Abstract
Background
Endoscopic sphincterotomy (EST) is the standard treatment for biliary duct stones. However, performing additional cholecystectomy after EST is controversial. In this study, we aimed to evaluate the effects of cholecystectomy after EST.
Methods
Between December 2008 and July 2011, we performed a prospective, randomized, single-center trial in 90 patients with proven gallstones who underwent EST and stone extraction. After the procedure, patients were randomly allocated to undergo cholecystectomy (n = 45) or to the group of GB left in situ (n = 45). The primary outcome was biliary complications at follow-up.
Results
Cholecystectomy was performed in 26 patients (60.5 %) in cholecystectomy group and in 13 patients (28.9 %) in intended conservative group. The median follow-up was 41 months. An intention-to-treat analysis showed that 8 patients (18.6 %) in the cholecystectomy group and 9 (20.0 %) in those who had their GB left in situ had recurrent biliary events (Kaplan–Meier curve, Breslow test, p = 0.555). In an as-treated analysis, 4 patients (10.3 %) who underwent cholecystectomy and 13 patients (26.5 %) who did not undergo cholecystectomy had additional biliary events during the follow-up period (Log-rank, p = 0.037). However, additional biliary events of cholangitis were similar in the two groups, except for a case of cholecystitis (Log-rank, p = 0.998).
Conclusions
Cholecystectomy after EST for biliary duct stones fails to reduce additional recurrent cholangitis but reduces additional cholecystitis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Endoscopic sphincterotomy (EST) is the standard treatment for bile duct stones. However, after EST, recurrent biliary events occur in 7–47 % of cases within a 2.5–15-year follow-up period [1–5]. To reduce recurrent biliary events after EST, additional cholecystectomy is an optional treatment after EST. However, there is some doubt whether this strategy reduces biliary events, especially choledocholithiasis related biliary events [1, 6–8]. In addition, primary biliary duct stones are predominant among Asians, rather than in Western populations [9]. Therefore, to validate the clinical usefulness of cholecystectomy after EST, we compared the effects of cholecystectomy after EST with those of leaving the gallbladder (GB) in situ after EST for choledocholithiasis.
Methods
Study design
This study was a randomized, controlled trial that compared the effects of cholecystectomy with those observed after leaving the GB in situ after EST for choledocholithiasis. The Ethics Committee at the Kyungpook National University Hospital approved the study protocol, and patients provided their consent for participation in this study. This study was registered at Clinical Trial Registry (www.cris.nih.go.kr, approved number: KCT 0000017). The study followed good clinical practice as well as the guidelines of the Declaration of Helsinki.
Patients
We recruited patients from the departments of internal medicine and gastroenterology of Kyungpook National University Hospital from December 2008 to July 2011. All patients between 18 and 90 years of age, who had undergone EST and extraction of common bile duct (CBD) stone and had radiologically proven gallstones through abdominal ultrasonography, computed tomography, or endoscopic ultrasonography, were eligible for the trial. We excluded patients who were not willing to participate or patients with a previous history of extraction of CBD stones, intrahepatic stones, combined pancreatobiliary malignancy, cholecystitis, were not fit for surgery (American Society of Anesthesiologists (ASA) physical status grade IV and V), or had severe comorbidities that could affect their life spans.
Intervention and randomization
The initial endoscopic retrograde cholangiopancreatography (ERCP) was performed using a side-viewed endoscope (TJF-160; Olympus Optical Corporation, Tokyo, Japan). EST was performed using a wire-guided sphincterotome (Olympus Optical Corporation). The CBD stones were extracted using basket, balloon, or lithotripsy occasionally.
Before hospital discharge, patients were randomly allocated to one of two assigned groups: to undergo a laparoscopic cholecystectomy or have their GB left in situ with cholecystectomy available on demand. Computer-generated randomization was performed by an external statistician using SPSS software (version 18.0, Chicago, IL, USA). The random list was kept by the study coordinator. The patients were enrolled and treatment assignment ascertained by the study investigators.
Follow-up
After hospital discharge, patients in each of the treatment groups visited our outpatient department every 3 months. Laboratory test and imaging, such as abdominal ultrasonography or computed tomography, were conducted, if clinically needed. Those who did not return for scheduled clinical follow-up were contacted by telephone to check on their status.
