Abstract
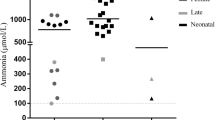
A female infant, weighing 2786 g, was born at 39 weeks gestational age with Apgar scores of 8 points at 1 min and 9 points at 5 min after birth. She had no family history of hereditary disorders. Although she had no medical problems at birth and consumed her mother’s breast milk, she developed fever with increased white blood cell counts (WBC: 22,070/μL) and C-reactive protein level (CRP: 1.2 mg/dL) at 2 days after birth. Bacterial infection was suspected, and she received antibiotic therapy. Subsequently, she developed jaundice, convulsions, and respiratory failure and required respiratory support. As the doctors were concerned about a risk of neonatal herpes infection, she received γ-globulin and acyclovir treatments. In addition, she developed mild acidosis and hyperammonemia >400 μg/dL (normal range: 30–80 μg/dL). Urea cycle disorders were suspected, and she was treated with arginine, sodium benzoate, and high glucose infusion. Unfortunately, her plasma ammonia level increased to 2000 μg/dL at 3 days after birth (Fig. 12.1), and she was transferred to a neonatal intensive care unit for treatment with hemodialysis and possible liver transplantation. Her blood ammonia levels gradually improved and normalized at 21 days after birth. Her blood glutamine, glutamic acid, glycine, aspartic acid, citrulline, and arginine levels were 3262 μmol/L (control: 416–740 μmol/L), 265 μmol/L (12–83 μmol/L), 705 μmol/L (140–427 μmol/L), 29 μmol/L (trace–7.2 μmol/L), trace (18–48 μmol/L), and 69 μmol/L (32–150 μmol/L), respectively. The results of the neonatal tandem mass spectrometry screening test for inherited metabolic diseases and analysis test for urinary orotic acid were negative. She was definitively diagnosed with carbamoyl phosphate synthetase 1 deficiency (CPSD) by identification of a mutation of the carbamoyl phosphate synthetase 1 gene (c.2339G>A and c.2945G>A). She underwent a living donor liver transplantation with her father as the donor at the age of 6 months. The subject is presently 7 years and 5 months old, attends primary school, and lives a stable life.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Case Report
A female infant, weighing 2786 g, was born at 39 weeks gestational age with Apgar scores of 8 points at 1 min and 9 points at 5 min after birth. She had no family history of hereditary disorders. Although she had no medical problems at birth and consumed her mother’s breast milk, she developed fever with increased white blood cell counts (WBC: 22,070/μL) and C-reactive protein level (CRP: 1.2 mg/dL) at 2 days after birth. Bacterial infection was suspected, and she received antibiotic therapy . Subsequently, she developed jaundice , convulsions, and respiratory failure and required respiratory support. As the doctors were concerned about a risk of neonatal herpes infection, she received γ-globulin and acyclovir treatments. In addition, she developed mild acidosis and hyperammonemia >400 μg/dL (normal range: 30–80 μg/dL). Urea cycle disorders were suspected, and she was treated with arginine, sodium benzoate, and high glucose infusion. Unfortunately, her plasma ammonia level increased to 2000 μg/dL at 3 days after birth (Fig. 12.1), and she was transferred to a neonatal intensive care unit for treatment with hemodialysis and possible liver transplantation. Her blood ammonia levels gradually improved and normalized at 21 days after birth. Her blood glutamine, glutamic acid, glycine, aspartic acid, citrulline , and arginine levels were 3262 μmol/L (control: 416–740 μmol/L), 265 μmol/L (12–83 μmol/L), 705 μmol/L (140–427 μmol/L), 29 μmol/L (trace–7.2 μmol/L), trace (18–48 μmol/L), and 69 μmol/L (32–150 μmol/L), respectively. The results of the neonatal tandem mass spectrometry screening test for inherited metabolic diseases and analysis test for urinary orotic acid were negative. She was definitively diagnosed with carbamoyl phosphate synthetase 1 deficiency (CPSD) by identification of a mutation of the carbamoyl phosphate synthetase 1 gene (c.2339G>A and c.2945G>A). She underwent a living donor liver transplantation with her father as the donor at the age of 6 months. The subject is presently 7 years and 5 months old, attends primary school, and lives a stable life.
