Abstract
Coronary microvascular dysfunction (CMD) has been implicated in a wide spectrum of cardiovascular disease. The underlying mechanisms of CMD appear to be heterogeneous, including several structural and functional alterations. Among them, central to coronary vasomotion abnormalities are threefold: enhanced coronary vasoconstrictive reactivity (i.e. coronary spasm) at epicardial and microvascular levels, reduced endothelium-dependent and -independent coronary vasodilator capacity, and increased coronary microvascular resistance, all of which can cause myocardial ischemia due to CMD and often coexist in various combinations even in the absence of obstructive coronary artery disease. The endothelium plays essential roles in modulating vascular tone by synthesizing and releasing endothelium-derived relaxing factors, including vasodilator prostaglandins, nitric oxide (NO), and endothelium-dependent hyperpolarization (EDH) factors in a distinct vessel size–dependent manner; NO mainly mediates vasodilatation of relatively large, conduit vessels (e.g. epicardial coronary arteries), while EDH factors in small resistance vessels (e.g. coronary microvessels). Endothelium-derived hydrogen peroxide (H2O2) is a physiological signaling molecule serving as one of the major EDH factors especially in coronary microcirculation and has gained increasing attention in view of its emerging relevance for cardiovascular disease. In this chapter, we will briefly summarize the latest knowledge on the pathophysiology of CMD with a special reference to endothelial modulation of vascular tone mediated by H2O2/EDH factor and coronary microvascular spasm, in addition to discussing clinical implications of and therapeutic approaches to CMD in cardiovascular disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Coronary microvascular dysfunction
- Endothelial function
- Endothelium-dependent hyperpolarization
- Nitric oxide
- Hydrogen peroxide
1 Introduction
A growing body of evidence has demonstrated that coronary microvascular dysfunction (CMD) plays important roles in the pathophysiology of cardiac ischemia in patients with a wide spectrum of cardiovascular disorders, including ischemic heart disease (IHD) [1, 2], aortic stenosis [3], and heart failure with preserved ejection fraction (HFpEF) [4,5,6]. More than 50% of patients undergoing invasive coronary angiography for the evaluation of suspected obstructive coronary artery disease (CAD) have no significant coronary artery stenosis [7], where the role of CMD has been recognized as an alternative mechanism for symptoms and signs of myocardial ischemia. Indeed, recent studies using comprehensive assessment of coronary physiology by multimodality protocols have unveiled that a substantial proportion of patients with ischemia and no obstructive coronary artery disease (INOCA) differ in the underlying coronary microvascular physiology [8,9,10,11]. Mechanistically, structural and functional abnormalities of “epicardial” coronary arteries in patients with IHD are the focus of previous studies; however, those of coronary microvasculature, referred to as CMD, have attracted much attention in view of their unexpectedly high prevalence in and significant prognostic impact on this population in many clinical settings [12,13,14]. The etiologies of CMD appear to be heterogeneous; several structural (e.g. luminal obstruction, vascular remodeling, vascular rarefaction, and extramural compression) and functional alterations (e.g. endothelial dysfunction, vascular smooth muscle cells [VSMC] dysfunction, and microvascular spasm) have been proposed for the pathophysiological mechanisms of CMD [15,16,17,18,19]. Among them, central to coronary vasomotion abnormalities [1, 20] are enhanced coronary vasoconstrictive reactivity (i.e. coronary spasm) not only at epicardial but also at microvascular levels, reduced endothelium-dependent and -independent coronary vasodilator capacity (e.g. coronary flow reserve [CFR] <2.0), and increased coronary microvascular resistance (e.g. index of microvascular resistance [IMR] >25), all of which can cause myocardial ischemia due to CMD even in the absence of obstructive CAD and often coexist in various combinations in patients with angina and non-obstructive CAD [8, 10, 11].
In this chapter, we will briefly summarize the current knowledge on the pathophysiology of CMD with a special reference to endothelial modulation of vascular tone and coronary microvascular spasm, in addition to briefly discussing clinical implications of and therapeutic approaches to CMD in cardiovascular disease. Further discussions on the coronary microcirculation physiology are available elsewhere [15,16,17,18,19, 21, 22].
2 Endothelial Modulation of Vascular Tone: NO and EDH Factors
2.1 Vessel Size–Dependent Contribution of Endothelium-Derived Relaxing Factors
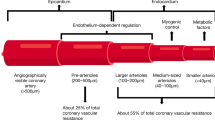
The endothelium plays pivotal roles in modulating the tone of underlying VSMC by synthesizing and releasing endothelium-derived relaxing factors (EDRFs) in an autocrine and paracrine manner, including vasodilator prostaglandins (PGs) (e.g. prostacyclin), nitric oxide (NO), and endothelium-dependent hyperpolarization (EDH) factors, as well as endothelium-derived contracting factors [1, 23, 24] (Fig. 6.1). Endothelial dysfunction is characterized by reduced production and/or action of EDRFs, serving as the hallmark of atherosclerotic cardiovascular diseases as well as one of the major pathogenetic mechanisms of CMD [15,16,17,18]. Of note is that these EDRFs regulate vascular tone in a distinct vessel size–dependent fashion [25, 26] (Fig. 6.1); endothelium-derived NO mainly mediates vasodilatation of relatively large, conduit vessels (e.g. epicardial coronary arteries), while EDH factors-mediated responses are the predominant mechanisms of endothelium-dependent vasodilatation of resistance arteries (e.g. coronary microvessels). By contrast, vasodilator PGs play a small but constant role in general, independent of vessel size. This vessel-size-dependent contribution of NO and EDH factors in endothelium-dependent vasodilatation is well preserved from rodents to humans, shaping a physiological balance between them [1, 23]. Thus, EDH factors-mediated vasodilatation is a vital mechanism especially in microcirculations, where blood pressure and organ perfusion are critically determined. Moreover, such redundant mechanisms in endothelium-dependent vasodilatations are advantageous for ensuring proper maintenance of vascular tone under pathological conditions, where one of EDRFs-mediated responses is impaired, favoring a vasoconstrictor and proinflammatory state. Indeed, in various pathological conditions with atherosclerotic risk factors, NO-mediated relaxations are easily compromised, while EDH factors-mediated responses are fairly preserved or even enhanced to serve as a compensatory vasodilator system [26, 27]. Multiple mechanisms are involved in the enhanced EDH factors-mediated responses in small resistance vessels, including negative interactions between NO and several EDH factors, as discussed later. The regulatory mechanisms of NO-mediated responses are extensively reviewed elsewhere [28,29,30].
Vessel size–dependent contribution of endothelium-derived relaxing factors and Rho-kinase-mediated vascular smooth muscle hypercontraction. cGMP cyclic guanosine monophosphate, EDH endothelium-dependent hyperpolarization, NO nitric oxide, PGs prostaglandins. (Reproduced from Shimokawa and Godo [24])
2.2 EDH Factors: The Predominant Mechanism of Vasodilatation in Small Arteries
In 1998, Feletou and Vanhoutte [31] and Chen et al. [32] independently demonstrated the existence of endothelium-derived non-NO, non-prostanoid relaxing factors, unforeseen EDH factors. EDH factors-mediated responses are the major mechanism of endothelium-dependent vasodilatations in resistance arteries, although, by definition, the contribution of EDH factors is determined only after the blockade of both vasodilator PGs and NO. EDH factors cause hyperpolarization and subsequent relaxation of underlying VSMC with resultant vasodilatation of small resistance vessels and thus finely regulate blood pressure and organ perfusion instantaneously in response to diverse physiological demands [23, 33]. The nature of EDH factors varies depending on the vascular bed, vessel size, and species of interest, including epoxyeicosatrienoic acids (EETs), metabolites of arachidonic P450 epoxygenase pathway [34, 35], electrical communication through gap junctions [36], K+ ions [37], and as we demonstrated, endothelium-derived hydrogen peroxide (H2O2) [24, 38] (Fig. 6.2). EETs mainly participate in EDH-mediated relaxations in bovine [34], porcine [35], and human coronary arteries [39]; K+ ions in rat hepatic and mesenteric arteries [37, 40], porcine [41] and bovine [42] coronary arteries, and human kidney interlobar arteries [43]; and H2O2, at physiologically low concentrations, in human [44], porcine [45], and canine coronary arteries [46,47,48].
