Abstract
Quantifying of pain is necessary for optimal dose of opioid. In pain quantification, there have been many attempts to analyze the photoplethysmography (PPG) waveform as a promising maker of autonomic function. In this paper, we investigate the feasibility of PPG amplitude variability (PPGV) as a novel marker of pain quantification. We derived 8 parameters related to the PPG amplitude and amplitude variability: ACAbaseline, ACAdia, PPGAVsys, PPGAVdia, PPGAVsys/ACAbaseline, PPGAVsys/ACAdia, PPGAVdia/ACAbaseline and PPGAVdia/ACAdia, and calculated frequency domain variables, TP, VLF, LF, HF, nLF, nHF and LF/HF, that have been used for heart rate variability analysis. Every parameter was derived in clinical dataset obtained before and after surgery, and a significant difference was statistically verified using paired t-test. Consequently, a significant difference (p < 0.05) was found in every derived variable except for most variables in ACAbaseline, ACAdia, PPGAVsys, PPGVdia, in nHF of PPGAVsys/ACAbaseline, in nHF, LF/HF of PPGAVsys/ACAdia, in nLF, nHF of PPGAVdia/ACAdia, and in nLF, nHF of PPGAVdia/ACAbaseline. This result suggests that the possibility of frequency domain analysis of PPGV as a novel indicator of surgical pain quantification.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
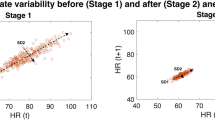
Assessment of surgical pain has been attempted with difficulties because it is not easy to describe degree of pain objectively. There have been many attempts to quantify pain such as skin conductance-based method [1, 2], analgesia nociception index (ANI, Mdoloris Medical System, Lille, France) [3, 4] and surgical plethysmographic index (SPI, GE Healthcare, Chicago, USA) [5]. Skin conduction was reported to correlate significantly with a numeric rating scale (NRS) in postoperative pain [6] and ANI seems more sensitive than heart rate and systolic blood pressure to moderate nociceptive stimuli in propofol-anaesthetized patients [7]. Especially, SPI which based on continuous cardiovascular variables like heartbeat intervals (HBI) and photoplethysmography amplitude (PPGA) was evaluated as a promising index of postoperative pain assessment [8]. The result of SPI could be interpreted as changes of heart rate and blood volume with sympathetic activation [9, 10]. In this study, we consider the possibility of assessing surgical pain by analyzing PPG amplitude variability (PPGV) as another pain indicator. For this, we assumed that the PPGV has relevance with blood pressure variability (BPV), which is a method to measure systolic blood pressure and detect changes in the short or long term and estimates the physiological state via the mean of the measured blood pressure or a standard deviation [11], because blood volume could be proportionally changed with blood pressure excluding the consideration of vascular property. In analyzing PPGV, we adapted frequency domain analysis metric of heart rate variability (HRV).
2 Methods
2.1 Dataset
Sixty surgical patients (29 males, 31 females, 52.1 ± 11.4 years old) were enrolled to the experiment, and 58 pair of dataset was used except 2 pair of dataset which has recording error. According to the protocol, PPG data was recorded before and after surgery, and dataset recorded before and after surgery were regarded as a painless and pain dataset, respectively. Every record has 6-min length of 300 Hz sampling frequency. To calculate the area of PPG waveform, every upper and lower peak location of the PPG waveform was detected and validated by proficient researchers.
2.2 Parameter Extraction
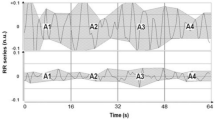
Derived parameters were defined as the amplitude from baseline to systolic peak (ACAbaseline), the amplitude from diastolic peak to systolic peak (ACAdia), the amplitude difference of adjacent systolic peaks (PPGAVsys), the amplitude difference of adjacent diastolic peaks (PPGAVdia), the ratio of PPGAVsys to ACAbaseline (PPGAVsys/ACAbaseline), the ratio of PPGAVsys to HPH (PPGAVsys/HPH), the ratio of PPGAVdia to ACA (PPGAVdia/ACA), and the ratio of PPGAVdia to HPH (PPGAVdia/HPH). Figure 1 shows the graphical representation of parameters, and Eqs. (1)–(5) represents mathematical equation of ACAdia, BP, ACAbaseline, PPGAVsys, PPGAVdia, respectively (see Table 1).
2.3 Validation
Every parameter was derived in pain and painless dataset, and it was verified whether there is significant different using paired t-test.
3 Result and Discussion
Table 2 shows that the mean, standard deviation, coefficient of variation and significance of difference of the result according to the nociceptive pain. As a result, statistical difference was not found in TP, VLF, LF, HF, nLF of ACAbaseline, TP, LF, HF, nLF of ACAdia, TP, VLF, KF, HL, nHF of PPGAVsys, TP, VLF, LF, HF, nLF, nHF of PPGVdia, nHF of PPGAVsys/ACAbaseline, nHF, LF/HF of PPGAVsys/ACAdia and nLF, nHF of PPGAVdia/ACAdia, nLF, nHF of PPGAVdia/ACAbaseline. LF component of BPV reflects sympathetic vasomotor activity which is known as Mayer wave [12,14,15,16,17,17]. Otherwise, high frequency component of BPV reflects mechanical function of hemodynamics according to the pressure change inside thoracic cage [15]. In the result of this study, LF value of ACAbaseline and ACAdia was decreased but there is no statistical significance, moreover, PPGAVsys and PPGAVdia also shows increases with no significance. However, in every normalized parameter, LF value is increased with statistical significance (p < 0.05). This result could be interpreted that normalization reduced the ambiguity of PPG amplitude which is measured as an arbitrary unit. In terms of parameters, amplitude variability parameter, PPGAVsys, PPGAVdia shows clear classification result compared with simple amplitude-based variables, ACAbaseline and ACAdia. This result suggests that the frequency domain variables of PPGV has a possibility in pain quantification and that the significant changes were reflected better in normalized variables.
