Abstract
Coronary artery disease (CAD) remains the leading global public health burden in cardiovascular diseases. Atherosclerosis is a primary mechanism to cause CAD with the contribution of epidemiological, traditional, genetic, and epigenetic risk factors. Statins, prescribed drugs for lowering of cholesterol levels, also have pleiotropic effect on oxidative stress, inflammation, apoptosis, etc. Reactive oxygen species (ROS)-induced oxidative stress associates with risk factors and participates in initiation and progression of disease. ROS molecules generated as superoxides (O2•ˉ), singlet/triplet oxygen, peroxides (H2O2, ONOO−), and hydroxyl radicals (HO•) via reactions catalyzed by endothelial nitric oxide synthase, myeloperoxidase, NADPH oxidase, and xanthine oxidase enzyme are encoded by eNOS, MPO, NOX, and XO genes, respectively. Polymorphisms in eNOS, MPO, NOX, and XO genes influence the expression and attributes to interindividual variation in response to statin drugs. Differential response to statin drug insights into emerging of pharmacogenetic studies to understand the genetic makeup and treat the patient with suitable drug and dose. In clinical practice, pharmacogenetic approach toward oxidative stress is a future emerging trend in personalized medicine development.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
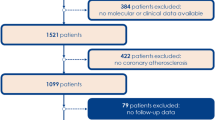
Coronary artery disease (CAD) is the foremost leading cause of cardiovascular diseases (CVD), and it is estimated that the CVD annual deaths may rise from 17.5 million to 22.2 million from 2012 to 2030 [1]. In India, CAD is the second rising burden among the noncommunicable diseases, and the occurrence of ischemic heart disease is increased to 8.7% from 3.7% since 1990 to 2016 [2].
Coronary atherosclerosis is the chief underlying mechanism of the coronary artery disease. Atherosclerosis is preceded by fatty streak formation, accumulation of lipids and lymphocytes, inflammation, and thrombosis. Atherosclerotic plaque narrows the lumen of coronary artery and diminishes blood flow to the myocardium [3, 4]. CAD is a multifactorial disease influenced by epidemiological, traditional, and novel risk factors for its initiation and development [5,6,7]. Recent studies also implicate the importance of genetic and epigenetic factors in the pathophysiology of coronary artery disease. Evidences suggest oxidative stress (OS) is a key contributor to the initiation and exacerbation of atherosclerosis [8, 9] (Fig. 26.1).
Reactive oxygen species (ROS) are generated endogenously by mitochondria, peroxisomes, endoplasmic reticulum, and phagocytes and exogenously by cigarette smoking, ultraviolet rays, radiation, pesticides, alcohol, and metals as superoxides (O2•ˉ), singlet/triplet oxygen, peroxides (H2O2, ONOO−), hydroxyl radicals (HO•), etc. [10]. Increased levels of ROS have various effects including endothelial dysfunction by loss of nitric oxide (NO) activity, increased lipid peroxidation by regulation of oxidized low-density lipoprotein (oxLDL) production, inflammation by NF-kβ activation, and thrombosis by vascular smooth muscle cell apoptosis [8]. Regulation of ROS production is a potential mechanism to control CAD initiation and progression.
Statins (hydroxymethylglutaryl coenzyme A reductase inhibitors) are common drugs used for the treatment of coronary artery disease [11]. These drugs significantly reduce the cholesterol levels by competitively inhibiting hydroxymethylglutaryl coenzyme A reductase (HMGCR) enzyme in hepatic cholesterol biosynthetic (mevalonate) pathway [12]. In clinical practice, statins show primarily cholesterol-dependent and additionally cholesterol-independent (pleiotropic) beneficial effects in CAD patients [13]. Cholesterol-independent beneficial effects include antioxidant, anti-inflammatory, anti-angiogenic, and anti-apoptotic activities [14, 15].
However, pharmacogenetic studies revealed that there is a variability in clinical response to statin treatment in CAD patients depending upon their genetic variations and expression of genes involved in absorption, transportation, and metabolic pathways. Genetic variations in CYP, ABC, Apo, IL family genes, HMGCR, PCSK9, LDLR, SLCO1B1, ACE, CETP, SREBP1, MMP, eNOS, NOX, XO, MPO, etc. genes are significantly affecting pharmacokinetics and dynamic properties of statins [14, 15]. Pharmacogenetic investigation insights into response to statin drug and doses and novel treatment strategies in CAD patients based on the genetic makeup of an individual. The present chapter is focused to discuss the impact of oxidative stress-associated candidate gene polymorphisms and their relative expression on efficacy of statin drugs in the treatment of coronary artery disease.
