Abstract
After endoscopic removal of common bile duct stones, cholecystectomy can be considered to reduce recurrent biliary complications in patients with gallbladder (GB) stones. To date, several retrospective and prospective studies have been reported. However, these studies had limitations with different designs, small sample sizes, and short follow-up durations, and the results varied. Some recent large-scale population-based studies recommended prophylactic cholecystectomy to reduce recurrent biliary complications in patients with concomitant GB stones after endoscopic stone removal. Whether prophylactic cholecystectomy is necessary even in elderly patients with comorbid diseases is controversial. The timing of a cholecystectomy can affect the occurrence of additional biliary events during the waiting period, the development of surgical complications, and the conversion to open surgery. As the optimal timing for cholecystectomy, it is recommended to perform early cholecystectomy after endoscopic retrograde cholangiopancreatography during the same hospitalization period.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) and stone removal are the current standard treatments for common bile duct (CBD) stones. CBD stones predominantly originate in the gallbladder (GB) and migrate to the CBD, or may primarily form in the CBD. The remaining GB stones after ERCP stone removal may later migrate to the CBD and cause complications such as biliary obstruction, acute cholangitis, and gallstone pancreatitis. Moreover, GB stones themselves cause biliary colic and acute cholecystitis. Therefore, cholecystectomy seems a reasonable method for reducing CBD stone recurrence and its complications when GB stones are present.
Prospective studies of patients with concomitant GB stones who underwent ERCP stone removal have shown that cholecystectomy reduces the risk of recurrent biliary events compared to the wait-and-see policy [1, 2]. In addition, several retrospective studies recommend cholecystectomy after ERCP stone removal [3,4,5,6]. However, other studies have shown that elective cholecystectomy after ERCP stone removal does not reduce the incidence of recurrent biliary complications [7,8,9,10,11]. In recent years, after endoscopic CBD stone removal, prophylactic cholecystectomy in patients with GB stones is generally recommended to reduce biliary complications. However, the necessity of cholecystectomy is frequently debated.
Endoscopic sphincterotomy (ES) is generally required for CBD stone removal. In this procedure, the biliary orifice is widened so that the subsequent small CBD stone or sludge can pass spontaneously into the duodenum without causing an obstruction. Additionally, ES can reduce recurrent pancreatitis by separating the biliary and pancreatic orifice, eliminating common channels [12]. ES alone may reduce recurrent biliary complications.
Laparoscopic cholecystectomy is preferred over open cholecystectomy as surgical treatment because it has a lower morbidity and requires a shorter hospital stay. However, 3–20% of laparoscopic cholecystectomies require conversion to open cholecystectomy because of technical difficulties such as bleeding and adhesions [13, 14]. Furthermore, elderly patients, who make up the majority of patients with complicated gallstone disease, have a higher incidence of comorbidity, an increased conversion rate to open cholecystectomy, and higher morbidity and mortality than do younger patients. Therefore, the wait-and-see policy without cholecystectomy can be considered in elderly or surgically high-risk patients [15, 16]. In addition, optimal timing of cholecystectomy after ERCP stone removal is important to reduce recurrent biliary events and the conversion rate to open cholecystectomy; however, there is no consensus on this.
Biliary Complications After ERCP Stone Removal
After successful removal of CBD stones, biliary complications such as recurrent CBD stones and cholecystitis occur in 7–47% of patients within 2.5–15 year follow-up periods [17,18,19,20,21]. The risk factors for the development of biliary complications include GB stones, dilated CBD, mechanical lithotripsy, periampullary diverticulum, and bile duct strictures [11, 17, 20, 22,23,24,25].
Considering CBD stone recurrence, its incidence after ERCP stone removal has found to be 2–22% in follow-up studies [17,18,19,20,21, 24,25,26,27] and 11.3% in a population-based study [28]. Recurrence of CBD stones after ERCP stone removal is caused by a number of mechanisms. Migration of the GB stone into the CBD is an important mechanism. Moreover, reflux of duodenal contents into the bile duct, stricture at the ES site, and dilated CBD lead to bile stasis and bacterial infection with consequent sludge and stone formation in the CBD.
