Abstract
As IgG4-related sclerosing cholangitis (IgG4-SC) exhibits various cholangiographic features similar to those of primary sclerosing cholangitis (PSC), pancreatic cancer, and cholangiocarcinoma, the differential diagnosis of IgG4-SC from these three progressive or malignant diseases is very important. In the criteria of Japanese group, diagnosis of IgG4-SC is based on the following four criteria: characteristic biliary imaging findings, elevation of serum IgG4 levels, coexistence of IgG4-related diseases, except those of the biliary tract, and characteristic histopathologic features. IgG4-SC is frequently associated with autoimmune pancreatitis (AIP), and this association is useful for diagnosis of IgG4-SC. However, it is particularly difficult to accurately diagnose IgG4-SC in the absence of AIP. Evaluation of the effectiveness of steroid therapy is an optional extra diagnostic criterion to confirm a diagnosis of IgG4-SC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- IgG4-related Sclerosing Cholangitis (IgG4-SC)
- IgG4-related Kidney Disease
- Characteristic Histopathological Features
- Autoimmune Pancreatitis (AIP)
- Primary Sclerosing Cholangitis (PSC)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Diagnostic Criteria of IgG4-Related Sclerosing Cholangitis
Introduction
IgG4-related sclerosing cholangitis (IgG4-SC) is a characteristic type of sclerosing cholangitis with an unknown pathogenic mechanism. IgG4-SC patients have increased serum IgG4 levels [1] and dense infiltration of IgG4-positive plasma cells with extensive fibrosis in the bile duct wall [2]. IgG4-SC is frequently associated with autoimmune pancreatitis (AIP) and generally shows a good prognosis and responds to steroid therapy [3,4,5,6,7].
As various cholangiographic features of IgG4-SC are similar to those of primary sclerosing cholangitis (PSC), pancreatic cancer, and cholangiocarcinoma [8, 9], it can be difficult to discriminate IgG4-SC from these progressive or malignant diseases on the basis of cholangiographic findings alone [10, 11]. Therefore, these three diseases should be taken into account in the diagnostic criteria for IgG4-SC.
Diagnostic Criteria
Two sets of diagnostic criteria for IgG4-SC have been proposed. The HISORt criteria were originally developed for AIP and adapted for IgG4-SC [7] (Table 7.1). These criteria are based on histological findings, imaging, serological examination, other organ involvement, and response to steroid therapy.
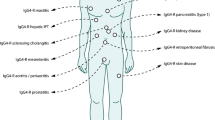
A second set of diagnostic criteria for IgG4-SC has been proposed by a Japanese group [12] (Table 7.2). Diagnosis of IgG4-SC is based on the following four criteria: (1) characteristic biliary imaging findings, (2) elevation of serum IgG4 concentration, (3) coexistence of IgG4-related diseases except those of the biliary tract, and (4) characteristic histopathological features. The effectiveness of steroid therapy is an optional extra diagnostic criterion used to confirm a diagnosis of IgG4-SC. Furthermore, the typical cholangiographic features are shown schematically and diseases to be discriminated from IgG4-SC and the necessary examinations for diagnosis are described to facilitate clinical application of these diagnostic criteria [12] (Fig. 7.1).
The cholangiographic classification of IgG4-related sclerosing cholangitis and differential diagnosis. Stenosis is located only in the lower part of the common bile duct in Type 1; stenosis is diffusely distributed in the intra- and extrahepatic bile ducts in Type 2. Type 2 is further subdivided into two types. Extended narrowing of the intrahepatic bile ducts with prestenotic dilation is widely distributed in Type 2a. Narrowing of the intrahepatic bile ducts without prestenotic dilation and reduced bile duct branches is widely distributed in Type 2b; stenosis is detected in both the hilar hepatic lesions and the lower part of the common bile ducts in Type 3; and strictures of the bile duct are detected only in the hilar hepatic lesions in Type 4. * IDUS: intraductal ultrasonography. ** EUS-FNA: endoscopic ultrasound-guided fine-needle aspiration. *** IBD: inflammatory bowel disease
Diagnostic Imaging Findings
Narrowing of the Bile Duct
IgG4-SC shows various cholangiographic features similar to those of pancreatic cancer, PSC, and cholangiocarcinoma. The characteristic features of IgG4-SC can be classified into four types based on the stricture regions revealed by cholangiography and differential diagnosis (Fig. 7.1) [13].
