Abstract
Diabetes is a major problem affecting millions of people today and if left unchecked can create enormous implication on the health of the population. Among the various noninvasive methods of detection, breath analysis presents an easier, more accurate and viable method in providing comprehensive clinical care for the disease. This paper examines the concentration of acetone levels in breath for monitoring blood glucose levels and thus predicting diabetes. The analysis uses the support vector mechanism to classify the response to healthy and diabetic samples. For the analysis ten subject samples of acetone levels are taken into consideration and are classified according to three labels which are healthy, type 1 diabetic and type 2 diabetic.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
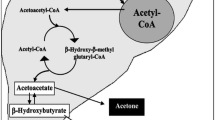
Diabetes can be described as a group of metabolic diseases where the blood glucose level in the body is higher than the normal prescribed parameter. When a person suffers from diabetes, it is seen that their body is either unable to secrete enough insulin or their body is not able to use the insulin produced by the liver. This causes sugar to build up in the blood thus leading to diabetes. There are two major types of diabetes which include type 1 and type 2. Type 1 diabetes is the result of the body ‘s failure to produce enough insulin. While type 2 is a condition in which cells fail to respond to the insulin produced in the body properly. It is seen that the prescribed parameter of blood glucose levels (BGL) in healthy subjects before meals is around 70–80 mg/dL. Sugar less than 100 mg/dL while fasting is considered normal by today’s standards. Any BGL higher than normal is considered unhealthy. The most common method of obtaining glucose levels in the body is by drawing blood samples using invasive techniques. A lancet device is used to draw the blood by pricking the figure or the forearm [1]. The droplet of blood obtained is then placed on a disposable strip which consists of a sensing element. A glucometer is then used to calculate the blood glucose levels form these strips. Though this process is highly accurate, it is also painful and inconvenient especially when multiple readings are required to be taken in a day. Thus there is an essential need for a non-invasive technique for monitoring BGL. Investigations show that urine, sweat, saliva, tears and breath contain traces of glucose in them and these traces vary with the levels of glucose in the blood. Therefore these human serums have recently gained recognition as feasible alternatives to using blood for glucose measurement. Extensive research conducted in this area conclude that human breath is a good alternative to monitor and diagnose glucose levels as acetone in the breath has shown a good correlation to BGL. Using breath as a deduction technique allows deduction of blood glucose levels by just exhaling into the monitoring device. It is seen that in the human breath there are number of chemical compounds that relate to different diseases [2, 3]. Traces of acetone in the breath are used for the detection of diabetes. According to the studies it is seen that patients who have diabetes have body cells that are unable to absorb the glucose in blood. In such cases, when the liver breaks down fat for energy, there occurs an abnormal increase in ketone bodies in the patient‘s blood. Acetone is one of the three kinds of ketone bodies which are volatile, and the body exhales the acetone thus formed. Therefore higher concentration of acetone is found in the exhaled air of a diabetic patient [4]. Initially complicated techniques such as gas chromatography mass spectroscopy, selected ion flow tube mass spectroscopy and cavity ringdown spectroscopy were used to determine the concentrations of acetone in breath. Gas chromatography-mass spectroscopy [5] works on the principal that the difference in the chemical properties between the different molecules in the gaseous mixture and their relative affinity for the stationary phase of the column promotes the separation of the molecules. In the Selected ion flow tube-mass spectroscopy method it was seen that when the neutral analyte molecules of a sample vapor meets the precursor ions they may undergo chemical ionization which depends on their chemical properties, such as their proton affinity or ionization energy [6]. Cavity Ringdown Spectroscopy [7] is an optical spectroscopic technique that measures the absolute extinction by samples that absorb or scatter light. These techniques remain unsuitable for clinical application due to their low portability, complex mechanisms and high cost. The electronic nose or e-nose model [8, 9] overcomes these drawbacks significantly and is emerging as a good alternative suited to clinical applications. Research conducted with e-nose provides substantial data on acetone concentrations in breath [10]. This paper classifies acetone concentration and uses support vector mechanism (SVM) classifier to analyze the data signals. Different acetone concentration levels are classified healthy breath, type 1 diabetic and type 2 diabetic which is then displayed as the output. Initially the acetone levels were classified using SVM classifier but the accuracy levels remained inadequate. To overcome this issue and increase the level of accuracy SVM classification with margin sampling has been adopted.
2 Breath Analysis Procedure
2.1 Proposed Analysis
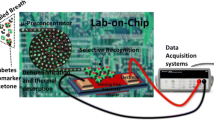
The proposed analysis system here distinguishes the concentration of acetone levels in the breath as healthy or diabetic. The basic model of the proposed system is described by the following flow chart given in Fig. 1.