Acute cholecystitis is another concern in patients who have undergone CBD stone removal, especially in patients with GB stones. The risk of acute cholecystitis has been suggested to be increased after ES. Dysfunction of the biliary sphincter after ES might be a cause of reflux of duodenal contents into the bile duct and biliary infection, leading to infection of the GB and subsequent cholecystitis [3].
The development of acute cholecystitis is a definite indication of cholecystectomy. A study of 100 patients who had their CBD stone removed without cholecystectomy reported that acute cholecystitis occurred in 17% and CBD stone recurred in 15% of the patients. The risk factors of acute cholecystitis include nondilated CBD (<11 mm) and absence of jaundice (serum total bilirubin <1.3 mg/dL) at the time of CBD stone removal [29]. Small CBD stones in association with a nondilated CBD are more likely to originate from the GB. If cholecystectomy is not performed in such patients, development of acute cholecystitis due to cystic duct obstruction by a small gallstone is a risk during passage of gallstones.
Prophylactic Cholecystectomy
Several retrospective, prospective, and population-based studies of cholecystectomies performed after ERCP stone removal have been conducted. Each study differs in design, including sample size, follow-up duration, age of the patients studied, and whether only patients with GB stones or those with intact GB are included (Table 1).
Patients Without GB Stones
Patients without GB stones have a lower recurrence rate of CBD stone than do patients with GB stones [3, 4, 19]. Furthermore, CBD stone recurrence rate was lower in patients with acalculous GB in situ than in patients who had previously undergone a cholecystectomy [4]. Theoretically, because GB stone migration from the GB is a possible mechanism of CBD stone recurrence, a patient without GB stones is not considered a surgical candidate. It has also been reported that a GB without stones after ERCP stone removal does not increase the risk of acute cholecystitis [3]. A GB without gallstones after ERCP stone removal helps to wash away bile and prevent new stone formation or flush out newly produced gallstones [30]. Therefore, prophylactic cholecystectomy after ERCP stone removal is not generally recommended in patients without GB stones in terms of its preventive effect on recurrent CBD stones.
Patients with GB Stones
Patients with GB stones are considered to have an increased risk of recurrent CBD stone secondary to stone migration from the GB and subsequent acute cholecystitis. There has been much research on the prophylactic effect of cholecystectomy after ERCP stone removal. Some studies recommended cholecystectomy, while others do not. Most of these studies had had small sample sizes, short follow-up durations, and retrospective chart reviews; moreover, there is a lack of large randomized studies.
Schreurs et al. conducted a large cohort study of 447 patients with symptomatic GB and CBD stones. Of these patients, 164 underwent ERCP stone removal and no additional cholecystectomy, and 78 underwent cholecystectomy after ERCP stone removal. Of the patients who underwent only ERCP stone removal, 27 (16%) developed recurrent biliary complications. Specifically, 12 had recurrent CBD stones, 3 developed cholangitis, and 1 had papillary stenosis. Of these 27 patients, 13 underwent cholecystectomy. Of the cholecystectomized patients, 6 (7.6%) developed recurrent biliary complications. In patients who did not undergo cholecystectomy, the risk of biliary complications was similar to that in the normal population with silent stones. The authors concluded that when CBD stones are successfully removed and the patient is asymptomatic, routine prophylactic cholecystectomy is not required [10].
Boerma et al. conducted a randomized, prospective study that evaluated 120 patients with GB stones who underwent ERCP stone removal. All patients underwent ERCP and were randomized to a wait-and-see policy arm (64 patients) versus laparoscopic cholecystectomy (56 patients). They found that 47% of the wait-and-see group developed recurrent biliary symptoms compared with 2% of the laparoscopic cholecystectomy group, and 22 of 27 (81%) patients in the wait-and-see arm subsequently underwent cholecystectomy for recurrent biliary symptoms. The conversion rate to open cholecystectomy was 55% in the wait-and-see group and 23% in the laparoscopic cholecystectomy group. The authors concluded that a wait-and-see policy after ERCP stone removal in patients with concomitant GB stones cannot be recommended as standard treatment given the high rate of recurrent biliary symptoms and high conversion rate to open cholecystectomy [1].
