Abstract
Nuclear medicine allows imaging of (patho) physiological processes within the body and contributes in the diagnosis and treatment of specific diseases. In patients with bone metastases, nuclear medicine not only plays an important role in the diagnosis, but may also be used for therapeutic purposes. For several decades, bone scintigraphy has been used and nowadays is still the nuclear medicine imaging method of choice for diagnosing bone metastases in many malignant diseases. Its sensitivity (>90 %) is still superior to any other available imaging method. However, the specificity is rather low and interpretation of scans needs to be carefully evaluated by expert nuclear medicine physicians together with other biological, anatomical and clinical information.
In the last two decades, nuclear medicine rapidly evolved. New radiopharmaceuticals (SPECT and PET) were produced, specific for a certain cancer type. Recent development in soft- and hard-ware led to the introduction of hybrid camera systems (SPECT-CT and PET-CT), combining (patho)physiology and anatomy together, leading to better diagnostic results and many advantages, also for the patient.
In this chapter the basic principles of nuclear medicine, the different camera systems, and the technique and procedure of the bone scintigraphy will be explained. An overview is given of the available radiopharmaceuticals (SPECT and PET) to detect bone metastases in different cancer types. The role of nuclear medicine in patients with prostate cancer, breast cancer, lung cancer, and some other cancer types will be discussed more extensively.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In the study of bone metastases, nuclear medicine not only plays an important role in diagnosis, but also in therapy. This chapter focuses on the role of nuclear medicine in diagnosing bone metastases.
Bone imaging was one of the first applications of nuclear medicine in humans and still is one of the hallmarks of this discipline. The sensitivity of this nuclear medicine technique in diagnosing bone metastases is remarkably high, exceeding 90 %. On the other hand, the specificity is rather low, although the specificity rates have improved since the introduction of hybrid cameras that make it possible to combine (patho) physiological and anatomical information together. Interpretation of scans needs to be carefully evaluated by expert physicians in combination with other biological and clinical information or by other imaging modalities.
In this chapter we will explain the basics of nuclear medicine and the working mechanisms of the different imaging techniques. We will then give an overview of the available radiopharmaceuticals that are used for diagnosing bone metastases, followed by some special imaging characteristics in the most common malignancies that metastasize to the bone.
2 Basics of Nuclear Medicine
2.1 Radiopharmaceuticals and Isotopes
In the field of nuclear medicine, radiopharmaceuticals are used to image (patho) physiological processes in the body. A radiopharmaceutical is a synthesized compound consisting of a radioactive isotope and a pharmaceutical. Isotopes are nuclides with the same number of protons in their nucleus and are therefore nuclides of the same element. Most nuclei that are present in nature are stable. However, some are not stable and want to transform themselves to form stable configurations. These nuclides are called radionuclides or radioactive isotopes. Transformation to their stable state is achieved by emission of either particles or energy from the nuclei. Radionuclides may emit gamma-rays (which can be imaged on a gamma camera), beta-rays (which are used for therapy purposes), or both. Some radionuclides are positron emitters (positively charged electrons) and may be used for positron emission tomography (PET) imaging. The transformation process, occurring spontaneous and at random, is also called radioactive decay. The rate at which the atoms decay is measured in disintegrations per second, also called Becquerel (Bq), the radiation unit. One disintegration per second is equal to 1 Bq. Each radionuclide has its uniquely defined decay constant, also called the physical half-life. This is the time required for half of the amount of radionuclide to decay. This half-life is important in imaging purposes, since it determines the time intervals between which imaging has to take place.
The biodistribution and targeting characteristics of the radiopharmaceutical is determined by the drug to which the radionuclide is attached. The presence of the radionuclide may not alter these drug characteristics. The drug part of the radiopharmaceutical can be almost every target that is characteristic of a disease or a target that is present on a particular cell (drug, antibody, enzyme, receptor, etc.). For example, in bone scan imaging, the ligand hydroxymethylene-diphosphonate (HDP) is the drug part that is preferentially taken up by osteoblasts. Consequently, by chemically attaching HDP to the radionuclide 99mTechnetium (99mTc), the radiopharmaceutical is transported to the bone for imaging purposes.
Radiopharmaceuticals are usually administered intravenously. Therefore, the patient is the source of the radioactivity, in contrast with radiology where the imaging devices emit X-rays or gamma-rays through the patient. The detection of gamma-rays (photons) emitted from the patient and transforming it into an image is the main principle of the camera systems used in nuclear medicine (the gamma-camera and the PET-camera).
2.2 Gamma-Camera
A decaying radionuclide emits photons in all directions. Different radionuclides produce different characteristic photons of a specific energy. 99mTc for instance predominantly emits photons with an energy of 140 keV, whereas radioactive iodine (131I) emits predominantly 364 keV energy photons. A gamma-camera consists of one, two, or three heads with a detector that registers the impact of these photons. Each detector consists of a collimator, a scintillation crystal, a light guide, photomultiplier tubes, and a positioning and energy discrimination system.
A collimator is made of parallel strips of lead with multiple holes. The holes guide the individual photons towards the scintillation crystal. Photons that do not travel in the right direction are absorbed in the septa between the holes. Different types of collimators are available, depending on the energy level of the emitted photons. In the scintillation crystal the photons are absorbed and converted into a small flash of light. Brighter flash of light means a higher energy of the photon. This light reaches the photomultiplier tubes (PMTs), where it interacts with photocathodes and transforms into a photoelectron. This signal is amplified by electrodes or dynodes at increasing voltages, and eventually all the signals are combined in a position system, which gives each signal from the individual PMTs different weights to derive the position information of the photons in x- and y-direction. Only photons falling within a determined photopeak region are accepted. This described technique forms the basis of conventional planar nuclear medicine images.
2.3 SPECT(-CT)
The image contrast of conventional planar imaging is rather low due to overlying structures that may interfere with the region of interest. This limitation can be overcome by acquiring images from different angles (64–128°) in a circular manner around a patients and subsequently reconstruct a 3D-image. This technique is called Single Photon Emission Computed Tomography (SPECT). These collected imaged can be reconstructed into different slices and visualized in transverse, sagittal and coronal views. The resolution of this technique is around 8 mm.
