Abstract
-
Many treatment strategies either need modification or are not appropriate for patients with dementia. Treatment options will often depend on the setting of care and the availability of carers and need to be individualized.
-
Much of the assessment may need to be discussed with carers, and it is important to recognize that family members may feel uncomfortable discussing and being involved in this intimate area of care with their loved ones and vice versa.
-
Continence aids are often a mainstay of treatment. Options of modifying the environment to improve access and reduce the risk of falls and incontinence include decluttering, ensuring adequate lighting and highlighting the toilet.
-
Ensuring bowels are regular has a greater emphasis in dementia patients to avoid incontinence both of bowel and bladder.
-
Patients with Alzheimer’s disease may be managed with cholinesterase inhibitors that can cause or exacerbate urinary frequency and incontinence.
-
Medications used for urge incontinence should not be completely dismissed in patients with dementia despite their potential side effects.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
-
Many treatment strategies either need modification or are not appropriate for patients with dementia. Treatment options will often depend on the setting of care and the availability of carers and need to be individualized.
-
Much of the assessment may need to be discussed with carers, and it is important to recognize that family members may feel uncomfortable discussing and being involved in this intimate area of care with their loved ones and vice versa.
-
Continence aids are often a mainstay of treatment. Options of modifying the environment to improve access and reduce the risk of falls and incontinence include decluttering, ensuring adequate lighting and highlighting the toilet.
-
Ensuring bowels are regular has a greater emphasis in dementia patients to avoid incontinence both of bowel and bladder.
-
Patients with Alzheimer’s disease may be managed with cholinesterase inhibitors that can cause or exacerbate urinary frequency and incontinence.
-
Medications used for urge incontinence should not be completely dismissed in patients with dementia despite their potential side effects.
A 76-year-old woman with diabetes underwent a total hip joint replacement. She was a former Professor of the Arts who lived alone and in recent years had become more withdrawn, no longer attending her previous clubs or visiting colleagues. Her operation was deemed successful and her indwelling catheter from theatre was removed on day 3. The night nursing staff found themselves responding to her requests every hour for assistance to use the toilet with her bed sometimes wet before they arrived. An IDC was inserted to avoid the nocturnal disturbance to staff, but she subsequently developed a UTI and delirium. She was later discharged to rehabilitation where she made slow progress and appeared depressed. With the IDC removed, a pad was applied for the persistent wetness.
9.1 Introduction
9.1.1 Incontinence Is a Symptom, Not a Diagnosis
Urine incontinence is considered to be one of the “geriatric giants”. Unfortunately there is misperception amongst health professionals and society that it is an inevitable consequence of ageing with nothing that can be done. Without proper assessment, critical underlying conditions or treatment options that could greatly improve the lives of older people affected may be missed.
Incontinence has been associated with mood disorders, social isolation and risk of placement in residential care [1, 2]. It can result in a significant financial cost to the individual and society. Carers, who may need to provide assistance in toileting and personal hygiene, are at significant risk of fatigue [3].
A comprehensive geriatric assessment should include screening for incontinence as many older people are unlikely to volunteer this information [4, 5]. Clinicians need a sensitive approach, acknowledging any impact of culture or other beliefs may have on this embarrassing issue. Establishing rapport, understanding potential boundaries and obtaining consent for examinations are critical to the assessment process.
An older person is likely to have a multifactorial basis for their incontinence. The role of the physician is to evaluate the symptom of incontinence to determine potential underlying factors and the diagnosis. A multidisciplinary team approach of nursing, physiotherapists and other allied health will benefit the assessment and management. Depending on the underlying causes, geriatricians, urogynaecologists and urologists may have a role. The goal of assessment is to reduce the symptom burden and improve the quality of life for older individuals and their carers.
9.2 How Do We Normally Remain Continent?
9.2.1 Understanding the Underlying Physiology and Pathology
Remaining continent at any age requires a complex interaction of multiple body systems with suitable access to a toilet. Ageing changes can make an older person more vulnerable to the many disease processes, medications or environmental factors that can potentially lead to incontinence. The incidence of incontinence tends to be equivalent in men and women later in life [6].