In another prospective study, further biliary events after ERCP stone removal developed more frequently in patients with GB in situ than in cholecystectomized patients (24% versus 7%). The most common biliary event in both groups was cholangitis, for which the authors recommended cholecystectomy, just as in the previous report [2]. However, in a recent prospective study, cholecystectomy after CBD stone removal failed to reduce additional recurrent cholangitis, and the authors suggested that cholecystectomy should be limited to patients with symptomatic GB stones [7]. Furthermore, several retrospective studies show different results on this issue [3,4,5,6, 8, 9, 11].
A recent meta-analysis of 7 randomized control trials with 916 patients showed no difference in mortality between patients who underwent cholecystectomy after ERCP stone removal and patients who did not. In addition, there was no difference in the rate of acute pancreatitis between the two groups. However, pooled relative risk (RR) for occurrence of biliary colic and cholecystitis in the wait-and-see policy patients was 9.82 (4.27–22.59) compared to prophylactic cholecystectomy patients, and the RR for cholangitis and recurrent jaundice was 2.16 (1.14–4.07). Therefore, the author recommended laparoscopic cholecystectomy because of the lower rates of subsequent recurrent cholecystitis, cholangitis, and biliary colic, even in high-risk surgical patients [31].
A Korean population-based study reported different CBD stone recurrence rates in patients with GB stones who underwent cholecystectomy after ERCP stone removal and those who did not. During the follow-up period, CBD stone recurrence occurred in 7.92% (920/11,617) in the cholecystectomy group and in 14.60% (773/5,293) in the no-cholecystectomy group. The recurrence rate of CBD stone in the no-cholecystectomy group was about two times than that in the cholecystectomy group (RR = 1.961, 95% CI = 1.783–2.158, p < 0.0001). The RR for CBD stone recurrence in the no-cholecystectomy group compared with the cholecystectomy group was 3.198 in patients aged <50 years, 2.371 in patients aged 50–59 years, 1.618 in patients aged 60–69 years, and 1.262 in patients aged ≥70 years. The RR for CBD stone recurrence in the no-cholecystectomy group was higher in younger patients. As age increased, the RR decreased. The authors recommended cholecystectomy in patients aged < 70 years with GB stone to reduce the risk of CBD stone recurrence as well as cholecystitis, and it was strongly recommended for relatively younger patients [28].
In addition, Huang et al. reported that the cumulative incidence of recurrent biliary events 60 days after discharge was 10.3% in the no-cholecystectomy group, 1.4% in the early cholecystectomy group, and 1.3% in the delayed cholecystectomy group. Prophylactic cholecystectomy within 60 days after ERCP was associated with 87–88% RR reduction for recurrent biliary events compared to the no-cholecystectomy group [32].
Elderly Patients
Due to comorbidities and low-performance status, elderly patients are thought to be at risk of increased perioperative morbidity and mortality. A systemic review demonstrated that early cholecystectomy for acute cholecystitis in patients aged ≥70 years is associated with a perioperative morbidity of 24% and a mortality of 3.5% [33]. These rates are higher than those in non-elderly patients, which have been investigated in a meta-analysis, being approximately 15% and <1%, respectively [34].
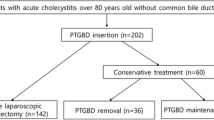
Some investigators do not recommend cholecystectomy after ERCP stone removal in elderly patients with GB stones [15, 16]. In a cost-effectiveness analysis, cholecystectomy was not recommended in elderly patients considering economic and survival benefits [15]. According to a Japanese study, in very elderly patients (those older than 80), the incidence of acute cholecystitis is low even when GB is preserved after ERCP stone removal, with a similar risk of CBD stone recurrence. The author does not recommend cholecystectomy after ERCP stone removal in very elderly patients [16]. GB contractile function in very elderly patients might decline, and they rarely develop acute cholecystitis. The low incidence of acute cholecystitis in very elderly patients might be explained by the decreased preference for fatty foods by older patients, which can trigger the development of cholecystitis [35].