2 Oxidative Stress in Atherosclerosis
Oxidative stress is a form of imbalance between oxidants (ROS) and antioxidants of cells. Oxygen (O2) is a major molecule for all the metabolic processes and generates as free radical by reduction. Enzymatic and non-enzymatic reactions, auto-oxidation, electron transport chain, etc. are the major sources for superoxide generation by transferring an electron to molecular oxygen [16].
-
Enzymatic and non-enzymatic reaction
-
Auto-oxidation
Accumulating evidence suggests that various metabolic pathways including enzymes like endothelial nitric oxide synthase (eNOS), myeloperoxidase (MPO), NOX family enzymes (NOXs), xanthine oxidase (XO), etc are involved in the ROS production and imbalance between oxidants and antioxidants resulting in oxidative stress [10, 17,18,19,20].
Increased ROS has a vital role in initiation and progression of lesions at coronary arteries, for example, superoxide radical reacts with NO• forming peroxynitrite (ONOO−) which consequently reduces the bioavailability of nitric oxide (NO). In addition to superoxides, NO• reacts with hydroxyl (HO•) and lipid radicals (LO• and LOO•) forming OLNO and LOONO, respectively [10]. Peroxynitrite inactivates metal-centric eNOS enzymes, mitochondrial enzymes, and creatinine kinase and activates MMPs, NF-kβ, PARP, etc. by cysteine oxidation attributing to the pathology of CAD [21].
Initially, ROS modifies phospholipids by lipid peroxidation and results in the formation of oxidized LDL (oxLDL). Further OxLDL activates immune cells such as T cells, dendritic cells, monocytes, and macrophages and evokes the synthesis of inflammatory cytokines like IL-1, 6, TNFα, etc. These OxLDL molecules are taken up by macrophage receptors CD36, scavenger receptor class A, and lectin-like oxLDL receptor-1 and develop into foam cells and further trigger the formation of thrombus in the arterial layers as plaque [22, 23]. The plaque fibrous cap made up of VSMCs, collagen, proteoglycans, and elastin. Apoptosis of VSMCs and macrophages ruptures the fibrous cap and releases thrombosis into the blood stream and obstructs the blood flow to the myocardium [3, 8, 24].
3 Statins (Hydroxymethylglutaryl Coenzyme A (HMGCoA) Reductase Inhibitors)
Statin drugs are commercially approved in 1987 by the Food and Drug Administration, USA; these drugs act as HMGCoA analogues to inhibit the HMGCoA reductase enzyme at mevalonate pathway and regulate the cholesterol biosynthesis in hepatocytes. As per the 2013 ACC/AHA Guidelines, statin therapy is the most predominant treatment to patients with increased CAD risk [25]. Lovastatin is the first commercialized statin in the market. Based on the synthesis, statins are synthetic and semisynthetic statins. Synthetic statins include fluvastatin, atorvastatin, rosuvastatin, and pitavastatin, whereas semisynthetic statins include mevastatin, lovastatin, simvastatin, and pravastatin (Fig. 26.2) [26]. Among these, atorvastatin and rosuvastatin are worldwide chief drugs to treat CAD patients to reduce cholesterol levels.
3.1 Cholesterol Biosynthesis and Its Inhibition by Statins
Cholesterol biosynthesis by mevalonate pathway includes mevalonate, isopentyl phosphate, squalene, and lanosterol synthetic reactions. Mevalonate pathway converts acetyl coenzyme A to sterol (squalene) and non-sterol (farnesylated pyrophosphate and geranylgeranyl pyrophosphate) isoprenoids. Sterol isoprenoids participate in cholesterol synthesis while non-sterol in Rho, Ras, Rab, and nuclear laminin synthesis [27]. HMGCoA to mevalonate reduction is a rate-limiting step, catalyzed by HMGCR enzyme (Fig. 26.3). Statins are class of drugs designed to bind active site of HMGCoA reductase (HMGCR) and inhibit the enzyme activity in cholesterol biosynthetic pathway. Three decades of research and clinical studies established that statins have also antioxidant, anti-inflammatory, anti-angiogenic, and anti-apoptotic activities as pleiotropic effects [28].