Outcomes
The primary endpoint was at least a recurrent biliary event after initial EST. Biliary events included cholangitis, cholecystitis, obstructive jaundice, biliary colic, or GB carcinoma. Secondary endpoints were defined as the interval between EST and cholecystectomy, the rate of patients converted to open cholecystectomy, and adverse events of EST or cholecystectomy.
Sample size calculation and statistical methods
After EST with stone extraction, the recurrent biliary event rate was known as 20 % in those whom the GB was left in situ and 1 % in those who underwent cholecystectomy. To detect such a difference with a power of 0.80 and a two-sided α = 0.05, the required number of patients in each group was 40 patients. We expected a dropout of 10 %; 90 patients were randomly allocated to each group.
Analysis was performed by intention-to-treat (ITT), per-protocol (PP), and as-treated. Significances of differences between groups were tested using Fisher’s exact test and Student’s t test. The Kaplan–Meier method was used to determine the times to events. The log-rank test or Breslow test were performed to compare the recurrent biliary events between the two groups using SPSS software (version 18.0, Chicago, IL, USA).
Results
Participant flow
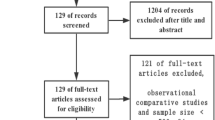
A total 554 patients with bile duct stones were referred for ERCP and stone removal at our institution between December 2008 and July 2011. We excluded 464 patients from the trial because of a previous history of extraction for CBD stones (n = 158), combined cholecystitis (n = 41), no EST (n = 108), age > 90 years (n = 13), combined pancreatobiliary malignancy (n = 34), no GB stone (n = 39), or no consent (n = 36). Ninety patients with cholangitis, CBD stones, and concomitant gallstones were enrolled in this study. After ERCP with stone extraction, these patients were randomly allocated to undergo cholecystectomy (n = 45) or to have their GB left in situ (n = 45). Two patients in the cholecystectomy group were withdrawn from this study; thus, 88 patients were analyzed. Nine patients did not complete the trial (five patients died of another non-biliary disease, and four patients moved from the area without leaving an address). Twenty-six patients (67.4 %) underwent cholecystectomy, and 17 patients (37.8 %) in whom the GB was left in situ group received cholecystectomy (Fig. 1).
Baseline characteristics
Similar baseline characteristics were observed between the two study groups. However, patients with non-biliary malignancies and high ASA grade were predominant in the group in which the GB was left in situ (Table 1).
Primary outcomes
According to the intention-to-treat analysis, the cumulative recurrence of additional biliary-related events was similar between the two groups when analyzed using the Kaplan–Meier survival curve (Breslow test, p = 0.555) (Fig. S1). In the per-protocol analysis, the cumulative recurrence of additional biliary-related events was higher in the group assigned to have their GB left in situ. However, this difference was not statistically significant (Breslow test, p = 0.070) (Fig. S2). According to the as-treated analysis, the cumulative recurrence rate was significantly different between the two groups (Log-rank, p = 0.037) (Fig. 2A). In the cholecystectomy group, four patients (10.3 %) had additional cholangitis during the follow-up. Whereas, 4 patients (8.2 %) had additional cholangitis, and 9 patients (18.4 %) had additional cholecystitis in the group assigned to have their GB left in situ (Table 2). No difference in additional cholangitis event rates was found between the two groups using the Kaplan–Meier survival curve (Log-rank, p = 0.998), except in the case of additional biliary events of cholecystitis (Fig. 2B).
Adverse events, duration of hospitalization, and outcomes after cholecystectomy
In the as-treated analysis, no difference in the incidence of adverse events and hospital stay due to cholecystectomy, and the conversion rate to open cholecystectomy (12.8 vs. 4.1 %, p = 0.449) was observed between the two groups. Among the cases of conversion to open cholecystectomy, each group had one case of emergent operation. The other cases were elective surgery. The median interval from the initial EST to cholecystectomy was 2.2 weeks in cholecystectomy group in ITT analysis. In the as-treated analysis, the interval from the initial EST to cholecystectomy in those whom the GB was left in situ was longer than in those who had undergone cholecystectomy. However, this difference was not significantly different (mean days, 54.1 vs. 442.1 days, p = 0.054) (Table 3).