In a previous Korean population-based study, the RR reported for CBD stone recurrence in the no-cholecystectomy group was only 1.262 for patients over 70 years old. The authors recommended to decide the cholecystectomy for patients over 70, considering the risk of operation and the comorbid illnesses [28].
Young et al. conducted a propensity score matching population-based study of 670 patients over 70 years of age to evaluate the preventive effect of cholecystectomy against recurrent pancreatitis. The incidence rate of recurrent pancreatitis was 12.39 per 1000 person-year in the cholecystectomy cohort and 23.94 per 1000 person-year in the control cohort. The risk of recurrent pancreatitis was significantly lower in the cholecystectomy cohort (hazard ratio [HR] = 0.56, 95% CI = 0.59–0.95, p = 0.021). The HR for all-cause mortality among the cholecystectomy cohort was 0.75 (95% CI = 0.59–0.95; p = 0.016) compared with the control cohort. The authors concluded that prophylactic cholecystectomy should be recommended in these elderly patients [36].
Furthermore, in a population-based study of patients over 65 years of age, prophylactic cholecystectomy was significantly associated with a 50–70% RR reduction in recurrent CBD stones, cholangitis, and gallstone pancreatitis compared to only ES. This benefit was preserved in patients over the age of 75 and in those with serious comorbidities such as cancer and heart failure, and did not appear to be outweighed by surgical complications [37].
Endoscopic Balloon Biliary Dilatation
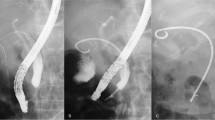
Endoscopic papillary balloon dilation (EPBD) can be another alternative to ES in selected patients, such as those with an altered anatomy or at bleeding risk. Several studies have shown that EPBD alone or in combination with small ES and lithotripsy can be used for the management of difficult biliary stones [38,39,40]. The advantage of EPBD is that it can preserve the biliary sphincter function, which prevents duodeno-biliary reflux and bacterial contamination [41].
In a prospective multicenter randomized controlled trial that compared the early outcomes after ES and EPBD, the overall incidence of late biliary complications in the EPBD group was significantly lower than that in the ES group (10.1% versus 25.0%, p = 0.016). The biliary sphincter dysfunction after ES results in additional late complications [42].
However, according to a propensity score-based cohort study that compared cholecystectomy and the wait-and-see approach after EPBD, the rates of late biliary complications were 5.4 and 25.2% in the cholecystectomy and wait-and-see groups, respectively. Recurrent CBD stones rates were 4.1 and 19.0%, and cholecystitis rates were 0.7 and 6.1%, respectively. The majority of late complications in the group with GB left in situ with stones was CBD stone recurrence, which had likely migrated from the GB. Preserved papillary function after EPBD had no impact on the prevention of CBD stone recurrence in this group. The authors recommended prophylactic cholecystectomy to all surgically fit patients after EPBD for CBD stones with concomitant GB stones [43].
Decision of Prophylactic Cholecystectomy in the Real World
Taken together, the results of previous retrospective and prospective studies showed equivocal outcomes of recommendations for cholecystectomy [1,2,3,4,5,6,7,8,9,10,11, 43]. However, several large-scale population-based studies and meta-analyses recommend cholecystectomy [28, 31, 32, 36, 37].
The decision to perform cholecystectomy in patients who undergone ERCP stone removal should be considered in two ways. One is the effect on the prevention of recurrent biliary complications, and the other is the burden on morbidity, mortality, and health care expenditure associated with cholecystectomy. Unless patients are at high risk for cholecystectomy, it is reasonable to recommend cholecystectomy for patients with GB stones after ERCP stone removal regardless of age. However, in reality, cholecystectomy is not always performed in line with patients’ preferences or comorbidities in elderly patients. In retrospective population-based cohort studies, the proportion of patients who underwent no-cholecystectomy after ERCP stone removal was 48% in the United States [32] and 78.8% in Taiwan [44]. The rate of laparoscopic cholecystectomy was over 95% in Australia and 90% in the United States [32]. In contrast, the population-based study in Taiwan found that the proportion of patients undergoing laparoscopic cholecystectomy was only 51.16%. In addition, the durations of hospital stay were longer in the open surgery group. This is one reason for the relatively low rate of prophylactic cholecystectomy in Taiwanese patients [44]. Whether cholecystectomy is performed in the actual clinical field, is influenced by hospital factors such as volume and location, and patient factors such as race and insurance status.