The operation of the system happens in five stages. Initially the subject‘s breath samples are used for the acetone concentration prediction. The acetone concentration data from various samples are taken individually as input in the next stage. The SVM classification model then classifies the acetone concentration levels based on the thresholds described in the next section. In the final stage the output is displayed under any one of the three classifiers considered for this system. Thus the diabetic and the healthy breath samples are separated in this analysis model.
2.2 Acetone Level Concentration
Human breath consists of many biomarkers which are used for the detection of many diseases. It is explained previously how acetone in the breath is used as the biomarker for the prediction of diabetes. Wang et al. [11] carried out extensive studies and found a linear correlation between the mean concentration of breath acetone and the mean blood glucose levels of each group. It was also observed that the breath acetone declined linearly with blood glucose levels [12]. According to [12, 13], it is seen that the concentration of acetone levels in the breath vary for a healthy and a diabetic subject. It is seen that in all healthy samples acetone levels are less than 0.76 ppmv and in all samples with diabetes acetone levels showed levels higher than 1.71 ppmv. The Table 1 shows the variation of the concentration of acetone levels. For this analysis ten different concentrations of acetone levels are considered and are used for the classification of the data. The acetone concentrations in the breath of 10 subjects are taken in this paper. These data samples are further given to the classifier. The acetone concentration that are detected from the breath for this analysis are in the range of parts per million.
2.3 Classification
In this paper, a support vector machine (SVM) classifier is used to classify the data samples into three classes. SVM [14] is a supervised learning model that is used to analyze a given data set and help recognize patterns that is used for the classification of the samples. These models construct hyper planes that are used for the classification and the regression of the data [15]. Here the SVM divides the acetone concentration data which is the input into three different classes. Based on the above mentioned range of acetone concentrations the SVM classifier is used to distinguish them. The acetone levels are classified into their labels which are H for healthy breath, T1 for type 1 diabetes and T2 for type 2 diabetes. From the threshold range mentioned in the previous section it can be seen that there is an order in the levels of acetone concentrations which do not overlap each other and they conform to the guideline of T1 > T2 > H. Here 10 various acetone concentrations are considered for the classification. The input sample vector is taken as these concentrations and the trained samples are the classified data. A set of hyper planes are used here so as to classify the ten samples into the three different classes. The classifier chooses the hyper planes such that the nearest trained data point has the largest distance so that a good segregation of the data points are achieved. The Fig. 2 shows the graphical representation of the acetone concentrations of the subjects considered for this analysis. The bar graph that is plotted clearly shows the variation of the acetone levels of a healthy breath and a diabetic patient. Hence the above thresholds can easily segregate the samples as healthy, type 1 or type 2 diabetes. The scatter plot that distinguishes the acetone levels are represented in the Fig. 3. This figure gives the details of the classification of the acetone levels for a diabetic type 1 and type 2 as well as marks the healthy samples of the ten acetone concentrations which are considered in this paper. It is seen that for the type 2 and type 1 diabetic subjects the levels of acetone in their breath is high compared to the normal breath acetone levels.
3 Result and Discussion
The classified acetone concentrations of the ten subjects are done using the SVM classifier and the classified acetone level output is tabulated and presented in Table 2 shown below. It is seen that based on the threshold parameters described in the previous section the classification and the labeling of the data has been performed. It is clearly seen that the acetone concentrations in the breath of a diabetic patient (Type 1 and Type 2) is greater than the normal breath standards. When the ten trained samples were classified, it was found that a higher level of accuracy can be obtained using an SVM classifier with margin sampling. This approach has given the data a clear margin over which they can be segregated. The ten concentrations were labeled into the three categories namely Healthy, Type 1 diabetic and Type 2 diabetic and the samples are placed according to the values in any one of these above mentioned categories.
4 Conclusion and Future Work
This paper investigates the concentration of acetone levels for classification of breath samples in monitoring diabetes. Acetone concentrations were collected and classified for predicting diabetes. The samples were classified using the SVM classifier and were divided into three groups labeled as healthy, type 1 and type 2 diabetes. In this paper an attempt has been made to refine the existing classification approach (healthy and diabetic) further for a more accurate evaluation (healthy, type 1 and type 2 diabetic). The future work will include designing and developing the sensory array for examination of acetone concentrations in real time breath samples.