2 Diagnosis
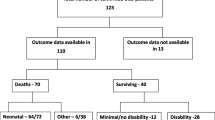
A medical doctor should correctly diagnose urea cycle disorders (UCDs) in patients developing hyperammonemia crises such as for the case described in the Case Report. A diagnostic flowchart for hyperammonemia is shown in Fig. 12.2. Encephalopathy associated with hyperammonemia in the neonatal period constitutes the most important clinical feature for diagnosis, although the late onset type can occur at any age. Other important diseases that present with hyperammonemia include mitochondrial disorders, fatty acid metabolism disorders, systemic sepsis, liver failure, and portosystemic shunt. Congenital metabolic disorders should be initially suspected in hyperammonemia without liver failure; however, cases with liver failure have also been reported, indicating the need for caution.
Diagnostic flowchart of urea cycle disorders. ARGD arginase 1 deficiency, ASLD argininosuccinate lyase deficiency, ASSD argininosuccinate synthetase deficiency, CPSD carbamoyl phosphate synthetase 1 deficiency, NAGSD N-acetyl glutamate synthetase deficiency, OTCD ornithine transcarbamylase deficiency
UCDs constitute diseases presenting with severe hyperammonemia, typically in the neonatal period, caused by congenital defects in the metabolic enzymes that comprise the urea cycle (urea synthesis pathway) (Nagata et al. 1991) (Table 12.1). UCDs are classified as rare diseases and estimated to have a prevalence of 1/50,000 births (Nagata et al. 1991) in Japan and 1/35,000 in the EU/USA (Batshaw et al. 2014).
The urea cycle is a metabolic pathway that converts ammonia to urea in the liver and excretes endogenous or exogenous nitrogen sources out of the body. The urea cycle comprises five enzymes, two of which, carbamoyl phosphate synthetase 1 (CPS1: EC 6.3.5.5) and ornithine transcarbamylase (OTC: EC 2.1.3.3), are present in the mitochondrial matrix, whereas the remaining three (argininosuccinate synthetase (ASS: EC 6.3.4.5), argininosuccinate lyase (ASL: EC 4.3.2.1), and arginase 1 (ARG: EC 3.5.3.1)), are present in the cytoplasm. Furthermore, N-acetyl glutamate synthetase (NAGS: EC 2.3.1.1) and at least two other transporter proteins are essential to urea cycle function (Fig. 12.3).
In UCDs, ammonia cannot be converted to urea and excreted from the body because of dysfunction in any of these enzymes; therefore, patients with UCDs develop hyperammonemia and present with neurological abnormalities including vomiting, ataxia, confusion, and irritability. In the absence of appropriate intervention, the patients will develop seizures , become comatose, and die. The various conditions may be classified according to symptoms and age as follows:
-
Presymptomatic, identified through family history analysis and screening tests
-
Neonatal onset , presenting with severe hyperammonemia during the neonatal period
-
Late onset , presenting with neurological symptoms or hyperammonemia after the neonatal period and deterioration of symptoms or severe hyperammonemia after a trigger such as infection or starvation
UCDs are further classified according to the affected enzyme/system as follows:
-
1.
Primary urea cycle disorders
Includes N-acetyl glutamate synthetase deficiency (NAGSD), carbamoyl phosphate synthetase deficiency (CPSD), ornithine transcarbamylase deficiency (OTCD), argininosuccinate synthetase (ASSD, type 1 citrullinemia), argininosuccinate lyase deficiency (ASLD), and arginase 1 deficiency (ARGD, argininemia)
-
2.