Molecular mechanisms of endothelial modulation of vascular tone. AMPKα1 α1-subunit of AMP-activated protein kinase, CaM calmodulin, CaMKKβ Ca2+/CaM-dependent protein kinase β, cAMP cyclic AMP, cGMP cyclic GMP, COX cyclooxygenase, EETs epoxyeicosatrienoic acids, eNOS endothelial NO synthase, EOX epoxygenase, HETEs hydroxyeicosatetraenoic acids, H2O2 hydrogen peroxide, IP3 inositol trisphosphate, I/R ischemia-reperfusion injury, KCa calcium-activated potassium channel, KIR inwardly rectifying potassium channel, LOX lipoxygenase, LTs leukotrienes, NO nitric oxide, ONOO− peroxynitrite, PGI2 prostacyclin, PKG1α 1α-subunit of protein kinase G, PLA2 phospholipase A2, PLC phospholipase C, SOD superoxide dismutase. (Reproduced from Shimokawa and Godo [24])
Coronary vascular resistance is predominantly determined by the pre-arterioles (>100 μm in diameter) and arterioles (<100 μm) where EDH factors-mediated responses become more prominent than NO-mediated relaxations. Given that H2O2 has potent vasodilator properties in coronary resistance vessels, impaired H2O2-mediated vasodilatation may lead to CMD. In the next section, we will focus on endothelium-derived H2O2 as an EDH factor in detail. Readers are encouraged to refer to an excellent textbook for more comprehensive information on the role of other EDH factors [49].
3 Endothelium-Derived H2O2 as an EDH Factor
3.1 Identification of H2O2/EDH Factor
Reactive oxygen species (ROS) have been considered to be primarily harmful because of their detrimental property to cells and tissues and pathological implications in various cardiovascular diseases including CMD [50]. However, as exemplified by endothelium-derived H2O2/EDH factor, many studies have demonstrated that physiological levels of ROS can serve as crucial signaling molecules in health and disease [51] and have acknowledged H2O2 as a physiological signaling molecule, regulating blood pressure [52], metabolic functions [53, 54], and coronary microcirculation [46,47,48].
Following the original reports on the existence of EDH factors in 1988 [31, 32], we hypothesized that a putative EDH factor might be a non-NO vasodilator substance (likely ROS) derived from endothelial NO synthases (NOSs) system, based on a hint from several early observations and notions. First, both NO-mediated and EDH-mediated responses are susceptible to vascular injuries caused by atherosclerotic risk factors, and inversely, the treatment of those risk factors can restore both responses [1, 26]. Second, it had been previously demonstrated that endothelium-derived free radicals exert endothelium-dependent vasodilator and vasoconstrictor effects in canine coronary arteries [55]. Third, both endothelial NOS (eNOS)-derived NO generation and EDH-mediated responses are dependent on calcium/calmodulin [56]. Fourth, a simple molecule (like NO), rather than complex substances, may be opportune for modulating vascular tone instantaneously in response to various physiological demands in the body. On the basis of these notions, in 2000, we demonstrated for the first time that endothelium-derived H2O2 is an EDH factor in mouse mesenteric arteries; EDH-mediated hyperpolarizations and relaxations of underlying VSMC were inhibited by catalase, a specific H2O2 inhibitor, in small mesenteric arteries from wild-type mice and were significantly reduced in eNOS-knockout (KO) mice [38]. This was also true for other vascular beds, including human mesenteric [57] and coronary [58] arteries, porcine [45] and canine [46,47,48] coronary arteries, and piglet pial arterioles [59]. Notably, the estimated concentrations of endothelium-derived H2O2/EDH factor are in micromolar order (<50 μmol/L) [45, 47], which are much lower concentrations than those observed in various pathological conditions [60]. When applied in organ chamber experiments, approximately 10–100 μmol/L of exogenous H2O2 elicits vasodilatation of human coronary arterioles [58, 61] and mouse small mesenteric arteries [38, 62, 63], while higher concentrations of H2O2 rather induce vasoconstriction by releasing cyclooxygenase-derived thromboxane [64]. Here, only 10–15% of H2O2 applied exogenously reaches the intracellular targets due to endogenous antioxidants and membrane impedance [65].
3.2 Source of H2O2/EDH Factor
Endothelium-derived H2O2 is mainly produced by the dismutation of superoxide anions derived from various sources in the endothelium, including NADPH oxidase, mitochondrial electron transport chain, xanthine oxidase, lipoxygenase, and NOSs (Fig. 6.2) [60]. Importantly, superoxide anions relevant to H2O2/EDH factor are not derived from pathologically uncoupled eNOS because H2O2-mediated EDH-type responses are not cancelled by NOS inhibitors (i.e. L-arginine analogs) and upregulation of eNOS co-factor tetrahydrobiopterin has no effects on the responses [66]. eNOS produces superoxide anions under physiological conditions when synthesizing NO from L-arginine and oxygen, while Cu,Zn-SOD dismutates those superoxide anions into H2O2. Cu,Zn-SOD-KO mice show markedly impaired EDH-mediated hyperpolarizations and relaxations in mesenteric arteries and coronary circulation without VSMC dysfunction [67]. Other sources of superoxide anions in H2O2-mediated vasodilatation have been identified in human coronary arterioles, including mitochondrial respiratory chain in flow-mediated dilatation [68] and NADPH oxidase in bradykinin-induced relaxation [69].
3.3 Regulatory Mechanisms of Physiologically Relevant H2O2
Recent studies have provided potential regulatory mechanisms underlying the physiologically relevant H2O2 in the endothelium [51]. It is important to note that local subcellular concentrations at microdomains, rather than net cellular concentrations, may be critical to determine whether the effects of ROS can be detrimental or beneficial for cellular signaling and that co-localization of the source and target of H2O2 may help to avoid non-specific harmful oxidations [70, 71]. In addition, specific cysteine residues, such as peroxiredoxins, can function as a redox-dependent molecular switch to regulate ROS-mediated signaling [60]. Moreover, a novel mechanism of CMD in human CAD has been proposed [22, 72, 73]. As mentioned above, healthy human coronary circulation is regulated by NO and low physiological levels of H2O2/EDH factor. However, various atherosclerotic risk factors (e.g. aging, hypertension, obesity, and smoking) can cause a switch from NO to H2O2 in the mediator of endothelium-dependent vasodilatation in human coronary arteries. The resultant impaired production of NO and pathologically elevated levels of H2O2 manifest as CMD that favors a vasoconstrictor and pro-inflammatory state, leading to the development of coronary atherosclerosis [22, 72, 73].
3.4 Mode of Action of H2O2/EDH Factor
Among several modes of action of H2O2/EDH factor [74, 75], oxidative modification of cGMP-dependent protein kinase (PKG) plays a central role in H2O2-induced hyperpolarization and relaxation of underlying VSMC [52, 76] (Fig. 6.2). Briefly, H2O2 induces dimerization of 1α-isoforms of PKG (PKG1α) through an interprotein disulfide bond formation between them to enhance the kinase activity through phosphorylation. The activated PKG1α subsequently stimulates K+ channels with resultant hyperpolarization and vasodilatation in mouse mesenteric arteries [52] and human coronary arterioles [58, 61]. H2O2 also promotes the translocation of PKG1α from cytoplasm to membrane in human [61] and porcine [77] coronary arteries. Such reversible post-translational modification, like phosphorylation, is advantageous for the fine control of vascular tone in response to various demand fluctuation in vivo [30].
3.5 Clinical Significance of H2O2/EDH Factor
The oxidant-mediated signaling by H2O2 is of clinical importance because it is associated with blood pressure control in vivo [52]. Pharmacological inhibition of catalase decreases arterial blood pressure in association with enhanced PKG1α dimerization in vivo [77]. Moreover, the ‘redox-dead’ knock-in mice of Cys42Ser PKG1α, whose mutant PKG1α is unable to be activated by H2O2-induced dimerization because of the deletion in its redox-sensitive sulfur, exhibit markedly impaired EDH-mediated hyperpolarization and relaxation in resistance arteries ex vivo associated with systemic arterial hypertension [52]. Furthermore, physiological levels of H2O2 have potent vasodilator properties in coronary resistance vessels, contributing to coronary autoregulation [46], cardioprotection against myocardial ischemia-reperfusion injury [47], and tachycardia-induced metabolic coronary vasodilatations [48] in dogs in vivo. Given that coronary vascular resistance is predominantly determined by the prearterioles and arterioles [17] where the effect of EDH-mediated responses on vascular tone is superior to that of NO-mediated relaxations, it is important to maintain the vessel size–dependent contribution of NO and EDH factors for the treatment of CMD. Taken together, endothelium-derived H2O2 functions as an important endogenous second messenger at its physiological low concentrations to elicit EDH-meditated vasodilatation and to maintain vascular homeostasis in the coronary circulation [23, 74]. In the clinical settings, it has been repeatedly reported that the effects of chronic nitrate therapy are neutral or even harmful in patients with cardiovascular diseases [78,79,80,81,82] and that antioxidant treatments are disappointingly ineffective to prevent cardiovascular events [83]. These lines of evidence suggest the importance of the physiological balance between NO and H2O2/EDH factor in maintaining cardiovascular homeostasis and in curing diseases associated with endothelial dysfunction.