4 Statins and Oxidative Stress
Statins apart from lowering the LDL also have other pleiotropic effects like regulation of genes involved in ROS production and their expression by inhibiting various pathways [28,29,30]. Endothelial nitric oxide synthase (eNOS), myeloperoxidase (MPO), nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX), and xanthine oxidase (XO) genes are associated with reactive oxygen intermediate production. Studies show that genetic variations in these genes and their expression attribute to the interindividual differences in the efficacy of statins [31, 32]. The pharmacogenetic implications of statins on regulation of genes involved in oxidative stress are summarized as below:
4.1 Endothelial Nitric Oxide Synthase (eNOS) Gene
Endothelial nitric oxide synthase (NOS3/eNOS) gene located on chromosome 7q36.1 with 28 exons encodes endothelial nitric oxide synthase enzyme. eNOS enzyme couples with cofactors tetrahydrobiopterin (BH4) and oxygen to produce nitric oxide (NO) by oxidizing L-arginine to L-citrulline (Fig. 26.4). Coupled eNOS inhibits endothelial leukocyte adhesion, platelet aggregation, and VSMC migration and proliferation to prevent atherogenesis [33, 34]. Previous reports suggested that uncoupled eNOS generates superoxides (O2•ˉ) which react with NO and form peroxynitrite (ONOO−) and inactivates NO [35, 36]. Endothelial dysfunction is also due to downregulation of eNOS expression in endothelial cells [37].
Studies evidenced that the statins attribute to upregulate the expression of endothelium nitric oxide synthase gene by extending half-life of mRNA [38], inhibiting mevalonate pathway and Rho kinase activity [39,40,41]. In addition, statins activate phosphatidylinositol 3-kinase signal (PI3K)-Akt pathway to enhance the bioavailability of nitric oxide [28].
In our earlier study, we have reported significantly higher levels of nitric oxide and malondialdehyde (MDA) levels in CAD patients [37, 42]. Further when CAD patients were treated with ATV 40 mg/day for 6 months, there was a significant reduction in NOx and MDA levels in both men and women (unpublished data). Another study by Kureishi et al. suggested that simvastatin and pravastatin increase Akt serine 473 phosphorylation in endothelial cells to produce NO, which leads to the improvement of endothelium function [43]. Besides cholesterol biosynthesis inhibition, statins also inhibit GTP binding proteins Rho/Rho kinase, Ras, and Rac synthesis in mevalonate pathway. Inhibition of these proteins decrease VSMC contraction and oxidative stress and increases NO bioavailability, which are favorable factors for the efficacy of statins in treatment [44].
Pharmacogenetic studies suggested that fluvastatin and atorvastatin are significantly increasing eNOS gene expression in endothelial cells by regulating transcriptional activity and mRNA stability. It has been reported that RPA1 binds to the promoter of eNOS to repress the expression and this activity of RPA1 is regulated by statin drugs [45]. Studies reporting functional implications of eNOS gene promoter -786T>C polymorphism have been found that the individual with CC genotype has lower NO levels compared to TT genotype [29, 45].
Abe et al. treated human umbilical vein endothelial cells (HUVECs) with fluvastatin and observed that the cells with eNOS -786CC genotype have improved eNOS mRNA levels [31]. Nagassaki et al. treated eNOS -786TT and -786CC genotype subjects with 10 mg/day atorvastatin and placebo for 14 days. Interestingly they found that individuals with CC genotype have significantly reduced nitrite levels compared to TT genotype in subjects treated with ATV. Consequently nitrite level reduction in subjects with CC genotype implies the importance of genotype in modulating the response to drug [32]. These in vitro and clinical studies reported fluvastatin and atorvastatin to be associated with reduction of elevated levels of plasma nitrite concentrations in CC genotype individuals. These results indicate statins have capacity to restore diminished nitric oxide production in those carrying CC genotype of -786T>C polymorphism and are good responders for statin drug treatment [31, 32].
4.2 Myeloperoxidase (MPO) Gene
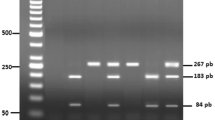
Myeloperoxidase (MPO) gene localized at 17q22 with 12 exons translates as myeloperoxidase enzyme. It is synthesized as translational product with 80 kDa, subsequently converts into Apopro MPO (90 kDa) and proMPO (90 kDa), and undergoes proteolytic processing to produce homodimeric matured MPO (74 kDa) [46]. MPO enzyme is present in neutrophils, monocytes, macrophages, etc. and a key contributor for inflammation in cardiovascular diseases. MPO catalyzes various reactions in biological system and generates reactive oxygen species, cytotoxic hypochlorous acid, tyrosyl radical (Fig. 26.5) [6, 47, 48].
Studies on MPO gene polymorphisms have shown association with the risk of coronary artery disease. MPO promoter polymorphic variants potentially influence transcription factors binding and MPO levels. Yan Wang et al., in their meta-analysis study, have observed that the MPO -463G/A and -129G/A polymorphisms regulate the gene expression and A allele of -463G/A and A allele of -129G/A polymorphisms are associated with the lower levels of MPO [49].