Development in soft- and hardware led to the implementation of hybrid systems, combining SPECT with multi-detector computed tomography (CT). An example of a SPECT-CT camera is shown in Fig. 5.1. SPECT and CT are performed in an immediate sequential setting, without changing the position of patients. This allows us to correlate the (patho) physiological information with anatomical information, leading to better specificity rates and better diagnostic accuracy. Acquiring SPECT images takes approximately 20 min per part of the body (head and neck, thorax, abdomen etc.)
2.4 PET (-CT)
Positron Emission Tomography (PET) is another imaging tool to visualize various processes in the body. For this technique, radionuclides are used that emit a positively charged particle (a positron) to become stable. At the end of its kinetic energy (or at the end of its range, maximum 2,8 mm) the positron reacts with an electron. The masses of the positron and electron are transformed into energy (E = mc2) forming two photons that are emitted with the same energy (511 keV) in exactly opposite directions. This process is called annihilation. This phenomenon is registered by a PET camera by using a ring detector around a patients, thereby registering the photons by opposite detectors and within a certain time window, to consider these two as one pair from the same annihilation process. New developments in software lead to a correction method for the time a photon needs to travel from its origin to the detector. This correction, called Time-of-Flight (TOF) has advantages for spatial resolution. The resolution of this technique is approximately 4 mm.
Nowadays, PET cameras are always combined with CT (PET-CT, see Fig. 5.2) with the same advantages as SPECT-CT. Moreover, costs are reduced (one imaging modality) and the one-stop-shop principle (one scan on one department instead of two scans on two departments) reduces waiting time for the patient. In contrast to SPECT-CT, where only a part of the body can be imaged, a patient can be imaged completely by moving in the PET-CT camera. A PET-CT scan of the body (head to mid-thigh) is nowadays performed in approximately 20 min.
2.5 Radiation Issues
The use of radioactive materials means that not only the tumor endures radiation, but also healthy organs and tissues. Furthermore, persons nearby should be protected from the radiation exposure. To put this in perspective: the annual radiation burden from background radiation by natural radiation sources in general is around 2–2.5 mSv. The radiation burden of a bone scan (including SPECT) using a radiopharmaceutical with an administered activity of 500 MBq is 2.3 mSv. For 18F-fluorodeoxyglucose (18F-FDG), the most often used PET radiopharmaceutical, the radiation burden is around 7.6 mSv (using 400 MBq). The radiation dose of a low dose CT is approximately 1.5 mSv. However, in contrast to the natural background radiation that is continuously present in our environment, the activity rate from diagnostically injected amount of a radiopharmaceutical decreases exponentially over time. The radiation burden for people nearby is calculated at a distance of 1 m and overall exposure is marginal compared to the natural background radiation. Another consideration when referring to the radiation exposure is the age of a person. The added risk decreases with increasing age. Consequently, young children are most susceptible to damage due to radiation exposure.
3 Bone Metastases from the Nuclear Medicine Point of View
Several diagnostic modalities are available for the detection of metastatic bone lesions. These include plain X-rays, CT scan and Magnetic Resonance Imaging (MRI). All these techniques, described elsewhere, are based on the anatomical characteristics of bone metastases and do not provide any information concerning the (patho) physiology or metabolic activity of evaluated lesions. Therefore, nuclear imaging modalities are valuable, not only in diagnosing bone metastases, but also in the differential diagnosis between metastases and other bone lesions or pathology. By applying specific radiopharmaceuticals, specific for a specific type of tumor, different biophysical and biochemical characteristics of bone metastases are depicted, helping physicians to establish an accurate diagnosis. In the following subchapters, the characteristics of different SPECT and PET radiopharmaceuticals are described and their role in detecting bone metastases is discussed.
4 Bone Scintigraphy
Bone scintigraphy is widely available and is a well established modality within nuclear medicine. It is one of the oldest techniques within nuclear medicine imaging with a clinical experience of almost 50 years. It still remains the cornerstone of modern nuclear medicine imaging in the evaluation of bone metastases. Its sensitivity is high (>90 %); however, its specificity is rather limited.
4.1 99mTc-Diphosphonates
The most commonly used radiopharmaceutical for the detection of bone metastases is 99mTc labelled with diphosphonates. Different forms exist, such as 99mTc-hydroxymethylenediphosphonate (99mTc-HDP), 99mTc-methyldiphosphonate (99mTc-MDP), and 99mTc-dicarboxypropane diphosphonate (99mTc-DPD) with slightly different kinetic qualities, all three being incorporated in the bone (hydroxyapatite deposition) by the activity of osteoblasts. The differences between these three diphosphonates are marginal, and all three can be used for bone scintigraphy, each of them showing high lesion-to-normal bone ratio. The factors that control accumulation of phosphonates in bone are the blood flow and the extraction efficiency, which in turn depends on capillary permeability, acid–base balance, parathyroid hormone levels, etc. Overall, about 50 % of the injected radiopharmaceutical accumulates in the skeletal system. The maximum bone accumulation takes place 1 h after injection and remains practically constant for up to 72 h.
4.2 Imaging Techniques and the Three Phases
Bone scintigraphy images the distribution in the skeletal system and can be performed in several ways:
-
Limited bone scintigraphy or spot views (planar images of a preselected part of the body)
-
Whole body bone scintigraphy (planar images of the entire skeleton in both anterior and posterior view)
-
Single Photon Emission Computed Tomography (SPECT) combined with CT of a preselected part of the body
-
Three phase bone scintigraphy (flow, bloodpool, and late planar images)
In oncology, the standard recommended technique is whole body scintigraphy, complemented by SPECT (CT) imaging if necessary. However, for best accuracy in single lesions and best differential diagnosis between benign and malignant lesions, a three phase bone scintigraphy may be the best choice. The first phase (or flow phase) is sort of an angiogram, performed dynamically for 2 min directly after administration, over the part of interest. In this phase, the radiopharmaceutical is delivered to the surface of the bone. Increased bone uptake is seen in areas with high blood flow. The second phase (also called blood pool phase) is a soft tissue phase, performed directly after the first phase (2–5 min after injection). The third phase (or static/planar phase) represents the situation in which the radiopharmaceutical has been absorbed into the hydroxyapatite matrix of the bone and is usually performed 3 h after administration. A three phase bone scintigraphy characterizes the vascularization of a process as well as its metabolic activity and may help distinguishing bone metastases from infectious processes, recent fractures and primary bone neoplasms.