4 Mechanisms of Enhanced H2O2/EDH Factor in Microcirculation
4.1 Diverse Roles of Endothelial NOSs System
Endothelium-derived NO and EDH factors share the roles in modulating vascular tone in a distinct vessel size–dependent manner through the diverse roles of endothelial NOSs system (Fig. 6.2). In large conduit vessels, NOSs mainly act as a NO-generating system to cause soluble guanylate cyclase (sGC)-cyclic guanosine monophosphate (cGMP)-mediated vasodilatation, whereas in small resistance vessels, they serve as a superoxide-generating system to evoke H2O2/EDH factor-mediated responses [84]. Among three NOS isoforms (neural NOS [nNOS, NOS1], inducible NOS [iNOS, NOS2], and eNOS, NOS3) expressed in the cardiovascular system, eNOS is the dominant isoform in blood vessels [85] and the most important isoform in generating H2O2/EDH factor in the endothelium [86]. As mentioned above, genetic ablation of eNOS in mice results in impaired EDH-mediated vasodilatation associated with systemic hypertension [87]. Using singly-eNOS-KO, doubly-n/eNOS-KO, and triply-n/i/eNOS-KO mice, we have previously demonstrated that EDH-mediated relaxations are progressively reduced in accordance with the number of NOS genes ablated [84]. As compared with wild-type mice, H2O2-mediated EDH-type relaxations of small mesenteric arteries are reduced approximately by half in singly-eNOS-KO mice, further diminished in doubly-n/eNOS-KO mice, and are finally absent in triply-n/i/eNOS-KO mice without underlying VSMC dysfunction [84]. The remaining EDH-mediated relaxation of small mesenteric arteries in eNOS-KO mice is still sensitive to catalase [38]. Collectively, these results indicate that three NOSs isoforms compensate each other to maintain H2O2-mediated EDH-type relaxations.
4.2 Mechanisms for H2O2/EDH Factor Dominance in Coronary Microcirculation
Accumulating evidence has provided mechanistic insights into vessel size–dependent contribution of NO and H2O2/EDH factor in coronary microcirculation. Pretreatment with NO donors attenuates EDH-mediated vasodilatation in porcine coronary arteries in vitro [88] and canine coronary microcirculation in vivo [89] and NO exerts a negative-feedback effect on endothelium-dependent vasodilatation through cGMP-mediated desensitization in canine coronary arteries ex vivo [90]. Mechanistically, cGMP-dependent activation of PKG desensitizes VSMC to H2O2 by inhibiting H2O2-induced PKG1α dimerization, a central mechanism of H2O2/EDH factor-mediated vasodilatation, and conversely, pharmacological inhibition of sGC sensitizes conduit vessels, but not resistance vessels, to H2O2-induced vasodilatation in mice [91]. In addition, mouse resistance vessels have less NO production and less antioxidant capacity, predisposing PKG1α to be more sensitive to H2O2-induced activation [91]. Other key players for enhanced H2O2/EDH factor-mediated vasodilatation in coronary microcirculation include endothelial caveolin-1, a negative regulator of eNOS [62, 92], and α1-subunit of endothelial AMP-activated protein kinase [93]. Taken together, these mechanisms are compatible with the widely held view that EDH-mediated responses function as a compensatory vasodilator system when NO-mediated relaxations are compromised. It is important to maintain the vessel size–dependent contribution of NO and EDH factors because excessive endothelial NO production by either caveolin-1 deficiency or eNOS overexpression disrupts the physiological balance between NO and EDH factors in endothelium-dependent vasodilatation, compromising coronary flow reserve in mice in vivo [63, 92].
5 Coronary Microvascular Spasm
Besides endothelial dysfunction, CMD can be caused by endothelium-independent mechanisms in general, which encompass impaired coronary microvascular dilatation and enhanced coronary microvascular constriction. Coronary artery spasms at both epicardial and microvascular levels have been implicated in a wide variety of IHD [1]. Mechanistically, Rho-kinase-induced myosin light chain phosphorylation with resultant VSMC hypercontraction is the central mechanism in the pathogenesis of coronary artery spasm at epicardial [94, 95] as well as at microvascular [96] levels, whereas the role of endothelial dysfunction may be minimal (Fig. 6.1) [1, 20]. Intracoronary administration of a Rho-kinase inhibitor, fasudil, is effective not only for relieving refractory coronary spasm resistant to nitrates or calcium-channel blockers but also for suppressing coronary microvascular spasm in most patients with the disorder [97]. In addition, enhanced epicardial and coronary microvascular spasms are associated with increased production of other vasoconstrictive mediators, such as endothelin [98] and serotonin [99] in patients with CMD.
Intracoronary acetylcholine (ACh) provocation test is useful in inducing coronary artery spasm with high sensitivity and specificity in the cardiac catheter laboratory [100]. A high prevalence of ACh-induced coronary microvascular spasm has been reported in one-third of patients with stable chest pain and non-obstructive CAD [101, 102]. The Coronary Vasomotion Disorders International Study (COVADIS) Group proposed a consensus set of standardized diagnostic criteria for microvascular angina attributable to CMD, including ACh-induced coronary microvascular spasm [103]. The diagnostic value of these criteria has been demonstrated by a recent randomized clinical trial [104]. More recently, we have demonstrated that increased coronary microvascular resistance as evaluated by IMR is associated with Rho-kinase activation in the pathogenesis of coronary functional abnormalities [11]. Considering that patients with coronary artery spasm are not necessarily associated with conventional coronary risk factors and positive results of non-invasive functional stress tests, comprehensive assessment of coronary physiology using multimodality protocol is of diagnostic value to identify coronary vasomotion abnormalities and to avoid false reassurance in patients with INOCA [10, 11, 100].
6 Clinical Implications
6.1 Importance of Endothelial Function Tests
Assessment of endothelial function has been acknowledged as an excellent surrogate marker of future cardiovascular events in many clinical settings [105], although it is challenging to specifically assess EDH factors-mediated responses in humans in vivo. The reason for this difficulty is at least twofold: (1) the contribution of EDH factors could be determined only after the blockade of both vasodilator PGs and NO and (2) coronary resistance arteries are not visible on coronary angiography. Endothelial dysfunction is manifested as impaired production and/or action of EDRFs. EDH factors-mediated vasodilation can be temporarily enhanced to compensate for impaired NO-mediated responses in the early stage of atherosclerotic conditions [33, 74]. However, after prolonged exposure to atherosclerotic risk factors, this compensatory role of EDH factors-mediated responses is finally disrupted to cause metabolic disturbance [106]. Endothelial dysfunction, as evaluated by impaired flow-mediated dilation (FMD) of the brachial artery or digital reactive hyperemia index (RHI) in peripheral arterial tonometry, is associated with future cardiovascular events in patients with CAD and one standard deviation decrease in FMD or RHI is associated with doubling of cardiovascular event risk [105]. More recently, peripheral endothelial dysfunction has been shown to be common in patients with coronary vasomotion abnormalities [107, 108].