Type 1 IgG4-SC shows stenosis only in the lower part of the common bile duct, which should be differentiated from chronic pancreatitis, pancreatic cancer, and cholangiocarcinoma. IgG4-SC associated with AIP frequently shows a stricture in the lower common bile duct. This stricture can originate from thickening of the bile duct or the effect of pancreatic inflammation and/or edema [14].
Type 2 IgG4-SC, in which stenosis is diffusely distributed throughout the intrahepatic and extrahepatic bile ducts, should be differentiated from PSC. Band-like stricture, a beaded and pruned tree appearance, and diverticulum-like outpouching are significantly more frequent in PSC. In contrast, segmental strictures, long strictures with prestenotic dilation, and strictures of the lower common bile duct are significantly more common in IgG4-SC. Type 2 is subdivided into Type 2a, which involves narrowing of the intrahepatic bile ducts with prestenotic dilation, and Type 2b, which involves narrowing of the intrahepatic bile ducts without prestenotic dilation and reduced bile duct branches. The latter is caused by marked lymphocytic and plasmacyte infiltration into the peripheral bile ducts.
Type 3 IgG4-SC is characterized by stenosis in both the hilar hepatic lesions and the lower part of the common bile duct. Type 4 IgG4-SC shows strictures of the bile duct only in hilar hepatic lesions. The cholangiographic findings of Types 3 and 4 should be discriminated from those of cholangiocarcinoma.
Thickening of the Bile Duct
Abdominal ultrasonography (US) [15], abdominal computed tomography [16], abdominal magnetic resonance imaging, endoscopic ultrasonography, and intraductal ultrasonography (IDUS) [17] show circular-symmetric wall thickening, smooth outer and inner margins, and homogenous internal echo. These characteristic features are recognized not only in the stenotic areas or occasionally in the gallbladder but also in areas without stenosis that appear normal on cholangiogram. Bile duct wall thickening extends continuously from the intrapancreatic bile duct to the upper bile duct in most IgG4-SC cases. To differentiate IgG4-SC from cholangiocarcinoma, a bile duct wall thickness of 0.8 mm that appears normal on a cholangiogram is the optimum cutoff established by a study on IDUS [17]. Patients with PSC also have widespread thickening of the bile duct, which shows IDUS findings of an irregular inner margin, diverticulum-like outpouching, and disappearance of three layers [18].
Hematological Examination
An elevated serum IgG4 level is a diagnostic criterion for IgG4-SC [1]. The cutoff serum IgG4 levels are 140 mg/dl (nephelometric method) in the HISORt criteria [7] and 135 mg/dl in the Japanese criteria [12].
However, an elevated serum IgG4 level is also observed in atopic dermatitis, pemphigus, asthma, etc.; in particular, elevated serum IgG4 levels are also observed in PSC and some malignant cholangiopancreatic diseases (e.g., pancreatic cancer and cholangiocarcinoma) [19, 20]. Oseini et al. evaluated the utility of serum IgG4 level to discriminate IgG4-SC from cholangiocarcinoma [20]. They concluded that some patients with cholangiocarcinoma, particularly PSC, had elevated serum IgG4 levels, and diagnosis using a twofold higher cutoff serum IgG4 level (>280 mg/dl) may not reliably distinguish IgG4-SC from cholangiocarcinoma. A cutoff level fourfold higher than the upper limit of normal (> 560 mg/dl) had 100% specificity for IgG4-SC.
A Japanese multicenter study was performed to establish a serum IgG4 cutoff value to differentiate IgG4-SC from pancreatic cancer, PSC, and cholangiocarcinoma [21]. A total of 344 IgG4-SC patients were enrolled, together with 245, 110, and 149 patients with pancreatic cancer, PSC, and cholangiocarcinoma, respectively, as controls. The cutoff values from receiver operating characteristic (ROC) curves showed similar sensitivity and specificity to that of 135 mg/dl when all IgG4-SC cases and controls were compared. Of the pancreatic cancer, PSC, and cholangiocarcinoma cases, 5.7%, 12.7%, and 8.1%, respectively, had serum IgG4 levels higher than the cutoff value. A serum IgG4 cutoff value of 182 mg/dl increased the specificity to 96.6% for distinguishing Types 3 and 4 IgG4-SC from cholangiocarcinoma, and a cutoff of 207 mg/dl enabled discrimination of Types 3 and 4 IgG4-SC from cholangiocarcinoma.