4.3 Role of Bone Scan in Diagnosing Bone Metastases
The sensitivity of bone scintigraphy is determined by the level of osteoblastic activity. This means that in case of osteoblastic metastases a bone scan will reveal highly intense uptake in the metastases. In case of osteolytic metastases, normal bone tissue surrounding metastatic lesions will normally respond with compensatory osteoblastic activity, which will also lead to highly intense uptake of the radiopharmaceutical. Only in case of slowly growing osteolytic metastases there can be absence of an osteoblastic reaction that would render the metastases undetectable through bone scanning. The incidence of lytic, blastic, and mixed type of bone metastases is different in various tumor types. Bone metastases of bladder, kidney, and thyroid cancer and lesions of multiple myeloma are invariably lytic. Cold spots on the bone scan, i.e. focal absence of activity, is typically observed in patients with multiple myeloma with large osteolytic lesions. Blastic lesions are frequently seen in prostate and breast cancer, and occasionally in lung, stomach, pancreas, and cervix carcinomas [1].
The radiopharmaceutical is excreted by the kidneys and the bladder and these organs are normally visualized on a bone scan. However, in some cases there is extremely high uptake in the bones and absence of activity in kidneys and bladder. This is called a superscan, suggestive for metastatic disease in the entire skeleton. Three examples of a bone scan, made to visualize or exclude bone metastases, are shown in Fig. 5.3.
The major limitation of the interpretation of bone scans is the low specificity. It may be difficult to distinguish bone metastases from degenerative changes, inflammatory processes, traumata, mechanical stress, Paget’s disease, fibrous dysplasia or benign or malignant primary bone tumours [2].
A recent meta-analysis of the role of bone scintigraphy in the diagnosis of bone metastases from various malignancies showed a pooled sensitivity of 86 % and a specificity of 81 % [3]. A meta-analysis only in breast cancer showed a pooled sensitivity of 87 % and a specificity of 88 % [4]; in lung cancer a pooled sensitivity of 86 % and specificity of 88 % was reported [5]. Even-Sapir et al. reported that for the detection of bone metastases in patients with high-risk prostate cancer bone scintigraphy had a low sensitivity of 70 %, a specificity of 57 % and a positive and negative predictive value of 64 % and 55 % respectively. However, by using SPECT, the sensitivity was improved to 92 %, the specificity to 82 %, and the positive and negative predictive values reached 86 % and 90 % respectively [6]. Combining SPECT with CT may offer even better results.
5 Other SPECT Radiopharmaceuticals
The following SPECT radiopharmaceuticals are unspecific for bone metastases. They are specific for certain tumor types, depicting also bone disease if present. Because of their non-specificity to bone, it may be difficult to localize exactly the location or to distinguish metastatic bone lesions from localization in surrounding soft tissues. Therefore, SPECT-CT should be performed in these cases.
5.1 123Iodine and 131Iodine
123Iodine (123I) and 131Iodine (131I) accumulate in the thyroid where it is built into thyroid hormone and stored for later secretion. Because of this characteristic it can be used to identify well-differentiated (papillary and follicular) thyroid tumours and their metastases. 123I is a gamma-emitter with a half life of 13 h and can be used for diagnostic reasons before treatment with high dose 131I. The latter emits beta-rays for therapeutic purposes and gamma-rays which makes imaging possible. The half-life of 131I is 8 days. Theoretically a high treatment dose provides a better sensitivity as compared to the low diagnostic dose of 123I, but several researchers found no differences between the diagnostic accuracy of 123I pre-treatment scanning with low dose and 131I post-treatment scanning with high dose [7, 8].
For the initial diagnostic work-up for nodule investigation or thyroid cancer, 123I or 131I scanning has no role anymore, since ultrasound and fine needle aspiration (FNA) biopsy are standard diagnostic procedures. Similarly, the follow-up of recurrent disease is done by following thyroglobulin levels instead of 123/131I scanning. However, in some cases diagnostic scanning with 123/131I is worthful, especially when searching for metastases. Both isotopes may also be used before ablation therapy, to reveal the amount of thyroid remnant after surgery or to see if there are metastases. Furthermore, after treatment with 131I because of differentiated thyroid cancer, a post-treatment scan (7–10 days after therapy) is always performed (Fig. 5.4).
Even though these radiopharmaceuticals are highly specific for thyroid tumours, scintigraphy is associated with a poor signal-to-noise ratio. Upon the physiological accumulation in the salivary glands, liver, spleen, intestines, kidneys and bladder, little to no accumulation is seen in structural tissues which makes if often difficult to identify the exact localization of (bone) metastases. SPECT-CT should therefore be performed to exactly localize metastatic (bone) disease in patients with thyroid tumours.
5.2 123I- and 131I-MIBG
Metaiodobenzylguanidine (MIBG) is a noradrenalin analogue which accumulates in neurosecretory granules of adrenergic tissue. This makes it suitable for imaging neuroendocrine tumours, such as phaeochromocytomas, carcinoid, and paragangliomas. In children, it may also be used for the diagnosis and staging of neuroblastoma. 123I-MIBG is only used for diagnostic purposes, whereas 131I-MIBG (since 131I is a beta- and gamma-emitter) may be used for both diagnosis and therapy. The advantage of 123/131MIBG is its high specificity for tissue characterization and reported sensitivities and specificities are high. In detecting phaeochromocytomas and neuroblastoma, the diagnostic accuracy of MIBG scintigraphy is superior to other imaging modalities [9]. For the detection of other neuroendocrine tumours, sensitivity is lower, and other imaging modalities may be preferred. The specificity for neuroblastoma is mentioned to be 84 %. However, since other neuroendocrine tumours in childhood are rare, a positive MIBG scan is nearly diagnostic for a neuroblastoma [10].