Secondary urea cycle disorders
Includes hyperornithinemia-hyperammonemia-homocitrullinuria (HHH) syndrome, lysinuric protein intolerance , citrin deficiency (type 2 citrullinemia), and ornithine aminotransferase deficiency (gyrate atrophy of choroid and retina)
3 Amino Acid Analysis
Amino acids profiling is useful for the diagnosis of UCDs, which allows the detection of an accumulation of precursor amino acids and a reduction in product amino acids resulting from and thereby specifying the defective enzyme. For example, in patients with OTCD, plasma glutamine, glutamate, and glycine levels should be increased, with a decrease in citrulline and arginine levels in the plasma and urine (Maestri et al. 1992; Berry and Steiner 2001). ARGD and ASLD can be differentiated by the concentrations of arginine and argininosuccinic acid, whereas hypercitrullinemia without elevated argininosuccinic acid is suggestive of ASSD. Decreased levels of citrulline and arginine with elevated urinary orotic acid are suggestive of OTCD, whereas reduced urinary orotic acid is suggestive of CPSD or NAGSD. HHH syndrome should be suspected with hyperammonemia associated with high blood ornithine and urinary homocitrulline. Accordingly, planning of pilot screening for UCDs in Japan using amino acids profiling is currently underway.
4 Urinary Orotic Acid
Orotic acid is effective for distinguishing between OTCD and CPSD (Fig. 12.4). Orotic acid is a heteroaromatic compound that was initially discovered in whey. Biochemically, orotic acid constitutes a biosynthetic intermediate of pyrimidine bases that is produced by dihydroorotate dehydrogenase from dihydroorotate and is converted to orotidine monophosphate by orotate phosphoribosyltransferase. Dihydroorotate is synthesized from carbamoyl phosphate and asparagine acid. This metabolic system for synthesis of pyrimidine bases is essential in all cells in the human body. Because the majority of OTC in human is expressed in the cytosol of hepatocytes with little in other cell types, orotic acid is considered to be synthesized consequent to the accumulation of carbamoyl phosphate in hepatocytes and excreted into the urine.
In UCDs, when the urinary orotic acid value is high, OTCD, ASSD, ASLD, and/or HHH syndrome should be suspected. In contrast, orotic acid is not elevated in CPSD. Notably, urinary orotic acid correlates with the clinical course and metabolic status in the body. In particular, urinary orotic acid excretion increases in allopurinol loading tests, which are performed to detect “non-symptomatic” female OTCD or select living donors for liver transplantation. However, the low sensitivity of these tests is a concerning issue of which clinicians should be aware.
5 Enzyme Activity
To directly interrogate enzyme function, hepatic tissue pathology is assessed, and the activity of urea cycle enzymes in the liver is measured. Specifically, the urea cycle is completed only in the liver with CPS, OTC, and NAGS expressed primarily in liver cells. Thus, it is essential to measure enzyme activity using liver tissue. Furthermore, because OTCD constitutes an X-linked genetic disorder, the enzyme activities in female patients with OTCD depend upon the location of the measured site in their liver, in accordance with the lyonization principle (i.e., will vary depending on the proportion of wild-type to mutant X chromosomes having undergone X-inactivation in the sample site).
6 Genetic Analysis
A definitive diagnosis is conducted through gene analysis using white blood cells. The sensitivity of genetic analysis in each country is approximately 80%, and genetic diagnosis in conjunction with prenatal diagnosis or other such means is essential. Although UCDs can often be classified with biochemical diagnostics, genetic analysis may be utilized for definitive diagnosis. For example, in the CPSD case discussed above, a compound heterozygous mutation in the CPS1 gene was identified.
7 Biochemical and Molecular Perspectives
In 1932, Krebs et al. reported that ornithine activates urea synthesis and described the urea (ornithine) cycle. Specifically, the urea cycle removes ammonia generated via proteolysis. Previously, it was considered that the urea cycle was restricted to animals. However, it has been reported that in some diatoms, the urea cycle is used to generate ammonia from fixed nitrogen, a phenomenon that is attracting considerable attention. This metabolism state does not exist in the human body; instead, ammonia in the body is thought to be generated by the following four routes:
-
1.