Other Organ Involvement
IgG4-SC is frequently associated with AIP. Ghazale et al. reported that 49 of 53 patients with IgG4-SC had AIP [7]. In a Japanese multicenter study, 329 of 344 (95.6%) IgG4-SC cases were associated with AIP [21]. Association with AIP is useful for diagnosis of IgG4-SC. However, some IgG4-SC patients do not have AIP and are thus difficult to diagnose; most isolated IgG4-SC cases have hilar biliary strictures [22,23,24].
Occasionally, IgG4-SC is associated with other systemic IgG4-related diseases, including IgG4-related symmetrical dacryoadenitis/sialadenitis, IgG4-related retroperitoneal fibrosis, and IgG4-related kidney disease [25,26,27,28]. These associations can also assist diagnosis of IgG4-SC. Inflammatory bowel disease is usually not an associated condition, unlike its frequent association with PSC [29].
Pathological Findings of the Bile Duct
In IgG4-SC cases, fibroinflammatory involvement is observed mainly in the submucosa of the bile duct wall, whereas the bile duct epithelium is intact [30]. However, slight injury and/or neutrophil infiltration are occasionally observed in cases of IgG4-SC with secondary cholangitis. PSC should be excluded if inflammation is observed, particularly in the bile duct wall epithelium.
Endoscopic transpapillary bile duct biopsy is performed to rule out cholangiocarcinoma. Ghazale et al. reported that the immunostaining results of 14 (88%) of 16 patients indicated abundant IgG4+ cells in bile duct biopsy specimens [7]. However, it is difficult to obtain enough biliary tract tissue to assess the histology of IgG4-SC biopsy specimens (e.g., storiform fibrosis and obliterative phlebitis) [13]. We were able to diagnose IgG4-SC in only 3 (18%) of 17 patients on the basis of its characteristic histopathological features [17]. In addition, 1 of 11 cholangiocarcinoma cases presented abundant IgG4+ plasma cells. Zhang et al. also reported abundant IgG4+ plasma cells in 7 (18%) of 38 cases of cholangiocarcinoma [31]. It is important to note that the superficial nature of endoscopic biopsy specimens limits their usefulness for demonstrating the characteristic histological features of IgG4-SC.
Ampullary biopsy is occasionally useful in the diagnosis of IgG4-SC patients with swelling of the pancreatic head caused by AIP [32]. Liver biopsy can be useful for diagnosing IgG4-SC cases with intrahepatic bile duct strictures [33, 34].
Exclusion of Secondary Sclerosing Cholangitis
It is necessary to rule out the following features of secondary sclerosing cholangitis: common bile duct stone, cholangiocarcinoma, trauma, biliary tract surgery, congenital biliary anatomy, corrosive cholangitis, ischemic bile duct stenosis, AIDS-related cholangitis, and biliary injury due to intra-arterial chemotherapy.
Effectiveness of Steroid Therapy
In the HISORt criteria, response to steroid treatment is defined as a decrease in liver enzyme levels to less than twofold the upper limit of normal and/or improvement in biliary strictures [7]. In the Japanese criteria, this optional diagnostic criterion should be applied only to IgG4-SC cases in which the effect of steroid therapy can be evaluated by imaging modalities after negative work-up for malignancy [12]. Accordingly, clinical conditions or hematological findings cannot be evaluated by this method. It is sometimes difficult to obtain sufficient biopsy specimens from patients suffering from diseases not only of the biliary tract but also of other organs, such as the pancreas, lachrymal gland, salivary gland, and retroperitoneum. However, efforts should be made to collect sufficient tissue samples for diagnosis, and steroid trials should be avoided [12].
The effectiveness of steroid therapy should be cautiously evaluated because some malignant lesions improve after steroid administration [35]. If neoplastic lesions cannot be clinically ruled out after steroid therapy, a reevaluation should be performed to rule out malignant cholangiopancreatic diseases.
References
Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–8.
Zen Y, Harada K, Sasaki M, Sato Y, Tsuneyama K, Haratake J, et al. IgG4-related sclerosing cholangitis with and without hepatic inflammatory pseudotumor, and sclerosing pancreatitis-associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis? Am J Surg Pathol. 2004;28:1193–203.