9.3 Urinary System
Our bladder has two major functions physiologically: to store and expel urine. Storage is reliant on a compliant smooth muscle in the bladder with adequate supports in the form of pelvic floor musculature and sphincters. To expel urine an adequate bladder contraction is required to empty the bladder to less than 50 ml, ideally with an unobstructed urethra [7]. Normal physiological changes in an ageing bladder are reduced compliance and capacity, bladder sensation and contractility [8]. These changes can lead to higher residuals in older individuals and more frequent voiding.
9.3.1 Classifying the Pathological Conditions Affecting the Urinary System
There are three major syndromes affecting the urinary system leading to incontinence: stress, urge and overflow incontinence. There is commonly overlap, especially as we age, which is classified as mixed incontinence.
Stress incontinence is involuntary leakage of urine caused by increases in abdominal pressure such as coughing or sneezing [9]. It can be caused by weakness in the pelvic floor musculature leading to urethral hypermobility [10]. Major risk factors include increasing parity or complicated childbirths, obesity and repetitive straining that can worsen the integrity of the pelvic floor musculature. Stress incontinence can also result from weakness or deficiency of urinary sphincters. Examples of this include complications of prostate surgery in men or pelvic surgeries in women.
Urge incontinence involves involuntary leakage associated with an inability to defer voiding and a strong urge [9]. Frequency of small volumes and nocturia are commonly associated with this. There are a number of important causes to rule out in patients with urge incontinence such as bladder infections, calculi, malignancy or inflammation. Clues are often in the associated symptoms and if it is of recent onset. Otherwise the most likely pathology in the older person is neurologic or idiopathic detrusor overactivity. Neurologic aetiologies such as strokes or Parkinson’s can lead to an interruption to the normal inhibition of bladder relaxation with subsequent uninhibited bladder contractions. Idiopathic detrusor overactivity has an increasing prevalence with age and is a common cause [11].
Overflow incontinence occurs once the bladder has reached and exceeded maximum storage capacity leading to leakage [12]. This can be the result of obstruction to urine flow or a weak bladder contraction or a combination of the two. Neurological causes of bladder weakness in the older person include autonomic neuropathy from diabetes, Parkinson’s syndromes or spinal cord pathologies. Obstruction is typically related to the prostate in men and rarely gynaecological tumours or massive prolapses in women.
9.4 Nervous and Musculoskeletal Systems
Our urinary system is under the control of the central and peripheral nervous system. Conscious decisions about where, and when, to void are controlled by the frontal cortex. As the bladder fills up to capacity, this sensation becomes increasingly unpleasant, leading to a desire to void. This desire to void can also be triggered by our emotions, such as anxiety, or cues such as running water. It is these types of triggers that are often targeted by bladder retraining.
Our midbrain contains the micturition centre that coordinates the contraction of the bladder and relaxation of our sphincters and vice versa. The parasympathetics travelling via the pelvic nerve lead to contraction, whilst the sympathetics via T11–L2 lead to bladder relaxation. The internal sphincter and pelvic floor muscles receive the input of the somatic nervous system S2–S4 via the pudendal nerve, which supports the bladder’s storage of urine.

Once the desire to void is generated, an older person must be able to safely navigate to the toilet. Falls in particular are a major concern in the frail elderly especially at night. Conditions affecting balance and dexterity are also likely to impact on continence.
9.4.1 Pathological Conditions Affecting the Nervous System
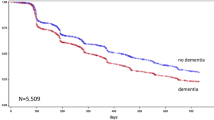
Dementia or strokes are examples of conditions affecting cortical control of continence. They can impair the ability to recognize the fullness of the bladder, response to urge signals and understanding socially appropriate places to void.
Detrusor sphincter dyssynergia describes the condition when there is incoordination of bladder contraction and sphincter relaxation due to abnormalities with the micturition centre or its signalling [13]. Importantly this can result in high pressures within the bladder from the obstruction to flow and poor bladder emptying. Conditions such as multiple sclerosis, cerebrovascular disease or spinal cord pathology can be the culprits.
Acute changes in bladder and bowel function including new onset incontinence should always lead to consideration of spinal cord pathology.
9.5 Assessment
The goal of assessment is to determine the factors that have led to incontinence and their reversibility. In the geriatric population, there may not be any specific bladder pathology, but managing other factors identified in the assessment can still lead to excellent results. Where possible, assessing someone in their home is often the best, allowing an insight into the patient’s environment and how they are coping. It is always important to rule out potentially sinister underlying causes first.