Ammonia production in the intestinal tract
Ammonia is produced through catabolism of glutamine by glutaminase (mucosal epithelial cells), glutamate dehydrogenase (GDH; small intestine), and bacterial deaminase (large intestine). Urea is also broken down by bacterial urease (large intestine), generating ammonia.
-
2.
Nitrogen metabolism associated with amino acid catabolism (deamination reactions)
-
3.
Ammonia production by GDH
In normal conditions, GDH functions to biosynthesize glutamate; however, the GDH reaction is reversible in catabolic states, such as during excessive exercise. In such states GDH instead catabolizes glutamate to ammonia and α-ketoglutarate (brain, intestine, renal tubules).
-
4.
Ammonia production by glutaminase
The ammonia nitrogen produced in various tissues of the body is transported as blood glutamine or alanine into the liver, wherein these amino acids are converted into glutamate via transamination and ammonia is released through oxidative deamination. Glutamine is broken down into ammonia and glutamate by glutaminase.
The increase in ammonia with conditions such as a portosystemic shunt is thought to be due to the processes described in (1); moreover, if catabolism is accelerated, the reactions described in (2–4) increase, which leads to convulsions . The biosynthesis conducted in the urea cycle is shown in the following equation:
Thus, the conversion of two molecules of ammonia to urea requires 3ATP, which indicates that approximately 10% of the ATP produced in the mitochondria is consumed by the urea cycle. In this manner, our bodies actively excrete ammonia as fixed nitrogen in the form of urea.
Notably, the process of maturation in the human urea cycle is similar to that of urea cycle maturation during amphibian metamorphosis, consistent with the classic phrase that ontogeny recapitulates phylogeny. Among amphibians, aquatic larval tadpoles discharge ammonia into the water as nitrogen sources, similar to fish, but perform little urea synthesis (Fig. 12.5) (Mori 1991). However, during the transformation from tadpoles to frogs, the urea cycle enzymes are induced, allowing nitrogen to be excreted into urine as urea.
Change of urea cycle enzymes activities under the growth process of the amphibian. (Citation from “Journey of nitrogen in the living body (Seitai no tisso no tabi)” by Mori 1991). The enzyme activities in the urea cycle are enhanced in the process through which tadpoles transform into a frog. ARG arginase 1, CPS carbamoyl phosphate synthetase 1, OTC ornithine transcarbamylase. Dashed line: Urea excreting ability
As also demonstrated in experiments in rat (Fig. 12.6), the expression of enzymes comprising the human urea cycle increases during the process of development from the fetal stage to infancy and then through childhood and adulthood.
Change of urea cycle enzymes activities under the growth process of the rat. (Modified for N.C.R. Räihä, in “The Urea Cycle” Grisolia S, et al. (ed.), 1976). The enzyme activities in the urea cycle are enhanced in the process through which the rat develops from a fetus to an infant. ARG arginase 1, ASL argininosuccinate lyase, ASS argininosuccinate synthetase , CPS carbamoyl phosphate synthetase 1, OTC ornithine transcarbamylase. Dashed line: Urea synthetic ability
8 Primary Urea Cycle Disorders
8.1 Ornithine Transcarbamylase Deficiency (OTCD)
OTCD is an X chromosome-linked, recessive genetic disease (Nagata et al. 1991). The condition is more severe in hemizygotic males than in heterozygotic females; thus, it was thought that heterozygote females either have a mild version of OTCD or are asymptomatic. However, Uchino et al. reported that female patients with late-onset OTCD in Japan did not necessarily represent mild cases (Uchino et al. 1998). The clinical symptoms observed in male neonates comprise severe hyperammonemia that typically manifests a few days after birth. Conversely, late-onset OTCD generally occurs in heterozygotic female patients and in some male patients. Late-onset OTCD is characterized by the episodic appearance of symptoms with acute hyperammonemia, interspersed with healthy periods, and it may occur at any age. These attacks often occur after consumption of a high-protein meal or after the individual has been in a catabolic state, such as during infection. Falling into a coma or death is possible during hyperammonemia, and mental developmental delays are highly possible after exposure to severe hyperammonemia. Laboratory findings during an episode of hyperammonemia include elevated plasma glutamine and alanine concentrations, as well as elevated urinary orotic acid . Definitive diagnosis can be achieved with genetic analysis or measurement of OTC enzyme activity in the liver. Prenatal diagnosis is performed via fetal liver biopsy or chorionic villi genetic analysis . Asymptomatic, heterozygote female carriers can sometimes be identified using an oral protein challenge (allopurinol loading test) that elevates plasma ammonia and urinary orotic acid concentrations. Notably, however, such “asymptomatic” carriers usually exhibit mild brain dysfunction compared to unaffected siblings.