Discussion
We found that cholecystectomy reduced additional recurrent cholecystitis after EST with CBD stone extraction, but did not reduce additional cholangitis in this study.
In previous similar randomized-controlled trials, patients who underwent cholecystectomy had lesser additional biliary events than those in whom the GB was managed in situ. Lau et al. showed that 6 patients (7 %) in the cholecystectomy group developed further biliary events, whereas 21 of those (24 %) in whom the GB was left in situ had additional biliary events [6]. However, the additional cholangitis rate was not much different between two groups (5.6 vs. 14.6 %; relative risk 1.1; 95 % CI 1.000–1.221). Boerma et al. reported that one patient (2 %) in their cholecystectomy group had recurrent biliary symptoms compared with 27 patients (47 %) in the wait-and-see group (relative risk 22.42; 95 % CI 3.16–159.14; p < 0.001). However, recurrent biliary cholecystitis events also occurred in many patients in the wait-and-see group (7 patients, 12 %). Most recurrent biliary events of uncomplicated pain that occurred in the wait-and-see group (18 patients, 31 %) may have been due to GB colic. Moreover, recurrent biliary events of cholangitis were not found during the follow-up period of this study [5].
In contrast with endoscopic procedures, surgery such as cholecystectomy has a higher incidence of postoperative morbidity and mortality, especially in elderly patients who do not always have suitable indications for cholecystectomy [10, 11]. Cholecystectomy should not be performed, unless this surgery is beneficial. Laparoscopic cholecystectomy, which is a less invasive procedure than open cholecystectomy, is the current standard procedure. However, during the operation, switching to open cholecystectomy may be warranted. Converting to open cholecystectomy usually increases hospital stay and recovery period [12]. In our study, the conversion rate to open cholecystectomy in the group who had their GB left in situ was higher than that in the cholecystectomy group (as-treated analysis, 12.6 vs. 28.6 %), but this difference was not statistically significant (p = 0.347). In addition, there is another problem after cholecystectomy. In a recent study, Tsai el al. recently reported that patients with cholecystectomy before endoscopic treatment had larger stones (1.3 ± 0.6 cm, p = 0.004), larger diameter of CBDs (1.7 ± 0.6 cm, p < 0.001), and had a higher rate of undergoing lithotripsy (11 %, p = 0.018). Patients with prior cholecystectomy may develop bile stasis due to the absence of a “pumping” effect of the GB. These patients also lost the storage function of their GBs, which resulted in larger CBD size and more sizeable stone formation [13]. Many previous studies have reported that a larger bile duct and large bile duct stones are proven risk factors for recurrent bile duct stones [1, 13, 14].
Gallstones primarily comprise cholesterol and bile pigments. In studies focusing on patients from Western countries, GB stones are mainly composed of cholesterol (consisting of >50 % cholesterol) [15]. In addition, most of the CBD stones are secondary, resulting from the passing of gallstones, and primary CBD stones are seen less frequently in Western countries. However, the incidence of primary CBD stones, which is not associated with gallstones, is more frequent among Asians [9]. Bilirubinate stone is the predominant composition of CBD stone in Asia [16]. Therefore, cholecystectomy after EST with stone extraction may be not a preferable strategy for reducing the incidence of CBD stones among Asians.
Consequently, we should carefully select patients for additional cholecystectomy after EST with stone extraction. We conducted a subgroup analysis of characteristic of initial CBD stones. Although, the sample size of the GB in situ group was relatively small, we found that all of two patients with cholesterol CBD stones had recurrent cholecystitis during follow-up period. However, the recurrent cholecystitis rate was low in brown or black pigment CBD stones (12.9 and 18.8 %, respectively). Further studies to investigate the risk factors for additional cholecystitis after EST are warranted. Perhaps, in the future, we will perform a tailored cholecystectomy after EST with CBD stone extraction.