Nakazawa T, Ohara H, Yamada T, Ando H, Sano H, Kajino S, et al. Atypical primary sclerosing cholangitis cases associated with unusual pancreatitis. Hepato-Gastroenterology. 2001;48:625–30.
Nakazawa T, Ohara H, Sano H, Ando T, Aoki S, Kobayashi S, et al. Clinical differences between primary sclerosing cholangitis and sclerosing cholangitis with autoimmune pancreatitis. Pancreas. 2005;30:20–5.
Nishino T, Toki F, Oyama H, Oi I, Kobayashi M, Takasaki K, et al. Biliary tract involvement in autoimmune pancreatitis. Pancreas. 2005;30:76–82.
Hirano K, Tada M, Isayama H, Yagioka H, Sasaki T, Kogure H, et al. Long-term prognosis of autoimmune pancreatitis with and without corticosteroid treatment. Gut. 2007;56:1719–24.
Ghazale A, Chari ST, Zhang L, Smyrk TC, Takahashi N, Levy MJ, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008;134:706–15.
Nakazawa T, Ohara H, Sano H, Aoki S, Kobayashi S, Okamoto T, et al. Cholangiography can discriminate sclerosing cholangitis with autoimmune pancreatitis from primary sclerosing cholangitis. Gastrointest Endosc. 2004;60:937–44.
Nishino T, Oyama H, Hashimoto E, Toki F, Oi I, Kobayashi M, et al. Clinicopathological differentiation between sclerosing cholangitis with autoimmune pancreatitis and primary sclerosing cholangitis. J Gastroenterol. 2007;42:550–9.
Kalaitzakis E, Levy M, Kamisawa T, Johnson GJ, Baron TH, Topazian MD, et al. Endoscopic retrograde cholangiography does not reliably distinguish IgG4-associated cholangitis from primary Sclerosing cholangitis or cholangiocarcinoma. Clin Gastroenterol Hepatol. 2011;9:800–3.e2.
Nakazawa T, Ando T, Hayashi K, Naitoh I, Okumura F, Miyabe K, et al. Diagnostic criteria for IgG4-related sclerosing cholangitis based on cholanigiographic classification. J Gastroenterol. 2012;40:79–87.
Ohara H, Okazaki K, Tsubouchi H, Inui K, Kawa S, Kamisawa T, et al. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J Hepatobiliary Pancreat Sci. 2012;19:536–42.
Nakazawa T, Ohara H, Sano H, Ando T, Joh T. Schematic classification of sclerosing cholangitis with autoimmune pancreatitis by cholangiography. Pancreas. 2006;32:229.
Hirano K, Tada M, Isayama H, Yamamoto K, Mizuno S, Yagioka H, et al. Endoscopic evaluation of factors contributing to intrapancreatic biliary stricture in autoimmune pancreatitis. Gastrointest Endosc. 2010;71:85–90.
Koyama R, Imamura T, Okuda C, Sakamoto N, Honjo H, Takeuchi K, et al. Ultrasonographic imaging of bile duct lesions in autoimmune pancreatitis. Pancreas. 2008;37:259–64.
Itoh S, Nagasaka T, Suzuki K, Satake H, Ota T, Naganawa N. Lymphoplasmacytic sclerosing cholangitis: assessment of clinical, CT, and pathological findings. Clin Radiol. 2009;64:1104–14.
Naitoh I, Nakazawa T, Ohara H, Andoh T, Hayashi K, Tanaka H, et al. Endoscopic transpapillary intraductal ultrasonography and biopsy in the diagnosis of IgG4-related sclerosing cholangitis. J Gastroenterol. 2009;44:1147–55.
Naitoh I, Nakazawa T, Hayashi K, Miyabe K, Shimizu S, Kondo H, et al. Comparison of intraductal ultrasonography findings between primary sclerosing cholangitis and IgG4-related sclerosing cholangitis. J Gastroenterol Hepatol. 2015;30:1104–9.
Mendes FD, Jorgensen R, Keach J, Katzmann JA, Smyrk T, Donlinger J, et al. Elevated serum IgG4 concentration in patients with primary sclerosing cholangitis. Am J Gastroenterol. 2006;101:2070–5.
Oseini AM, Chaiteerakij R, Shire AM, Ghazale A, Kaiya J, Moser CD, et al. Utility of serum immunoglobulin G4 in distinguishing immunoglobulin G4-associated cholangitis from Cholangiocarcinoma. Hepatology. 2011;54:940–8.