8.2 Carbamoyl Phosphate Synthetase 1 Deficiency (CPSD)
The carbamoyl phosphate precursor, N-acetylglutamate (NAG), is synthesized by the enzyme NAG synthetase. NAG synthetase deficiency (NAGSD) and CPSD present with the same clinical and biochemical symptoms. CPSD exhibits more severe and varied symptoms, along with a broader range of onset age. Generally, this condition develops during the neonatal period a few days after birth, with the onset of hyperammonemia signs and symptoms, with cases often being severe and resulting in death or mental retardation . Laboratory findings show elevated plasma glutamine and alanine concentrations, whereas there is no increase in urinary orotic acid . Definitive diagnosis is achieved with genetic analysis or by measuring CPS1 enzyme activity in the liver; however, sophisticated technology is needed to differentiate this condition from NAGSD using enzyme activity measurements.
8.3 Argininosuccinate Synthetase Deficiency (ASSD)
ASSD presents with a considerable diversity of clinical and biochemical findings, with clinical symptoms ranging from severe to asymptomatic. The signs and symptoms during neonatal onset are identical with those observed in neonatal onset of CPSD and OTCD. The symptoms in late onset comprise either phased onset of stunted growth, frequent vomiting, developmental delay, and dry brittle hair or appear as acute episodes, as observed in OTCD. In some patients, the symptoms may not appear until the third decade of life. Laboratory findings include marked elevation of plasma citrulline concentration, elevation of plasma glutamine and alanine concentrations, and mild elevation of urinary orotic acid . Diagnosis is confirmed by genetic analysis and fibroblast enzyme activity measurement. Prenatal diagnosis is confirmed by amniotic cell enzyme activity measurement. Most patients carry two different recessive alleles and are therefore compound heterozygotes . The prognosis is extremely poor if the condition develops during the neonatal period, whereas a good prognosis is obtained for patients with mild disorders on a protein-restricted diet.
8.4 Argininosuccinate Lyase Deficiency (ASLD)
There is a substantively wide range in the severity of ASLD clinical and biochemical findings. In neonatal onset , severe hyperammonemia appears from a few days after birth, and the mortality rate is extremely high. Late onset is associated with mental retardation , stunted growth, and hepatomegaly. Hair abnormalities have diagnostic value specific to this disease. Furthermore, sequelae frequently observed in ASLD include continuous hepatomegaly associated with a bleeding tendency caused by mild elevation of deviant hepatic enzymes and coagulation factor abnormalities. Acute episodes of severe hyperammonemia occur when the patient is in a catabolic state, such as during infection. Laboratory findings include hyperammonemia, mild elevation of hepatic deviation enzymes, non-specific elevated plasma glutamine and alanine concentrations, moderate elevation of plasma citrulline concentration, and marked elevation of plasma argininosuccinate. Argininosuccinate can also be found in the urine and cerebrospinal fluid, with the concentrations being higher in the cerebrospinal fluid than in the plasma. ASL is present in red blood cells, the liver, and fibroblasts. Prenatal diagnosis is confirmed with amniotic cell enzyme activity measurements; specifically, there is an increased level of argininosuccinate in the amniotic fluid of affected fetuses.