9.5.1 Key Areas to Focus on in History
9.5.1.1 Lower Urinary Tract Symptoms
Lower urinary tract symptoms can be non-specific, but an attempt should be made to determine to what degree the patient is suffering from urge (Do you leak or have difficulty holding on when the urge to pass urine comes on? Do you leak on the way to the toilet?) or stress incontinence (Do you leak when you cough, sneeze or perform physical tasks such as lifting or exercise?). The duration of these symptoms and their change over time should be explored. Other general questions include the frequency of toileting, the presence of hesitancy, the quality of the stream and whether they feel completely empty after voiding. Serious pathology may be present if there has been haematuria, pelvic pain, dysuria or systemic symptoms such as loss of weight or fever. A history of recurrent urinary tract infections should also be asked as this may be an indicator of poor bladder emptying, renal tract calculi or anatomical abnormalities of the urinary tract. Finally the impact of anxiety and mood disorders on bladder function needs to be explored.
9.5.1.2 Nighttime Symptoms and Nocturia
Many elderly who seek assistance with bladder control do so because of interruption to sleep with potential consequences of daytime fatigue, carer stress or falls [14, 15]. Sleep can be disturbed by nocturia or waking after an episode of nocturnal enuresis. Due to decreasing bladder capacity as we age, getting up twice at night or less may be considered normal.
A good sleep history is required to determine whether waking is due to the need to void or there is some other factor such as mental health, restless legs or poor sleep hygiene causing waking with subsequent voiding, “just in case”.
Nocturia may be due to nocturnal polyuria which is defined generally as a greater than 33% of a 24-h output occurring overnight [16]. This can be diagnosed with the aid of a bladder diary. When present, questions will need to be directed at potentially underlying causes including edematous states (e.g. congestive cardiac failure) polyuric conditions (diabetes insipidus and mellitus) or obstructive sleep apnea (affecting ADH production). Older people whose blood pressure does not fall overnight may also lead to greater urine production, but the overall relationship between blood pressure and nocturia is not entirely clear [17].
9.5.1.3 Neurological History
Questions regarding falls, balance problems or cognitive difficulties are useful to screen for possible underlying neurological conditions contributing to incontinence.
9.5.1.4 Bowels
The bowels need to be considered both specifically for their own management and also their impact on bladder continence. Physiological changes in the bowels during ageing include reduced rectal sensation and reduced external sphincter squeeze pressure [18]. Baseline questions should include the frequency and softness of the stool, whether there is any straining, and if faecal incontinence is present. Questions gauging the degree of leakage, urgency and the presence or absence of anal sensation should follow.
Recent changes in bowel habit may indicate serious underlying bowel pathology (malignancy, inflammatory conditions, etc.). Once serious pathology is excluded, often diet, fibre and fluid intake need exploring to establish their potential role in either constipation or loose stools. Constipation in particular can exacerbate urgency symptoms and reduce bladder emptying. Medications, including previous and current laxative, should be reviewed.
9.5.1.5 Obstetric and Gynaecological History
Even with older patients enquiring about the number of babies they had, birth weights, types of deliveries and whether there were any complications will help determine the potential risk for pelvic floor muscle weakness. Asking about prolapses is also important, as they are often associated with pelvic muscle weakness. The timing of menopause and previous use of hormone replacement therapy will help screen for vaginal atrophy. Previous operations for stress incontinence, IDCs or other pelvic procedures should be asked about.
9.5.1.6 Oral Intake and Weight
Many older people drink less than the recommended 1.5–3 L of fluid a day to avoid incontinence, placing them at risk of dehydration and constipation. Drinking more than this may suggest a polyuric condition. Caffeinated drinks such as coffee, tea and soft drinks can exacerbate urge and frequency. Obese patients should have their diet and motivation reviewed to determine the potential for weight loss.
9.5.1.7 Medication Review
Polypharmacy is common in the elderly, and there are many drugs that can impact on bladder or bowel function directly or indirectly. Drugs that can exacerbate urge symptoms include diuretics or cholinesterase inhibitors. Drugs that impair bladder emptying include those with anticholinergic properties such as TCADs or antipsychotics or indirectly by the multitude of drugs that lead to constipation. Any drug that can cause sedation or delirium will potentially impact on cognitive control of continence. In all cases a thorough review of these medications as to their ongoing indication or whether alternatives could be used should be explored.
9.5.1.8 Home Environment
Questions should be asked regarding the location of toilets and lighting and whether walking aids or home modifications are required to reduce the risk of falls and incontinence.