As described earlier, the imaging characteristics of 123/131I are poor, not showing accumulation in structural tissues, rendering the exact localization of metastases difficult. Fusion of the MIBG scintigraphy (SPECT) with a morphological imaging modality (CT) improved the diagnostic value [11] with the main advantage being the identification of normal distribution of the radiolabelled MIBG in organs such as intestines and renal system, leading to a reduction of false positive results. Also, better differentiation of bone metastases from a local recurrence of a phaeochromocytoma, was possible.
The use of MIBG scintigraphy purely to diagnose bone metastasis is still doubtful. The paper by Zuetenhorst et al. directly compared MIBG scintigraphy with the bone scan in carcinoid tumours with bone metastases. The bone scan outperformed MIBG scintigraphy, showing multiple bone lesions in all patients, whereas MIBG scintigraphy only identified lesions in 22 % [12].
5.3 Radiolabelled Somatostatin Analogues
Neuroendocrine tumours frequently express a high density of somatostatin receptors, which is exploited by nuclear medicine imaging techniques using somatostatin analogues. These analogues have been developed since somatostatin itself has a short plasma half life (approximately 3 min). For most somatostatin analogues, internalization of the 111In-octreotide complex with residualization of the 111In label (gamma-emitter, half-life 2.8 days) is the most likely mechanism accounting for the good scintigraphic tumor-to-background ratio observed 24 h after injection [13]. Based on the high receptor expression, somatostatin receptor scintigraphy (SRS) provides important information on tumour localization and metastases of many neuroendocrine tumours. Best results are published in paragangliomas and neuroendocrine gastrointestinal tumours (87 % and 88 % sensitivity) [9]. Of course, functional mapping by using SPECT/CT was reported as leading to higher diagnostic accuracy [14]. However, SRS failed to detect a large proportion (50 %) of metastatic bone lesions that were detected by bone scintigraphy [12]. More recently other radiolabelled somatostatin analogues have been successfully used, such as 99mTc-EDDA-HYNIC-TOC and 99mTc-Depreotide.
6 PET Radiopharmaceuticals
PET has two major advantages in comparison to SPECT. First of all, the better spatial resolution (4 mm compared to 8 mm), allows the investigators to see smaller structures. Secondly, PET offers the possibility of absolute quantification, leading to an improved sensitivity of the follow-up of metastatic lesions. PET imaging allows us to diagnose and monitor not only the number and size of pathological lesions, but also the amount of uptake per lesion. This uptake intensity is calculated by using the Standardized Uptake Value (SUV). It represents the tissue activity within a region of interest corrected for the injected activity and for patient’s weight or lean body mass [15]. This quality makes PET imaging useful to monitor response to therapy and/or disease progression [2].
6.1 18F-Fluoride
18F-fluoride is a positron emitter specific for bones since it images any form of calcification. The radiopharmaceutical itself was already used in the 1950s for bone scintigraphy, using an old general-purpose rectilinear scanner for imaging purposes. It was abandoned due to the fast introduction of 99mTc, the development of diphosphonates, and the introduction of the gamma-camera. The “normal” bone scan (labelled diphosphonates) became the gold standard in nuclear bone imaging. Since the introduction of high resolution PET cameras in the early 1990s, 18F-fluoride is reintroduced into nuclear medicine imaging.
Fluoride ions enter the extracellular fluid of bone by diffusion through capillaries, leading to a slow exchange with hydroxyapatite crystals and the formation of fluoroapatite [2]. The faster blood clearance of 18F-fluoride and the twofold higher uptake in developing bone cells of fluoride, makes it possible to image earlier (1 h after injection), and leads to better ratios between uptake in bone with faster turn-over and normal bone [16].
The characteristics of 18F-fluoride are in general identical to the diphosphonate complexes. Both radiopharmaceuticals are normally symmetrically distributed throughout the entire skeleton. 18F-fluoride deposition favours the axial (spine and pelvis) over the appendicular (shoulder girdles and limbs) skeleton and is greater for joints than for shafts of long bones [17]. The route of excretion is through the urinary tract. In accordance with the 99mTc-diphosphonate bone scan, the degree of uptake does not differentiate benign from malign. However, the pattern may be suggestive for a specific diagnosis. Still, physiological uptake may be more variable in 18F-fluoride due to higher resolution of the PET/CT camera.
Limitations of this technique are the high costs (five times higher compared to the bone scan with diphosphonates) and the non-possibility to perform flow and blood pool imaging. A study performed by Even-Sapir et al., reported a sensitivity for bone metastases of 100 %, a specificity of 62 %, a positive predictive value of 74 %, and a negative predictive value of 100 %. By applying CT to the PET scan all afore mentioned parameters were improved to 100 % [6].
At the moment, the classical bone scan with diphosphonates is the gold standard for the detection of bone metastases. However, 18F-fluoride PET is at least as sensitive and specific and should be considered for the individual patient although most bone metastases can also be detected with 18F-FDG.
6.2 18F-FDG
The glucose analogue 18F-fluorodeoxyglucose (18F-FDG) is used extensively in various malignant and infectious diseases, and is also a useful radiopharmaceutical for bone imaging. Processes with high glucose turnover show a high uptake of FDG, because of its intracellular accumulation. FDG enters the cell by using several glucose transporters (mainly GLUT-1 and GLUT-3) that are located on cellular membranes. After phosphorylation of normal glucose by hexokinase, glucose-6 phosphate is formed and further metabolized by glycolysis. On the contrary, FDG is phosphorylated to FDG-6-phosphate, which cannot be glycosylated and is therefore retained in the cell. Malignant cells have an increased glucose turn-over, which is related to a higher density of GLUT-1 and GLUT-3 transporters on the cell membrane and to a higher concentration of hexokinase. This leads to a favourable signal-to-noise ratio which has made 18F-FDG an extensively used radiopharmaceuticals for all kind of malignancies.