Evidences suggest that the different concentrations of lovastatin, simvastatin, atorvastatin, and pravastatin are significantly downregulating the expression of MPO mRNA. Kumar et al. reported that 50 μM of lovastatin and simvastatin are showing greatest effect with 194 ± 8-fold and 45 ± 5-fold reduction in MPO mRNA expression, respectively, in peripheral blood monocytes [47]. Ndrepepa et al. reported that the statins are significantly (p < 0.005) reducing the MPO levels by regulating expression of MPO gene in acute coronary syndrome patients [50]. Sygitowicz et al. treated acute myocardial infarction (MI) patients with ATV 40 mg/40 days and found significantly decreased MPO gene expression in 60.5% of MI patients. The differences in the efficacy of ATV might be due to the promoter polymorphism of MPO gene [51].
4.3 NADH/NADPH Oxidase (NOX) Gene
Nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX 1) gene, located at Xq22.1 with 14 exons, encodes NADPH family of enzymes. NOX enzyme is involved in the production of reactive oxygen species, i.e., superoxide, in the vascular system (Fig. 26.6).
NOX isoforms and component subunits are shown in Table 26.1. Among NOX isoforms, NOX1, 2, 4, and 5 isoforms catalyze to release superoxide/hydrogen peroxide influencing proliferation, differentiation, endothelial impairment, and vascular structure in coronary atherosclerosis [52, 53].
NOX enzyme has complex, membrane-bound subunits gp91phox and p22phox; cytosolic subunits p40phox, p47phox, and p67phox; and small GTP binding protein Rac to form complexes and transfer electrons in biological system as represented in Fig. 26.7 [54]. NOX1, 2, and 5 are expressed in endothelial cells, VSMCs, and NOX4 in vascular cell walls [20, 55].
Guzik et al. measured the NOX-produced superoxide in blood vessels, which reacts with nitric oxide and forms peroxynitrite, and found a proportionately deficit NO bioavailability leading to endothelial impairment in atherosclerosis [56]. Zhang et al. evidenced that the mRNA expression of NOX subunits was significantly higher in endothelial progenitor cells in CAD. Out of all subunits, p47phox and p22phox regulate the activity of NADPH for production of superoxide radicals and hydrogen peroxide. Activation of p47phox occurs when it is translocated from cytosol to plasma membrane of endothelial cells, and it was observed that the activation rate is enhanced in CAD patients (p < 0.05) [53, 57]. The genes encoding NOX enzyme subunits are shown in Table 26.2.
Genetic variations in genes encoding NOX subunits influence the activity of enzyme and generation of reactive oxygen species. One of the chief components of NOX is p22phox, encoded by CYBA/p22phox gene located at 16q24.2 with seven exons. Cahilly et al. suggested that the T-allele of C242T polymorphism in p22phox gene is significantly associated with 3- to 5-fold loss in minimum lumen diameter and disease progression [58]. Ito et al. observed a high frequency of T allele of C242T polymorphism in CVD patients than the controls in Japanese population [59].
Meta-analysis conducted by Xu et al. included functional studies which suggested the association of p22phox 640G allele with mRNA stability and processing in CAD patients and also found significant decrease in ROS formation. Further it has been suggested that the individuals with 640G allele might show protection against CAD [60, 61]. Antioxidant capacity of statins includes the regulation of ROS production in cells participating in coronary atherosclerotic process. A number of studies evidenced that the statins are reducing the ROS production by inhibiting the NOX enzyme and Rac. Hamilton et al. evidenced 10/20 mg/day atorvastatin (ATV) reduces the Rac GTPases on membranes of platelet in hyperlipidemia patients, which may reduce the activity of NOX [62].
Antoniades et al. treated preoperative coronary artery bypass-grafted patients with 40 mg/day atorvastatin for 3 days to find the redox rate in vein graft and found significant reduction in basal and vascular NOX stimulating O2•ˉ and Rac1 activation in vein grafts. ATV treatment has no impact on NOX1/2/4 protein levels but significantly reduced Rac1 and p67phox of NOX [63]. Studies have indicated that atorvastatin and simvastatin were involved in downregulating the expression of Rac1 gene [30]. Furthermore, evidences by Inoue et al. have shown that HUVECs treated with different concentrations of fluvastatin, simvastatin, pravastatin, and cerivastatin showed a significantly downregulated expression of p22phox mRNA and decreased p47phox protein levels in response to fluvastatin and simvastatin [64].
