Abstract
The ovary is an important reproductive organ in the female pelvic cavity. The ovary is small while the ovarian histoembryology, anatomy, and endocrine function are extremely complex. The type, morphology, and nature of the ovarian mass are various. The traditional diagnostic method of ovarian masses is pelvic bimanual examination. The examiners evaluate the ovarian size, shape, and texture by hand, which is difficult to detect early masses. When the masses can be palpable by bimanual examination, most patients are already in the middle and late stage of the tumor. In recent years, with the rapid development of imaging technology, CT and MRI can clearly show the mass less than 5 mm, lymph node metastasis, and ascites. However, due to the high price, it is limited to screen early ovarian masses. The serum markers for the diagnosis of ovarian cancer (CA125, AFP) are one of the screening tools for ovarian cancer, while the screening sensitivity needs to be improved.
This chapter was translated by Linlin Ma, Department of Obstetrics and Gynecology, Beijing Hospital, National Center of Gerontology, Beijing, China
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
5.1 Ultrasonic Diagnosis of Uterine Leiomyomas
-
(I)
Basic Concepts
-
Uterine leiomyomas, commonly referred to as fibroid or myoma, are composed of amounts of smooth muscle and fibrous tissue, and the etiology is due to uterine smooth muscle cell proliferation. It is the most common benign tumor in the female reproductive system, the incidence accounting for 4–11% and 70–80% occurrence in women between 30 and 50 years old.
-
Almost 80% of the uterine leiomyomas are multiple according to the pathoanatomy, sometimes even more than one hundred. Fibroids are commonly classified into two subgroups by location: corpus and cervical, of which the former accounts for about 90%. The corpus leiomyomas are classified as intramural, subserosal, submucosal, and broad ligament leiomyomas. These tumors are usually multiple and various types of leiomyomas can coexist in one uterus.
-
The appearance of leiomyomas may be various which may be according to the replacement of various degenerative tissues as abnormal blood supply. The degeneration is classified into hyaline, myxoid, cystic, calcific, red, necrosis, fatty, infection, and malignant degeneration. Special types, such as cellular leiomyoma, atypical leiomyoma, mitotically active leiomyoma, and intravenous leiomyoma, are also listed here.
-
The clinical manifestations are mainly related to the location and size of uterine leiomyoma. The most common symptoms include menstrual cycle changing, abdominal mass, and compression symptoms. The majority of patients complain of abnormal uterine bleeding, heavy menstrual bleeding and shortened menstrual cycle. Bowel dysfunction and bladder symptoms such as urinary frequency and urgency may be present by large fibroids.
-
During physical examination, we can find an enlarged, solid uterus with an irregular contour which is consistent with fibroids. In addition, submucosal fibroids may prolapse to the endometrial cavity, cervix, or vagina.
-
Ultrasonography is particularly helpful to assess the location, size, and number of myomas. Transvaginal ultrasonography provides superior resolution for fibroids smaller than 2 cm in diameter. However, ultrasonic attenuation is usually accompanied by large fibroids, and it is recommended to choose low-frequency probe and increase the gain.
-
-
(II)
Ultrasonic diagnosis
-
Enlarged or irregular-shaped uterine can be caused by multiple leiomyomas. The size and shape of the uterine are normal when accompanied by a single small intramural leiomyoma. In cases of submucosal leiomyoma or multiple leiomyomas, the uterine shape is abnormal with distorted endometrium (Figs. 5.1, 5.2, and 5.3).
-
Leiomyomas may have variable appearances because of the different portions of smooth muscle and fibrous tissue. The leiomyomas can represent hypoechoic, hyperechoic, isoechoic, or punctate echo, with a typical linear shadowing effect (also known as swirling echo, Figs. 5.4, 5.5, and 5.6).
-
Leiomyomas are easy to be diagnosed and measured by ultrasonography. Most represent a spherical mass, with hypoechoic or lightly hyperechoic pseudocapsule (Fig. 5.7).
-
Color Doppler flow imaging shows a circular or semicircular blood flow around the leiomyomas (Fig. 5.8).
-
Uterine leiomyomas occasionally undergo various forms of degeneration. The ultrasonic changes include the disappearance of normal swirling structure, hypoechoic mass, irregular cystic area in the mass, and hyperechoic area accompanied by attenuated acoustic shadowing within or around the mass. Degenerated leiomyoma is more common in pregnancy and postpartum, and often manifests as hypoechoic mass. In addition, calcification of leiomyoma usually occurs in postmenopausal women (Figs. 5.9 and 5.10).
-
-
(III)
Special tips
-
A relatively full bladder is important for transabdominal ultrasonography. Transvaginal sonography alone may fail to show the entire fibroids larger than 8 ~ 10 cm in diameter, and the combination scanning of TAS with TVS is recommended (Fig. 5.11).
-
Subserosal leiomyoma with long peduncle or broad ligament leiomyoma may be misdiagnosed as ovarian mass. Pay attention to the relationship between the leiomyoma and the ovary (Fig. 5.12).
-
Cystic degenerated leiomyoma should be distinguished from adnexa cyst and pregnant sac (Fig. 5.13).
-
The leiomyoma should be distinguished from adenomyosis, uterine hypertrophy, endometrial polyp, adnexa mass, and uterine malformation, etc. (Fig. 5.14, 5.15, 5.16, 5.17, and 5.18).
-
-
(IV)
Typical cases
Differential diagnosis of leiomyoma and intrauterine remainder. (a) A hypoechoic subserosal fibroid with a distinct boundary. (b) Seven days after a drug-induced abortion. Sonogram shows a heterogeneous hyperechoic mass in the uterus of a patient with vaginal bleeding. The arrow indicates the intrauterine residual
A 41-year-old patient presents with a palpable mass in the abdomen, with normal menstruation. (a, b) The ultrasonography shows a normal-appearing uterus and a mixed mass at the right posterior to the uterus with solid and cystic heterogeneous. As there are irregular fluid areas in the mass, it is suspected as an ovarian tumor. (c) Gross specimen from operation shows a fibroid located in the posterior of the uterine isthmus. The pathological diagnosis is leiomyoma with extensive degeneration
A 30-year-old patient complains of pain for 1 month. (a) Ultrasonography shows a normal uterus with an intrauterine device. A huge solid mass is shown in the pelvic and is suspected as a solid ovarian tumor. The operation confirms that it is a leiomyoma in the left broad ligament. (b) Gross specimen. The pathological diagnosis is leiomyoma with myxoid degeneration
5.2 Sonographic Features of Adenomyosis
-
(I)
Basic concepts
Adenomyosis is characterized by the endometrial glands and stroma are present in the myometrium, which is combined with a proliferation of smooth muscles and fibrous tissues. The etiologies are commonly reported as chronic endometritis and trauma in the myometrium which is secondary to multiple gravidity and deliveries. Adenomyosis was called internal endometriosis previously.
Adenomyosis commonly occurs in 30–50 years old multipara and 50% of the patients coexists with leiomyoma. Adenomyosis may coexist with pelvic and other organic endometriosis, also known as external endometriosis.
Adenomyosis affects the myometrium diffusely and shows as an enlarged global uterus. The diffuse or focal lesions in the myometrium are clarified and the lesions often locate in the posterior myometrium. It leads to more thickened posterior myometrium than the anterior. The ultrasonic display of focal adenomyosis, sometimes called adenomyoma, is similar to leiomyoma. While the former shows indistinct demarcate, island glands and stroma are visible in the myometrium under a microscope.
The symptoms of adenomyosis are characterized by progressive dysmenorrhea, menometrorrhagia, menostaxis, and even infertility. Some patients are asymptomatic. A diffusely enlarged and solid uterus can be palpable, accompanied with tenderness sometimes.
-
(II)
Sonographic features
-
Sonogram shows a diffused enlarged uterus in a normal shape or globular shape. In general, the uterus shows a longer length, width, and anteroposterior diameter (Fig. 5.21).
-
Most patients with adenomyosis represent a thickened posterior myometrium and the endometrium is distorted forward or backward (Fig. 5.22).
-
Thickened myometrium usually represents hyperechoic. The ultrasonic display of focal adenomyosis is similar to leiomyoma but shows an indistinct border with peripheral myometrium (Fig. 5.23).
-
Sporadic and irregular tiny fluid areas are visible in the lesion during the menstrual period, which disappears after menstruation (Fig. 5.24).
-
The image of diffuse adenomyosis shows that the whole myometrium is thickened, and diffusely enhanced echo. The location of the endometrium is normal (Fig. 5.25).