References
Prashanth Makaram, Dawn Owens and Juan Aceros, “Trends in Nanomaterial-Based Non-Invasive Diabetes Sensing Technologies”; Diagnostics 2014.
Wolfram Miekisch, Jochen K Schubert, Gabriele F.E Noeldge—Schomburg;—Diagnostic potential of breath analysis—Focus on volatile organic compounds‖; Clinica Chimica Acta 2004.
Kim DG Van de Kant, Linda J.T.M van der Sande, Quirijn Jöbsis, Onno C.P van Schayck, Edward Dompeling;—Clinical use of exhaled volatile organic compounds in pulmonary diseases: a systematic review.‖ Respiratory Research 2012.
Tassopoulos, C.N.; Barnett, D.; Fraser, T.R;—Breath-acetone and blood-sugar measurements in diabetes‖: Lancet 1969.
Chunhui Deng, Jie Zhang, Xiaofeng Yu, Wei Zhang and Xiangmin Zhang; —Determination of acetone in human breath by gas chromatography–mass spectrometry and solid-phase microextraction with on-fiber derivatization‖; Journal of Chromatography 2004.
Moorhead, D. Lee, J. G. Chase, A. Moot, K. Ledingham, J. Scotter, R. Allardyce, S. Senthilmohan, and Z. Endre;—Classification Algorithms for SIFT-MS medical diagnosis‖; Proceedings of the 29th Annual International Conference of the IEEE EMBS Cité Internationale, Lyon, France August 23–26, 2007.
Chuji Wang, Armstrong Mbi and Mark Shepherd;—A Study on Breath Acetone in Diabetic Patients Using a Cavity Ringdown Breath Analyzer: Exploring Correlations of Breath Acetone With Blood Glucose and Glycohemoglobin A1C‖; IEEE Sensors Journal, Vol. 10, NO. 1, January 2010.
P. Wang, Y. Tan, H. Xie, and F. Shen;—A novel method for diabetes diagnosis based on electronic nose‖; Biosensors and Bioelectronics, Vol. 12, No. 9, pp. 1031–1036, 1997.
D. Guo, D. Zhang, N. Li, L. Zhang, and J. Yang;—A novel breath analysis system based on electronic olfaction‖; IEEE Transaction on Biomedical Engineering, Vol. 57, No. 11, November 2010.
P. Wang, Y. Tan, H. Xie, and F. Shen; “A novel method for diabetes diagnosis based on electronic nose‖; Biosensors and Bioelectronics”, Vol. 12, No. 9, pp. 1031–1036, 1997.
C. Wang, A. Mbi, and M. Shepherd, “A study on breath acetone in diabetic patients using a cavity ringdown breath analyzer: Exploring correlations of breath acetone with blood glucose and glycohemoglobin a1c”, IEEE Sens. J., vol. 10, no. 1, pp. 54–63, Jan. 2010.
C. Turner, C. Walton, S. Hoashi, and M. Evans, ‘Breath acetone concentration decreases with blood glucose concentration in type I diabetes mellitus patients during hypoglycaemic clamps’, ‖ J. Breath Res., vol. 3, no. 4, p. 046004, Dec. 2009.
C. Deng, J. Zhang, X. Yu, W. Zhang, and X. Zhang, ‘Determination of acetone in human breath by gas chromatography-mass spectrometry and solid-phase microextraction with on-fiber derivatization,’ J. Chromatogr. B, vol. 810, no. 2, pp. 269–275, 2004.
C.-C. Chang and C.-J. Lin,–LIBSVM: A library for support vector machines,’ ACM Trans. Intell. Syst. Technol.’, vol. 2, no. 3, 27, pp. 1–27, 2011.
C. J. Burges,—A tutorial on support vector machines for pattern recognition,’ Data Mining Knowl. Discovery’, vol. 2, no. 2, pp. 121–167, 1998.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media Singapore
About this paper
Cite this paper
Mohapatra, S.K., Mahapatra, S.K., Tripathy, S.K., Kanoje, L. (2017). Concentration of Acetone Levels in Breath for Monitoring Blood Glucose Level. In: Mandal, J., Satapathy, S., Sanyal, M., Bhateja, V. (eds) Proceedings of the First International Conference on Intelligent Computing and Communication. Advances in Intelligent Systems and Computing, vol 458. Springer, Singapore. https://doi.org/10.1007/978-981-10-2035-3_3
Download citation
DOI: https://doi.org/10.1007/978-981-10-2035-3_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2034-6
Online ISBN: 978-981-10-2035-3
eBook Packages: EngineeringEngineering (R0)