9.5.1.9 Degree of Bother
Ascertaining the degree of bother of a client’s bladder symptoms is imperative in determining the amount of investigation and management desired. How many pads or other aids an older person is using will give an idea about the degree of wetness. Questions also need to be asked about whether there is avoidance of social interaction, jobs or intimate relationships. Carers should be asked about whether they are fatigued by the burden of attending to personal hygiene or sleep deprived.
9.5.1.10 Bladder and Bowel Diaries
Diaries are an objective assessment tool that can assist with diagnosis as well as providing useful feedback to the patient about their current habits. A standard bladder diary will reveal the type and amount fluid intake, urine output with the volumes voided and frequency, as well as comments on leakage and potential triggers. Bladder diaries can help diagnose nocturnal polyuria. Ideally they should be completed over three days, and this may need assistance from carers. Bowel charts can similarly objectively determine the frequency and consistency of stool.
The arts professor’s bladder diary one month post-rehab admission
Date | Time | Fluid intake (ml) | Urine output (ml) | Comments |
|---|---|---|---|---|
8/11 | 06:00 | 100 | Wet bed | |
07:30 | Coffee 250 | |||
08:00 | 75 | |||
09:45 | 75 | |||
10:00 | Coffee 250 | |||
10:10 | 150 | Wet pad ++ on way to toilet | ||
11:00 | 100 | |||
13:00 | Coffee 250 | |||
13:15 | 50 | Wet pad +++ on way to toilet | ||
15:00 | Water 50 | 50 | ||
15:30 | Coffee 200 | |||
16:00 | 75 | |||
18:00 | Water 200 | 150 | Wet pad + on way to toilet | |
20:00 | Wine 200 | |||
22:00 | 50 | Went to bed 2300 | ||
9/11 | 01:00 | 75 | ||
02:00 | Water 50 | 10 | ||
04:00 | 50 | Wet bed on waking | ||
05:00 | 25 | |||
07:00 | 50 | Got up at 0700 | ||
Totals | 1450 | 1085 + wet pads | ||
Overnight output 210/1085 = 19% |
9.6 Examination
The important components of examination.
9.6.1 Neurological
A complete neurological examination is required with a focus on excluding:
-
Extrapyramidal syndromes
-
Spinal cord or cauda equina syndromes
-
Cerebrovascular disease
-
Autonomic neuropathies
9.6.2 Cardiovascular
-
Fluid assessment
-
Postural BP
9.6.3 Gynaecological/Groin Examination
-
PV examination:
-
Prolapses
-
-
Demonstrations of stress incontinence:
-
Vaginal atrophy
-
Rashes
-
Pelvic floor muscle strength
-
-
Penis examination:
-
Anatomical abnormalities
-
9.6.4 Abdominal
-
PR examination—masses, anal tone, faecal matter, prostate size
9.7 Investigations
Routine testing for urinary incontinence should include:
-
1.
Dipstick/MSU to exclude active sediments, infection or inflammation.
-
2.
Post-void residual/ultrasound—Repeat measurements can improve accuracy. Formal renal ultrasounds should be ordered with markedly raised residuals or worsening renal function.
-
3.
Blood tests to screen for any clinically suspected underlying conditions.
Further investigations of the bladder will be determined by clinical suspicion. Investigations for faecal incontinence may include screening for underlying conditions or more specifically investigations to ensure adequate anal sphincter integrity such as anal manometry or ultrasound.
9.8 Urodynamics
Urodynamics is the investigation of choice to confirm the presence of stress incontinence, detrusor overactivity and whether there is obstruction or hypocontractility causing poor bladder emptying. The results include measurements of bladder capacity, compliance and bladder and urethral pressures during filling and voiding. When combined with video, further information is obtained such as the underlying mechanism of stress incontinence, the presence of bladder diverticulum indicating high pressures and the ability to diagnose detrusor sphincter dysnergia.
It is used less as people age as it can be technically difficult and embarrassing and is rarely used in patients with cognitive impairment. Indications may include diagnostic dilemmas after failed conservative management, if surgery is being considered or if there is a suspicion of a high pressure bladder [19].