-
Color Doppler shows that the blood flow is sporadic and stellate distributed in the focus of adenomyosis (Fig. 5.26).
-
-
(III)
Special tips
-
The ultrasound images of adenomyosis and hysteromyoma are extremely similar. Except to consider the clinical manifestations, we should pay more attention to the boundary of the lesion and surrounding muscle.
-
Transvaginal ultrasonic scanning is recommended to identify the lesion boundary and endometrium in multipara patients (Fig. 5.27).
-
5.3 Ultrasonic Diagnosis of Endometrial Carcinoma
-
(I)
Basic concepts
Endometrial carcinoma, one of the three common malignant reproductive tumors in females, accounts for 20–30% of the malignant reproductive tumors in females. The incidence is related to race and region. According to recent statistical data, the incidence of endometrial carcinoma increases, which is most prevalent in patients aged 58–61.
The exact cause of endometrial carcinoma remains unclear. The high-risk factors include long-term and continuous endometrial stimulation by exogenous or endogenous estrogen, endometrial hyperplasia, obesity, hypertension, diabetes, unmarried, nulliparous, delayed menopause, genetic factors, etc.
The pathological findings of endometrial carcinoma are mainly divided into the diffuse type and localized type. Most of the lesions of localized type locate in the fundus of the uterus, especially near the uterine cornu. In the early stages, the endometrium shows a rough surface, the lesions are superficial and small without a mass. Sometimes, a pathological section could probably not find an obvious carcinoma lesion, which might be due to the previous diagnostic curettage or multiple curettages. Diffuse endometrial carcinoma involves a wide range of endometrium or multifocal lesions. Localized carcinoma shows polypoid or cauliflower-like growth in the uterine cavity. The common cell types of endometrial carcinoma include endometrioid adenocarcinoma (accounting for 70–80% of endometrial carcinoma), adenocarcinoma with squamous epithelial differentiation, special types such as serous papillary carcinoma and clear cell carcinoma, etc. The typical metastasis of endometrial carcinoma involves myometrial invasion, lymphatic invasion, vascular invasion, and advanced hematogenous metastasis, etc.
The typical clinical symptoms are intermittent or persistent postmenopausal vaginal bleeding. Premenopausal patients usually complain of increased menstrual volume, prolonged menstrual period, or intermenstrual bleeding. Some patients manifest with vaginal discharge, while bloody and pyometra discharge with the strong stench in advanced patients. The cervical invasion of tumor may lead to obstruction of the cervical canal, resulting in hematocele or pyometra in the uterine cavity and manifesting lower abdominal pain. In the late stages, it may cause pain in the lower abdomen and lumbosacral region which is related to the tumor invasion of surrounding tissue or compression of the mass.
In the early stages, most patients do not have any obvious systemic symptoms or signs. The enlarged and softened uterus could be palpated. Irregular nodular masses around or beside the uterus could be found in advanced patients.
The diagnosis of endometrial carcinoma is based on the pathological results of curettage.
-
(II)
Ultrasonic diagnosis
-
In the early stages of endometrial carcinoma, doctors could not find obvious endometrial morphologic changes by ultrasonographic image. Some patients with endometrial carcinoma only show slightly thickened endometrium or fluid in the uterine cavity (Fig. 5.28).
-
Sonographic image finds enlarged uterus in patients with advanced stages of endometrial carcinoma. The enlarged uterus is especially found in patients with original atrophic after menopause. The single layer of endometrium may be thicker than 0.5 cm, with an irregular solid mass in the uterine cavity in some cases (Fig. 5.29).
-
When the infiltration is involved into the myometrium, the endometrial-like echo extends to the myometrium. Endometrial carcinoma may also obstruct the cervical canal, resulting in irregular hyperechoic findings in the cervical canal (Fig. 5.30).
-
An ultrasonographic image shows fluid, hematometra, and pyometra in the endometrial cavity, due to the obstruction of the cervix (Fig. 5.31).
-
-
(III)
Special tips
-
For postmenopausal women with the single layer of endometrial thickness ≥ 0.4 cm, or unevenly thickened, or space-occupying lesions; or premenopausal women with menstrual disorder accompanied by menometrorrhagia, it is advisable to carry out the diagnostic dilatation and curettage as soon as possible (Fig. 5.32, 5.33, 5.34, and 5.35).
-
Endometrial carcinoma should be distinguished from endometrial hyperplasia, submucous myoma, endometrial polyp, senile endometritis, uterine effusion, and functional uterine bleeding.
-
-
(IV)
Classic cases
-
A reproductive woman represented with irregular vaginal bleeding for 3 months. Ultrasonography shows a space-occupying mass in the uterine cavity, which is suspected residue, and endometrial carcinoma is confirmed by pathological examination after curettage (Fig. 5.36).
-
An elderly woman, with no vaginal bleeding, represented an obvious fluid area in the uterine cavity, without thickened endometrium. The uterine effusion and endometrial carcinoma were confirmed by diagnostic dilation and curettage (Fig. 5.37).
-
Endometrial carcinoma (I). (a) A 57-year-old patient represented with irregular vaginal bleeding for 1 month. A solid mass (arrow), 2.0 cm in diameter, and fluid (shown with “*”) are shown in the uterine cavity. (b) A 63-year-old postmenopausal patient, menopause for 13 years, presents mild vaginal bleeding. Sonogram shows the fluid area (arrow) in the uterine cavity, with a diameter of 5.7 cm
Endometrial carcinoma (II). (a) A 44-year-old patient with a history of menstrual disorder for half a year. Sonogram represents a thickened endometrium and heterogeneous echo. (b) A woman with a postmenopausal period of 10 years. Sonogram shows an enlarged uterus with thickened hyperechoic endometrium. (c) A woman with a postmenopausal period of 6 years, represented with mild vaginal bleeding. The ultrasonogram shows the thickened heterogeneous endometrium, with multiple cystic changes. (d) Ultrasonographic findings showed the thickened, heterogeneous, and mass-like endometrium, with fluid area in it (arrow)
Endometrial carcinoma (III). (a) Sonogram shows the thickened endometrium and the “nibbling like” endometrial invasion. (b) A 61-year-old patient complained of vaginal bleeding for half a year. Ultrasonographic images show the thickened hyperechoic endometrium with ascites around the uterus. (c) A patient with endometrial and cervical adenocarcinoma. Sonogram shows the hypoechoic mass in the uterine cavity and posterior wall of the cervix (arrow)
Endometrial carcinoma (IV). (a) A 65-year-old patient, with a postmenopausal period of 10 years, represented mild vaginal bleeding. Ultrasonographic image shows a small amount of fluid in the uterine cavity and a hyperechoic mass in the anterior wall of myometrium, with a diameter of nearly1.5 cm. (b) A patient with a postmenopausal period of 6 years, accompanied by hypertension and diabetes mellitus, represented with vaginal spotting for one month. Ultrasonographic images show the fluid area with a diameter of 3.0 cm and tiny dot-like echoes (arrow) in the uterine cavity
Endometrial carcinoma (V). A 38-year-old patient represented irregular vaginal bleeding for 3 months. (a) Ultrasonography showed a space-occupying mass in uterine cavity, which was suspected residue. (b) Gross specimen. Endometrial carcinoma was diagnosed after an operation, with a confirmed pathological diagnosis of moderately and highly differentiated endometrial adenocarcinoma
Endometrial carcinoma (VI). A 57-year-old patient with a postmenopausal period of 9 years represented vaginal bleeding for 5 days. (a) Ultrasonography shows the fluid in the uterine cavity and a slightly hyperechoic mass with a diameter of 2.0 cm at the fundus. Endometrial carcinoma was diagnosed by subsequent curettage. (b) Gross specimens after the operation
5.4 Ultrasonic Diagnosis of Benign Endometrial Lesion
-
(I)
Basic concept
Endometrial polyp is a common tumor-like lesion, which is composed of local hyperplasia of endometrial glands and stroma. Endometrial polyps with pedicles grow into the uterine cavity. Some of the pedicels are relatively long, even protruding to the internal cervical os. It can occur at any age, especially in women aged 50–60 years.
Histologically, endometrial polyp has smooth surface, sometimes complaint as hemorrhage, necrosis and ulceration when accompanied by infection. It can be single, multiple, or diffuse lesions with different shapes and ranges from millimeters to centimeters. Pathologically, it can be divided into functional, nonfunctional, adenomyomatous, and postmenopausal endometrial polyps. The pedicles are different in thickness and length.
The typical clinical manifestation is menometrorrhagia or spotting bleeding. A single small polyp can be asymptomatic.