6.2 Role of H2O2/EDH Factor in the Pathophysiology of Coronary Artery Disease
Previous studies focused on structural and functional abnormalities of “epicardial” coronary arteries in patients with CAD because they are easily visible on coronary angiography and amenable to procedural intervention (e.g. percutaneous coronary intervention). However, those of coronary microvasculature, referred to as CMD, have gained increasing attention as a novel research target in this population [12,13,14]. It is conceivable that impaired H2O2/EDH factor-mediated vasodilatation is involved in the pathogenesis of CMD in light of its potent vasodilator properties in coronary resistance vessels where EDH factors-mediated responses become relatively dominant to NO-mediated relaxations. A good example of this is that CMD caused by impaired H2O2/EDH factor is also associated with cardiac diastolic dysfunction in eNOS-KO mice [109]. Thus, it is essential to maintain the physiological balance between NO and H2O2/EDH factor for the treatment of CAD, which notion is supported by the fact that significant negative interactions exist between NO and several EDH factors [63, 88,89,90,91] and that nitrates as NO donors are not beneficial for the treatment of CMD [78, 80]. More recently, it has been highlighted that endothelium-dependent CMD is associated with low endothelial shear stress, larger plaque burden, and vulnerable plaque characteristic beyond conventional coronary risk factors in angina patients with INOCA [110, 111]. Shear stress is one of the important physiological cues that make endothelial cells synthesize and release EDRFs to maintain vascular homeostasis, while altered oscillatory or low shear stress with disturbed flow on coronary artery wall is implicated in the local progression of atherosclerotic coronary plaque through endothelial and VSMC proliferation, inflammation, lipoprotein uptake, and leukocyte adhesion [110, 111]. Indeed, altered shear stress on the coronary artery wall has been implicated in the local progression of atherosclerotic coronary plaque [112].
6.3 Lessons from Clinical Trials Targeting NO: Less Is More?
Although the role of CMD has been implicated in patients with obstructive CAD who underwent successful revascularization [113], the effects of isosorbide-5-mononitrate were unexpectedly neutral in patients with residual microvascular ischemia despite successful percutaneous coronary intervention [82]. Moreover, recent studies highlighted the high prevalence and pathophysiological relevance of CMD in patients with HFpEF [4,5,6]. Contrary to the premise that enhancing NO-mediated vasodilatation could exert beneficial effects on patients with HFpEF, the results of systemic and long-term administrations of inorganic nitrite in those patients were neutral or even harmful in randomized clinical trials [79, 81]. Similarly, antioxidant therapies for patients with cardiovascular diseases had no benefits [83], although multiple mechanisms may be involved in so-called “antioxidant paradox” in clinical trials, including inadequate dose, short treatment duration, and pro-oxidant effects of antioxidants upon supplementation. These lines of evidence indicate that it is important to turn our attention to avoid excessive NO supplementation and to pay attention to the potential harm of non-specific elimination of ROS by antioxidants. An alternative explanation for such “paradox” of NO-targeted therapy may be nitrosative stress induced by an excessive amount of supplemental NO [92, 114], again suggesting the importance of physiological balance between NO and EDH factors in endothelium-dependent vasodilatation. Although standard medications used for the treatment of cardiovascular diseases share the pleiotropic effects on endothelial function by enhancing NO-mediated vasodilatation with modest antioxidant capacities, including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and statins, further research is warranted to address how to modulate CMD to improve clinical outcomes of patients with cardiovascular diseases.
6.4 CMD as Systemic Vascular Dysfunction beyond the Heart
Recent studies have highlighted the importance of CMD with major clinical implications. First, if complicated with CMD, even angina patients who have angiographically normal coronary arteries or non-obstructive CAD are associated with increased future cardiac events, including myocardial infarction, percutaneous or surgical revascularization, cardiac death, and hospitalization for unstable angina [11, 12, 115, 116]. Moreover, the prevalence of CMD in this clinical entity is not negligible [8,9,10,11]. Although contemporary non-invasive stress tests have limited diagnostic accuracy for detecting CMD in patients with chest pain and non-obstructive CAD [9, 117], comprehensive invasive assessment of coronary vasomotor reactivity using intracoronary ACh, adenosine, and other vasoactive agents is safe, feasible, and of diagnostic value to identify patients with CMD [8, 9, 100, 104, 118]. Second, CMD is a cardiac manifestation of the systemic small artery disease [107], which supports the novel concept of “primary coronary microcirculatory dysfunction” [119]. Despite the high prevalence of CMD in patients with INOCA, they are often underestimated and offered no specific treatment or follow-up under the umbrella of “normal” coronary arteries. On the contrary to this otherwise common practice, patients with CMD are predisposed to future coronary events and associated worse outcomes [12, 115, 116]. Furthermore, CMD may be attributable to residual cardiac ischemia even after successful revascularization of significant epicardial coronary stenosis [113]. Identifying CMD in patients with stable IHD may provide physicians with useful information for decision making and risk stratification beyond conventional coronary risk factors.
7 Conclusions
This chapter highlighted the pathophysiology of CMD with emphasis placed on endothelial modulation of vascular tone mediated by H2O2/EDH factor and coronary microvascular spasm. It remains an open question for future research how to improve CMD without affecting the delicate balance between NO and EDH factors. Further characterization and better understanding of CMD are indispensable to this end, which helps us develop novel therapeutic strategies in patients with the disease.
Abbreviations
- CAD:
-
Coronary artery disease
- cGMP:
-
Cyclic guanosine monophosphate
- CMD:
-
Coronary microvascular dysfunction
- EDH:
-
Endothelium-dependent hyperpolarization
- EDRF(s):
-
Endothelium-derived relaxing factor(s)
- EETs:
-
Epoxyeicosatrienoic acids
- eNOS:
-
Endothelial nitric oxide synthase
- H2O2:
-
Hydrogen peroxide
- HFpEF:
-
Heart failure with preserved ejection fraction
- IHD:
-
Ischemic heart disease
- INOCA:
-
Ischemia and no obstructive coronary artery disease
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- PGs:
-
Prostaglandins
- PKG:
-
cGMP-dependent protein kinase
- ROS:
-
Reactive oxygen species
- sGC:
-
Soluble guanylate cyclase
- SOD:
-
Superoxide dismutase
- VSMC:
-
Vascular smooth muscle cells
References
Shimokawa H. 2014 Williams Harvey lecture: importance of coronary vasomotion abnormalities-from bench to bedside. Eur Heart J. 2014;35(45):3180–93. https://doi.org/10.1093/eurheartj/ehu427.
Kaski JC, Crea F, Gersh BJ, Camici PG. Reappraisal of ischemic heart disease. Circulation. 2018;138(14):1463–80. https://doi.org/10.1161/circulationaha.118.031373.
Michail M, Davies JE, Cameron JD, Parker KH, Brown AJ. Pathophysiological coronary and microcirculatory flow alterations in aortic stenosis. Nat Rev Cardiol. 2018;15(7):420–31. https://doi.org/10.1038/s41569-018-0011-2.
Crea F, Bairey Merz CN, Beltrame JF, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Camici PG. The parallel tales of microvascular angina and heart failure with preserved ejection fraction: a paradigm shift. Eur Heart J. 2017;38(7):473–7. https://doi.org/10.1093/eurheartj/ehw461.
Dryer K, Gajjar M, Narang N, Lee M, Paul J, Shah AP, Nathan S, Butler J, Davidson CJ, Fearon WF, Shah SJ, Blair JEA. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am J Physiol Heart Circ Physiol. 2018;314(5):H1033–H42. https://doi.org/10.1152/ajpheart.00680.2017.
Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, Beussink-Nelson L, Fermer ML, Broberg MA, Gan LM, Lund LH. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J. 2018;39(37):3439–50. https://doi.org/10.1093/eurheartj/ehy531.
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, Brindis RG, Douglas PS. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–95. https://doi.org/10.1056/NEJMoa0907272.
Lee BK, Lim HS, Fearon WF, Yong AS, Yamada R, Tanaka S, Lee DP, Yeung AC, Tremmel JA. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131(12):1054–60. https://doi.org/10.1161/circulationaha.114.012636.
Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. J Am Coll Cardiol Intv. 2015;8(11):1445–53. https://doi.org/10.1016/j.jcin.2015.06.017.
Ford TJ, Yii E, Sidik N, Good R, Rocchiccioli P, McEntegart M, Watkins S, Eteiba H, Shaukat A, Lindsay M, Robertson K, Hood S, McGeoch R, McDade R, McCartney P, Corcoran D, Collison D, Rush C, Stanley B, McConnachie A, Sattar N, Touyz RM, Oldroyd KG, Berry C. Ischemia and no obstructive coronary artery disease: prevalence and correlates of coronary vasomotion disorders. Circ Cardiovasc Interv. 2019;12(12):e008126. https://doi.org/10.1161/circinterventions.119.008126.