4.4 Xanthine Oxidase (XO) Gene
Xanthine oxidase (XO)/xanthine dehydrogenase (XDH) gene located at 2p23.1 with 37 exons, encodes xanthine oxidase enzyme. It exists as a homodimer with approximately 290 kDa molecular mass [65]. Xanthine oxidase catalyzes the oxidation of hypoxanthine to xanthine, followed by xanthine to uric acid in purine metabolism (Fig. 26.8). In the process of oxidation, XO reduces molecular oxygen (O2) to superoxide radical (O2•ˉ) and peroxides (H2O2). Chung et al. reported that XO is highly expressed in endothelial, epithelial, and polymorphonuclear cells [66]. Previous studies evidenced that superoxides and peroxides were involved in a variety of clinicopathological conditions including endothelial dysfunction, elevated uric acid levels, and chemoattractant for neutrophils in coronary artery disease [66, 67]. Landmesser et al. evidenced an enhanced expression of XO protein and subsequent XO-dependent endothelial superoxide production in response to the stimulus of angiotensin II hormone in bovine aortic endothelial cells [68].
Kudo et al. functionally characterized various polymorphisms in XO gene and observed the loss of enzyme activity for subjects with 445C>T (Arg149Cys) and 2729C>A (Thr910Lys) variations and decreased enzyme activity for 1663C>T (Pro555Ser), 1820G>A (Arg607Gln), 1868C>T (Thr623Ile), 2727C>A (Asn909Lys), 3449C>G (Pro1150Arg), and 3953G>A (Cys1318Tyr) [65].
Recent study on rs2073316 (g.31583C>T), rs1054889 (g.85304C>T) and rs1042039 (g.84306A>G) polymorphisms of XDH gene revealed an association with hypertension. Frequency of C allele for rs1042039 is higher, while C allele of rs1054889 and A allele of rs2073316 are significantly lower in hypertensives compared to controls. These polymorphisms may regulate the expression of XDH gene and might be associated with hypertension in Chinese population [69]. CAD patients had higher levels of XO protein and activity [68]; several studies evidenced that XO inhibition improved the endothelial function and decreased the free radical and uric acid production levels [70].
Greig et al. reported that 4 weeks of atorvastatin 20 mg/day treatment independently decreased the levels of MDA, uric acid and flow-dependent endothelial-mediated vasodilation in heart failure patients. Possibly statins might have decreased the expression of endothelial XO by inhibiting Rac1 or NOX and transcription of XO gene [70]. In addition, simvastatin prevented 50% superoxide anion production by angiotensin II-dependent ROS production in rats, which plays a pivotal role in XO activity and endothelial dysfunction [71]. The above reports suggest that increased expression of XO and angiotensin II genes might be key factors for the stimulation of enhanced ROS production to initiate the atherosclerotic plaque and inhibition of these genes may be additional therapeutic targets of statins.
5 Conclusion and Future Directions
Coronary artery disease is a devastating disease, and oxidative stress plays a crucial role in initiation and progression of disease. Statins, the prescribed drugs for lowering of cholesterol levels, have also other pleiotropic effects on oxidative stress, inflammation, apoptosis, etc. The generation of oxidative stress is influenced by the genetic variations in eNOS, MPO, XO, NOX, etc. Differential response to statin drug insights into emerging of pharmacogenetic studies to understand the genetic makeup and treat the patient with suitable drug and dose. In clinical practice, pharmacogenetic approach toward oxidative stress is a future emerging trend in personalized medicine development.