Timing of Prophylactic Cholecystectomy
The timing of cholecystectomy following ERCP is also important. Traditionally, surgeons have been reluctant to perform early cholecystectomy because of concerns about inflammation, which may increase the risk of surgical complications. Generally, a cholecystectomy after ERCP stone removal is classified as early cholecystectomy if performed during index admission, delayed cholecystectomy if performed within 60 days of discharge, and no-cholecystectomy if not performed within 60 days of discharge [32, 44,45,46]. Early cholecystectomy is also often defined as a cholecystectomy performed within 72 hours, 7 days, 14 days, or 6 weeks after ERCP [47,48,49,50]. In the literature, the proportion of early cholecystectomy in patients who underwent cholecystectomy after ERCP stone removal was 28.6–79.1%, varying by country or medical institution [32, 44, 45, 47, 48, 50].
In a retrospective study of patients awaiting delayed cholecystectomy (a delayed median of 7 weeks) following ERCP for CBD stone, 20% of all patients had recurrent biliary events during the waiting period. The median time between ERCP and the development of recurrent complications was 22 days. These recurrent complications were associated with a significantly longer hospital stay [51]. Another retrospective study of patients with mild biliary pancreatitis requiring ERCP found a strong protective effect of early cholecystectomy against biliary complications compared to delayed cholecystectomy [48]. Reinders et al. performed a randomized trial of 96 patients with GB stones who underwent ERCP stone removal. Patients were randomly assigned to groups that underwent early cholecystectomy (within 72 hours after ES, n = 49) or delayed cholecystectomy (after 6–8 weeks, n = 47). During the waiting period for cholecystectomy, 17 (36.2%) patients in the delayed group developed recurrent biliary events compared with 1 patient in the early group (p < 0.001) [49]. In addition, early cholecystectomy is important because it can reduce morbidity during the waiting period for elective cholecystectomy, hospital stay, and operating time [52].
A retrospective cohort study in the United States demonstrated practice patterns for performing cholecystectomy following ERCP for CBD stones in 4,516 patients. Of these patients, 41.2% underwent early cholecystectomy (at the index admission), 10.9% underwent delayed cholecystectomy (within 60 days of discharge), and 48.0% underwent no-cholecystectomy. Early cholecystectomy reduced RR of recurrent biliary events within 60 days by 92% compared with delayed or no-cholecystectomy (p < 0.001) [32]. On the other hand, a recent Taiwanese population-based study found that early cholecystectomy had no effect on reducing the interval recurrent biliary event, but delayed cholecystectomy reduced medical expenses [44].
Delayed cholecystectomy can increase the conversion rate to open cholecystectomy. This is thought to be due to local inflammation related to biliary complications and progression of subsequent scarring as these factors make delayed laparoscopic cholecystectomy more difficult. Prior randomized studies have demonstrated a higher rate of open cholecystectomy when surgery is delayed [1, 2]. Open cholecystectomy is associated with increased postoperative pain, more pulmonary complications and wound infections, and a lengthened hospital stay [53,54,55]. A study specifically considering the timing of laparoscopic cholecystectomy after ERCP in relation to the conversion rate found that it was significantly higher when laparoscopic cholecystectomy was performed 2–6 weeks after ERCP than when the operation was performed within 2 weeks after ERCP [56]. In a systemic review of 14 studies with 1,930 patients, the conversion rate increased when the delay between ERCP and laparoscopic cholecystectomy increased. The conversion rate was 4.2% when laparoscopic cholecystectomy was performed within 24 hours of ERCP, and it was 7.6% for 24–76 hours’ delay, 12.3% within 2 weeks, 12.3% after 2–6 weeks, and 14% after more than 6 weeks [57]. Recently, however, there are reports suggesting that early cholecystectomy is not associated with the conversion rate [45, 47, 50].