Suda A, Takahashi J, Hao K, Kikuchi Y, Shindo T, Ikeda S, Sato K, Sugisawa J, Matsumoto Y, Miyata S, Sakata Y, Shimokawa H. Coronary functional abnormalities in patients with angina and nonobstructive coronary artery disease. J Am Coll Cardiol. 2019;74(19):2350–60. https://doi.org/10.1016/j.jacc.2019.08.1056.
Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, Johnson BD, Sopko G, Bairey Merz CN. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s ischemia syndrome evaluation) study. J Am Coll Cardiol. 2010;55(25):2825–32. https://doi.org/10.1016/j.jacc.2010.01.054.
Jespersen L, Hvelplund A, Abildstrom SZ, Pedersen F, Galatius S, Madsen JK, Jorgensen E, Kelbaek H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33(6):734–44. https://doi.org/10.1093/eurheartj/ehr331.
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, Dorbala S, Blankstein R, Rimoldi O, Camici PG, Di Carli MF. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. 2014;129(24):2518–27. https://doi.org/10.1161/circulationaha.113.008507.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356(8):830–40. https://doi.org/10.1056/NEJMra061889.
Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. 2014;35(17):1101–11. https://doi.org/10.1093/eurheartj/eht513.
Crea F, Lanza G, Camici P. Mechanisms of coronary microvascular dysfunction. In: Coronary microvascular dysfunction. Milan: Springer; 2014. p. 31–47.
Camici PG, d'Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015;12(1):48–62. https://doi.org/10.1038/nrcardio.2014.160.
Pries AR, Reglin B. Coronary microcirculatory pathophysiology: can we afford it to remain a black box? Eur Heart J. 2017;38(7):478–88. https://doi.org/10.1093/eurheartj/ehv760.
Shimokawa H. Reactive oxygen species in cardiovascular health and disease: special references to nitric oxide, hydrogen peroxide, and Rho-kinase. J Clin Biochem Nutr. 2020;66(2):83–91. https://doi.org/10.3164/jcbn.19-119.
Gould KL, Johnson NP. Coronary physiology beyond coronary flow reserve in microvascular angina: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72(21):2642–62. https://doi.org/10.1016/j.jacc.2018.07.106.
Gutterman DD, Chabowski DS, Kadlec AO, Durand MJ, Freed JK, Ait-Aissa K, Beyer AM. The human microcirculation: regulation of flow and beyond. Circ Res. 2016;118(1):157–72. https://doi.org/10.1161/circresaha.115.305364.
Vanhoutte PM, Shimokawa H, Feletou M, Tang EH. Endothelial dysfunction and vascular disease -a 30th anniversary update. Acta Physiol. 2017;219(1):22–96. https://doi.org/10.1111/apha.12646.
Shimokawa H, Godo S. Nitric oxide and endothelium-dependent hyperpolarization mediated by hydrogen peroxide in health and disease. Basic Clin Pharmacol Toxicol. 2020;127(2):92–101. https://doi.org/10.1111/bcpt.13377.
Shimokawa H, Yasutake H, Fujii K, Owada MK, Nakaike R, Fukumoto Y, Takayanagi T, Nagao T, Egashira K, Fujishima M, Takeshita A. The importance of the hyperpolarizing mechanism increases as the vessel size decreases in endothelium-dependent relaxations in rat mesenteric circulation. J Cardiovasc Pharmacol. 1996;28(5):703–11. https://doi.org/10.1097/00005344-199611000-00014.
Urakami-Harasawa L, Shimokawa H, Nakashima M, Egashira K, Takeshita A. Importance of endothelium-derived hyperpolarizing factor in human arteries. J Clin Invest. 1997;100(11):2793–9. https://doi.org/10.1172/jci119826.
Ozkor MA, Murrow JR, Rahman AM, Kavtaradze N, Lin J, Manatunga A, Quyyumi AA. Endothelium-derived hyperpolarizing factor determines resting and stimulated forearm vasodilator tone in health and in disease. Circulation. 2011;123(20):2244–53. https://doi.org/10.1161/circulationaha.110.990317.
Vanhoutte PM. How we learned to say NO. Arterioscler Thromb Vasc Biol. 2009;29(8):1156–60. https://doi.org/10.1161/atvbaha.109.190215.
Feletou M, Kohler R, Vanhoutte PM. Nitric oxide: orchestrator of endothelium-dependent responses. Ann Med. 2012;44(7):694–716. https://doi.org/10.3109/07853890.2011.585658.
Vanhoutte PM, Zhao Y, Xu A, Leung SW. Thirty years of saying NO: sources, fate, actions, and misfortunes of the endothelium-derived vasodilator mediator. Circ Res. 2016;119(2):375–96. https://doi.org/10.1161/circresaha.116.306531.
Feletou M, Vanhoutte PM. Endothelium-dependent hyperpolarization of canine coronary smooth muscle. Br J Pharmacol. 1988;93(3):515–24. https://doi.org/10.1111/j.1476-5381.1988.tb10306.x.
Chen G, Suzuki H, Weston AH. Acetylcholine releases endothelium-derived hyperpolarizing factor and EDRF from rat blood vessels. Br J Pharmacol. 1988;95(4):1165–74. https://doi.org/10.1111/j.1476-5381.1988.tb11752.x.
Feletou M, Vanhoutte PM. EDHF: an update. Clin Sci. 2009;117(4):139–55. https://doi.org/10.1042/CS20090096.
Campbell WB, Gebremedhin D, Pratt PF, Harder DR. Identification of epoxyeicosatrienoic acids as endothelium-derived hyperpolarizing factors. Circ Res. 1996;78(3):415–23. https://doi.org/10.1161/01.res.78.3.415.
Fisslthaler B, Popp R, Kiss L, Potente M, Harder DR, Fleming I, Busse R. Cytochrome P450 2C is an EDHF synthase in coronary arteries. Nature. 1999;401(6752):493–7. https://doi.org/10.1038/46816.
Griffith TM, Chaytor AT, Edwards DH. The obligatory link: role of gap junctional communication in endothelium-dependent smooth muscle hyperpolarization. Pharmacol Res. 2004;49(6):551–64. https://doi.org/10.1016/j.phrs.2003.11.014.
Edwards G, Dora KA, Gardener MJ, Garland CJ, Weston AH. K+ is an endothelium-derived hyperpolarizing factor in rat arteries. Nature. 1998;396(6708):269–72. https://doi.org/10.1038/24388.
Matoba T, Shimokawa H, Nakashima M, Hirakawa Y, Mukai Y, Hirano K, Kanaide H, Takeshita A. Hydrogen peroxide is an endothelium-derived hyperpolarizing factor in mice. J Clin Invest. 2000;106(12):1521–30. https://doi.org/10.1172/jci10506.
Miura H, Gutterman DD. Human coronary arteriolar dilation to arachidonic acid depends on cytochrome P-450 monooxygenase and Ca2+-activated K+ channels. Circ Res. 1998;83(5):501–7. https://doi.org/10.1161/01.res.83.5.501.
Dora KA, Garland CJ. Properties of smooth muscle hyperpolarization and relaxation to K+ in the rat isolated mesenteric artery. Am J Physiol Heart Circ Physiol. 2001;280(6):H2424–9. https://doi.org/10.1152/ajpheart.2001.280.6.H2424.
Beny JL, Schaad O. An evaluation of potassium ions as endothelium-derived hyperpolarizing factor in porcine coronary arteries. Br J Pharmacol. 2000;131(5):965–73. https://doi.org/10.1038/sj.bjp.0703658.
Nelli S, Wilson WS, Laidlaw H, Llano A, Middleton S, Price AG, Martin W. Evaluation of potassium ion as the endothelium-derived hyperpolarizing factor (EDHF) in the bovine coronary artery. Br J Pharmacol. 2003;139(5):982–8. https://doi.org/10.1038/sj.bjp.0705329.
Bussemaker E, Popp R, Binder J, Busse R, Fleming I. Characterization of the endothelium-derived hyperpolarizing factor (EDHF) response in the human interlobar artery. Kidney Int. 2003;63(5):1749–55. https://doi.org/10.1046/j.1523-1755.2003.00910.x.
Miura H, Bosnjak JJ, Ning G, Saito T, Miura M, Gutterman DD. Role for hydrogen peroxide in flow-induced dilation of human coronary arterioles. Circ Res. 2003;92(2):e31–40. https://doi.org/10.1161/01.res.0000054200.44505.ab.