References
World Health Organization (2016) Technical package for cardiovascular disease management in primary health care. Hearts 76
MoHFW (2017) India: health of the nation’s states. Government report, pp 70–75
Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 352:1685–1695
Hansson GK, Libby P, Tabas I (2015) Inflammation and plaque vulnerability. J Intern Med 278:483–493
Mack M, Gopal A (2016) Epidemiology, traditional and novel risk factors in coronary artery disease. Heart Fail Clin 12:1–10
Teng N, Maghzal GJ, Talib J, Rashid I, Lau AK, Stocker R (2017) The roles of myeloperoxidase in coronary artery disease and its potential implication in plaque rupture. Redox Rep 22:51–73
Libby P, Rocha VZ (2018) All roads lead to IL-6: a central hub of cardiometabolic signaling. Int J Cardiol 259:213–215
Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK (2018) Reactive oxygen species in metabolic and inflammatory signaling. Circ Res 122:877–902
Vichova T, Motovska Z (2013) Oxidative stress: predictive marker for coronary artery disease. Exp Clin Cardiol 18:88–91
Cai H, Harrison DG (2000) The role of oxidant stress. Circ Res 87:840–844
Reiner, De Backer G, Fras Z, Kotseva K, Tokgözoglu L, Wood D, De Bacquer D (2016) Lipid lowering drug therapy in patients with coronary heart disease from 24 European countries – findings from the EUROASPIRE IV survey. Atherosclerosis 246:243–250
Catapano AL, Graham I, De Backer G et al (2016) 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 37:2999–3058l
Oesterle A, Laufs U, Liao JK (2017) Pleiotropic effects of statins on the cardiovascular system. Circ Res 120:229–243
Kitzmiller JP, Binkley PF, Pandey SR, Suhy AM, Baldassarre D, Hartmann K (2013) Statin pharmacogenomics: pursuing biomarkers for predicting clinical outcomes. Discov Med 16:45–51
Mangravite LM, Thorn CF, Krauss RM (2006) Clinical implications of pharmacogenomics of statin treatment. Pharm J 6:360–374
Phaniendra A, Jestadi DB, Periyasamy L (2015) Free radicals: properties, sources, targets, and their implication in various diseases. Indian J Clin Biochem 30:11–26
Panth N, Paudel KR, Parajuli K (2016) Reactive oxygen species: a key hallmark of cardiovascular disease. Adv Med 2016:1–12
Madamanchi NR, Vendrov A, Runge MS (2005) Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol 25:29–38
Ushio-fukai M, Zafari AM, Fukui T, Ishizaka N, Griendling KK (1996) p22 phox is a critical component of the superoxide-generating NADH/NADPH oxidase system and regulates angiotensin II- induced hypertrophy in vascular smooth muscle cells ∗. J Biol Chem 271:23317–23321
Sorescu D, Weiss D, Lassègue B et al (2002) Superoxide production and expression of Nox family proteins in human atherosclerosis. Circulation 105:1429–1435
Pacher P, Beckman JS, Liaudet L (2007) Nitric oxide and peroxynitrite in health and disease. Physiol Rev 87:315–424
Chistiakov DA, Melnichenko AA, Myasoedova VA, Grechko AV, Orekhov AN (2017) Mechanisms of foam cell formation in atherosclerosis. J Mol Med 95:1153–1165
Yu XH, Fu YC, Zhang DW, Yin K, Tang CK (2013) Foam cells in atherosclerosis. Clin Chim Acta 424:245–252
Mishra TK, Mishra C, Das B (2013) An approach to the classification, diagnosis and management of vulnerable plaque. J Indian Coll Cardiol 3:57–66
Stone NJ, Robinson JG, Lichtenstein AH et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol 63:2889–2934
Endo A (2010) A historical perspective on the discovery of statins. Proc Jpn Acad Ser B 86:484–493
Singh P, Saxena R, Srinivas G, Pande G, Chattopadhyay A (2013) Cholesterol biosynthesis and homeostasis in regulation of the cell cycle. PLoS One 8(3):e58833. https://doi.org/10.1371/journal.pone.0058833
Liao JK, Laufs U (2005) Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol 45:89–118
Oliveira-Paula GH, Lacchini R, Tanus-Santos JE (2017) Clinical and pharmacogenetic impact of endothelial nitric oxide synthase polymorphisms on cardiovascular diseases. Nitric Oxide Biol Chem 63:39–51
Laufs U, Kilter H, Konkol C, Wassmann S, Bohm M, Nickenig G (2002) Impact of HMG CoA reductase inhibition on small GTPases in the heart. Cardiovasc Res 53:911–920
Abe K, Nakayama M, Yoshimura M et al (2005) Increase in the transcriptional activity of the endothelial nitric oxide synthase gene with fluvastatin: a relation with the -786T>C polymorphism. Pharmacogenet Genomics 15:329–336