Ohara H, Nakazawa T, Kawa S, Kamisawa T, Shimosegawa T, Uchida K, et al. Establishment of a serum IgG4 cut-off value for the differential diagnosis of IgG4-related sclerosing cholangitis: a Japanese cohort. J Gastroenterol Hepatol. 2013;28:1247–51.
Hamano H, Kawa S, Uehara T, Ochi Y, Takayama M, Komatsu K, et al. Immunoglobulin G4-related lymphoplasmacytic sclerosing cholangitis that mimics infiltrating hilar cholangiocarcinoma: part of a spectrum of autoimmune pancreatitis? Gastrointest Endosc. 2005;62:152–7.
Graham R, Smyrk T, Chari S, Takahashi N, Zhang L. Isolated IgG4-related sclerosing cholangitis: a report of 9 cases. Hum Pathol. 2014;45:1722–9.
Nakazawa T, Ikeda Y, Kawaguchi Y, Kitagawa H, Takada H, Takeda Y, et al. Isolated intrapacreatic IgG4-related sclerosing cholangitis. World J Gastroenterol. 2015;21:1334–43.
Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–4.
Ohara H, Nakazawa T, Sano H, Ando T, Okamoto T, Takada H, et al. Systemic extrapancreatic lesions associated with autoimmune pancreatitis. Pancreas. 2005;31:232–7.
Hamano H, Arakura N, Muraki T, Ozaki Y, Kiyosawa K, Kawa S. Prevalence and distribution of extrapancreatic lesions complicating autoimmune pancreatitis. J Gastroenterol. 2006;41:1197–205.
Naitoh I, Nakazawa T, Ohara H, Andoh T, Hayashi K, Tanaka H, et al. Clinical significance of extrapancreatic lesions in autoimmune pancreatitis. Pancreas. 2010;39:e1–5.
Sano H, Nakazawa T, Ando T, Hayashi K, Naitoh I, Okumura F, Miyabe K, Yoshida M, Takahashi S, Ohara H, Joh T. Clinical characteristics of inflammatory bowel disease associated with primary sclerosing cholangitis. J Hepatobiliary Pancreat Sci. 2011;18:154–61.
Nakanuma Y, Zen Y. Pathology and immunopathology of immunoglobulin G4-related sclerosing cholangitis: the latest addition to the sclerosing cholangitis family. Hepatol Res. 2007;37(Suppl 3):S478–86.
Zhang L, Lewis JT, Abraham SC, Smyrk TC, Leung S, Chari ST. IgG4+ plasma cell infiltrates in liver explants with primary sclerosing cholangitis. Am J Surg Pathol. 2010;34:88–94.
Kubota K, Kato S, Akiyama T, Yoneda M, Fujita K, Ogawa M. Differentiating sclerosing cholangitis caused by autoimmune pancreatitis and primary sclerosing cholangitis according to endoscopic duodenal papillary features. Gastrointest Endosc. 2008;68:1204–8.
Umemura T, Zen Y, Hamano H, Kawa S, Nakanuma Y, Kiyosawa K, et al. Immunoglobulin G4-hepatopathy: association of immunoglobulin G4-bearing plasma cells in liver with autoimmune pancreatitis. Hepatology. 2007;46:463–71.
Naitoh I, Zen Y, Nakazawa T, Ando T, Hayashi K, Okumura F, et al. Small bile duct involvement in IgG4-related sclerosing cholangitis: liver biopsy and cholangiography correlation. J Gastroenterol. 2011;46:269–76.
Tomiyama T, Uchida K, Matsushita M, Ikeura T, Fukui T, Takaoka M, et al. Comparison of steroid pulse therapy and conventional oral steroid therapy as initial treatment for autoimmune pancreatitis. J Gastroenterol. 2011;46:696–704.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Ohara, H., Naitoh, I., Hayashi, K., Miyabe, K., Nakazawa, T. (2019). Diagnostic Criteria. In: Kamisawa, T., Kim, MH. (eds) IgG4-Related Sclerosing Cholangitis. Springer, Singapore. https://doi.org/10.1007/978-981-10-4548-6_7
Download citation
DOI: https://doi.org/10.1007/978-981-10-4548-6_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-4547-9
Online ISBN: 978-981-10-4548-6
eBook Packages: MedicineMedicine (R0)