Matoba T, Shimokawa H, Morikawa K, Kubota H, Kunihiro I, Urakami-Harasawa L, Mukai Y, Hirakawa Y, Akaike T, Takeshita A. Electron spin resonance detection of hydrogen peroxide as an endothelium-derived hyperpolarizing factor in porcine coronary microvessels. Arterioscler Thromb Vasc Biol. 2003;23(7):1224–30. https://doi.org/10.1161/01.atv.0000078601.79536.6c.
Yada T, Shimokawa H, Hiramatsu O, Kajita T, Shigeto F, Goto M, Ogasawara Y, Kajiya F. Hydrogen peroxide, an endogenous endothelium-derived hyperpolarizing factor, plays an important role in coronary autoregulation in vivo. Circulation. 2003;107(7):1040–5. https://doi.org/10.1161/01.cir.0000050145.25589.65.
Yada T, Shimokawa H, Hiramatsu O, Haruna Y, Morita Y, Kashihara N, Shinozaki Y, Mori H, Goto M, Ogasawara Y, Kajiya F. Cardioprotective role of endogenous hydrogen peroxide during ischemia-reperfusion injury in canine coronary microcirculation in vivo. Am J Physiol Heart Circ Physiol. 2006;291(3):H1138–46. https://doi.org/10.1152/ajpheart.00187.2006.
Yada T, Shimokawa H, Hiramatsu O, Shinozaki Y, Mori H, Goto M, Ogasawara Y, Kajiya F. Important role of endogenous hydrogen peroxide in pacing-induced metabolic coronary vasodilation in dogs in vivo. J Am Coll Cardiol. 2007;50(13):1272–8. https://doi.org/10.1016/j.jacc.2007.05.039.
Feletou M. The endothelium: part 2: EDHF-mediated responses “the classical pathway”. San Rafael, CA: Morgan & Claypool Life Sciences Publisher; 2011.
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Oshima T, Chayama K. Endothelial function and oxidative stress in renovascular hypertension. N Engl J Med. 2002;346(25):1954–62. https://doi.org/10.1056/NEJMoa013591.
Holmstrom KM, Finkel T. Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat Rev Mol Cell Biol. 2014;15(6):411–21. https://doi.org/10.1038/nrm3801.
Prysyazhna O, Rudyk O, Eaton P. Single atom substitution in mouse protein kinase G eliminates oxidant sensing to cause hypertension. Nat Med. 2012;18(2):286–90. https://doi.org/10.1038/nm.2603.
Nakajima S, Ohashi J, Sawada A, Noda K, Fukumoto Y, Shimokawa H. Essential role of bone marrow for microvascular endothelial and metabolic functions in mice. Circ Res. 2012;111(1):87–96. https://doi.org/10.1161/circresaha.112.270215.
Reddi AR, Culotta VC. SOD1 integrates signals from oxygen and glucose to repress respiration. Cell. 2013;152(1–2):224–35. https://doi.org/10.1016/j.cell.2012.11.046.
Rubanyi GM, Vanhoutte PM. Oxygen-derived free radicals, endothelium, and responsiveness of vascular smooth muscle. Am J Physiol. 1986;250:H815–21. https://doi.org/10.1152/ajpheart.1986.250.5.H815.
Nagao T, Illiano S, Vanhoutte PM. Calmodulin antagonists inhibit endothelium-dependent hyperpolarization in the canine coronary artery. Br J Pharmacol. 1992;107(2):382–6. https://doi.org/10.1111/j.1476-5381.1992.tb12755.x.
Matoba T, Shimokawa H, Kubota H, Morikawa K, Fujiki T, Kunihiro I, Mukai Y, Hirakawa Y, Takeshita A. Hydrogen peroxide is an endothelium-derived hyperpolarizing factor in human mesenteric arteries. Biochem Biophys Res Commun. 2002;290(3):909–13. https://doi.org/10.1006/bbrc.2001.6278.
Liu Y, Bubolz AH, Mendoza S, Zhang DX, Gutterman DD. H2O2 is the transferrable factor mediating flow-induced dilation in human coronary arterioles. Circ Res. 2011;108(5):566–73. https://doi.org/10.1161/circresaha.110.237636.
Lacza Z, Puskar M, Kis B, Perciaccante JV, Miller AW, Busija DW. Hydrogen peroxide acts as an EDHF in the piglet pial vasculature in response to bradykinin. Am J Physiol Heart Circ Physiol. 2002;283(1):H406–11. https://doi.org/10.1152/ajpheart.00007.2002.
Burgoyne JR, Oka S, Ale-Agha N, Eaton P. Hydrogen peroxide sensing and signaling by protein kinases in the cardiovascular system. Antioxid Redox Signal. 2013;18(9):1042–52. https://doi.org/10.1089/ars.2012.4817.
Zhang DX, Borbouse L, Gebremedhin D, Mendoza SA, Zinkevich NS, Li R, Gutterman DD. H2O2-induced dilation in human coronary arterioles: role of protein kinase G dimerization and large-conductance Ca2+-activated K+ channel activation. Circ Res. 2012;110(3):471–80. https://doi.org/10.1161/circresaha.111.258871.
Ohashi J, Sawada A, Nakajima S, Noda K, Takaki A, Shimokawa H. Mechanisms for enhanced endothelium-derived hyperpolarizing factor-mediated responses in microvessels in mice. Circ J. 2012;76(7):1768–79. https://doi.org/10.1253/circj.cj-12-0197.
Godo S, Sawada A, Saito H, Ikeda S, Enkhjargal B, Suzuki K, Tanaka S, Shimokawa H. Disruption of physiological balance between nitric oxide and endothelium-dependent hyperpolarization impairs cardiovascular homeostasis in mice. Arterioscler Thromb Vasc Biol. 2016;36(1):97–107. https://doi.org/10.1161/atvbaha.115.306499.
Garcia-Redondo AB, Briones AM, Beltran AE, Alonso MJ, Simonsen U, Salaices M. Hypertension increases contractile responses to hydrogen peroxide in resistance arteries through increased thromboxane A2, Ca2+, and superoxide anion levels. J Pharmacol Exp Ther. 2009;328(1):19–27. https://doi.org/10.1124/jpet.108.144295.
Antunes F, Cadenas E. Estimation of H2O2 gradients across biomembranes. FEBS Lett. 2000;475(2):121–6. https://doi.org/10.1016/s0014-5793(00)01638-0.
Takaki A, Morikawa K, Murayama Y, Yamagishi H, Hosoya M, Ohashi J, Shimokawa H. Roles of endothelial oxidases in endothelium-derived hyperpolarizing factor responses in mice. J Cardiovasc Pharmacol. 2008;52(6):510–7. https://doi.org/10.1097/FJC.0b013e318190358b.
Morikawa K, Shimokawa H, Matoba T, Kubota H, Akaike T, Talukder MA, Hatanaka M, Fujiki T, Maeda H, Takahashi S, Takeshita A. Pivotal role of Cu,Zn-superoxide dismutase in endothelium-dependent hyperpolarization. J Clin Invest. 2003;112(12):1871–9. https://doi.org/10.1172/jci19351.
Liu Y, Zhao H, Li H, Kalyanaraman B, Nicolosi AC, Gutterman DD. Mitochondrial sources of H2O2 generation play a key role in flow-mediated dilation in human coronary resistance arteries. Circ Res. 2003;93(6):573–80. https://doi.org/10.1161/01.res.0000091261.19387.ae.
Larsen BT, Bubolz AH, Mendoza SA, Pritchard KA Jr, Gutterman DD. Bradykinin-induced dilation of human coronary arterioles requires NADPH oxidase-derived reactive oxygen species. Arterioscler Thromb Vasc Biol. 2009;29(5):739–45. https://doi.org/10.1161/atvbaha.108.169367.
Sartoretto JL, Kalwa H, Pluth MD, Lippard SJ, Michel T. Hydrogen peroxide differentially modulates cardiac myocyte nitric oxide synthesis. Proc Natl Acad Sci U S A. 2011;108(38):15792–7. https://doi.org/10.1073/pnas.1111331108.
Shiroto T, Romero N, Sugiyama T, Sartoretto JL, Kalwa H, Yan Z, Shimokawa H, Michel T. Caveolin-1 is a critical determinant of autophagy, metabolic switching, and oxidative stress in vascular endothelium. PLoS One. 2014;9(2):e87871. https://doi.org/10.1371/journal.pone.0087871.