8.5 Arginase 1 Deficiency (ARGD)
Humans carry two genetically different types of arginase, one of which is present in the cytoplasm and is expressed in the liver and red blood cells, whereas the other is found in kidney mitochondria. In ARGD, the cytoplasmic ARG enzyme is deficient. The clinical symptoms are completely different to those of other UCDs. At a few months after birth, infants are normally asymptomatic continuing for the first few years. Then, previously normal infants present with progressive spastic diplegia with scissors gait or choreiform movement and loss of developmental indices. Seizures occur frequently in this disease, and mental retardation is progressive. Hepatomegaly may also occur although severe hyperammonemia is infrequent. Laboratory findings include marked elevation of arginine in the plasma and cerebrospinal fluid and moderate elevation of urinary orotic acid . Plasma ammonia concentration is either normal or very slightly elevated. Excretion of arginine, lysine, cysteine, and ornithine in the urine may be elevated but is also sometimes normal. Urinary guanidino compounds (α-keto guanidino valerate and alginate) are significantly elevated. Plasma amino acid quantitative determination is extremely important. Diagnosis is determined based on red blood cell arginase measurement. Treatment includes a low-protein diet with absolutely no arginine along with frequent quantitative determination of plasma amino acid concentrations. The composition of the therapeutic diet and the daily consumption of protein must be carefully measured and controlled.
8.6 NAG Synthetase Deficiency (NAGSD)
NAGSD presents with hyperammonemia, similar to CPS1 deficiency, owing to deficiency in N-acetyl glutamate synthetase, which is essential for CPS activation. Administration of carbamylglutamate serves as an effective treatment.
9 Secondary Urea Cycle Disorders
In addition to the six aforementioned UCDs, urea cycle-related diseases include ornithine transaminase enzyme deficiency, citrin deficiensy, lysinuric protein intolerance, and hyperornithinemia-hyperammonemia-homocitrullinuria syndrome.
-
1.
Lysinuric protein intolerance
This is a functional abnormality of the dibasic amino acid transporter protein y + L. The amino acid transporter y + LAT-1 is mainly present in the epithelial basement membrane of the kidneys and small intestine. Hyperammonemia is caused by a secondary urea cycle disorder as a result of an absorption disorder of dibasic amino acids (lysine, arginine, and ornithine) in the small intestine epithelium owing to y + LAT-1 deficiency. Administration of citrulline is an effective therapy.
-
2.
Hyperornithinemia-hyperammonemia-homocitrullinuria syndrome
This disease constitutes an abnormality of the system for ornithine transport from the cytoplasm to the mitochondria, causing an accumulation of ornithine in the cytoplasm and deficiency of ornithine in the mitochondria. This in turn results in hyperornithinemia, homocitrullinuria, and hyperammonemia. Protein restriction and administration of ornithine are effective treatments.
10 Therapy
Following a definitive diagnosis, the treatment is implemented in accordance with the treatment guidelines for UCDs in each country. Each treatise or guideline (in the EU and USA) is available online. Collaboration with specialist doctors is essential; however, as transport is often difficult during acute attacks, it is preferable to receive treatment in a base hospital until the patient disease condition stabilizes while communicating with the specialist, rather than transferring the affected infant or child while they are in an unstable condition.
-
1.
The main treatments in the acute phase are indicated as follows. Dialysis therapy is first instigated to rapidly reduce the plasma ammonia concentration.
-
(a)
Plasma ammonia reduction.
Hemodialysis is one of the best treatments to immediately reduce the plasma ammonia concentration, as the faster the blood flow, the more rapidly the clearance will occur and symptoms improve. The dialysis method depends on the condition of the affected patient and the available equipment. Specific methods include blood filtration (either artery-vein, or vein-vein), hemodialysis, peritoneal dialysis, and continuous drainage peritoneal dialysis. Continuous hemodiafiltration is often used with neonates.
-
(b)
Pharmacotherapy to excrete surplus nitrogen via an alternative metabolic pathway.