-
(II)
Ultrasonic diagnosis
-
The uterus is normal or slightly enlarged, without morphology change.
-
Space-occupying lesion is visible in the uterine cavity, with discontinued or distorted endometrium. Most of them are hyperechoic, round, or punctate, attached to the inner wall of the uterine cavity, and well-defined with the endometrium (Figs. 5.38 and 5.39).
-
-
(III)
Special tips
-
Transvaginal ultrasound is recommended to show the morphology of the endometrium. Ultrasound images show abnormally thickened endometrium in the cases of diffuse heterogeneity polyps. Sonohysterography is helpful to distinguish between the endometrial polyps and endometrial thickening.
-
Endometrial polyps should be differentiated from endometrial hyperplasia, submucous myoma, endometrial carcinoma, and intrauterine residue (Figs. 5.40, 5.41, 5.42, 5.43, 5.44 and 5.45).
-
Endometrial polyps (I). (a-d) Sonogram shows the space-occupying lesions and the discontinued endometrial line. (e) A 61-year-old patient with a postmenopausal period of 10 years represented a little amount of vaginal bleeding. Sagittal and transverse TVS shows a slightly hyperechoic lesion with a diameter of about 2.0 cm in the uterine cavity, with multiple small cysts in it. (f) A 66-year-old patient with a postmenopausal period of 13 years. Sagittal and transverse TVS shows an intrauterine space-occupying hyperechoic lesion with a diameter of about 3.5 cm. Multiple small cysts are visible in the lesion (arrow)
Endometrial polyps (II). A 45-year-old patient with a history of menstrual disorder for 1+ year received an ultrasonic examination. (a) Sagittal view of TVS shows heterogenous thickened endometrium. (b) Multiple polyps are shown protruding into the fluid in the uterine cavity after saline infusion (arrow)
Identification of endometrial polyp and intrauterine residue. (a) The space-occupying lesion was shown in the uterine cavity and the endometrium discontinued; (b) Sagittal view of TVS shows the thickened endometrium. (c) Sonogram shows a hyperechoic mass with a diameter of about 3.0 cm floating in uterine fluid after saline infusion (arrow)
Identification of submucous myoma and endometrial polyp. (a) A patient complained of excessive volume of menses with blood clots for 2+ years. Sonogram shows a hypoechoic mass, 2.4 cm in diameter with a well-defined boundary, in the uterine cavity. (b) A patient diagnosed with primary infertility represented menstrual disorder for 3 years. Sonogram shows the thickened endometrium. (c) Multiple hyperechoic masses are shown in the uterine cavity after saline infusion (arrow)
The differential diagnosis of endometrial polyp and tuberculosis. (a) A 37-year-old patient represented menstrual disorder with an excessive volume of menses for 2 years. Ultrasonography shows multiple irregular, heterogeneous hyperechoic masses in the uterine cavity; (b) A 24-year-old patient with a history of tuberculosis and secondary amenorrhea for 7 years. Heterogeneous hyperechoic mass is shown in the uterine cavity, which is suspected as endometrial tuberculosis (arrow)
Other endometrial lesions. (a) A 32-year-old patient complained of secondary amenorrhea for 7 years after induced abortion. Strip-like hyperechoic tissue with an attenuated shadow is found in the uterine cavity, which is identified as residual calcification and intrauterine adhesions. (b) Hypomenorrhea for 3 years after induced abortion. Sonogram shows irregular hyperechoic tissue with acoustic shadow, indicating calcification (arrow)
5.5 Ultrasonic Diagnosis of Cervical Lesions
-
(I)
Basic concepts
-
The cervix, a part of the uterus, is mainly composed of fibrous connective tissue and a small amount of smooth muscle cells. It is cylindrical and 2.5–3.0 cm in length. The cervical canal locates in the center, and the inner membrane of the canal can secret alkaline mucus. Cervix has many defense functions, but it is vulnerable to be injured by childbirth and uterine cavity operation, leading to chronic cervicitis, which is the most common disease in gynecology.
-
Due to the special characteristics of cervical anatomy and histology, the formation of the squamous columnar junction is highly sensitive to the stimulations caused by some carcinogenic factors. Cervical cell dysplasia, disordered cell arrangement, abnormal cells, and increased mitosis may exist and lead to invasive cervical cancer eventually.
-
Cervical cancer is the most common malignant tumor of the reproductive tract, with a high incidence in 35–39-year-old and 60–64-year-old women. The exact cause is not completely understood. Recently, human papillomavirus (HPV) infection, especially persistent high-risk HPV infection, is considered to be the main cause of cervical precancerous lesions and cervical cancer. Other related risk factors include early childbirth, multipara, high-risk male partners, and immune suppression.
-
Common histological types include squamous cell carcinoma, adenocarcinoma, squamous adenocarcinoma, spinous adenocarcinoma, clear cell carcinoma, and undifferentiated carcinoma. According to the differentiation level, cervical cancer is divided into high differentiated, moderately differentiated, and poorly differentiated carcinoma. According to the different development stages, cervical carcinoma is divided into carcinoma in situ, early invasive carcinoma, and late invasive carcinoma.
-
Exogenic type, endogenic type, ulcerative type, and endocervical type are common cervical squamous cell carcinoma, which accounts for 80–85% of all cervical carcinoma. Cervical adenocarcinoma accounts for about 15%. The main metastasis of cervical cancer is direct invasion and lymphatic metastasis.
-
In general, there are not any obvious clinical symptoms and signs are shown in the early stage of cervical cancer. Once manifestations are present, usually shown as vaginal bleeding and abnormal vaginal discharge. Symptoms such as frequent urination, urgent urination, constipation, edema and pain of lower limbs, and even systemic cachexia can be complained in the late-stage patients with lesions spreading to pelvic connective tissue. In advanced-stage patients, cervical cauliflower mass can be seen protruding to the vagina during the pelvic examination, with a bleeding tendency. In the endocervical types, the cervix is hypertrophic and firm, with smooth surface or superficial ulcer, cervical canal is enlarged, and depressed ulcers are visible in advanced-stage patients. Thickened and nodular parametrial tissues can be palpated in the gynecological examination, even invaded into the pelvic wall, forming a frozen pelvis.
-
The main clinical symptoms of chronic cervicitis are increased vaginal discharge, hemorrhagic leucorrhea, and postcoital bleeding. When the inflammation involves other adjacent organs or spreads to the pelvis, lumbosacral pain and lower abdominal pain may occur.
-
The pathological changes of chronic cervicitis include cervical erosion, cervical polyp, cervical mucositis, cervical Nabothian’s cyst and cervical hypertrophy, etc.
-
-
(II)
Ultrasonic diagnosis
-
The main ultrasonic manifestations of chronic cervicitis, including cervical Nabothian’s cyst, cervical hypertrophy, and cervical polyp.
The enlarged cervix with multiple anechoic cysts (Fig. 5.46).
-
Ultrasonic images of cervical cancer.
-
No obvious ultrasonic findings are shown in the early stage of cervical cancer. When the lesion grows to a certain size and protrudes to the external os or appears as a mass, the ultrasonic image shows an enlarged cervix with a diameter of more than 3 cm. The morphology of the endocervical membrane is abnormal or disappeared (Figs. 5.47 and 5.48).
-
A heterogeneous, hypoechoic, or hyperechoic, irregular mass can be shown in the cervix. When the tumor infiltrates the bladder and parametrium, the ultrasonic images show an unsmooth bladder wall and irregular hypoechoic tissue around the uterus (Fig. 5.49).
-
Color Doppler shows abundant blood flow in cervical cancer (Fig. 5.50).
