Abstract
Advances in virology of the hepatitis C virus (HCV) have enabled rapid progress in developing direct-acting antivirals (DAAs) that directly target viral proteins. The use of these drugs has considerably improved treatment outcomes. However, the effects of these inhibitors are weakened by the presence of resistance-associated variants (RAVs). In addition, it is becoming clear that DAA-resistant variants exist in a certain proportion of cases that are naïve to DAAs. Genotype 1b variants that are resistant to NS3 protease inhibitors exist naturally, although they are uncommon. Variants resistant to nucleotide NS5B inhibitors are almost never observed in treatment-naïve patients. Conversely, the genotype 1b NS5A Y93H variant and the genotype 1a NS3 Q80K variant, which are resistant to NS5A or NS3/4 inhibitors, respectively, reportedly exist at relatively high frequency; hence, more care needs to be taken when administering DAA treatment.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- HCV
- Direct-acting antivirals (DAAs)
- Resistance-associated variants (RAVs)
- NS5A inhibitor
- Protease inhibitor
6.1 Introduction
Hepatitis C virus (HCV) infects 170 million people worldwide and is a major pathogen causing liver cirrhosis and hepatocellular carcinoma [1, 2]. In Japan, there are over 1.5 million patients with chronic hepatitis C, many of whom are elderly and have increased risk of liver cancer. Because chronic hepatitis C is the primary cause of chronic liver disease and liver cancer, effective antiviral therapies are needed to reduce cancer-related deaths. For a number of years, combination therapy with interferon and ribavirin remained the standard of care therapy for chronic hepatitis C. However, the sustained virological response rate associated with this therapy in patients with HCV genotype 1 infection is insufficient at around 50 % [3]. In addition, the need for interferon-free therapies has become dire owing to the discovery of cases that are nonresponsive to interferon therapy, including those with an unfavorable SNP genotype in the IFNL3 locus [4].
In 1999, Lohmann et al. developed a way to culture HCV strains in vitro [5]. Along with advancements in the structural analyses of HCV proteins, this innovation led to rapid progress in developing direct-acting antivirals (DAAs), which directly target viral proteins. DAAs are broadly divided into three classes: those that inhibit the HCV NS3 protease, those that inhibit the HCV NS5A protein, and those that inhibit the NS5B polymerase. Combination therapies with these DAAs have reportedly achieved positive therapeutic effects in patients with an unfavorable (non-TT) genotype IFNL3 as well as in patients with liver cirrhosis and elderly patients, for whom interferon therapy is poorly tolerated [6, 7]. However, these inhibitors are reported to be less effective in the presence of resistance-associated variants (RAVs).
While these DAAs have extremely high antiviral activities, RAVs are known to appear at high frequencies when administered alone. As stated above, the therapeutic effects can decrease considerably when RAVs are present. In addition, it is becoming clear that DAA-resistant variants exist naturally in a certain proportion of cases that are naïve to DAAs. The NS5A Y93H and L31M/V variants, which are resistant to NS5A inhibitors, are reported to exist at relatively high frequencies in genotype 1b HCV cases. Similarly, naturally occurring DAA-resistant variants such as NS3 Q80K, which is known to attenuate the effects of simeprevir, exist at relatively high frequencies in patients with genotype 1a. In this chapter, we describe the frequency and resistance profiles of naturally occurring HCV variants and outline their viral characteristics.
6.2 Naturally Occurring Protease Inhibitor-Resistant Variants
DAAs that inhibit HCV protease were developed first, due to the early determination of the structure of the HCV protease. The HCV NS3/4A protein is known to function as a protease that enables HCV proteins to function by cleaving the nonstructural proteins from the translated HCV polyprotein. Therefore, inhibiting the activity of HCV protease can suppress viral replication. HCV protease inhibitors are divided into two groups based on their structure. One group is the first-generation protease inhibitors, which include telaprevir and boceprevir, which have a linear molecular structure with no branches. Succeeding these drugs were the second wave and second-generation drugs, such as simeprevir and vaniprevir, which have circular (macrocyclic) or branched molecular structures. There are RAVs with profiles unique to both first-generation and second-generation protease inhibitors.
Variants resistant to the first-generation protease inhibitor telaprevir include the V36, T54, R155, A156, and V170 variants. In a Japanese study using direct sequencing by Suzuki et al., V36A and T54S variants were detected in 0.3 % (1/307) and 3.3 % (10/307) of DAA-naïve cases, respectively [8]. An investigation of 493 cases by Itakura et al. found T54S and A156S in 2.8 % (14/493) and 0.2 % (1/493) of cases, respectively [9] (Table 6.1).