Inhibiting ammonia production can be achieved with intravenous administration of l-arginine hydrochloride and nitrogen-removing agents (e.g., sodium phenylbutyrate or/and sodium benzoate) (Brusilow 1991; Brusilow and Horwich 2001; Brusilow et al. 1979). After a loading dose, the patient receives a maintenance dose, which is initially performed using intravenous administration and then switched to oral administration once symptoms have stabilized. Moreover, oral lactulose contributes to decreasing blood ammonia by means of increasing the degree of acidity and lowering the production and absorption of ammonia in the intestinal tract.
-
(c)
Removal of surplus nitrogen in the diet.
Excess dietary nitrogen can be eliminated through use of a protein-restricted diet or protein-free formula (Leonard 2001).
In addition, carbohydrates and fats can be used as calories during the acute phase, such as through intravenous administration of >10% glucose and fat emulsion or administration of protein-free milk via a gastric tube. It is considered best practice to transition from non-oral administration to enteral administration as early as possible. However, complete protein removal for more than 24 h to 48 h is not recommended because this induces catabolism owing to nonavailability of essential amino acids . It is thus important to administer small amounts of protein (0.1–0.3 g/kg/day) from an early stage under the acute hyperammonemia state.
-
(d)
Reduce the risk of neurological disorders.
It is vital to maintain the circulating plasma volume and blood pressure. However, excess fluid administration can promote cerebral edema; thus, vasopressors should be used appropriately, and the total body water and circulating volume must be controlled.
-
(a)
-
2.
Management of the chronic phase.
-
(a)
Prevention of initial symptoms.
Prevention of the recurrence of hyperammonemia is important. Treatment should include protein-restricted diet and formula.
-
(b)
Prevention of secondary infections.
Every effort should be made to minimize the risk of respiratory infections and gastrointestinal infections in the household.
-
(c)
Prevent exposure to excessive stress.
There are reports of hyperammonemia cases being induced by excessive internal bleeding after a major fracture or trauma as well as by steroid administration; therefore, considerable caution with regard to patients with UCDs under an enhanced state of metabolic stress is essential. Taking valproic acid, long-term hunger or starvation, intravenous steroids, and high intake of protein or amino acids can induce hyperammonemia and must be avoided.
-
(d)
Liver transplants have been performed in a large number of patients with UCDs, which has contributed to an improved prognosis (Morioka et al. 2005; Kasahara et al. 2010; Wakiya et al. 2011).
-
(e)
Treatments currently being researched are as follows:
-
Clinical trials of liver cell transplantation therapy are currently in progress in the USA and EU.
-
Clinical trials of liver stem cell transplantation therapy are currently in progress in Belgium and the USA.
-
-
(a)
As a result of the development of hemodialysis treatment and liver transplantation, patients with UCDs have a higher chance of survival compared to that before the turn of the century. The prognosis for neurological development has also improved (Uchino et al. 1998; Kido et al. 2012). Control of blood ammonia has become easier with the use of arginine, citrulline , benzoate, and sodium phenylbutyrate. However, without liver transplantation there is always the risk of developing hyperammonemia owing to metabolic stress, including the common cold or trauma. Recently, more facilities have begun to gain experience regarding the patients with UCDs being pregnant and giving birth. Meticulous care is essential for the delivery of patients with UCDs, and it is necessary to frequently check patient blood ammonia levels for approximately 2 weeks after the delivery (Langendonk et al. 2012; Kido et al. 2012). However, in relation to mental development , it is impossible to prevent an effect of raised glutamine and ammonia in the central nervous system even if the individual does not develop an intellectual disability. Therefore, it cannot accurately be stated that the long-term prognosis for patients with UCDs is favorable.
Questions
-
1.
What should be considered when differentially diagnosing hyperammonemia? For UCDs, what tests should be performed subsequently?
-
2.
What treatments are recommended for UCDs? Why is it essential to reduce elevated blood ammonia concentrations?
-
3.
What are the most important developmental outcomes in the management of UCDs?