9.9 Treatment Options
9.9.1 General Principles
The first important step in managing incontinence in the older person is to provide an explanation to patients and carers about the causes for their incontinence. In addition to understanding the basis for their incontinence and therefore its management, such explanation also provides reassurance for those patients who may have been worried that a sinister underlying pathology was causing their symptoms. Appropriate continence aids should be advised with the aim of achieving social continence. Products including pads and pull-up underwear, toilets or bottles, IDCs and condom drainage and mattress protectors may be enough to address concerns about personal hygiene and smell. All of the factors otherwise identified in assessment such as fluid intake, diet, bowel management, medications and mental health should be addressed. These conservative measures alone may be sufficient to improve and manage incontinence to a satisfactory level and usually should be implemented prior to further management.
Topical oestrogen therapy may have a role in treating incontinence in postmenopausal women with possibilities of improvement with urge and stress symptoms, with its main role in alleviating the symptoms of vaginal atrophy [20].
9.10 Stress Incontinence Management Options
9.10.1 General Measures
The initial steps are to reduce weight and avoid or manage precipitating factors such as heavy lifting or cough.
9.10.2 Pelvic Floor Exercises
For those older persons with adequate cognition and motivation, a course of pelvic floor exercises usually over many months can produce benefits with incontinence and small prolapses [21]. Correct identification of pelvic floor muscles and technique may require a continence physiotherapist.
9.10.3 Surgical Options
For those with persistent troublesome symptoms despite conservative measures, corrective procedures including slings for women or artificial sphincters for men can be explored. Age alone should not be a barrier for an assessment with a surgeon, with many operations able to be done as day procedures.
9.11 Urge Incontinence Management Options
9.11.1 Bladder Retraining
For motivated cognitively intact older individuals, bladder retraining involves employing deferment techniques when the urge to pass urine is first felt, to delay voiding. The goal of this process is to “train the bladder” to hold more urine, which over time can increase the functional bladder capacity, reducing urge and frequency [22]. Examples of simple deferment techniques include curling toes or counting slowly to ten. Pelvic floor exercises or medication can enhance this process to achieve good results [21]. Using bladder diaries before and after bladder training can objectively assess improvements.
9.11.2 Medications
Medications are effective in reducing incontinence, urge and frequency [23]. The choice of medication is often determined by cost and their differing side effect profile. Whilst they can lead to improvement after days, usually a few weeks is required to assess their initial effectiveness. Some individuals will use them only as needed before going out or before the most bother sometimes such as at night. There is no absolute on treatment duration, but some may choose to cease after feeling they have successfully retrained their bladder, whilst others will continue as long as symptoms are being alleviated. It is not advised to use these medications where poor bladder emptying co-exists unless catheter drainage is also being used.
9.11.3 Antimuscarinics
Bladder targetting anticholinergic agents (e.g. oxybutynin, darifenacin, solifenacin) are thought to act by reducing bladder contractions during filling [23]. They can be limited in the elderly by their side effect profile, with typical anticholinergic effects such as dry mouth, dry eyes and to a lesser extent constipation sometimes leading to cessation of therapy. Their potential for cognitive side effects in the geriatric population means that monitoring is recommended and caution is needed in those with baseline impairment.
9.11.4 Beta 3-Adrenoceptor Agonists
Mirabegron is a newer agent that directly activates relaxation of the smooth muscle of the bladder [24]. Side effects of note include potential severe rises in blood pressure. Otherwise tachycardia and potential prolongation of the QT interval are recognized. It may have benefit in the elderly due to the likely lack of cognitive side effects, but currently cost can be prohibitive.
9.11.5 Botulinum Toxin Therapy
For those with persistent urge incontinence due to detrusor overactivity, direct injections of botulinum toxin into the bladder can be of benefit [25]. It requires that a patient has the capacity to self-catheterize in the event of a temporary atonic bladder which can be an issue in the elderly. Beneficial effects can last 6–12 months or longer with repeated dosing possible [23].
9.11.6 Other Therapies
There is limited availability and practice of treatments such as sacral nerve stimulation or neuromodulation for incontinence, but clinicians should be aware that some specialists may be able to offer these or other surgical options in severe cases.
9.12 Poor Bladder Emptying
9.12.1 General Measures
Poor bladder emptying may be improved by addressing constipation or ceasing medications with anticholinergic actions. Double voiding is a practice of returning to the toilet soon after the initial attempt to empty the bladder, to see if further emptying is possible. Where appropriate, surgery should be considered for outflow obstruction such as that caused by an enlarged prostate.