-
-
-
(III)
Special tips
Cervical cancer (I). (a) Sagittal view of TVS shows a larger cervical diameter compared with the uterine anteroposterior dimension, and the cervix is hypoechoic. (b) Transabdominal ultrasonography shows a larger cervical diameter compared with the uterine anteroposterior dimension, and the cervical canal is disappeared, accompanied by the abnormal cervical morphology
Cervical cancer (II). A 59-year-old patient with a postmenopausal period of 7 years represented vaginal bleeding for 3 months. (a) Ultrasonic images show atrophic corpus, abnormal cervical morphology, and an irregular mass with a diameter of about 7.0 cm. (b) Transverse images show the mass of the same patient
Cervical cancer infiltration. (a) Sonogram shows the enlarged cervix with abnormal shape, and the mass infiltrated into the bladder wall (arrow). (b) Sonogram shows the enlarged cervix without the normal cervical canal, obstructed internal os, and uterine effusion (arrow). (c) Sonogram shows the irregular parametrial cystic lesion, indicating parametrial invasion
The blood flow of cervical sarcoma and cervical cancer. A 51-year-old patient represented recurrent vaginal bleeding four times. (a) Sonogram shows the abnormal cervix morphology, absent endocervical endometrium, with the cervical diameter larger than the corpus. (b) In the same patient, color Doppler shows abundant blood flow in the cervical tumor. Pathological diagnosis of cervical sarcoma is confirmed. (c) A 67-year-old patient represented with irregular vaginal bleeding history for half a year. Sagittal view of TVS shows an obvious enlargement of the cervix. (d) Sagittal view of the same patient. Abundant blood flow is shown in the cervical lesions by color Doppler. Cancer cells are found on the cervical smear and cervical carcinoma is diagnosed by operation and pathological examination
The differentiation of cervical cancer and cervical pregnancy. (a) A cervical cancer patient shows an abnormal cervix with an enlarged diameter and hCG is negative. (b) The cervix is “barrel-like” enlarged, with gestational sac or heterogeneous hyperechoic tissue in the cervical canal, and hCG is positive
The differentiation of cervical cancer and cervical myoma. (a) A cervical cancer patient. Sonogram shows the larger cervical diameter compared with the corpus, abnormal cervical morphology, and irregular and heterogeneous mass. (b) Cervical leiomyoma, which is mostly located in the posterior labium of the cervix, is usually well-defined, and the endocervical endometrium is visible by altering the scanning angle
5.6 Ultrasonic Diagnosis of Uterine Sarcoma
-
(I)
Basic concepts
Uterine sarcoma, which is rare, is the most malignant tumor of the female genital system. Leiomyosarcoma accounts for about 0.64% of the smooth muscle tumors of the uterus, and 45–75% of the leiomyosarcoma. Leiomyosarcoma generates from the myometrium or the connective tissue in the myometrium. Uterine sarcomas are susceptible in perimenopausal women but also can occur in young women.
According to the different original tissues, sarcomas are mainly divided into the following types: (1) Leiomyosarcoma of the uterus, which arises from the myometrium or the smooth muscle fibers of the uterine vascular wall, or from the malignant transformation of uterine fibroids. (2) Endometrial stromal sarcoma, which is derived from endometrial stromal cells and divided into low-grade and high-grade malignant stromal sarcoma. (3) Malignant mixed müllerian disease, also known as carcinosarcoma, arises from residual embryonic cells or interstitial cells metaplasia.
The main clinical symptom is vaginal bleeding, which is characterized by an excessive volume of menses, irregular bleeding, or postmenopausal bleeding. The amount of the blood varies from bloody leucorrhea to purulent discharge with a peculiar smell. Some patients have no obvious symptoms and are diagnosed as palpable abdominal mass. Advanced patients may represent anemia, cachexia, lower abdominal pain, backache, and so on. Gynecological examination revealed an enlarged, irregular, and soft uterus, even occupying the whole pelvic cavity.
-
(II)
Ultrasonic diagnosis
-
Ultrasonic scanning shows the myoma grows rapidly within a short time, with obvious attenuation, and it is difficult to recognize the three-layer structure of the uterus (Fig. 5.53).
-
A large solid mass is visible in the pelvic cavity, while the uterus is pressed to the side. Normal uterine morphology fails to be shown in some cases (Fig. 5.54).
-
Ultrasonography shows heterogeneous or disordered echo in large myomas.
-
-
(III)
Special tips
-
When a patient with a history of uterine fibroids represents rapidly fibroids enlargement within a short time, it should be a concern for the clinicians. The characteristics of the uterine echo and the three-layer structure should be identified during ultrasonic scanning.
-
Sarcomas should be distinguished from huge benign uterine fibroids and ovarian tumors. Women of childbearing age should be paid more attention to bilateral ovaries.
-
Uterine sarcoma. A 17-year-old female patient recurred with fibroids 1 year after myomectomy. (a) 2-D TAS shows multiple hypoechoic masses conglobated together in the myometrium of the right lower segment area and subserosal area, with the size of about 5.7 cm × 8.1 cm × 7.8 cm. The other one is located in the right anterior area of myometrium with the size of 2.2 cm × 2.9 cm × 2.9 cm. (b) Abundant blood flow signals are shown in the masses and peripheral area. Pathology confirmed the diagnosis of uterine leiomyosarcoma
Pelvic sarcoma. An 18-year-old patient experienced left lower abdominal pain for 1 month. Ultrasound image shows a mass in the pelvic cavity. (a) TAS shows a solid mass in the pelvic cavity, which is measured comparably to the uterus of 16 gestational weeks. The uterus is challenging to be recognized. (b) The gross specimen. Pathological diagnosis is embryonal rhabdomyosarcoma
5.7 Ultrasonic Diagnosis of Abnormal Development of Female Reproductive Organs
-
(I)
Basic concepts
-
At the third to fourth gestational weeks, primordial germ cells appear in the yolk-sac endoderm. At the fourth to fifth week, a genitourinary crista is formed. At the fourth to sixth week, primordial germ cells migrate to genitourinary crista to form primordial gonad. At the eighth week, primordial gonad differentiates into the ovary.
-
After the gonads develop into ovaries, the mesonephric tube on the lateral side of the urogenital ridge degenerates. The head segments of the accessory mesonephric tubes on both sides form two fallopian tubes, and the middle and tail segments on both sides combine to form the uterus and the upper segment of the vagina. At the early stage of syncopation, there is still a septum, which divides the syncopation into two chambers. The septum disappears at the end of 12 weeks and becomes a single lumen. The caudal end of the accessory mesonephric duct is connected with the urogenital sinus, meanwhile, it divides and proliferates to form the vagina cavity.
-
The abnormalities caused by the obstruction of normal duct formation of female reproductive organs include hymen atresia, vagina transverse, vagina mediastinum, congenital vagina atresia, and cervical atresia, etc. The abnormal uterine development caused by the hypoplasia or fusion obstacle of accessory mesonephric duct derivative includes a congenital absence of uterus, primordial uterus, uterine dysplasia (immature uterus), unicornuate uterus, uterus duplex, and uterus bicornis, saddle form uterus, mediastinal uterus, etc.
-
The clinical manifestations of female congenital malformation are as follows:
-
No menarche after puberty accompanied by periodic lower abdominal pain may experience following diseases, such as imperforate hymen, vaginal septum (diaphragm or oblique septum), partial atresia of the vagina and congenital cervical atresia, etc.
-
No menarche after puberty should be distinguished from the following situations, such as ametria, primordial uterus, and immature uterus, etc.
-
Patients with dyspareunia after marriage, recurrent abortions, premature delivery or infertility, should be examined to exclude the following conditions, such as the congenital absence of vagina, ametria, vaginal septum, vagina atresia, unicornuate uterus, uterus bicornis, and uterus septus, etc.
-
-
-
(II)
Ultrasonic diagnosis
-
Congenital absence of uterus is also called ametria. No uterus is visible by both TVS and TAS behind the bladder. Relatively smaller ovaries can be detected on both sides of the pelvic cavity in most patients. Congenital absence of uterus is often combined with congenital absence of vagina, resulting in the absence of vaginal gas line (Fig. 5.55).
-
Rudimentary uterus. Transabdominal or transvaginal ultrasonic images show only a small cord-like hyperechoic mass behind the filled bladder. No normal uterine morphology or endometrium is shown. Ovaries can be found on both sides of the pelvic cavity in some patients (Fig. 5.56).
-
Hypoplasia of uterus (infantile uterus). The uterus is shown in the pelvic cavity with a shorter anteroposterior dimension, length, and width compared to normal uterus. The anteroposterior dimension is less than 2 cm. The endometrium is unclear or in a thin line shape (Fig. 5.57).
-
Uterus didephys. Ultrasonography shows two separate uterus and two separate uterine cavities. When the transabdominal ultrasonic examination is used, it should be transversely scanned from the fundus to the cervix and vagina, or from the vagina to the cervix and fundus. On the transverse view, the fundus shows like a butterfly. When moving down the probe to the uterine body, the transverse diameter of the uterine body is wider than normal. Then the two cervical canals and vaginal gas lines can be displayed when the probe is a slant to the posterior pubis. In the longitudinal scanning, place the probe on the lower abdomen and move slowly to the opposite side, two separate uteruses are displayed in turn (Figs. 5.58 and 5.59).