Known RAVs affecting the second-generation protease inhibitors simeprevir, vaniprevir, and asunaprevir include the Q80K/R, R155K, A156S/T, and D168V/A/E/T variants. Q80K is observed more frequently before treatment in genotype 1a cases. In a population sequencing study, these RAVs were found in about 20 % of genotype 1a cases, although they were relatively rare in genotype 1b cases, which are common in Japan [10]. In the Japanese study by Suzuki et al., Q80R was found in 0.7 % (2/307) of cases, no instances of R155K were found, and D168V/A/E/T was found in 0.7 % (2/307) of cases [8]. The investigation of 493 cases by Itakura et al. found Q80K in 2.2 % (11/493) and D168V/A/E/T in 1.2 % (12/493) of cases, indicating that these variants are relatively rare [9] (Table 6.1).
6.3 Naturally Occurring NS5A Inhibitor-Resistant Variants
The HCV NS5A protein is a phosphorylated protein formed from 450 amino acids. Its functions have not been fully clarified, but it is known that NS5A exists as a dimer, possesses an RNA-binding domain, and binds with HCV RNA. As it is a part of the HCV replication complex, it is known to be involved in viral replication, although it also has important functions in particle formation and virus release. NS5A inhibitors are thought to bind with NS5A domain 1. Since this is a relatively well-preserved structure even between genotypes, picomolar quantities of NS5A inhibitors successfully exert their effects against the HCV replicons of several genotypes. NS5A inhibitors include daclatasvir, which in Japan is approved for use in combination with the protease inhibitor asunaprevir; the recently approved ledipasvir, which is combined with the NS5B inhibitor sofosbuvir; and ombitasvir, which is expected to be approved for use in combination with protease inhibitors.
NS5A inhibitors, while having strong antiviral activity as described above, are problematic because of the high proportion of naturally occurring NS5A inhibitor-resistant variants. In a phase III trial for daclatasvir/asunaprevir combination therapy in Japan, NS5A variants conferring resistance (Y93H, L31M/V) were found in 31 out of 222 cases. The SVR rate of these 31 cases was poor, at 45 % (14/31) [6].
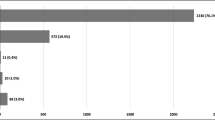
The existence of NS5A inhibitor-resistant variants in patients who have never been exposed to NS5A inhibitors has also been reported in Japan. In a direct sequencing study, Suzuki et al. observed Y93H variants in 8.2 % (24/294) and L31M in 2.7 % (8/294) of 294 cases. Furthermore, they observed the Y93H/L31 double mutant, which is known to be strongly resistant, in 0.3 % (1/294) of cases (Table 6.2). Itakura et al. reported Y93H in 19 % (78/410) and L31M in 2.2 % (9/410) of 410 cases. Miura et al. used next-generation sequencing to track NS5A inhibitor-resistant variants. They found Y93H in 30.9 % (34/110) and L31M/V/I in 11.8 % (13/110) of cases [11].
Surprisingly, the NS5A Y93H variant has also been reported to be associated with clinical factors. Miura et al. reported that Y93H was significantly more common in patients with the major IFNL3 SNP genotype. Itakura et al. also reported that Y93H was significantly more common when the IFNL3 SNP was the major type, as well as when platelet levels were low and the HCV viral load was high.
6.4 Naturally Occurring NS5B Inhibitor-Resistant Variants
The HCV NS5B protein functions as an RNA-dependent RNA polymerase and is essential for the replication of viral RNA. There are two classes of HCV NS5B inhibitors: nucleotide and non-nucleotide HCV NS5B inhibitors. Non-nucleotide inhibitors bind with NS5B catalyst domains to inhibit polymerase activity. Broadly, there are four types of non-nucleotide polymerase inhibitors that target different epitopes of the NS5B polymerase, and specific RAVs exist for each of them [12].
Nucleotide inhibitors inhibit replication of the viral genome when they are incorporated in the growing strand by the NS5B polymerase during viral RNA synthesis, causing chain termination. Thus, RAVs are less likely to arise for nucleotide polymerase inhibitors than for other DAAs, and these drugs possess antiviral activities against several HCV genotypes. Sofosbuvir is a nucleotide polymerase inhibitor that is currently being introduced in first-line therapies. In Japan it is being introduced clinically in combination with RBV to treat genotype 2 cases and is covered by health insurance to treat genotype 1-infected patients in combination with the NS5A inhibitor ledipasvir. A well-known sofosbuvir-resistant variant is S282T [13]. However, while this variant has been shown to dramatically decrease efficacy of the drug in vitro, it is reported to be very uncommon in nature. In a phase III trial for sofosbuvir as well as in database analysis, the S282T variant was not observed in a single case at baseline and is thought to be almost nonexistent in the natural environment [7, 14, 15] (Table 6.3). Thus, naturally occurring NS5B S282T variants are not expected to be a significant problem clinically.