The high glucose metabolism is related to growth, which makes 18F-FDG especially useful for aggressive, fast growing, less differentiated tumours and their (bone) metastases, such as lung cancer, melanoma, lymphoma, breast cancer, sarcomas etc. Less FDG-avid tumours are the slow growing, well-differentiated tumour types, such as prostate carcinoma, neuroendocrine tumours, and well-differentiated thyroid cancer. However, every form of these well-differentiated tumours may turn into FDG-avid tumours once they dedifferentiate.
Before undergoing a 18F-FDG PET scan, patients have to fast 4–6 h before the administration of the radiopharmaceutical. This fasting period stimulates the uptake of FDG into the organs of interest. In a 18F-FDG scan made directly after eating, all the FDG accumulates in the muscles, thereby hindering correct image interpretation. The blood glucose level should be <10 mmol/L to increase sensitivity. Physiological uptake is seen in the brain and in the left ventricle of the heart, and sometimes in the intestines. Excretion is by the urinary tract. To avoid uptake in muscles, patients have to lay quiet and are not allowed to talk during the waiting time, which is 1 h after injection.
As with bone scans, specificity is the limiting factor of 18F-FDG, since a variety of processes may show a high glucose metabolism. In the bone, such processes may include infections, loosening of prosthesis, benign bone tumours etc. The advantage of 18F-FDG PET over bone scintigraphy is that is also provides information on soft-tissue metastases (combined with CT). Secondly, by calculating SUV, better differentiation is possible between malignant and benign diseases. An example of an 18F-FDG PET/CT is shown in Fig. 5.5.
6.3 18F-FLT
The nucleoside analogue 3-deoxy-3-[18F]fluorothymidine (18F-FLT) is used to image tumour cell proliferation. The uptake of FLT relies on the thymidine kinase 1 (TK1) enzymatic activity and thus on DNA synthesis. 18F-FLT PET is mainly used to diagnose bone marrow diseases [18]. For imaging bone metastases, FLT is outperformed by 18F-FDG [19].
6.4 11C-Choline
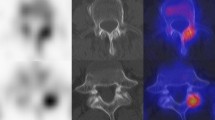
Since FDG is not taken up in huge amounts in slow growing well-differentiated tumours, it is not the radiopharmaceutical of choice in diagnosing and staging prostate cancer. Instead of 18F-FDG, 11C-Choline is used in the imaging of nodal metastases from prostate cancer as well as in the imaging of metastatic bone disease (Fig. 5.6). It was found that in malignancies there is a high intracellular trapping of phosphatidylcholine (PC) together with an up regulation of choline kinase, an enzyme that is responsible for the synthesis of PC. Consequently, by labelling choline with 11C, it enables imaging of PC trapped in malignant cells.
Another reason for the superiority of 11C-Choline over 18F-FDG in imaging prostate cancer is the low urinary clearance and therefore its low concentration in the bladder. The use of 18F-FDG is associated with higher urinary clearance and a high bladder activity that obscures the imaging of the prostate. However, imaging with 11C-Choline has also limitations. Benign prostatic hypertrophy also gives a high choline activity. Discrimination between benign and malignant lesions is not possible, also not by using SUV calculations. For patients with biochemical recurrence after initial treatment of the primary tumour, 11C-Choline is an accurate technique, identifying more abnormalities suspect for recurrent disease or metastases than 18F-FDG [20].
Currently, Choline is also labelled with 18F and used for imaging purposes. Results in sensitivity and specificity are similar. However, 18F is excreted by the urinary tract, so bladder emptying or placement of a catheter is necessary to visualize the prostate region.
In summary, 11C-Choline PET (-CT) is not an appropriate imaging technique for accurate T-staging of prostate cancer prior to radiotherapy. However, it holds great potential as a single step diagnostic procedure of lymph nodes and skeleton, which could also facilitate radiotherapy treatment planning [21].
6.5 11C-Methionine
Cellular proliferation is associated with protein synthesis. Since amino acids are the natural building blocks of proteins, avid uptake of these precursors is a normal feature of rapidly proliferating cells. Amino acid transport and protein synthesis are increased in most types of tumours compared to normal healthy tissue. The most frequently used radiolabelled amino acid is 1-[methyl-11C]-methionine (11C-Methionine), primarily reflecting the trans-membrane transport by the sodium-independent L-transporter into cells [22]. 11C-Methionine is mainly used to image brain tumours and metastases; however it also has a place in imaging prostate cancer and metastases. For diagnosing the primary tumour, 11C-Methionine was found equal to 18F-FDG [23]. In a study involving only a small group of patients it was reported that both sensitivity and specificity for imaging metastases was 70 % (both higher than 18F-FDG) [20]. This was also noticed in another study reporting 11C-Methionine was more effective than 18F-FDG for detecting bone metastases (69.8 % of metastatic bone lesions found with 11C-Methionine, vs 48.3 % with 18F-FDG). The authors assumed that the increased sensitivity of 11C-Methionine may be the result of differences in tumour metabolism between patients, or a time-dependent metabolic cascade in metastatic prostate cancer, with initial uptake of 11C-Methionine in dormant sites followed by increased uptake of 18F-FDG during progression of the disease [24].
6.6 18F-DOPA
The metabolic pathways by which neuroendocrine tumours synthesize peptides and the intracellular processes which are essential to sustain production of these peptides are ideal candidates for the development of radiopharmaceuticals specific for neuroendocrine tumours [9]. The most important one, in the catecholamine pathway, is 6-[18F]-L-3,4-di-hydroxyphenylalanine (18F-DOPA). Premedication with the decarboxylase inhibitor carbidopa is used to reduce the urinary extraction, resulting in lower renal and bladder activity and a higher availability of DOPA for neuroendocrine tumour cells. 18F-DOPA PET yields a very high sensitivity in the detection of carcinoid tumours, paragangliomas and phaeochromocytomas (higher than MIBG scintigraphy and SRS). With the application of 18F-DOPA for all metastatic lesions, including bone lesions, sensitivities ranging between 65 % and 100 % and specificities between 75 % and 100 % are reported [25]. In cases of dedifferentiation of the tumour and its metastases the intensity of the lesions by using 18F-DOPA may decrease, whereas the intensity increases when 18F-FDG is used.