9.12.2 Catheter Drainage
There is no absolute value of a post-void residual at which catheters should be introduced. Clear indications include retention, pain, worsening renal function or hydronephrosis. Urodynamic features such as the presence of a high pressure bladder (e.g. in detrusor sphincter dyssynergia) can lead to potential recommendations of the use of catheters to avoid potential renal dysfunction [13]. Another indication in the geriatric population may include the use of short-term catheters to allow wound healing should urine incontinence be compromising this. Where possible intermittent self-catheterization is preferred to permanent indwelling catheters, as a good technique is associated with reduced UTIs and can allow for greater freedom including sexual expression [26].
9.13 Nocturia
If nocturia is thought to be attributable to the conditions that have already been discussed, then the treatment won’t differ. If nocturnal polyuria is detected, treating any underlying cause should be the first goal of therapy. Minimizing oral fluids after dinner and afternoon diuretics can be trialled, but results are variable. If nocturnal polyuria is persistent, then DDAVP is a potential treatment option. However in the elderly, it would need to be used with great caution because of the potential for severe hyponatraemia and its consequences.
9.14 Continence Strategies in Patients with Dementia
Many of the treatment strategies already discussed either need modification or are not appropriate for patients with dementia. Treatment options will often depend on the setting of care and the availability of carers and need to be individualized. Much of the assessment may need to be discussed with carers, and it is important to recognize that family members may feel uncomfortable discussing and being involved in this intimate area of care with their loved ones and vice versa.
9.14.1 General Measures
Continence aids are often a mainstay of treatment, but they can be refused by some some patients who are resistive to care. Options of modifying the environment to improve access and reduce the risk of falls and incontinence include decluttering, ensuring adequate lighting and highlighting the toilet, for example, using a coloured toilet seat if everything else is white. A floor mat alarm can provide an early warning system for carers if the risk of falls is high, so that assistance can be provided for toileting overnight. For daytime symptoms timed or prompted toileting may be trialled for patients who have poor mobility or apathy [27]. Taking them to the toilet at regular intervals or after meals may prevent episodes of incontinence. Ensuring bowels are regular has a greater emphasis in dementia patients to avoid incontinence both of the bowel and bladder.
9.14.2 Medication Considerations
Patients with Alzheimer’s disease may be managed with cholinesterase inhibitors that can cause or exacerbate urinary frequency and incontinence [28]. There will be occasions when ceasing cholinesterase inhibitors may be warranted when the urinary symptoms are more bothersome than the perceived cognitive benefits. Medications used for urge incontinence should not be completely dismissed in patients with dementia despite their potential side effects. As long as the patient has a carer who can observe for cognitive side effects and take appropriate action, they might be able to reduce some of the burden of caring when a reduction in nocturia or incontinence is achieved.
The Case Revisited
In this case a simple brief bedside assessment would have identified potentially reversible factors leading to the Professor’s incontinence. She had suffered for many years with frequency and urgency and minimal stress incontinence symptoms. She became very worried that she would smell of urine so she avoided going out. This led to depression, and she had actually deferred her THJR previously as she was worried about the management of her incontinence in hospital. She had no neurology or other worrying features on history and examination. Her MSU was normal, and a post-void residual revealed only 23 ml. A presumptive diagnosis of idiopathic detrusor overactivity with urge incontinence was made.
She was linked into a continence clinic after leaving rehab, and a geriatrician advised her to cut back on her four coffees a day, and she commenced bladder retraining with a continence physiotherapist. She gained some improvement with this and elected to also try an anticholinergic given the severity of her symptoms. Four months later she was almost dry; she wore pads for minor leakage and had started attending her previous social engagements. She typically only got up once a night!
References
Morrison A, Levy R. Fraction of nursing home admissions attributable to urinary incontinence. Value Health. 2006;9:272.
Coyne KS, Wein AJ, Tubaro A, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009;103(Suppl 3):4.
Gotoh M, Matsukawa Y, Yoshikawa Y, et al. Impact of urinary incontinence on the psychological burden of family caregivers. Neurourol Urodyn. 2009;28:492.
Griffiths AN, Makam A, Edwards GJ. Should we actively screen for urinary and anal incontinence in the general gynaecology outpatients setting?—a prospective observational study. J Obstet Gynaecol. 2006;26(5):442–4.