Freed JK, Beyer AM, LoGiudice JA, Hockenberry JC, Gutterman DD. Ceramide changes the mediator of flow-induced vasodilation from nitric oxide to hydrogen peroxide in the human microcirculation. Circ Res. 2014;115(5):525–32. https://doi.org/10.1161/circresaha.115.303881.
Beyer AM, Freed JK, Durand MJ, Riedel M, Ait-Aissa K, Green P, Hockenberry JC, Morgan RG, Donato AJ, Peleg R, Gasparri M, Rokkas CK, Santos JH, Priel E, Gutterman DD. Critical role for telomerase in the mechanism of flow-mediated dilation in the human microcirculation. Circ Res. 2016;118(5):856–66. https://doi.org/10.1161/circresaha.115.307918.
Shimokawa H. Hydrogen peroxide as an endothelium-derived hyperpolarizing factor. Pflugers Arch. 2010;459(6):915–22. https://doi.org/10.1007/s00424-010-0790-8.
Chidgey J, Fraser PA, Aaronson PI. Reactive oxygen species facilitate the EDH response in arterioles by potentiating intracellular endothelial Ca2+ release. Free Radic Biol Med. 2016;97:274–84. https://doi.org/10.1016/j.freeradbiomed.2016.06.010.
Burgoyne JR, Madhani M, Cuello F, Charles RL, Brennan JP, Schroder E, Browning DD, Eaton P. Cysteine redox sensor in PKGIα enables oxidant-induced activation. Science. 2007;317(5843):1393–7. https://doi.org/10.1126/science.1144318.
Dou D, Zheng X, Liu J, Xu X, Ye L, Gao Y. Hydrogen peroxide enhances vasodilatation by increasing dimerization of cGMP-dependent protein kinase type Iα. Circ J. 2012;76(7):1792–8. https://doi.org/10.1253/circj.cj-11-1368.
Russo G, Di Franco A, Lamendola P, Tarzia P, Nerla R, Stazi A, Villano A, Sestito A, Lanza GA, Crea F. Lack of effect of nitrates on exercise stress test results in patients with microvascular angina. Cardiovasc Drugs Ther. 2013;27(3):229–34. https://doi.org/10.1007/s10557-013-6439-z.
Redfield MM, Anstrom KJ, Levine JA, Koepp GA, Borlaug BA, Chen HH, LeWinter MM, Joseph SM, Shah SJ, Semigran MJ, Felker GM, Cole RT, Reeves GR, Tedford RJ, Tang WH, McNulty SE, Velazquez EJ, Shah MR, Braunwald E. Isosorbide mononitrate in heart failure with preserved ejection fraction. N Engl J Med. 2015;373(24):2314–24. https://doi.org/10.1056/NEJMoa1510774.
Takahashi J, Nihei T, Takagi Y, Miyata S, Odaka Y, Tsunoda R, Seki A, Sumiyoshi T, Matsui M, Goto T, Tanabe Y, Sueda S, Momomura SI, Yasuda S, Ogawa H, Shimokawa H. Prognostic impact of chronic nitrate therapy in patients with vasospastic angina: multicentre registry study of the Japanese coronary spasm association. Eur Heart J. 2015;36(4):228–37. https://doi.org/10.1093/eurheartj/ehu313.
Borlaug BA, Anstrom KJ, Lewis GD, Shah SJ, Levine JA, Koepp GA, Givertz MM, Felker GM, LeWinter MM, Mann DL, Margulies KB, Smith AL, Tang WHW, Whellan DJ, Chen HH, Davila-Roman VG, McNulty S, Desvigne-Nickens P, Hernandez AF, Braunwald E, Redfield MM. Effect of inorganic nitrite vs placebo on exercise capacity among patients with heart failure with preserved ejection fraction: the INDIE-HFpEF randomized clinical trial. JAMA. 2018;320(17):1764–73. https://doi.org/10.1001/jama.2018.14852.
Golino M, Spera FR, Manfredonia L, De Vita A, Di Franco A, Lamendola P, Villano A, Melita V, Mencarelli E, Lanza GA, Crea F. Microvascular ischemia in patients with successful percutaneous coronary intervention: effects of ranolazine and isosorbide-5-mononitrate. Eur Rev Med Pharmacol Sci. 2018;22(19):6545–50. https://doi.org/10.26355/eurrev_201810_16070.
Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis. JAMA. 2007;297(8):842–57. https://doi.org/10.1001/jama.297.8.842.
Takaki A, Morikawa K, Tsutsui M, Murayama Y, Tekes E, Yamagishi H, Ohashi J, Yada T, Yanagihara N, Shimokawa H. J Exp Med. 2008;205(9):2053–63. https://doi.org/10.1084/jem.20080106.
Forstermann U, Li H. Therapeutic effect of enhancing endothelial nitric oxide synthase (eNOS) expression and preventing eNOS uncoupling. Br J Pharmacol. 2011;164(2):213–23. https://doi.org/10.1111/j.1476-5381.2010.01196.x.
Stuehr D, Pou S, Rosen GM. Oxygen reduction by nitric-oxide synthases. J Biol Chem. 2001;276(18):14533–6. https://doi.org/10.1074/jbc.R100011200.
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature. 1995;377(6546):239–42. https://doi.org/10.1038/377239a0.
Bauersachs J, Popp R, Hecker M, Sauer E, Fleming I, Busse R. Nitric oxide attenuates the release of endothelium-derived hyperpolarizing factor. Circulation. 1996;94(12):3341–7. https://doi.org/10.1161/01.cir.94.12.3341.
Nishikawa Y, Stepp DW, Chilian WM. Nitric oxide exerts feedback inhibition on EDHF-induced coronary arteriolar dilation in vivo. Am J Physiol Heart Circ Physiol. 2000;279(2):H459–65. https://doi.org/10.1152/ajpheart.2000.279.2.H459.
Olmos L, Mombouli JV, Illiano S, Vanhoutte PM. cGMP mediates the desensitization to bradykinin in isolated canine coronary arteries. Am J Physiol. 1995;268(2 Pt 2):H865–70. https://doi.org/10.1152/ajpheart.1995.268.2.H865.
Burgoyne JR, Prysyazhna O, Rudyk O, Eaton P. cGMP-dependent activation of protein kinase G precludes disulfide activation: implications for blood pressure control. Hypertension. 2012;60(5):1301–8. https://doi.org/10.1161/hypertensionaha.112.198754.
Saito H, Godo S, Sato S, Ito A, Ikumi Y, Tanaka S, Ida T, Fujii S, Akaike T, Shimokawa H. Important role of endothelial caveolin-1 in the protective role of endothelium-dependent hyperpolarization against nitric oxide-mediated nitrative stress in microcirculation in mice. J Cardiovasc Pharmacol. 2018;71(2):113–26. https://doi.org/10.1097/fjc.0000000000000552.
Enkhjargal B, Godo S, Sawada A, Suvd N, Saito H, Noda K, Satoh K, Shimokawa H. Endothelial AMP-activated protein kinase regulates blood pressure and coronary flow responses through hyperpolarization mechanism in mice. Arterioscler Thromb Vasc Biol. 2014;34:1505–13. https://doi.org/10.1161/atvbaha.114.303735.
Kikuchi Y, Yasuda S, Aizawa K, Tsuburaya R, Ito Y, Takeda M, Nakayama M, Ito K, Takahashi J, Shimokawa H. Enhanced Rho-kinase activity in circulating neutrophils of patients with vasospastic angina: a possible biomarker for diagnosis and disease activity assessment. J Am Coll Cardiol. 2011;58(12):1231–7. https://doi.org/10.1016/j.jacc.2011.05.046.
Nihei T, Takahashi J, Hao K, Kikuchi Y, Odaka Y, Tsuburaya R, Nishimiya K, Matsumoto Y, Ito K, Miyata S, Sakata Y, Shimokawa H. Prognostic impacts of Rho-kinase activity in circulating leucocytes in patients with vasospastic angina. Eur Heart J. 2018;39(11):952–9. https://doi.org/10.1093/eurheartj/ehx657.
Mohri M, Shimokawa H, Hirakawa Y, Masumoto A, Takeshita A. Rho-kinase inhibition with intracoronary fasudil prevents myocardial ischemia in patients with coronary microvascular spasm. J Am Coll Cardiol. 2003;41(1):15–9. https://doi.org/10.1016/s0735-1097(02)02632-3.
