and time, reducing accuracy. Fifth, as the model relies on observed deaths, countries with high cases yet few deaths like Singapore [10] cannot be modelled as it does not give the model sufficient information to predict cases.
3.7.2 Impacts on Results
First, pre-emptive interventions are penalised. If an intervention is implemented before the outbreak occurs, while it might have reduced \({R}_{t,m}\) significantly and lowered numbers in the outbreak, the model would register the intervention as increasing \({R}_{t,m}\) and thus have low-to-negative α. Second, if a country does not update interventions for an extended duration, the model is forced to believe that \({R}_{t,m}\) remains constant throughout. However, due to all three limitations, it is very likely a second outbreak will occur, as the governments have greater difficulty in enforcing restrictions. This is most obviously seen in Model A’s Sweden data, where the model believes Rt,m ≤ 1 even though the cases are on the rise.
3.7.3 Possible Improvements
-
(a)
For limitations 1 and 2, a possible solution is to take mobility data and split countries into multiple sub-regions of similar urban density, using mobility data to simulate people movement. Another possible study is to analyse mobility data within countries to determine the effectiveness of curfews, lockdowns, and self-isolation in different countries density, using mobility data to simulate people movement, allowing for a more in-depth analysis of changes in \({R}_{t,m}\).
3.8 Conclusion
By modifying Imperial College’s COVID-19 model, through the addition of the semi-mechanistic Bayesian hierarchical models, we present novel perspectives in the study of COVID-19 infection rates. Our model gives a clearer overview of the efficacies of NPIs based off the 14 European countries studied and provides insights into the ideal approaches governments should adopt to combat future pandemics.
After analysing selected European governments’ responses, we conclude that major NPIs like “School Closure”, “Lockdown” and “Border Closure” substantially reduced reproduction numbers. “Border closure” has also proven to be more effective than the “14-day quarantine”, possibly because it enables governments to focus on minimising community transmission. Most importantly, governments should also respond proactively instead of reactively to emerging pandemics and implement strict restrictions especially during the early stages.
Notes
- 1.
Infection, fatality and intervention data used can be found here: https://github.com/EthanKuai/Investigating-the-Effectiveness-of-NPIs-on-COVID19/blob/main/Sources.md.
References
Flaxman, S., et al. (2020). Report 13: Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-03-30-COVID19-Report-13.pdf, https://doi.org/10.25561/77731
Flaxman, S., et al. (2020). Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. https://www.nature.com/articles/s41586-020-2405-7
Worldometer. https://www.worldometers.info/.
Ferguson, N. M., et al. (2020). Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf , https://doi.org/10.25561/77482
Fraser, C. (2007). Estimating individual and household reproduction numbers in an emerging epidemic. https://pubmed.ncbi.nlm.nih.gov/17712406/, https://doi.org/10.1371/journal.pone.0000758
Jombart, T., et al. (2020). Inferring the number of COVID-19 cases from recently reported deaths. https://doi.org/10.1101/2020.03.10.20033761v1
Stan Development Team (2019). Stan modeling language users guide and reference manual, version 2.25. https://mc-stan.org/
Ferguson, N. M., et al. (2009). Household transmission of 2009 pandemic influenza a (H1N1) virus in the united states. https://doi.org/10.1056/NEJMoa0905498
Hens, N., et al. (2020). Estimating the generation interval for coronavirus disease (COVID-19) based on symptom onset data. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7201952/, https://doi.org/10.2807/1560-7917.ES.2020.25.17.2000257
https://www.reuters.com/article/health-coronavirus-singapore-explainer-idUSKBN2680TF
Jordan, M. I. (1998). Learning in graphical models. https://doi.org/10.1007/978-94-011-5014-9#about
Unwin, H. J. T., et al. (2020). State-level tracking of COVID-19 in the united states. https://www.nature.com/articles/s41467-020-19652-6
Vollmer, M. A. C., et al. (2020). Report 20—Using mobility to estimate the transmission intensity of COVID-19 in italy: A subnational analysis with future scenarios. https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/COVID-19/report-20-italy/
Mellan, T. A., et al. (2020). Report 21—Estimating COVID-19 cases and reproduction number in brazil. https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/COVID-19/report-21-brazil/
Walker, P. G., et al. (2020). Report 12: The global impact of COVID-19 and strategies for mitigation and suppresion. https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-03-26-COVID19-Report-12.pdf, https://doi.org/10.25561/77735
Lourenco, J., et al. (2020). Fundamental principles of epidemic spread highlight the immediate need for large-scale serological surveys to assess the stage of the sars-cov-2 epidemic. https://doi.org/10.1101/2020.03.24.20042291v1.full.pdf
Verity, R., et al. (2020). Estimates of the severity of COVID-19 disease. /https://doi.org/10.1101/2020.03.09.20033357v1.full.pdf
Bellman, R., & Harris, T. E. (1952). On age-dependent binary branching processes. https://www.jstor.org/stable/1969779?seq=1, https://doi.org/10.2307/1969779
Bellman, R., & Harris, T. E. (1948). On the theory of age-dependent stochastic branching processes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1079176/, https://doi.org/10.1073/pnas.34.12.601
Acknowledgements
The authors would like to gratefully acknowledge Dr. Chieu Hai Leong, Mr. Wee Liang Chi and Dr. Chai Kian Ming Adam from DSO National Laboratories INFO Division, for their support and guidance throughout this project. The authors would also like to thank NUS High School teacher mentors, Ms. Ye Xiajuan and Dr. Chiam Sher-Yi, for their encouragement and support during the entirety of this project. Additionally, the authors would like to acknowledge “Learning in graphical models” [11] which was referenced in much of the literature review on Bayesian modelling.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Angelina, W.Y.L., Ethan, K.E.K., Leong, C.H., Chi, W.L., Adam, C.K.M. (2022). Investigating the Effectiveness of Non-pharmaceutical Interventions on COVID-19. In: Guo, H., Ren, H., Wang, V., Chekole, E.G., Lakshmanan, U. (eds) IRC-SET 2021. Springer, Singapore. https://doi.org/10.1007/978-981-16-9869-9_3
Download citation
DOI: https://doi.org/10.1007/978-981-16-9869-9_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-9868-2
Online ISBN: 978-981-16-9869-9
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)