The rate of complications increases when cholecystectomy is delayed. Li et al. reported that intra-operative and postoperative complications were higher if surgery was delayed for more than 6 weeks after cholangitis [47]. In addition, in a recent study by Discolo et al., intra-operative, postoperative, and overall complications were higher in the delayed cholecystectomy group than early cholecystectomy group [45].
In the United States population-based study, a low-volume facility is associated with delayed cholecystectomy. Hispanics, Asian races, the availability of Medicaid insurance, and no insurance were associated with early cholecystectomy [32]. In a retrospective population-based study, there was wide variability in the rates of early cholecystectomy among census areas (range 0–96%) and health regions (range 20–66%) [48]. The reasons for disparity may be multifactorial. Individual hospitals use a variety of approaches in deciding when to operate on a patient. The culture of hospitals also has a significant impact on the timing of surgery. In addition, the availability of acute surgery at the institution, the experience of the surgeon, the communication between surgeons and endoscopists, and the aggressiveness of endoscopic management are factors to be considered [45, 48, 50].
Conclusion
Prophylactic cholecystectomy is recommended to reduce recurrent biliary complications in patients with GB stones who have undergone CBD stone removal. Although this recommendation applies to patients who are very old or with comorbid diseases, it is necessary to determine whether to perform the operation considering the surgical risk and the patient’s comorbid illness. When cholecystectomy is delayed, recurrent biliary complications, the rate of conversion to open surgery, and postoperative complications may increase. Therefore, it is advisable to perform early cholecystectomy during the index admission period, if possible. However, in practice, whether and when cholecystectomy is performed, varies between countries, regions, and institutions.
References
Boerma D, Rauws EAJ, Keulemans YCA, Janssen IMC, Bolwerk CJM, Timmer R, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: A randomised trial. Lancet. 2002;360:761–5.
Lau JYW, Leow C, Fung TMK, Suen B, Yu L, Lai PBS, et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in chinese patients. Gastroenterology. 2006;130:96–103.
Cui ML, Cho JH, Kim TN. Long-term follow-up study of gallbladder in situ after endoscopic common duct stone removal in Korean patients. Surg Endosc. 2013;27:1711–6.
Kageoka M, Watanabe F, Maruyama Y, Nagata K, Ohata A, Noda Y, et al. Long-term prognosis of patients after endoscopic sphincterotomy for choledocholithiasis. Dig Endosc. 2009;21:170–5.
Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Adamek HE, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–64.
Lai J, Wang H, Chang W, Chu C, Shih S, Lin S. Recurrent cholangitis after endoscopic lithotripsy of common bile duct stones with gallstones in situ: predictive factors with and without subsequent cholecystectomy. J Laparoendosc Adv Surg Tech A. 2012;22:324–9.
Heo J, Jung MK, Cho CM. Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones? Surg Endosc. 2015;29:1574–9.
Hammarstrom LE, Holmin T, Stridbeck H. Endoscopic treatment of bile duct calculi in patients with gallbladder in situ: long-term outcome and factors. Scand J Gastroenterol. 1996;31:294–301.
Lai KH, Lin LF, Lo GH, Cheng JS, Huang RL, Lin CK, et al. Does cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? Gastrointest Endosc. 1999;49:483–7.
Schreurs WH, Vles WJ, Stuifbergen, W. H. N. M., Oostvogel HJM. Endoscopic management of common bile duct stones leaving the gallbladder in situ. A cohort study with long-term follow-up. Dig Surg. 2004;21:60–4.
Song ME, Chung MJ, Lee DJ, Oh TG, Park JY, Bang S, et al. Cholecystectomy for prevention of recurrence after endoscopic clearance of bile duct stones in Korea. Yonsei Med J. 2016;57:132–7.
da Costa DW, Schepers NJ, Römkens TEH, Boerma D, Bruno MJ, Bakker OJ. Endoscopic sphincterotomy and cholecystectomy in acute biliary pancreatitis. Surgeon. 2016;14:99–108.