6.7 18F-FES
Approximately 75 % of breast tumours express the oestrogen receptor (ER) at diagnosis. Knowledge of the ER status of a patient has important consequences for treatment decision making, since patients with ER-positive tumours are likely to respond to antihormonal therapy. During metastatic disease, evaluation of ER status is also important to determine changes in receptor expression. Discordant ER expression between primary tumour and metastatic lesions occur in 18–55 % of patients. PET scanning with 16α-[18F]-fluoro-17-β-estradiol (18F-FES) provides a unique method to noninvasively obtain molecular information about ER expression (Fig. 5.7). Several studies have shown that 18F-FES-PET can reliably detect ER-positive tumour lesions and correlation with immunohistochemical scoring was well. Low 18F-FES uptake was a strong predictor for failure of antihormonal therapy. 18F-FES-PET may be used in breast cancer to give up-to-date information about the ER expression in known metastases. Furthermore, it may be used as valuable additional diagnostic tool when standard work-up is inconclusive [26].
6.8 18F-FDHT
18F-fluoro-5α-dihydrotestosterone (18F-FDHT) is a labelled analogue of the major ligand for the androgen receptor (AR), dihydrotestosterone. The androgen receptor is over expressed in 90 % of primary prostate tumours and plays a major role in tumor growth. 18F-FDHT could be used in the same diagnostic questions as in 18F-FES, i.e. to see if there are metastases, to solve diagnostic dilemmas and give up-to-date information about the AR expression in known metastases. At this moment, only a few studies with 18F-FDHT PET are available, but this radiopharmaceutical seems very useful in deciphering the role of AR in resistant and progressive metastatic disease and in assessment of treatment [27].
6.9 68Ga Labelled Somatostatin Analogues
68Gallium (68Ga) is a generator-produced radionuclide that can be chelated with DOTA to form a stable complex with somatostatin analogues. Several variants have been tested and compared to other imaging modalities, e.g. [68Ga-DOTA0, Tyr3] octreotide (68Ga-DOTATOC) and [68Ga-DOTA,1-naI3]octreotide (68Ga-DOTANOC), all sharing excellent image quality with better spatial resolution compared with the imaging of SPECT analogues. Some authors state that PET/CT with 68Ga-labelled somatostatin analogues will become the image modality to be used for SRS in the future [28]. These peptides could also be labelled with 177Lutetium (177Lu) or 90Yttrium (90Y) for therapy. A recent paper showed that bone metastases of neuroendocrine tumors have a good prognosis if well diagnosed and treated [29].
7 Nuclear Medicine Characteristics in Prostate Cancer
Prostate cancer cells metastasize mainly through the haematogenous route, and despite dissemination to multiple organs, growth preferentially occurs in the bone and particularly in the red marrow of the axial skeleton. The vertebral column is the most common site for prostate cancer cells to metastasize. Other common sites are the pelvis, ribs, and—to a lesser extent—the skull and extremities.
Prostate cancer cells release prostate specific antigen (PSA), a serine protease that cleaves the parathyroid hormone-related peptide that is responsible for tumour-induced bone resorption. PSA may also activate osteoblastic growth factor release in the bone microenvironment during the process of bone metastases formation. Increased bone turn-over is also caused by bone-derived factors such as bone morphogenetic proteins (BMPs). Moreover, there is a focal imbalance between osteoblastic and osteoclastic activity. All this may lead to a vicious cycle which results in the development of osteoblastic metastases [30].
For nearly 40 years, bone scintigraphy with 99mTc labelled diphosphonates has been the ‘reference standard’ to detect skeletal metastases, due to its availability and low cost.
Not all patients with prostate cancer should undergo a bone scan. Routine use of a bone scan is omitted when the serum PSA level is <10 ng/mL, and may also be not necessary for those with PSA levels between 10 and 20 ng/mL, when they have T1 disease and Gleason scores of 6 or lower [31]. Almost all patients with a PSA >100 ng/mL have a widespread skeletal involvement. Bone scintigraphy should also be performed when levels of alkaline phosphatase (ALP) are >90U/L [32]. In summary, bone scintigraphy should be performed in patients with high-risk cancer, elevated serum ALP levels, bone pain, or equivocal bone lesions on other imaging modalities. Serial scans are often used to assess the extent of bone involvement and the effectiveness of therapy.
PET radiopharmaceuticals may also be of value in detecting bone metastases in patients with prostate cancer. The most commonly used one, 18F-FDG, has been shown to be challenging in the imaging of prostate cancer. The glucose utilization in well-differentiated prostate cancer is often too low to visualize the metastases. Moreover, the uptake in the primary tumour is difficult to visualize, due to its proximity to the bladder that shows intense accumulation of FDG. The slow rates of prostatic tumour growth are associated with low rates of glycolysis and therefore a low tumour uptake, which is also evident in metastatic bone disease [33]. 18F-FDG-PET was shown to be less specific than planar bone scintigraphy in prostatic bone metastases. Prostate cancer is the “classic” malignancy with false-negative results on 18F-FDG-PET [34].
Other PET radiopharmaceuticals that are used for the assessment of patients with bone metastases from prostate cancer are 11C- or 18F-labelled choline, 18F-fluoride, and 18F-FDHT. 18F-fluoride was reported to be highly sensitive in detecting bone metastases [35, 36] and has been shown to be more sensitive and specific than the bone scan in detecting bone metastases [6]. Increased cell proliferation in tumours and up regulation of choline kinase in cancer cells are suggested as two possible mechanisms for increased choline uptake in prostatic cancer cells. 18F-Choline may be superior for early detection of metastatic bone disease (especially for bone marrow involvement) [2]. This statement should, however, be collaborated by other studies. In patients with negative suspicious sclerotic lesions (after 18F-Choline PET), a second bone-seeking agent such as 18F-fluoride is recommended [37]. 18F-FDHT may be used when current knowledge of androgen receptor (AR) expression is necessary, or to solve diagnostic dilemmas that conventional imaging techniques or imaging techniques with unspecific radiopharmaceuticals cannot solve.