Nagassaki S, Sertório JTC, Metzger IF, Bem AF, Rocha JBT, Tanus-Santos JE (2006) eNOS gene T-786C polymorphism modulates atorvastatin-induced increase in blood nitrite. Free Radic Biol Med 41:1044–1049
Gimbrone MA, García-Cardeña G (2016) Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res 118:620–636
Verhaar MC (2004) Free radical production by dysfunctional eNOS. Heart 90:494–495
Sullivan JC, Pollock JS (2006) Coupled and uncoupled NOS: separate but equal? Uncoupled NOS in endothelial cells is a critical pathway for intracellular signaling. Circ Res 98:717–719
Matsubara K, Higaki T, Matsubara Y, Nawa A (2015) Nitric oxide and reactive oxygen species in the pathogenesis of preeclampsia. Int J Mol Sci 16:4600–4614
Kumar GR, Spurthi KM, Kumar GK et al (2016) Genetic polymorphisms of eNOS (-786T/C, Intron 4b/4a & 894G/T) and its association with asymptomatic first degree relatives of coronary heart disease patients. Nitric Oxide Biol Chem 60:40–49
Laufs U, Liao JK (1998) Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem 273:24266–24271
Laufs U, La Fata V, Plutzky J, Liao JK (1998) Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation 97:1129–1135
Ruan F, Zheng Q, Wang J (2012) Mechanisms of bone anabolism regulated by statins. Biosci Rep 32:511–519
Wolfrum S, Dendorfer A, Rikitake Y, Stalker TJ, Scalia R, Dominiak P, Liao JK (2009) Inhibition of rho-kinase leads to rapid activation of phosphatidylinositol 3-kinase/protein kinase Akt and cardiovascular protection. Arterioscler Thromb Vasc Biol 24:1842–1847. NIH Public Access
Gundapaneni KK, Galimudi RK, Kondapalli MS, Gantala SR, Mudigonda S, Padala C, Shyamala N, Sahu SK, Hanumanth SR (2017) Oxidative stress markers in coronary artery disease patients with diabetes mellitus. Int J Diab Dev Ctries 37:190–194
Kureishi Y, Luo Z, Shiojima I, Bialik A, Fulton D, David J, Sessa WC, Walsh K (2010) The HMGCoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med 6:1004–1010. NIH Public Access
Shimokawa H, Takeshita A (2005) Rho-kinase is an important therapeutic target in cardiovascular medicine. Arterioscler Thromb Vasc Biol 25:1767–1775
Silva PS, Lacchini R, Gomes Vde A, Tanus-Santos JE (2011) Pharmacogenetic implications of the eNOS polymorphisms for cardiovascular action drugs. Arq Bras Cardiol 96:e27–e34
Grishkovskaya XI, Paumann-Page M, Tscheliessnig R et al (2017) Structure of human promyeloperoxidase (proMPO) and the role of the propeptide in processing and maturation. J Biol Chem 292:8244–8261
Kumar AP, Reynolds WF (2005) Statins downregulate myeloperoxidase gene expression in macrophages. Biochem Biophys Res Commun 331:442–451
Zhang R, Brennan ML, Shen Z, MacPherson JC, Schmitt D, Molenda CE, Hazen SL (2002) Myeloperoxidase functions as a major enzymatic catalyst for initiation of lipid peroxidation at sites of inflammation. J Biol Chem 277:46116–46122
Wang Y, Chen X-Y, Wang K, Li S, Zhang X-Y (2017) Myeloperoxidase polymorphism and coronary artery disease risk: a meta-analysis. Medicine (Baltimore) 96:e7280
Ndrepepa G, Braun S, Schömig A, Kastrati A (2011) Impact of therapy with statins, beta-blockers and angiotensin-converting enzyme inhibitors on plasma myeloperoxidase in patients with coronary artery disease. Clin Res Cardiol 100:327–333
Sygitowicz G, Maciejak A, Piniewska-Juraszek J, Pawlak M, Gora M, Burzynska B, Dluzniewski M, Opolski G, Sitkiewicz D (2015) Interindividual variability of atorvastatin treatment influence on the MPO gene expression in patients after acute myocardial infarction. Acta Biochim Pol 63(1):89–95. https://doi.org/10.18388/abp.2015_1014
Touyz RM, Briones AM, Sedeek M, Burger D, Montezano AC (2011) NOX isoforms and reactive oxygen species in vascular health. Mol Interv 11:27–35
Kwok JMF, Ma CCH, Ma S (2013) Recent development in the effects of statins on cardiovascular disease through Rac1 and NADPH oxidase. Vasc Pharmacol 58:21–30
Maack C, Kartes T, Kilter H, Schäfers HJ, Nickenig G, Böhm M, Laufs U (2003) Oxygen free radical, release in human failing myocardium is associated with increased activity of Rac1-GTPase and represents a target for statin treatment. Circulation 108:1567–1574
Antonopoulos AS, Margaritis M, Shirodaria C, Antoniades C (2012) Translating the effects of statins: from redox regulation to suppression of vascular wall inflammation. Thromb Haemost 108:840–848