6.5 Conclusion
As described above, drug-resistance variants are found to a certain extent in the natural environment. Depending on the treatment protocol, these RAVs can dramatically reduce the effectiveness of therapy. As such, the presence of RAVs before treatment should be investigated, and appropriate therapies should be selected. Further, it is becoming clear that RAVs appear at a high frequency in cases in which DAA therapy fails. Furthermore, new treatments designed to overcome RAVs that appear in the case of DAA treatment failure need to be investigated.
References
Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333–42.
Seeff LB. Natural history of chronic hepatitis C. Hepatology. 2002;36:S35–46.
McHutchison JG, Lawitz EJ, Shiffman ML, Muir AJ, Galler GW, McCone J, Nyberg LM, et al. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med. 2009;361:580–93.
Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, Sakamoto N, Nakagawa M, et al. Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet. 2009;41:1105–9.
Lohmann V, Korner F, Koch J, Herian U, Theilmann L, Bartenschlager R. Replication of subgenomic hepatitis C virus RNAs in a hepatoma cell line. Science. 1999;285:110–3.
Kumada H, Suzuki Y, Ikeda K, Toyota J, Karino Y, Chayama K, Kawakami Y, et al. Daclatasvir plus asunaprevir for chronic HCV genotype 1b infection. Hepatology. 2014;59:2083–91.
Mizokami M, Yokosuka O, Takehara T, Sakamoto N, Korenaga M, Mochizuki H, Nakane K, et al. Ledipasvir and sofosbuvir fixed-dose combination with and without ribavirin for 12 weeks in treatment-naive and previously treated Japanese patients with genotype 1 hepatitis C: an open-label, randomised, phase 3 trial. Lancet Infect Dis. 2015;15:645–53.
Suzuki F, Sezaki H, Akuta N, Suzuki Y, Seko Y, Kawamura Y, Hosaka T, et al. Prevalence of hepatitis C virus variants resistant to NS3 protease inhibitors or the NS5A inhibitor (BMS-790052) in hepatitis patients with genotype 1b. J Clin Virol. 2012;54:352–4.
Itakura J, Kurosaki M, Takada H, Nakakuki N, Matsuda S, Gondou K, Asano Y, et al. Naturally occurring, resistance-associated hepatitis C virus NS5A variants are linked to IL28B genotype and are sensitive to interferon-based therapy. Hepatol Res. 2015;45(10):E115–21.
Sarrazin C, Lathouwers E, Peeters M, Daems B, Buelens A, Witek J, Wyckmans Y, et al. Prevalence of the hepatitis C virus NS3 polymorphism Q80K in genotype 1 patients in the European region. Antiviral Res. 2015;116:10–6.
Miura M, Maekawa S, Sato M, Komatsu N, Tatsumi A, Takano S, Amemiya F, et al. Deep sequencing analysis of variants resistant to the non-structural 5A inhibitor daclatasvir in patients with genotype 1b hepatitis C virus infection. Hepatol Res. 2014;44:E360–7.
McCown MF, Rajyaguru S, Le Pogam S, Ali S, Jiang WR, Kang H, Symons J, et al. The hepatitis C virus replicon presents a higher barrier to resistance to nucleoside analogs than to nonnucleoside polymerase or protease inhibitors. Antimicrob Agents Chemother. 2008;52:1604–12.
Svarovskaia ES, Dvory-Sobol H, Parkin N, Hebner C, Gontcharova V, Martin R, Ouyang W, et al. Infrequent development of resistance in genotype 1–6 hepatitis C virus-infected subjects treated with sofosbuvir in phase 2 and 3 clinical trials. Clin Infect Dis. 2014;59:1666–74.
Omata M, Nishiguchi S, Ueno Y, Mochizuki H, Izumi N, Ikeda F, Toyoda H, et al. Sofosbuvir plus ribavirin in Japanese patients with chronic genotype 2 HCV infection: an open-label, phase 3 trial. J Viral Hepat. 2014;21:762–8.
Combet C, Garnier N, Charavay C, Grando D, Crisan D, Lopez J, Dehne-Garcia A, et al. euHCVdb: the European hepatitis C virus database. Nucleic Acids Res. 2007;35:D363–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Suda, G., Ito, J., Morikawa, K., Ogawa, K., Sakamoto, N. (2017). Incidence and Characteristics of Naturally Occurring Drug-Resistant Hepatitis C Virus Strains. In: Chayama, K. (eds) Hepatitis C Virus Treatment. Springer, Singapore. https://doi.org/10.1007/978-981-10-2416-0_6
Download citation
DOI: https://doi.org/10.1007/978-981-10-2416-0_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2415-3
Online ISBN: 978-981-10-2416-0
eBook Packages: MedicineMedicine (R0)