8 Nuclear Medicine Characteristics in Breast Cancer
Metastases in bone occur often in patients with breast cancer: In 26–50 % of patients bone is the first site of metastasis [38]. A high percentage of patients (30–85 %) with metastatic breast cancer will develop bone metastases during the course of the disease [39]. In most cases of metastatic bone lesions from breast cancer, mixed forms (both osteolytic and osteoblastic) are present. Breast cancer preferentially metastasizes to vertebrae and the pelvis, followed by ribs, skull and femur [40].
The detection rate of metastatic bone disease by using bone scintigraphy is 0.82 % in patients with stage I disease, 2.55 % in stage II, 16.75 % in stage III, and 40.52 % in stage IV [41, 42]. On the basis of these results routine screening with a bone scan in early stage breast cancer (stage I and II) is not recommended. The assessment of the response of bone metastases to therapy by solely following the changes in the intensity of bone scans is also not recommended [43]. For this purpose other imaging modalities (CT or MRI) may be better suitable.
In a meta-analysis, the value of bone scintigraphy and 18F-FDG-PET was evaluated in detecting bone metastases in patients with breast cancer. 18F-FDG-PET was found to have a higher specificity than a bone scan and proved to be superior to bone scintigraphy when used as a confirmatory imaging modality [44]. In another study it was reported that the morphologic appearance of the metastases influences their detection. Patients who had lytic or mixed type metastases had a higher number of lesions identified by using 18F-FDG, whereas in patients with sclerotic lesions the bone scan found a larger number of metastases [2].
As in prostate cancer, 18F-fluoride PET has the potential to replace the bone scan for routine patient assessment of breast cancer. When up-to-date knowledge of the estrogen receptor (ER) status is necessary or to solve diagnostic dilemmas that other imaging techniques cannot solve, 18F-FES could be the radiopharmaceutical of choice.
9 Nuclear Medicine Characteristics in Lung Cancer
The role of bone scintigraphy in patients with lung cancer has changed over the course of time. Advances in other imaging techniques (especially 18F-FDG PET/CT) have resulted in an improved accuracy of staging newly diagnosed lung malignancies. In the past, bone scintigraphy was commonly used as a routine staging technique for non small cell lung cancer (NSCLC) patients. Since the routine availability of PET/CT imaging, evidence of metastatic disease is often first identified in lymph nodes (hilar or mediastinal) or in distant organs (liver, adrenal glands), thereby obviating the need for bone scintigraphy. Furthermore, 18F-FDG PET/CT is also able to locate bone metastases with high sensitivity.
A study in 100 patients with NSCLS compared 18F-FDG-PET with conventional imaging modalities for staging. Ninety of the one hundred patients also underwent bone scintigraphy. In total, 12 patients were diagnosed with metastatic bone disease. 18F-FDG-PET identified bone metastases in 11 patients (92 %), only missing a bone metastasis located in the distal femur in 1 patient. That part of the body was not assessed during the study. The bone scan revealed metastatic bone lesions in only 6 (50 %) patients. The authors stated that the use of bone scintigraphy for staging NSCLC patients can be replaced by 18 F-FDG-PET [45]. Nowadays, 18F-FDG-PET/CT is indeed routinely used for staging lung cancer patients. There is no need any more for the bone scan in these patients.
10 Nuclear Medicine Characteristics in Other Solid Tumours
Various radiopharmaceuticals are available to stage neuroendocrine tumours, 123/131I-MIBG and somatostatin analogues for SPECT, 18F-FDG and 18F-DOPA for PET. The choice between all these options remains difficult. In carcinoid, reported sensitivities for 18F-DOPA-PET are high, ranging from 65 % to 100 % and this technique seems to be an excellent staging method. To localize tumours causing catecholamine excess (most often caused by phaeochromocytomas), 18F-DOPA PET was found superior to 123I-MIBG scintigraphy and CT/MRI [46]. 18F-FDG PET may be useful when tumours are dedifferentiated. Using 18F-DOPA of 18F-FDG is also dependent on the differentiation grade of the tumour. In patients with more aggressive and fast growing tumours, 18F-FDG performs better than 18F-DOPA and vice versa.
In well-differentiated thyroid cancer, 131I is still the radiopharmaceutical of choice, since it is possible to diagnose and predict therapeutic outcome. However, sometimes thyroglobulin levels are rising without any iodine uptake on the post therapy scan. Then 18F-FDG PET or 99mTc-HDP may be useful, to search for dedifferentiated metastases. In medullary thyroid carcinoma, 18F-DOPA PET imaging has been reported to perform equal or better than the reference imaging techniques. In this cancer type, there is a suspicion that one may have to rely on the calcitonin doubling-time to select the optimal PET radiopharmaceutical for the individual patient. Again, in more aggressive tumours (rapidly elevating calcitonin) 18F-FDG may perform better, in slow growing types 18F-DOPA is the radiopharmaceutical of choice.
Another cancer type is hepatocellular carcinoma (HCC), one of the most common cancers worldwide. Normally these patients are preoperatively staged by bone scintigraphy and CT of the chest in search for metastases. A recent study, however, showed that only a very minor percentage of patients (2 %) had positive findings on the bone scan. Recurrence rate and disease-free and overall survival showed no significant differences between patients with and without preoperative baseline bone scintigraphy. In conclusion, the authors state that there is no justification for routine preoperative bone scintigraphy to detect asymptomatic skeletal metastases in patients with resectable HCC [47].
11 Conclusions
Many radiopharmaceuticals are available and helpful for the diagnosis of bone metastases. Bone scintigraphy is still the nuclear medicine imaging method of choice in many malignancies and has been used for many years with good results. However, new emerging radiopharmaceuticals (SPECT and PET) are developed, specific for a certain type of cancer, and may also be used and may even—in some cancer types—replace bone scintigraphy. In general, PET radiopharmaceuticals are better to use than SPECT radiopharmaceuticals, since PET offers better spatial resolution and quantification is possible. Clinician and nuclear medicine physician have to work together, to use the best radiopharmaceutical for the individual patient leading to the best diagnostic accuracy.