Kikuchi Y, Takahashi J, Hao K, Sato K, Sugisawa J, Tsuchiya S, Suda A, Shindo T, Ikeda S, Shiroto T, Matsumoto Y, Miyata S, Sakata Y, Shimokawa H. Usefulness of intracoronary administration of fasudil, a selective Rho-kinase inhibitor, for PCI-related refractory myocardial ischemia. Int J Cardiol. 2019;297:8–13. https://doi.org/10.1016/j.ijcard.2019.09.057.
Halcox JP, Nour KR, Zalos G, Quyyumi AA. Endogenous endothelin in human coronary vascular function: differential contribution of endothelin receptor types A and B. Hypertension. 2007;49(5):1134–41. https://doi.org/10.1161/hypertensionaha.106.083303.
Odaka Y, Takahashi J, Tsuburaya R, Nishimiya K, Hao K, Matsumoto Y, Ito K, Sakata Y, Miyata S, Manita D, Hirowatari Y, Shimokawa H. Plasma concentration of serotonin is a novel biomarker for coronary microvascular dysfunction in patients with suspected angina and unobstructive coronary arteries. Eur Heart J. 2017;38(7):489–96. https://doi.org/10.1093/eurheartj/ehw448.
Lanza GA. Diagnostic approach to patients with stable angina and no obstructive coronary arteries. Eur Cardiol. 2019;14(2):97–102. https://doi.org/10.15420/ecr.2019.22.2.
Mohri M, Koyanagi M, Egashira K, Tagawa H, Ichiki T, Shimokawa H, Takeshita A. Angina pectoris caused by coronary microvascular spasm. Lancet. 1998;351(9110):1165–9. https://doi.org/10.1016/s0140-6736(97)07329-7.
Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol. 2012;59(7):655–62. https://doi.org/10.1016/j.jacc.2011.11.015.
Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, Kaski JC, Bairey Merz CN. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 2018;250:16–20. https://doi.org/10.1016/j.ijcard.2017.08.068.
Ford TJ, Stanley B, Good R, Rocchiccioli P, McEntegart M, Watkins S, Eteiba H, Shaukat A, Lindsay M, Robertson K, Hood S, McGeoch R, McDade R, Yii E, Sidik N, McCartney P, Corcoran D, Collison D, Rush C, McConnachie A, Touyz RM, Oldroyd KG, Berry C. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA trial. J Am Coll Cardiol. 2018;72(23):2841–55. https://doi.org/10.1016/j.jacc.2018.09.006.
Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4(11):e002270. https://doi.org/10.1161/jaha.115.002270.
Chadderdon SM, Belcik JT, Bader L, Peters DM, Kievit P, Alkayed NJ, Kaul S, Grove KL, Lindner JR. Temporal changes in skeletal muscle capillary responses and endothelial-derived vasodilators in obesity-related insulin resistance. Diabetes. 2016;65(8):2249–57. https://doi.org/10.2337/db15-1574.
Ford TJ, Rocchiccioli P, Good R, McEntegart M, Eteiba H, Watkins S, Shaukat A, Lindsay M, Robertson K, Hood S, Yii E, Sidik N, Harvey A, Montezano AC, Beattie E, Haddow L, Oldroyd KG, Touyz RM, Berry C. Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur Heart J. 2018;39(46):4086–97. https://doi.org/10.1093/eurheartj/ehy529.
Ohura-Kajitani S, Shiroto T, Godo S, Ikumi Y, Ito A, Tanaka S, Sato K, Sugisawa J, Tsuchiya S, Suda A, Shindo T, Ikeda S, Hao K, Kikuchi Y, Nochioka K, Matsumoto Y, Takahashi J, Miyata S, Shimokawa H. Marked impairment of endothelium-dependent digital vasodilatations in patients with microvascular angina: evidence for systemic small artery disease. Arterioscler Thromb Vasc Biol. 2020;40(5):1400–12. https://doi.org/10.1161/atvbaha.119.313704.
Ikumi Y, Shiroto T, Godo S, Saito H, Tanaka S, Ito A, Kajitani S, Monma Y, Miyata S, Tsutsui M, Shimokawa H. Important roles of endothelium-dependent hyperpolarization in coronary microcirculation and cardiac diastolic function in mice. J Cardiovasc Pharmacol. 2020;75(1):31–40. https://doi.org/10.1097/fjc.0000000000000763.
Siasos G, Sara JD, Zaromytidou M, Park KH, Coskun AU, Lerman LO, Oikonomou E, Maynard CC, Fotiadis D, Stefanou K, Papafaklis M, Michalis L, Feldman C, Lerman A, Stone PH. Local low shear stress and endothelial dysfunction in patients with nonobstructive coronary atherosclerosis. J Am Coll Cardiol. 2018;71(19):2092–102. https://doi.org/10.1016/j.jacc.2018.02.073.
Godo S, Corban MT, Toya T, Gulati R, Lerman LO, Lerman A. Association of coronary microvascular endothelial dysfunction with vulnerable plaque characteristics in early coronary atherosclerosis. EuroIntervention. (in press). 2019; https://doi.org/10.4244/eij-d-19-00265.
Corban MT, Eshtehardi P, Suo J, McDaniel MC, Timmins LH, Rassoul-Arzrumly E, Maynard C, Mekonnen G, King S 3rd, Quyyumi AA, Giddens DP, Samady H. Combination of plaque burden, wall shear stress, and plaque phenotype has incremental value for prediction of coronary atherosclerotic plaque progression and vulnerability. Atherosclerosis. 2014;232(2):271–6. https://doi.org/10.1016/j.atherosclerosis.2013.11.049.
Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, Keeble T, Mielewczik M, Kaprielian R, Malik IS, Nijjer SS, Petraco R, Cook C, Ahmad Y, Howard J, Baker C, Sharp A, Gerber R, Talwar S, Assomull R, Mayet J, Wensel R, Collier D, Shun-Shin M, Thom SA, Davies JE, Francis DP. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391(10115):31–40. https://doi.org/10.1016/s0140-6736(17)32714-9.
Schiattarella GG, Altamirano F, Tong D, French KM, Villalobos E, Kim SY, Luo X, Jiang N, May HI, Wang ZV, Hill TM, Mammen PPA, Huang J, Lee DI, Hahn VS, Sharma K, Kass DA, Lavandero S, Gillette TG, Hill JA. Nitrosative stress drives heart failure with preserved ejection fraction. Nature. 2019;568(7752):351–6. https://doi.org/10.1038/s41586-019-1100-z.
Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR Jr, Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation. 2000;101(9):948–54. https://doi.org/10.1161/01.CIR.101.9.948.
Halcox JP, Schenke WH, Zalos G, Mincemoyer R, Prasad A, Waclawiw MA, Nour KR, Quyyumi AA. Prognostic value of coronary vascular endothelial dysfunction. Circulation. 2002;106(6):653–8. https://doi.org/10.1161/01.cir.0000025404.78001.d8.
Cassar A, Chareonthaitawee P, Rihal CS, Prasad A, Lennon RJ, Lerman LO, Lerman A. Lack of correlation between noninvasive stress tests and invasive coronary vasomotor dysfunction in patients with nonobstructive coronary artery disease. Circ Cardiovasc Interv. 2009;2(3):237–44. https://doi.org/10.1161/circinterventions.108.841056.
Ong P, Athanasiadis A, Borgulya G, Vokshi I, Bastiaenen R, Kubik S, Hill S, Schaufele T, Mahrholdt H, Kaski JC, Sechtem U. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation. 2014;129(17):1723–30. https://doi.org/10.1161/circulationaha.113.004096.
Lerman A, Holmes DR, Herrmann J, Gersh BJ. Microcirculatory dysfunction in ST-elevation myocardial infarction: cause, consequence, or both? Eur Heart J. 2007;28(7):788–97. https://doi.org/10.1093/eurheartj/ehl501.
Acknowledgments
This work was supported in part by the Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Tokyo, Japan, and the Grants-in-Aid for Scientific Research from the Ministry of Health, Labour, and Welfare, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Godo, S., Shimokawa, H. (2021). Pathophysiology of Coronary Microvascular Dysfunction. In: Shimokawa, H. (eds) Coronary Vasomotion Abnormalities. Springer, Singapore. https://doi.org/10.1007/978-981-15-7594-5_6
Download citation
DOI: https://doi.org/10.1007/978-981-15-7594-5_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-7593-8
Online ISBN: 978-981-15-7594-5
eBook Packages: MedicineMedicine (R0)