There are some limitations to our study. First, many patients in one arm of the study crossed over to the other arm, which interfered with the interpretation of our results. However, this phenomenon was a real practical effect. Elderly patients with more comorbidity do not undergo surgery, such as cholecystectomy, and in our study, the patients in the cholecystectomy group were significantly younger than those who had their GB left in situ (as-treated analysis, 59.5 ± 13.3 vs. 67.6 ± 10.7, p = 0.002). Second, the follow-up period was relatively short, but considering that most choledocholithiasis related biliary events occur up to 2–4 years after EST [3, 17], we suggest a long follow-up duration would not significantly change our result. Third, we may have underestimated the rate of certain biliary events, such as GB colic. In contrast with cholecystitis, which is easily diagnosed by imaging and physical examinations, GB colic is a relative subjective symptom and can improve by itself. The rate of additional GB related biliary events may be higher than our results show.
Conclusions
Cholecystectomy after EST for bile duct stones is not needed to reduce additional recurrent cholangitis. We suggest that additional cholecystectomy, after EST with for bile duct stones, should be limited to the patients with symptomatic gallstone. In addition, further studies to investigate the risk factors for additional cholecystitis after EST are warranted.
References
Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H (2003) Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut 52:116–121
Sugiyama M, Atomi Y (2002) Risk factors predictive of late complications after EST for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 97:2763–2767
Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccala G, Perri V (2002) Long-term follow-up of patients after EST for choledocholithiasis, and risk factors for recurrence. Endoscopy 34:273–279
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, Utsunomiya N, Ikeda S (1998) Long-term consequence of EST for bile duct stones. Gastrointest Endosc 48:465–469
Prat F, Malak NA, Pelletier G, Buffet C, Fritsch J, Choury AD, Altman C, Liguory C, Etienne JP (1996) Biliary symptoms and complications more than 8 years after EST for choledocholithiasis. Gastroenterology 110:894–899
Lau JY, Leow CK, Fung TM, Suen BY, Yu LM, Lai PB, Lam YH, Ng EK, Lau WY, Chung SS, Sung JJ (2006) Cholecystectomy or GB in situ after EST and bile duct stone removal in Chinese patients. Gastroenterology 130:96–103
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, Boerma EJ, Obertop H, Huibregtse K, Gouma DJ (2002) Wait-and-see policy or laparoscopic cholecystectomy after EST for bile-duct stones: a randomised trial. Lancet 360:761–765
Lai KH, Lin LF, Lo GH, Cheng JS, Huang RL, Lin CK, Huang JS, Hsu PI, Peng NJ, Ger LP (1999) Does cholecystectomy after EST prevent the recurrence of biliary complications? Gastrointest Endosc 49:483–487
Tazuma S (2006) Gallstone disease: epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 20:1075–1083
Hazzan D, Geron N, Golijanin D, Reissman P, Shiloni E (2003) Laparoscopic cholecystectomy in octogenarians. Surg Endosc 17:773–776
Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ (2001) Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc 15:700–705
Bingener-Casey J, Richards ML, Strodel WE, Schwesinger WH, Sirinek KR (2002) Reasons for conversion from laparoscopic to open cholecystectomy: a 10-year review. J Gastrointest Surg 6:800–805
Tsai TJ, Lai KH, Lin CK, Chan HH, Wang EM, Tsai WL, Cheng JS, Yu HC, Chen WC, Hsu PI (2012) The relationship between GB status and recurrent biliary complications in patients with choledocholithiasis following endoscopic treatment. J Chin Med Assoc 75:560–566
Ohashi A, Tamada K, Wada S, Hatanaka H, Tomiyama T, Tano S, Nakazawa K, Sugano K (2009) Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc 21:73–77
Carey MC (1993) Pathogenesis of gallstones. Am J Surg 165:410–419
Tsai WL, Lai KH, Lin CK, Chan HH, Lo CC, Hsu PI, Chen WC, Cheng JS, Lo GH (2005) Composition of common bile duct stones in Chinese patients during and after EST. World J Gastroenterol 11:4246–4249
Bergman JJ, van der Mey S, Rauws EA, Tijssen JG, Gouma DJ, Tytgat GN, Huibregtse K (1996) Long-term follow-up after EST for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc 44:643–649
Disclosures
Jun Heo, Min Kyu Jung, and Chang Min Cho have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heo, J., Jung, M.K. & Cho, C.M. Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones?. Surg Endosc 29, 1574–1579 (2015). https://doi.org/10.1007/s00464-014-3844-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3844-8