-
Uterus bicornis or arcuate uterus. Transabdominal transverse scanning shows two uterine horns similar to the shape of sheep’s horn in the level of the fundus, accompanied by a separate uterine cavity. The lower segment of the uterine and cervix usually represents normal. When the probe is moved to scan the uterine body longitudinally, two uterus images may be shown, while only one cervix and vagina can be found. When the uterus bicornis shows a concave uterine fundus on transverse section, it is also called arcuate uterus (Fig. 5.60).
-
Uterus septus. No obvious changes can be found in the contour and morphology of the uterus. The transverse images show the wider fundus with a larger transverse diameter than normal. The uterine cavity shows similarly with the shape of the Chinese character “八” or the English letter “Y.” Two separate endometriums are visible from the fundus to the cervix in the complete septate uterus, from left to right or from anterior to posterior. Partial uterus septus is characterized by the attenuated septal echo between endometrium, as the septum does not extend from the fundus to the cervix (Figs. 5.61 and 5.62).
-
Rudimentary horn of uterus. A normal uterus can be seen in the pelvis with a solid mass on either side of the uterus. The echo of mass is similar to the nonpregnant uterus, without endometrium. It is easy to be confused with subserosal myoma. A small amount of fluid may be found in some rudimentary uterus. When pregnancy occurs in the rudimentary horn, the diagnosis of rudimentary horn of uterus may be considered (Fig. 5.63).
-
Congenital imperforate hymen. Sonogram shows the normal uterus, saccular or oval dilatation from cervix to the vagina, with weak or enhanced echo inside. Some patients combined with uterine cavity dilatation and cervix dilatation (Fig. 5.64).
-
Atrasia of vagina or vaginal septum. Sonogram shows the normal uterus, dilatated uterine cavity or cervix, and vaginal dilatation above the vaginal septum or oblique septum. Patients with a relatively longer history of the disease may accompany dilation of bilateral fallopian tube or bilateral adnexal masses, with retention of menses inside (Fig. 5.65).
-
-
(III)
Special tips
-
There are many different types of female congenital genital malformation. Various scanning methods are recommended. TAS is utilized to show the position and structure of the uterus for further diagnosis of the uterus didephys, uterus bicornis, and septate uterus. The endometrial echo is an important sign to identify uterine malformation.
-
Attention should be paid to differentiate bicornate uterus and rudimentary horn uterus from subserosal myoma and ovarian mass.
-
Female congenital genital malformation may be combined with malformation of urinary system, such as the absence of kidney, ectopic kidney, etc. (Fig. 5.66).
-
When it is difficult to identify the malformation of uterus by two-dimensional ultrasound, sonographic hysterography can be performed to show the endometrium and uterine cavity more clearly (Fig. 5.67).
-
Hypoplasia of uterus. (a) A 21-year-old patient represented with no menarche. TAS shows the anteroposterior dimension of uterus is 1.8 cm, without endometrium shown. (b) A 19-year-old patient represented oligomenorrhea and hypomenorrhea. The size of the uterus is 2.2 cm × 4.4 cm × 2.0 cm and the endometrial is extremely thin
Septate uterus. (a) Complete septate uterus is shown on the coronal plane. (b) The endometrium is shown as the shape of letter “Y” on the coronal view. (c) The transverse image of the uterus shows the typical endometrial morphology similar to “cat’s eye” (arrow). (d) The transverse view of the uterus showed the endometrium in the shape of the Chinese word “八” (arrow)
Congenital imperforate hymen. (a) A 14-year-old patient represented periodic lower abdominal pain for 4 months. TAS shows a normal uterus with fluid area in the uterine cavity, and cystic dilatation from the lower cervix to the vagina. (b) An 11-year-old patient represented periodic pain in the lower abdomen for half a year. TAS shows normal uterus and cystic dilatation of the vagina with tiny and weak echo inside
Atrasia of vagina (a) A 15-year-old patient had menstruation for 2 years with dysmenorrhea. TAS shows two uteruses, with hematometra in the right uterine cavity and vagina. The fluid area in the uterine cavity is connected with the vagina. The left uterus is slightly smaller than the right one, with normal morphology. Uterus didephys with atresia of the right vagina is confirmed by operation. (b) A 14-year-old patient represented with secondary amenorrhea and periodic lower abdominal pain for 1+ years. Sagittal TAS shows intrauterine hematometra connected with the fluid area in the middle and upper segments of the vagina. Adhesion and atresia of lower segment of vagina are diagnosed after operation
5.8 Ultrasonic Diagnosis of Ovarian Masses in Pelvic Cavity
The ovary is an important reproductive organ in the female pelvic cavity. The ovary is small while the ovarian histoembryology, anatomy, and endocrine function are extremely complex. The type, morphology, and nature of the ovarian mass are various. The traditional diagnostic method of ovarian masses is pelvic bimanual examination. The examiners evaluate the ovarian size, shape, and texture by hand, which is difficult to detect early masses. When the masses can be palpable by bimanual examination, most patients are already in the middle and late stage of the tumor. In recent years, with the rapid development of imaging technology, CT and MRI can clearly show the mass less than 5 mm, lymph node metastasis, and ascites. However, due to the high price, it is limited to screen early ovarian masses. The serum markers for the diagnosis of ovarian cancer (CA125, AFP) are one of the screening tools for ovarian cancer, while the screening sensitivity needs to be improved.
Recently, the application of ultrasonography in the diagnosis of ovarian diseases has shown obvious advantages. Transvaginal ultrasound scanning is especially well which can clearly show the physical properties and size of ovarian masses and provide valuable information for the clinician. Transvaginal Color Doppler ultrasonography is used in the diagnosis of ovarian tumors, which can obtain clear two-dimensional images. Moreover, it is helpful for the diagnosis and differentiation of benign and malignant ovarian masses by measurement of blood flow signals and the vascular resistance index. Due to the different characteristics of ovarian masses, the ultrasonic images are complex and diverse. Meanwhile, a given disease may be shown as different images and different diseases may be revealed as similar images. As a result, it is relatively difficult to determine the type of ovarian masses by ultrasound. According to the ultrasonic characteristics and clinical and pathological changes, the ultrasonic diagnosis of ovarian masses will be discussed in this section, including non-tumor cyst and ovarian tumor.
-
I.
Non-tumor cysts
-
Basic concepts
Most of the non-neoplastic cysts are retention cysts due to functional changes of the ovaries, mostly appeared in women of childbearing age. They are often associated with menstrual cycle, pregnancy, and endocrine disorders, and sometimes be related to iatrogenic medication. Most of these cysts can be absorbed by their own.
The volume of ovarian non-neoplastic cyst is generally small, with a diameter of 3–5 cm. Most of them have no clinical symptoms, while some of them can cause uterine functional bleeding, or irregular vaginal bleeding, menstrual disorders and so on. If the cyst ruptures or twists, acute abdominal pain can occur suddenly. Ovarian non-neoplastic cysts include follicular cysts, luteal cysts, luteinized cysts, parovarian cysts, polycystic ovaries, fallopian tube-ovarian cysts, simple cysts, and ovarian endometriotic cysts, etc.
-
Ultrasonic diagnosis
-
Follicular cysts
-
Mature follicles fail to rupture, ovulate, or atresia during menstrual cycles, and then the follicular fluid accumulates in the follicle cavity leading to cysts formation in females.
-
The diameter of the follicular cyst is generally less than 5.0 cm, round-shaped with thin-wall, well-circumscribed, and the fluid in the cyst is clear. Unilateral cyst is more common and most of them can vanish on their own during routine observation (Fig. 5.68).
-
-
Corpus luteum cyst.
-
The disordered blood and lymphatic supply of the corpus luteum from the ovary, or the formation of the hematoma in the corpus luteum, leads to the accumulation of clear fluid in the corpus luteum and results in cysts. This kind of cyst mostly belongs to the physiological lesion. Some of them are accompanied by delayed menstruation. The cysts will disappear naturally after menstrual onset. Similar corpus luteum cyst may also occur in early pregnancy disappear during the second trimester.
-
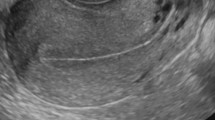
The corpus luteum cyst is mostly isolated with a translucent wall. It is usually glossy in appearance, mostly monolocular and round-shaped, with a diameter less than 5.0 cm. Color Doppler ultrasound shows abundant blood flow inside (Fig. 5.69).
-
-
Theca-lutein cyst
-
Theca-lutein cyst refers to the luteinization of theca cells on the wall of the follicular cyst, which is related to gonadal hormones from the placental, dysfunction of hypothalamic–pituitary–gonadal axis, application of ovulation induction drugs, and other factors. Theca-lutein cyst is more common in patients diagnosed as hydatidiform mole, with an incidence of 35–50%.