4 Conclusion
In this study, we investigated PPGV in surgical pain quantification. We derived frequency domain variable of PPGV before and after surgery and found that there is a significant difference (p < 0.05) in PPGV variables according to the pain stimuli. Especially, result indicated that a clear difference was found in normalized PPGV variables. Consequently, the result of this study suggests that the possibility of frequency domain analysis of PPGV as a novel indicator of surgical pain quantification.
References
Dube A. A., Duquette M., Roy M., Lepore F., Duncan G., Rainville P.: Brain activity associated with the electrodermal reactivity to acute heat pain. Neuroimage 45, 169–180 (2009)
Burton A. R., Birznieks I., Bolton P. S., Henderson L. A., Macefield V. G.: Effects of deep and superficial experimentally induced acute pain on muscle sympathetic nerve activity in human subjects. The Journal of Physiology 587(1), 183–193 (2009)
Luginbiihl M., Ypparila-Wolters H., Riifenacht M., Petersen-Felix S., Korhonen I.: Heart rate variability does not discriminate between different levels of haemodynamic responsiveness during surgical anaesthesia. British Journal of Anaesthesia 98(6), 728–736 (2007)
Seitsonen E. R. J., Korhonen I. K. J., Van Gils M. J., Huiku M., Lötjönen J. M. P., Korttila K. T., Yli‐Hankala A. M.: EEG spectral entropy, heart rate, photoplethysmography and motor responses to skin incision during sevoflurane anaesthesia. Acta Anaesthesiologica Scandinavica 49(3), 284–292 (2005)
Huiku M., Uutela K., Van Gils M., Korhonen I., Kymäläinen M., Meriläinen P., Yli-Hankala A.: Assessment of surgical stress during general anaesthesia. British journal of anaesthesia 98(4), 447–455 (2007)
Ledowski T., Bromilow J., Wu J., Paech M. J., Storm H., Schug S. A.: The assessment of postoperative pain by monitoring skin conductance: results of a prospective study. Anaesthesia 62(10), 989–993 (2007)
Jeanne M., Clement C., De Jonckheere J., Logier R., Tavernier B.: Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. Journal of clinical monitoring and computing 26(4), 289–294 (2012)
Ahonen J., Jokela R., Uutela K., Huiku, M.: Surgical stress index reflects surgical stress in gynaecological laparoscopic day-case surgery. British journal of anaesthesia 98(4), 456–461 (2007)
Awad A. A., Ghobashy M. A. M., Ouda W., Stout R. G., Silverman D. G., Shelley K. H.: Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesthesia & Analgesia 92(6), 1483–1486 (2001)
Korhonen I., YLI‐HANKALA A.: Photoplethysmography and nociception. Acta Anaesthesiologica Scandinavica 53(8), 975–985. (2009)
Mancia G.: Short-and Long-term blood pressure variability. Hypertension 60(2), 512–517. (2012)
Pagani M., Lombardi F., Guzzetti S., Rimoldi O., Furlan R. A. F. F. A. E. L. L. O., Pizzinelli P., Piccaluga E.: Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympathovagal interaction in man and conscious dog. Circulation research, 59(2), 178–193. (1986)
Van De Borne P., Montano N., Pagani M., Oren R., Somers V. K.: Absence of low-frequency variability of sympathetic nerve activity in severe heart failure. Circulation, 95(6), 1449–1454. (1997)
Pagani M., Montano N., Porta A., Malliani A., Abboud F. M., Birkett C., Somers V. K.: Relationship between spectral components of cardiovascular variabilities and direct measures of muscle sympathetic nerve activity in humans. Circulation, 95(6), 1441–1448. (1997)
Radaelli A., Bernardi L., Valle F., Leuzzi S., Salvucci F., Pedrotti L., Sleight P.: Cardiovascular autonomic modulation in essential hypertension. Effect of tilting. Hypertension, 24(5), 556–563. (1994)
Montano N., Cogliati C., Porta A., Pagani M., Malliani A., Narkiewicz K., Somers V. K.: Central vagotonic effects of atropine modulate spectral oscillations of sympathetic nerve activity. Circulation, 98(14), 1394–1399. (1998)
Malliani A., Pagani M., Lombardi F., Cerutti S.: Cardiovascular neural regulation explored in the frequency domain. Circulation, 84(2), 482–492. (1991)
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1C1A1A02036535).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Yang, Y.L., Seok, H.S., Shin, H. (2019). Investigation of the Feasibility of Postoperative Pain Assessment Using Frequency Analysis of Photoplethysmogram Variability. In: Lhotska, L., Sukupova, L., Lacković, I., Ibbott, G. (eds) World Congress on Medical Physics and Biomedical Engineering 2018. IFMBE Proceedings, vol 68/2. Springer, Singapore. https://doi.org/10.1007/978-981-10-9038-7_65
Download citation
DOI: https://doi.org/10.1007/978-981-10-9038-7_65
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-9037-0
Online ISBN: 978-981-10-9038-7
eBook Packages: EngineeringEngineering (R0)