Teunissen D, van Weel C, Lagro-Janssen T. Urinary incontinence in older people living in the community: examining help-seeking behaviour. Br J Gen Pract. 2005;55:776–82.
Gibbs CF, Johnson TM II, Ouslander JG. Office management of geriatric urinary incontinence. Am J Med. 2007;120(3):211–20.
Huang AJ, Brown JS, Boyko EJ, Moore EE, Scholes D, Walter LC, Lin F, Vittinghoff E, Fihn SD. Clinical significance of postvoid residual volume in older ambulatory women. J Am Geriatr Soc. 2011;59(8):1452–8. 7p
Zimmern P, Litman HJ, Nager CW, et al. Effect of aging on storage and voiding function in women with stress predominant urinary incontinence. J Urol. 2014;192:464.
IUGA/ICS Joint Report on the Terminology for Female Pelvic Floor Dysfunction. Standardisation and Terminology Committees IUGA and ICS, Joint IUGA/ICS Working Group on Female Terminology. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. Neurourol Urodyn. 2010;29(1):4–20. Int Urogynecol J. 2010;21:5–26.
Smith PP, van Leijsen SA, Heesakkers JP, Abrams P, Smith AR. Can we, and do we need to, define bladder neck hypermobility and intrinsic sphincteric deficiency?: ICI-RS 2011. Neurourol Urodyn. 2012;31:309–12.
Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36.
DuBeau CE, Kuchel GA, Johnson T II, Palmer MH, Wagg A. Incontinence in the frail elderly: report from the fourthth international consultation on incontinence. Neurourol Urodyn. 2010;29(1):165–78.
Bacsu CD, Chan L, Tse V. Diagnosing detrusor sphincter dyssynergia in the neurological patient. BJU Int. 2012;109(Suppl 3):31–4.
Foley AL, Loharuka S, Barrett JA, Mathews R, Williams K, McGrother CW, Roe BH. Association between the Geriatric Giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age Ageing. 2012;41(1):35–40.
Santini S, Andersson G, Lamura G. Impact of incontinence on the quality of life of caregivers of older persons with incontinence: a qualitative study in four European countries. Arch Gerontol Geriatr. 2016;63:92–101.
Weiss JP, Bosch JL, Drake M, Dmochowski RR, Hashim H, Hijaz A, Johnson TM, Juul KV, Nørgaard JP, Norton P, Robinson D, Tikkinen KA, Van Kerrebroeck PE, Wein AJ. Nocturia Think Tank: focus on nocturnal polyuria. Neurourol Urodyn. 2012;31:330–9.
Feldstein CA. Review Article: Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens. 2013;7(1):75–84.
Gardiner AB. The effects of ageing on the gastrointestinal system. Nurs Resid Care. 2013;15(1):30–3.
Yared J, Gormley EA. The role of urodynamics in elderly patients. Clin Geriatr Med. 2015;31:567–9.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012;10:CD001405.
Dumoulin C, Hay-Smith EJ, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;5:CD005654.
Karon S. A team approach to bladder retraining: a pilot study. Urol Nurs. 2005;25(4):269–76.
Bardsley A. Drug therapies for postmenopausal urinary incontinence. Nurse Prescrib. 2015;13(2):80–6.
Sanford M. Mirabegron: a review of its use in patients with overactive bladder syndrome. Drugs. 2013;73(11):1213–25.
Cruz F, Nitti V. Clinical data in neurogenic detrusor overactivity (NDO) and overactive bladder (OAB). Neurourol Urodyn. 2014;33(Suppl 3):S26–31. ISSN: 1520-6777
Wilson M. Clean intermittent self-catheterisation: working with patients. Br J Nurs. 2015;24(2):76–85.
Hägglund D. A systematic literature review of incontinence care for persons with dementia: the research evidence. J Clin Nurs. 2010;19(3/4):303–12.
Starr JM. Cholinesterase inhibitor treatment and urinary incontinence in Alzheimer’s disease. J Am Geriatric Soc. 2007;55:800–1.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 The Editor(s)
About this chapter
Cite this chapter
Marriott, J. (2018). The Problem of Incontinence in the Elderly. In: Nair, B. (eds) Geriatric Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-10-3253-0_9
Download citation
DOI: https://doi.org/10.1007/978-981-10-3253-0_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3252-3
Online ISBN: 978-981-10-3253-0
eBook Packages: MedicineMedicine (R0)