-
Bilateral theca-lutein cysts are more common, with a diameter of 20 cm or more, while some tiny ones can only be diagnosed under the microscope. The serum β-hCG level in patients with trophoblastic disease is significantly higher than in normal pregnancy. The masses are shown as multilocular cysts with uneven surfaces and thin septa. A clear liquid is visible in the cysts, with good acoustic transmission. The theca-lutein cysts can disappear after the primary disease is cured (Fig. 5.70).
-
-
Polycystic ovary, POC
-
The basic pathological change of polycystic ovary is homogeneously enlarged bilateral or unilateral ovaries, which is 2–3 times larger than normal with a smooth surface and thick capsule. The membrane of the ovary is thickened and the cortex is widened. Multiple follicles less than 1.0 cm usually locate peripherally along the envelope as “pearl strings” sign. Microscopical images show fibrosis of the cortical surface with fewer cells and there is little mature follicle formation and ovulation.
-
PCO is more common in women of adolescence and childbearing age. The ultrasonic images show the increased volume of bilateral ovaries, occasionally unilateral. The capsule is hyperechoic and thickened with multiple follicles less than 1.0 cm located peripherally along the cortex. They are in wheel-shaped or in net-like morphology. More than ten follicles can be seen on a single section with no mature follicle and no ovulation observed routinely. The ovarian medulla is acoustically enhanced. The ovaries are usually enlarged with multilocular cystoid alteration after the application of ovulation induction drugs (Fig. 5.71).
-
-
Simple ovarian cyst.
-
Ovarian simple cysts are usually monolocular, originated from follicular cysts or serous monolocular cysts which is usually not accompany by clinical manifestation. Pathologic examination cannot determine the origin of the cysts.
-
Most of simple ovarian cysts are unilateral and monolocular, regular round or oval shaped, with clear boundary, thin capsule, and clear fluid inside. Generally, it is rare to vanish naturally (Fig. 5.72).
-
-
Ovarian endometriotic cyst.
-
Ovarian endometriotic cyst is one of the most common lesions in external endometriosis. About 80% of the patients are involved in unilateral ovary and 50% of the patients are involved in bilateral ovaries. In the early stage of the lesion, small purple-brown spots or vesicles can be seen on the surface and in the cortex of the ovary. With the development of the disease, a single cyst or multiple cysts can be seen on the ovary, filled with dark brown, viscous and old blood, like chocolate, also known as “chocolate cyst” clinically.
-
Most patients represent dysmenorrhea and persistent pain in the lower abdomen. Progressive dysmenorrhea is usually aggravated year by year with the development of local lesions. The degree of pain is not necessarily related to the size of the lesions. About 20% of the patients do not have any obvious clinical symptoms. A few patients may have menstrual disorders. Forty percent of the patients accompany by infertility which is also a common cause of infertility.
-
Ultrasonic scanning shows round, oval, or irregular cysts on bilateral or rear of the uterus in the pelvic cavity. The capsules of the cysts are thick with an unsmooth surface. Larger cysts are usually pressed by surrounding organs or adhered to the surrounding organs. The boundary is not clearly shown.
-
The ultrasonic image of chocolate cyst varies according to the duration of lesion. The different echoes in the cysts include slightly hyperechoic uniform and dense spots, complex hyperechoic and weak echo, or anechoic clear liquid.
-
The diameter of a chocolate cyst is about 5 ~ 6 cm, and unilateral cyst is more common. The cyst may have fissures or even ruptures which may cause exuding or spreading of the cystic fluid into the pelvic cavity. And it results in adhesion between the ovary and adjacent organs. At this time, the contour of the cyst alters or even disappears (Figs. 5.73 and 5.74).
-
-
-
Special tips
-
Most of the non-tumor cystic masses on the ovary are caused by the change of an ovarian function. They are usually small in size and vanish by themselves without clinical management. But its morphology is often confused with tumor cyst.
-
TVS is very helpful to detect small lesions of an endometriotic cyst. However, it is easy to be misdiagnosed with other tumors due to the variety of sonograms of a chocolate cyst.
-
-
-
II.
Ovarian tumors
-
Basic concepts
-
The ovary is a small and complex organ, which has the most tumor types. Ovarian tumor is a common tumor of gynecologic malignancies, including benign, borderline, and malignant tumor. Cystic tumors are common and most of them are benign. Solid tumors are relatively rare. Exception for primary malignant ovarian tumors, metastasis from other organs is common, too.
-
Various types of ovarian malignant tumors have various pathological characteristics. The common pathological characteristics are the disorder of cell structure and arrangement, hemorrhage, and necrosis in the tumor. According to the histologic classification of ovarian tumors formulated by the World Health Organization (WHO), they are generally divided into epithelial tumors (50–70%), sex cord stromal tumors (about 5%), germ cell tumors (20–40%) and metastatic tumors (5–10%).
-
Ovarian cancer is one of the three common tumors of the female reproductive system, which accounts for about 15% of gynecological cancer, only lower than cervical cancer. It can occur at any age with the peak age of 45–64 years old. The survival rate is about 25–30%. The pathogenesis of ovarian cancer is mainly related to heredity, family history, environmental factors, and endocrine factors. 20–25% of patients with ovarian cancer have a family history.
-
Primary ovarian cancer can be divided into two categories: epithelial cancer and nonepithelial cancer. Metastatic tumors may metastasize from the primary malignancies of any other organs. Common metastatic tumors are common from breast, stomach, intestine, reproductive urinary tract, and other organs. The main metastasis methods are intraperitoneal implantation and lymphatic metastasis, followed by diaphragm metastasis.
-
Benign ovarian tumors are mostly asymptomatic clinically. They are often found occasionally in the routine gynecological examination. The tumors are moderately enlarged, which causes abdominal distention or palpablation. Spherical masses can be palpable unilateral or bilateral adnexal areas, either cystic or solid, indicating smooth and movability by gynecological examination. The tumors can grow big enough to occupy the full pelvis, even to the abdominal cavity. And compression symptoms may occur, such as frequent urination, constipation, difficulty in breathing and cardiopalmus, etc. Abdominal distention without shifting dullness can be found. Once the clinical symptoms of ovarian cancer appear, most patients are in advanced stages. If the tumor invades or compresses the nerves, it may cause abdominal pain, backache, lower limb pain, and anemia in the late stage.
-
The ovary locates in the deep pelvis, which makes it difficult to be palpable. Nowadays, reliable methods are not available for the early detection and diagnosis of ovarian tumors. Ultrasonography is a convenient and reliable noninvasive method for early detection of pelvic masses, which enables the possible early detection of ovarian tumors.
-
-
Ultrasonic diagnosis
-
The diagnosis of an ovarian tumor can be made by its characteristics of morphology and echo. Transvaginal ultrasound and color Doppler flow examination provide referable information for the primary judgment of ovarian tumor.
-
The sonographic images of ovarian cystic tumors are mostly unilateral or bilateral spherical or spheroid masses. Anechoic dark area can be seen in the cyst, unilocular or plurilocular. The septum of benign multilocular cysts is thin, without blood flow in the septum. Occasionally, the inner wall of some cystic tumors is uneven, or papillary solid hyperechoic protrusions are visible (Fig. 5.75).
-
The ultrasonic image of solid ovarian tumor mostly shows unilateral and moderately enlarged mass, with an unclear wall. The tumor is a homogeneous or heterogeneous solid mass, and calcification with an acoustic shadow is visible.
-
Solid tumors include ovarian fibroma, Boehner’s tumor, ovarian endometrial cancer, ovarian clear cell cancer, endodermal sinus cancer, dysgerminoma of the ovary, granular cell tumor, and theca cell tumor, etc. There are many kinds of solid tumors, without specific sonographic images, which should be confirmed by pathological examination (Fig. 5.76).
-
The ultrasound images of ovarian mixed tumors show the fluid, fibrous, and fatty structures inside the tumors. Fluid area, hypoechoic, hyperechoic, or attenuated echo is visible in the tumor, which is characterized by a disordered echo. The most common type of ovarian mixed tumor is ovarian teratoma, most of which have specific manifestations on the sonogram. Cystic teratomas appear variably ranging from completely anechoic to completely hyperechoic. The common images include dough sign, hair-clot sign, fat fluid level sign, and starflower sign, etc. (Figs. 5.77, 5.78, 5.79, 5.80, and 5.81).