Guzik TJ, West NEJ, Black E, McDonald D, Ratnatunga C, Pillai R, Channon KM (2000) Vascular superoxide production by NAD(P)H oxidase: association with endothelial dysfunction and clinical risk factors. Circ Res 86:e85–e90
Zhang J, Wang M, Li Z, Bi X, Song J, Weng S, Fu G (2016) NADPH oxidase activation played a critical role in the oxidative stress process in stable coronary artery disease. Am J Transl Res 8:5199–5210
Cahilly C, Ballantyne CM, Lim DS, Gotto A, Marian AJ (2000) A variant of p22(phox), involved in generation of reactive oxygen species in the vessel wall, is associated with progression of coronary atherosclerosis. Circ Res 86:391–395
Ito D, Murata M, Watanabe K, Yoshida T (2000) C242T polymorphism of NADPH oxidase p22 PHOX gene and ischemic cerebrovascular disease in the Japanese population. Stroke 31(4):936–940
Xu Q, Yuan F, Shen X, Wen H, Li W, Cheng B, Wu J (2014) Polymorphisms of C242T and A640G in CYBA gene and the risk of coronary artery disease: a meta-analysis. PLoS One 9(1):e84251. https://doi.org/10.1371/journal.pone.0084251
Gardemann A, Mages P, Katz N, Tillmanns H, Haberbosch W (1999) The p22 phox A640G gene polymorphism but not the C242T gene variation is associated with coronary heart disease in younger individuals. Atherosclerosis 145:315–323
Hamilton PK, Hughes SMT, Plumb RD, Devine A, Leahey W, Lyons KS, Johnston D, McVeigh GE (2010) Statins have beneficial effects on platelet free radical activity and intracellular distribution of GTPases in hyperlipidaemia. Clin Sci 118:359–366
Antoniades C, Bakogiannis C, Tousoulis D et al (2010) Preoperative atorvastatin treatment in CABG patients rapidly improves vein graft redox state by inhibition of Rac1 and NADPH-oxidase activity. Circulation 122(11 Suppl):S66–S73. https://doi.org/10.1161/CIRCULATIONAHA.109.927376
Inoue I, Goto S, Mizotani K, Awata T, Mastunaga T, Kawai S, Nakajima T, Hokari S, Komoda T, Katayama S (2000) Lipophilic HMG-CoA reductase inhibitor has an anti-inflammatory effect: reduction of MRNA levels for interleukin-1beta, interleukin-6, cyclooxygenase-2, and p22phox by regulation of peroxisome proliferator-activated receptor alpha (PPARalpha) in primary e. Life Sci 67:863–876
Kudo M, Moteki T, Sasaki T, Konno Y, Ujiie S, Onose A, Mizugaki M, Ishikawa M, Hiratsuka M (2008) Functional characterization of human xanthine oxidase allelic variants. Pharmacogenet Genomics 18:243–251
Chung HY, Baek BS, Song SH, Kim MS, Huh JI, Shim KH, Kim KW, Lee KH (1997) Oxidation xanthine oxidase I [(reversible XOD ) Proteolys ~ Xant ~ ine]. Age (Omaha) 20:127–140
Zdrenghea M, Sitar-Tǎut A, Cismaru G, Zdrenghea D, Pop D (2017) Xanthine oxidase inhibitors in ischaemic heart disease. Cardiovasc J Afr 28:201–204
Landmesser U, Spiekermann S, Preuss C, Sorrentino S, Fischer D, Manes C, Mueller M, Drexler H (2007) Angiotensin II induces endothelial xanthine oxidase activation: role for endothelial dysfunction in patients with coronary disease. Arterioscler Thromb Vasc Biol 27:943–948
Wu B, Hao Y, Shi J et al (2015) Association between xanthine dehydrogenase tag single nucleotide polymorphisms and essential hypertension. Mol Med Rep 12:5685–5690
Greig D, Alcaino H, Castro PF et al (2011) Xanthine-oxidase inhibitors and statins in chronic heart failure: effects on vascular and functional parameters. J Heart Lung Transplant 30:408–413
Delbosc S, Cristol JP, Descomps B, Mimran A, Jover B (2002) Simvastatin prevents angiotensin II-induced cardiac alteration and oxidative stress. Hypertension 40:142–147
Acknowledgments
This work was supported by UGC, New Delhi, India: MRP-2013 (F.No.42-52/2013[SR]), BSR-Fellowship, CPEPA, and OU-DST-PURSE-II Programme (C-DST-PURSE- II/23/2017), ICMR-SRF (ID No. 2019-4183).
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Shyamala, N., Hanumanth, S.R. (2019). Pharmacogenetic Implications of Statin Therapy on Oxidative Stress in Coronary Artery Disease. In: Chakraborti, S., Dhalla, N., Dikshit, M., Ganguly, N. (eds) Modulation of Oxidative Stress in Heart Disease. Springer, Singapore. https://doi.org/10.1007/978-981-13-8946-7_26
Download citation
DOI: https://doi.org/10.1007/978-981-13-8946-7_26
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8945-0
Online ISBN: 978-981-13-8946-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)