Bingener J, Richards ML, Schwesinger WH, Strodel WE, Sirinek KR. Laparoscopic cholecystectomy for elderly patients: gold standard for golden years? Arch Surg. 2003;138:531–6.
Bratzler DW, Murray CK. Laparoscopic cholecystectomy in older medicare patients. J Am Geriatr Soc. 1997;45:1157–8.
Drake BB, Arguedas MR, Kilgore ML, Hawn MT, Wilcox CM. Economical and clinical outcomes of alternative treatment strategies in the management of common bile duct stones in the elderly: wait and see or surgery? Am J Gastroenterol. 2006;101:746–52.
Yasui T, Takahata S, Kono H, Nagayoshi Y, Mori Y, Tsutsumi K, et al. Is cholecystectomy necessary after endoscopic treatment of bile duct stones in patients older than 80 years of age? J Gastroenterol. 2012;47:65–70.
Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116–21.
Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002;34:273–9.
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465–9.
Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763–7.
Prat F, Malak NA, Pelletier G, Buffet C, Fritsch J, Choury AD, et al. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996;110:894–9.
Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461–4.
Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42–8.
Jakobs R, Hartmann D, Kudis V, Eickhoff A, Schilling D, Weickert U, et al. Risk factors for symptomatic stone recurrence after transpapillary laser lithotripsy for difficult bile duct stones using a laser with a stone recognition system. Eur J Gastroenterol Hepatol. 2006;18:469–73.
Keizman D, Ish Shalom M, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006;64:60–5.
Bergman JJ, van der Mey S, Rauws EA, Tijssen JG, Gouma DJ, Tytgat GN, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–9.
Kim KY, Han J, Kim HG, Kim BS, Jung JT, Kwon JG, et al. Late complications and stone recurrence rates after bile duct stone removal by endoscopic sphincterotomy and large balloon dilation are similar to those after endoscopic sphincterotomy alone. Clin Endosc. 2013;46:637–42.
Park BK, Seo JH, Jeon HH, Choi JW, Won SY, Cho YS, et al. A nationwide population-based study of common bile duct stone recurrence after endoscopic stone removal in Korea. J Gastroenterol. 2018;53:670–8.
Lee JK, Ryu JK, Park JK, Yoon WJ, Lee SH, Lee KH, et al. Risk factors of acute cholecystitis after endoscopic common bile duct stone removal. World J Gastroenterol. 2006;12:956–60.
Frossard JL, Hadengue A, Amouyal G, Choury A, Marty O, Giostra E, et al. Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc. 2000;51:175–9.
Khan MA, Khan Z, Tombazzi CR, Gadiparthi C, Lee W, Wilcox CM. Role of cholecystectomy after endoscopic sphincterotomy in the management of choledocholithiasis in high-risk patients: a systematic review and meta-analysis. J Clin Gastroenterol. 2018;52:579–89.
Huang RJ, Barakat MT, Girotra M, Banerjee S. Practice patterns for cholecystectomy after endoscopic retrograde cholangiopancreatography for patients with choledocholithiasis. Gastroenterology. 2017;153:762–71.
Loozen CS, van Ramshorst B, van Santvoort HC, Boerma D. Early cholecystectomy for acute cholecystitis in the elderly population: a systematic review and meta-analysis. Dig Surg. 2017;34:371–9.
Cao AM, Eslick GD, Cox MR. Early cholecystectomy is superior to delayed cholecystectomy for acute cholecystitis: a meta-analysis. J Gastrointest Surg. 2015;19:848–57.
Iso H, Date C, Noda H, Yoshimura T, Tamakoshi A. Frequency of food intake and estimated nutrient intake among men and women: the JACC study. J Epidemiol. 2005;15(Suppl 1):S24–42.
Young S, Peng Y, Lin X, Chen Y, Luo J, Wang Y, et al. Cholecystectomy reduces recurrent pancreatitis and improves survival after endoscopic sphincterotomy. J Gastrointest Surg. 2017;21:294–301.
Elmunzer BJ, Noureldin M, Morgan KA, Adams DB, Coté GA, Waljee AK. The impact of cholecystectomy after endoscopic sphincterotomy for complicated gallstone disease. Am J Gastroenterol. 2017;112:1596–602.
Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–9.
Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–9.
Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–5.
Natsui M, Honma T, Genda T, Nakadaira H. Effects of endoscopic papillary balloon dilation and endoscopic sphincterotomy on bacterial contamination of the biliary tract. Eur J Gastroenterol Hepatol. 2011;23:818–24.
Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185–91.
Nakai Y, Isayama H, Tsujino T, Hamada T, Kogure H, Takahara N, et al. Cholecystectomy after endoscopic papillary balloon dilation for bile duct stones reduced late biliary complications: a propensity score-based cohort analysis. Surg Endosc. 2016;30:3014–20.
Wang C, Tsai M, Wang Y, Yang T, Chen H, Sung W, et al. Role of cholecystectomy in choledocholithiasis patients underwent endoscopic retrograde cholangiopancreatography. Sci Rep. 2019;9(1):2168. https://doi.org/10.1038/s41598-018-38428-z.
Discolo A, Reiter S, French B, Hayes D, Lucas G, Tan L, et al. Outcomes following early versus delayed cholecystectomy performed for acute cholangitis. Surg Endosc. 2019. https://doi.org/10.1007/s00464-019-07095-0. (Epub ahead of print).
Mador BD, Panton ONM, Hameed SM. Early versus delayed cholecystectomy following endoscopic sphincterotomy for mild biliary pancreatitis. Surg Endosc. 2014;28:3337–42.
Li VKM, Yum JLK, Yeung YP. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. Am J Surg. 2010;200:483–8.
Mador BD, Nathens AB, Xiong W, Panton ONM, Hameed SM. Timing of cholecystectomy following endoscopic sphincterotomy: a population-based study. Surg Endosc. 2017;31:2977–85.
Reinders JSK, Goud A, Timmer R, Kruyt PM, Kruijt PM, Witteman BJM, et al. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology. 2010;138:2315–20.
Severance SE, Feizpour C, Feliciano DV, Coleman J, Zarzaur BL, Rozycki GF. Timing of cholecystectomy after emergent endoscopic retrograde cholangiopancreatography for cholangitis. Am Surg. 2019;85:895–9.
Schiphorst AHW, Besselink MGH, Boerma D, Timmer R, Wiezer MJ, van Erpecum KJ, et al. Timing of cholecystectomy after endoscopic sphincterotomy for common bile duct stones. Surg Endosc. 2008;22:2046–50.
Gurusamy KS, Koti R, Fusai G, Davidson BR. Early versus delayed laparoscopic cholecystectomy for uncomplicated biliary colic. Cochrane Database Syst Rev. 2013;(6):CD007196. https://doi.org/10.1002/14651858.cd007196.pub3.
Hasukić S, Mesić D, Dizdarević E, Keser D, Hadziselimović S, Bazardzanović M. Pulmonary function after laparoscopic and open cholecystectomy. Surg Endosc. 2002;16:163–5.
Hendolin HI, Pääkönen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P. Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. Eur J Surg. 2000;166:394–9.
Neugebauer E, Troidl H, Spangenberger W, Dietrich A, Lefering R. Conventional versus laparoscopic cholecystectomy and the randomized controlled trial. cholecystectomy study group. Br J Surg. 1991;78:150–4.
de Vries A, Donkervoort SC, van Geloven AAW, Pierik EGJM. Conversion rate of laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis: does the time interval matter? Surg Endosc. 2005;19:996–1001.
Friis C, Rothman JP, Burcharth J, Rosenberg J. Optimal timing for laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreatography: a systematic review. Scand J Surg. 2018;107:99–106.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Park, B.K. (2020). Prophylactic Cholecystectomy in Patients with Concomitant Gallstones After Removal of CBD Stones by ERCP. In: Chung, J., Okazaki, K. (eds) Diseases of the Gallbladder. Springer, Singapore. https://doi.org/10.1007/978-981-15-6010-1_28
Download citation
DOI: https://doi.org/10.1007/978-981-15-6010-1_28
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-6009-5
Online ISBN: 978-981-15-6010-1
eBook Packages: MedicineMedicine (R0)