-
The size of ovarian malignant tumors varies, unilateral or bilateral. The shape is mostly irregular, spherical, or oval with an unsmooth surface. The capsules are unevenly thickened, incompletely or unclearly displayed. Complex and disordered echoes are commonly seen inside the masses. The multilocular masses are more common, with a dense and thick septum. Blood flow may be seen on the septum. Ascites are visible in the pelvic and abdominal cavity (Fig. 5.82, 5.83, 5.84, and 5.85).
-
-
Special tips
-
Ovarian tumors are complex and the ultrasonic images lack specific signs. Some different kinds of tumors may have similar images and a certain tumor may have different images. The diagnosis should be confirmed in combination with the clinical manifestations, medical history, and related auxiliary examination.
-
In the ultrasonic examination of pelvic ovarian tumors, the first step is to determine the position of the uterus, in order to identify the relationship between the tumor and the uterus and to exclude the diseases of the uterus. According to ultrasonic characteristics of the tumor, benign or malignant mass was presumptive diagnosed. Once uneven or disordered mass with ascites is found in the pelvis, a related auxiliary examination should be considered to exclude malignant neoplasia.
-
Solid ovarian mass should be differentiated from intramural and subserosal myoma. Cystic mass should be differentiated from a cystic change of uterine myoma. Large cyst should be differentiated from massive ascites.
-
-
-
III.
Ultrasound diagnosis of other masses in pelvic cavity
-
Inflammatary mass
-
Basic concepts
The infection of female internal genitalia are related to postpartum or abortion, uterine cavity operation, menstrual period infection with sexually transmitted diseases, and directly spreading from inflammation of adjacent organs, which can cause infection of the pelvic internal genitalia and surrounding connective tissue as well as pelvic peritoneum.
The pelvic inflammatory diseases include acute endometritis and myometritis, acute salpingoophoritis, pyosalpinx, tubo-ovarian abscess, acute parametritis, acute pelvic peritonitis, and sepsis.
The clinical manifestations include lower abdominal pain, some severe patients may present with chills, high fever, headache, and anorexia. Increased volume and menotaxis may occur in the period, while increased leucorrhea may occur non-menstrual period. Vaginal hyperemia and purulent secretion from the cervix can be seen in gynecological examination and inflammatory mass can be palpable in the pelvis. The mass may be fluctuant and tender. Total number of leukocytes and proportion of the neutrophils can be increased obviously.
-
Ultrasonic diagnosis
-
Endometritis and acute myometriitis: (i). Endometrium is swollen, thickened, and hypoechoic (Fig. 5.86). (ii). Myometritis shows a slightly enlarged uterus, attenuated echo, and obvious tenderness (Fig. 5.87).
-
Acute and chronic salpingoophoritis (also known as adnexitis): (1) Adnexitis is characterized by unilateral or bilateral adnexal masses, with a diameter of 4–6 cm in general. The ovary is slightly enlarged and hypoechoic, surrounded by a fluid area (Figs. 5.88 and 5.89). (2) The adnexal mass is cystic or septate cystic, with flocculent or reticular echo inside. The wall is thickened and rough. The fallopian tube can be found thickened with tenderness (Fig. 5.90).
-
Pyosalpinx and tube-ovarian abscess: Unilateral or bilateral cystic masses are shown with tiny echoes or flocculent hyperechoic material inside. Masses, with unclear boundary, are adhered to both sides and posterior uterus with an obscure margin of ovary and fallopian tube. Pyosalpinx shows flaky weak echoes, and severe tenderness when touching (Figs. 5.91 and 5.92).
-
-
-
Ultrasonic diagnosis of masses after pelvic surgery
-
Basic concepts
-
Hysterectomy or subtotal hysterectomy is carried out because of uterine diseases or ovarian tumors, and unilateral or bilateral ovaries remain. Anatomical relationships of the pelvic organs change after extensive procedures for malignant tumors. The recurrence of the tumor or inflammation and endocrine disorders may also occur. All the situations above may result in masses in the pelvis.
-
Ultrasonography has been a common method in following up for postoperative patients. The vaginal stump, masses in the pelvis, ascites, and effusion between intestines should be observed when scanning.
-
-
Ultrasonic diagnosis
-
Recurrence of myoma after operation. It usually occurs in the uterine body or the residual cervix, and the mass represents solid echoes of different sizes (Fig. 5.93).
-
Recurrence of ovarian or uterine malignancies. Heterogeneous or homogeneous solid mass can be found in pelvis, may be accompanied by ascites (Figs. 5.94 and 5.95).
-
Lymphocyst after tumor surgery: Most lymphocysts locate in bilateral ilium fossa or the posterior part of the pelvic cavity, presenting cystic echoes and clear boundary. Most of the lymphocysts are less than 5 cm (Fig. 5.96).
-
Inflammatory mass. Sonogram shows the irregular cystic mass in the adnexa area, with separated or reticular echoes. The fluid in the mass is not clear. The patient has tenderness and the mass can shrink or disappear after treatment.
-
Pelvic encapsulated effusion after operation. Sonogram shows irregular mass filled with fluid, with weak tiny echoes or linear septum inside (Fig. 5.97).
-
Ovary preservation. Ovary can be found in pelvic cavity. Non-tumor cysts or tumor may occur in the residual ovary (Fig. 5.98).
-
-
Special tips
-
With the widespread use and improvement of ultrasonic technology, it has been widely used in the field of gynecology. Ultrasonography can detect various pelvic masses at an early stage, which has been a routine method for pelvic examination.
-
Inflammatory mass is the most common one in the female pelvis, and it is also a common disease of gynecology. No special signs could be found by ultrasonography, thus more attention should be paid to differentiate it from other ovarian masses. It is vital to undertake routine ultrasonic follow-up, combined with the clinical history and treatment.
-
Due to the anatomical changes after pelvic surgery, we should pay attention to the reserved reproductive organs and their positions. Note the recurrence or metastasis in patients with malignant tumor histories.
-
-
-
Corpus luteum cyst. (a) On the 42nd day of pregnancy, ultrasonography shows intrauterine gestational sac and embryo. A mass with a diameter of about 3.0 cm is found in the right ovary, and the cystic fluid is clear. (b) On the patient’s 35th day of amenorrhea, hCG is negative. Ultrasound scanning shows normal uterus without an intrauterine gestational sac. A mass with a diameter of about 3.0 cm is found in the left ovary, with clear cystic fluid. The cyst disappeared after menstrual onset
Ruptured ovarian endometriotic cyst. (a) A 36-year-old patient represented abdominal pain for 3 hours with a history of dysmenorrhea. Emergency ultrasonography shows an irregular and heterogeneous hypoechoic mass in the left adnexa area, without an obvious cyst wall. (b) A patient represented pain in the lower abdomen for 2 days with a history of “chocolate cyst.” Sonogram shows irregular hypoechoic in bilateral adnexa area without clear boundary. The free fluid area in the pelvis is about 3.0 cm
Ovarian cystic tumor. (a) The cyst is unilocular, with clear fluid and clear boundary. (b, c) Septal cyst with clear fluid and clear septum; (d) An ovarian hemorrhagic cyst with a reticular septum, which disappeared after 3 months. (e) Solid echonic protuberance grows into the inner wall of the cyst
Ovarian solid tumor. (a) Sonogram shows a homogenic solid mass in the pelvic cavity, with similar echoic characteristics to uterine fibroma. Ovarian fibroma is confirmed by operation. (b, c) A 21-year-old patient represented with an abdominal mass. The ultrasonography revealed an irregular solid mass in the pelvic cavity, 9.0 cm in diameter, with a small amount of fluid area in the mass. It is diagnosed as an endodermal sinus tumor by the operation and pathology
Ovarian teratoma (V). (a, b) The mass is mainly cystic, with solid nodule protruding into the cystic cavity on the inner wall of the cyst. (c) A 52-year-old patient represented abdominal enlargement for half a year. Sonogram shows a huge cystic mass with multiple mobile spherical echogenic structures floating in the cystic fluid. A giant mature teratoma is confirmed by operation. (d) A complex echogenic cystic mass with septum