-
4.
What kinds of treatments are expected in the future?
Answers
-
1.
Important diseases that present with hyperammonemia include UCDs as well as mitochondrial disorders, fatty acid metabolism disorders, systemic sepsis, liver failure, and portosystemic shunt. Diagnostically, it is first important to measure blood ammonia. Specific diagnosis is possible with special tests including blood and urine amino acid analysis, orotic acid measurement, and genetic analysis.
-
2.
Treatment includes hemodialysis and pharmacotherapy such as l-arginine hydrochloride, sodium phenylbutyrate, and sodium benzoate, in combination with a protein-restricted diet and protein-free milk. Furthermore, in the chronic stage, it is important to prevent secondary infection and exposure to excessive stress. Liver transplantation is sometimes performed as a radical treatment. The aim of treatment is to avoid brain and neuron disorders caused by hyperammonemia and to achieve comparatively normal neurodevelopment.
-
3.
The most important outcomes are increasing normal height and weight and achieving normal neurodevelopment while avoiding hyperammonemia.
-
4.
Prospective future treatments include hepatocyte stem cell transplantation and gene therapy.
References
Batshaw ML, Tuchman M, Summar M et al (2014) A longitudinal study of urea cycle disorders. Mol Genet Metab 113:127–130
Berry GT, Steiner RD (2001) Long-term management of patients with urea cycle disorders. J Pediatr 138:S56–S60
Brusilow SW (1991) Phenylacetylglutamine may replace urea as a vehicle for waste nitrogen excretion. Pediatr Res 29:147–150
Brusilow SW, Horwich AL (2001) Urea cycle enzymes. In: Scriver CR, Beaudet AL, Sly WS et al (eds) The metabolic and molecular basis of inherited disease, 8th ed. McGraw-Hill, New York, pp 1909–1963
Brusilow SW, Valle DL, Batshaw M (1979) New pathways of nitrogen excretion in inborn errors of urea synthesis. Lancet 2:452–454
Kasahara M, Sakamoto S, Shigeta T et al (2010) Living-donor liver transplantation for carbamoyl phosphate synthetase 1 deficiency. Pediatr Transplant 14:1036–1040
Kido J, Nakamura K, Mitsubuchi H et al (2012) Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 35:777–785
Langendonk JG, Roos JC, Angus L et al. (2012) A series of pregnancies in women with inherited metabolic disease. J Inherit Metab Dis 35:419–424
Leonard JV (2001) The nutritional management of urea cycle disorders. J Pediatr 138:S40–S44, discussion S44–S45
Maestri NE, McGowan KD, Brusilow SW (1992, August) Plasma glutamine concentration: a guide in the management of urea cycle disorders. J Pediatr 121(2):259–261
Mori M (1991) Urea cycle. In: Journey of nitrogen in the living body (Seitai no tisso no tabi). Kyoritsu Shuppan Co., Ltd., Tokyo, pp 48–49
Morioka D, Kasahara M, Takada Y et al (2005) Current role of liver transplantation for the treatment of urea cycle disorder: a review of the worldwide English literature and 13 cases at Kyoto University. Liver Transpl 11:1332–1342
Nagata N, Matsuda I, Oyanagi K (1991) Estimated frequency of urea cycle enzymopathies in Japan. Am J Med Genet 39:228–229
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inherit Metab Dis 21:S151–S159
Wakiya T, Sanada Y, Mizuta K et al (2011) Living donor liver transplantation for ornithine transcarbamylase deficiency. Pediatr Transplant 15:390–395
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nakamura, K., Kido, J., Matsumoto, S. (2019). Urea Cycle Disorders. In: Oohashi, T., Tsukahara, H., Ramirez, F., Barber, C., Otsuka, F. (eds) Human Pathobiochemistry. Springer, Singapore. https://doi.org/10.1007/978-981-13-2977-7_12
Download citation
DOI: https://doi.org/10.1007/978-981-13-2977-7_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2976-0
Online ISBN: 978-981-13-2977-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)