Ovarian malignant tumors (II). (a) A 68-year-old patient with a postmenopausal period of 18 years. The ultrasonic images show an atrophic uterus. A cystic domained mixtured echogenic mass with a diameter of 10.0 cm is shown in the right adnexa area, accompanied by ascites. (b, c) Ultrasonic shows irregular solid echoes on the inner wall of the cystic mass, protruding into the cystic cavity. (d) Sonogram shows an irregular and heterogeneous mixed mass in the bilateral adnexa areas, without an obvious capsule
Ovarian malignant tumors (III). (a, b) A 62-year-old patient with a postmenopausal period of 8 years, represented with abdominal distention. Ultrasonography reveals a large amount of ascites in pelvic and abdominal cavity with an atrophic uterine, with an irregular solid mass measured 4.0 cm × 3.7 cm × 3.2 cm in the right adnexa area. Color Doppler shows inside blood flow
Ovarian malignant tumors (IV). A 29-year-old patient represented abdominal distension for 3 months 1+ years after the operation of gastric cancer. (a) Ultrasonic scanning shows a normal-sized uterus with an intrauterine device, and a large amount of unclear ascites in the pelvic and abdominal cavity. (b, c) Irregular solid masses are found in bilateral adnexa areas, with a small fluid sonolucent area. (d, e) Color Doppler shows rich blood flow in bilateral masses, with RI = 0.37. (f) Uneven thickened pelvic peritoneum is shown
Adnexal inflammatory mass (I). (a, b) Ultrasonography shows the right adnexal septate cystic mass with irregular shape and abdominal pain. (a) Reexamination of the same patient shows the mass significantly reduced after 1 month of treatment. (b, c, d) Ultrasonic image shows strip and flocculent echo in bilateral adnexal cystic masses with thick and rough boundary. (c) Reexamination of the same patient shows shrunk cystic masses after 3-month treatment
Pyosalpinx. (a) A 53-year-old patient represented lower quadrant pain for 10+ days, accompanied with conscious of fever and chills. The coronal image of the left fallopian tube shows dilated fallopian tube with a liquid area and flocculent echoes inside. (b) A 33-year-old patient represented with lower abdominal pain for 1+ month. The coronal scanning of the left fallopian tube shows “flask-like” change with hypoechoic materials inside. Both patients recovered after the salpingectomy
Pelvic abscess. (a) A 34-year-old patient represented lower abdominal pain half a year after an operation because of pelvic abscess. The ultrasonography shows a hypoechoic mass located in the posterior and right of the uterus, 8.0 cm in diameter, with tiny and short linear echoes inside. (b) A 42-year-old patient represented lower abdomen pain and fever for 1+ month. The ultrasonic scanning shows irregular weak echo mass in bilateral adnexal areas and an abscess is proved by operation
Recurrence of myoma after operation. (a, b) Myomectomy was carried out before. Ultrasonic reexamination shows in homogeneous myometrium, with multiple small myomas. (c) Subtotal hysterectomy was carried out because of myoma 5 years before. Routine ultrasonic following up shows a myoma on the top of the residual cervix
Recurrence of ovarian cancer. (a) A patient is followed up by ultrasonography for 1 year after the operation of ovarian cancer. Heterogeneous and irregular hypoechoic solid mass is visible in the pelvis, with a diameter of about 5.0 cm, accompanied by ascites in the intestines. (b) A patient undergoes ultrasonography 2 years after the operation for ovarian cancer. Hypoechoic solid mass is found in the pelvis with a diameter of 2.6 cm, and the serum CA125 is significantly increased
Lymphocyst after tumor surgery. (a) Four months after the operation of cervical cancer, the patient represented lower abdominal pain. Ultrasonic scanning shows cystic echoes in bilateral ilium fossa, with a diameter of 2.5 cm and 1.8 cm, respectively. (b) TAS shows a cystic mass with a diameter of 4.7 cm in the right ilium fossa, with a thin wall and clear fluid inside
Suggested Reading
Van T, Van D. Ultrasound diagnosis of endometriosis and adenomyosis: state of the art. Best Pract Res Clin Obstet Gynaecol. 2018;8(16–24):16–24.
Andres MP, Borrelli GM, Ribeiro J, et al. Transvaginal ultrasound for the diagnosis of Adenomyosis: systematic review and meta-analysis. J Minim Invasive Gynecol. 2017;25(2):635–40.
Chen J, Chen W, Zhang L, et al. Safety of ultrasound-guided ultrasound ablation for uterine fibroids and Adenomyosis: a review of 9988 cases[J]. Ultrason Sonochem. 2015;27:671–6.
Brindha D, Kandaswamy A, Lakshmideepika C. Digital image analysis of uterine ultrasound for classification of uterine Myoma and Adenomyoma. J Med Imaging & Health Informatics. 2015;5(8):1603–6.
Perrot D, Fernandez H, Levaillant JM, et al. Quality assessment of pelvic ultrasound for uterine myoma according to the CNGOF guidelines[J]. J Gynecol Obstetrics Human Reproduction. 2017;S2468784717300326
Rizzo S, Femia M, Buscarino V, et al. Endometrial cancer: an overview of novelties in treatment and related imaging key points for local staging. Cancer Imaging. 2018 Dec 04;18(1):45.
Lin MY, Dobrotwir A, McNally O, et al. Role of imaging in the routine management of endometrial cancer. Int J Gynaecol Obstet. 2018 Oct;143(Suppl 2):109–17.
Hefler L, Lafleur J, Kickmaier S, et al. Risk of endometrial cancer in asymptomatic postmenopausal patients with thickened endometrium: data from the FAME-Endo study: an observational register study. Arch Gynecol Obstet. 2018;298(4):813–20.
Skaznik-Wikiel ME, Jelovsek JE, et al. Accuracy of endometrial thickness in detecting benign endometrial pathology in postmenopausal women. Menopause. 2010;17(1):104–8.
Cogendez E, Eken MK, Bakal N, et al. The role of transvaginal power Doppler ultrasound in the differential diagnosis of benign intrauterine focal lesions. J Med Ultrason (2001). 2015 Oct;42(4):533–40.
Wong M, Crnobrnja B, Liberale V, et al. The natural history of endometrial polyps. Hum Reprod. 2017;32(2):340–5.
Bittencourt CA, Dos Santos SR, Bernardo WM, et al. Accuracy of saline contrast sonohysterography in detection of endometrial polyps and submucosal leiomyomas in women of reproductive age with abnormal uterine bleeding: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017 Jul;50(1):32–9.
Sahdev A. Cervical tumors. Semin Ultrasound CT MR. 2010 Oct;31(5):399–413.
Comparetto C, Borruto F. Cervical cancer screening: a never-ending developing program. World J Clin Cases. 2015 Jul 16;3(7):614–24.
Park GE, Rha SE. Ultrasonographic findings of low-grade endometrial stromal sarcoma of the uterus with a focus on cystic degeneration. Ultrasonography. 2016 Apr;35(2):124–30.
Alcázar JL. Extragenital endometrial stromal sarcoma arising in endometriosis. Gynecol Obstet lnvest. 2012;73(4):265–71.
Lin LH. Is Doppler ultrasound useful for evaluating gestational trophoblastic disease? Clinics (Sao Paulo). 2015 Dec;70(12):810–5.
Asmar FTC. Uterine artery Doppler flow velocimetry parameters for predicting gestational trophoblastic neoplasia after complete hydatidiform mole, a prospective cohort study. Clinics (Sao Paulo). 2017 May;72(5):284–8.
Antonini F, Laterza L, Fuccio L, Macarri G. Gastric metastasis from ovarian adenocarcinoma presenting as a subepithelial tumor and diagnosed by endoscopic ultrasound-guided tissue acquisition. World J Gastrointest Oncol. 2017 Nov 15;9(11):452–6.
Hong LUO, Tai-zhu YANG, Fan YANG, et al. The value of transvaginal color Doppler ultrasonography in the diagnosis of endometrial polyps. West China Med J. 2011;26(3):410–2.
Jiao CHEN, Tai-zhu YANG, Fan YANG, et al. Ultrasonic manifestations of uterine endometrial stromal sarcoma. Chin J Imaging Technol. 2014;30(4):600–2.
Xin CHEN, Bo ZHANG, Tai-zhu YANG, et al. Research on the diagnostic value of ultrasonography in examining oblique vaginal septum syndrome. West China Med J. 2011;26(11):1684–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Chemical Industry Press
About this chapter
Cite this chapter
Yang, T., Tang, Y., He, M., Xu, H., Tian, Y. (2022). Application of Diagnostic Ultrasound in Gynecology. In: Yang, T., Luo, H. (eds) Practical Ultrasonography in Obstetrics and Gynecology. Springer, Singapore. https://doi.org/10.1007/978-981-16-4477-1_5
Download citation
DOI: https://doi.org/10.1007/978-981-16-4477-1_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-4476-4
Online ISBN: 978-981-16-4477-1
eBook Packages: MedicineMedicine (R0)