The recent developments in soft- and hard-ware led to the introduction of hybrid camera systems, combining SPECT and PET with CT. All reports in literature point out that taking the (patho) physiology and anatomy together is essential for the field of nuclear medicine. Reported sensitivities, specificities, and diagnostic accuracies with the use of these new camera systems are better than before. For the patient it also has advantages: imaging can be performed earlier, is faster, and the patient only has to come once. Furthermore, the integrated reports of the radiologist and nuclear medicine physician should make it easier for the clinician to understand what is found.
References
Even-Sapir E (2005) Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med 46:1356–1367
Langsteger W, Heinisch M, Fogelman I (2006) The role of fluorodeoxyglucose, 18F-dihydroxyphenylalanine, 18F-choline, and 18F-fluoride in bone imaging with emphasis on prostate and breast. Semin Nucl Med 36:73–92
Yang HL, Wang XM, Deng SM (2011) Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol 21:2604–2617
Liu T, Cheng T, Xu W et al (2011) A meta-analysis of 18FDG-PET, MRI, and bone scintigraphy for diagnosis of bone metastases in patients with breast cancer. Skeletal Radiol 40:523–531
Qu X, Huang X, Yan W et al (2012) A meta-analysis of 18FDG-PET-CT, 18FDG-PET, MRI, and bone scintigraphy for diagnosis of bone metastases in patients with lung cancer. Eur J Radiol 81:1007–1015
Even-Sapir E, Metser U, Mishani E et al (2006) The detection of bone metastases in patients with high-risk prostate cáncer: 99mTc-MDP planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med 47:287–297
Urhan M, Dadparvar S, Mavi A et al (2007) Iodine-123 as a diagnostic imaging agent in differentiated thyroid carcinoma: a comparison with iodine-131 post-treatment scanning and serum thyroglobulin measurement. Eur J Nucl Med Mol Imaging 34:1012–1017
Alzahrani AS, Bakheet S, Al Mandil M et al (2001) 123I isotope as a diagnostic agent in the follow-up of patients with differentiated thyroid cancer: comparison with post 131I therapy whole body scanning. J Clin Endocrinol Metab 86:5294–5300
Koopmans KP, Neels ON, Kema IP et al (2009) Molecular imaging in neuroendocrine tumors: molecular uptake mechanisms and clinical results. Crit Rev Oncol/Hematol 71:199–213
Hiorns MP, Owens CM (2001) Radiology of neuroblastoma in children. Eur Radiol 11:2071–2081
Ozer S, Dobrozemsky G, Kienast O et al (2004) Value of combined CT/SPECT technology for avoiding false positive planar (123)I-MIBG scintigraphy. Nuklearmedizin 43:164–170
Zuetenhorst JN, Hoefnagel CA, Boot H et al (2002) Evaluation of (111)In-pentreotide, (131)I-MIBG and bone scintigraphy in the detection and clinical management of bone metastases in carcinoid disease. Nucl Med Commun 23:735–741
Krenning EP, Kwekkeboom DJ, Bakker WH et al (1993) Somatostatin receptor scintigraphy with [111In-DTPA-D-Phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med 20:716–731
Hillel PG, van Beek EJ, Taylor C et al (2006) The clinical impact of a combined gamma camera/CT imaging system on somatostatin receptor imaging of neuroendocrine tumors. Clin Radiol 61:579–587
Boellaard R, O’Doherty MJ, Weber WA et al (2010) FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging 37:181–200
Grant FD, Fahey FH, Packard AB et al (2008) Skeletal PET with 18F-fluoride: applying new technology to an old tracer. J Nucl Med 49:68–78
Bridges RL, Wiley CR, Christian JC et al (2007) An introduction to Na18F bone scintigraphy: basic principles, advanced imaging concepts, and case examples. J Nucl Med Techn 35:64–76
Agool A, Glaudemans AW, Boersma HH et al (2011) Radionuclide imaging of bone marrow disorders. Eur J Nucl Med Mol Imaging 38:166–178
Dittmann H, Dohmen BM, Paulsen F et al (2003) [18F]FLT PET for diagnosis and staging of thoracic tumors. Eur J Nucl Med Mol Imaging 30:1407–1412
Schröder H, Larson SM (2004) Positron emission tomography for prostate, bladder, and renal cancer. Semin Nucl Med 34:274–292
De Jong IJ, De Haan TD, Wiegman EM et al (2010) PET/CT and radiotherapy in prostate cancer. Q J Nucl Med Mol Imaging 54:543–552
Glaudemans AW, Enting RH, Heesters MA et al (2013) Value of 11C-methionine PET in imaging brain tumors and metastases. Eur J Nucl Med Mol Imaging 40(4):615–635
Shiiba M, Ishihara K, Kimura G et al (2012) Evaluation of primary prostate cancer using 11C-methionine PET/CT and 18F-FDG-PET/CT. Ann Nucl Med 26:138–145
Nunez R, Macapinlac HA, Yeung WH et al (2002) Combined 18F-FDG and 11C-methionine PET scans in patients with newly progressive metastatic prostate cancer. J Nucl Med 43:46–55
Jager PL, Chirakal R, Marriott CJ et al (2008) 6-L-18F-fluorodihyroxyphenylalanine PET in neuroendocrine tumors : basic aspects and emerging clinical applications. J Nucl Med 49:573–586
Van Kruchten M, Glaudemans AW, De Vries EF et al (2012) PET imaging of estrogen receptors as a diagnostic tool for breast cancer patients presenting with a clinical dilemma. J Nucl Med 53:182–190
Castelucci P, Jadvar H (2012) PET/CT in prostate cancer: non-choline radiopharmaceuticals. Q J Nucl Med Mol Imaging 56:367–374
Teunissen JJ, Kwekkeboom DJ, Valkema R et al (2011) Nuclear medicine techniques for the imaging and treatment of neuroendocrine tumours. Endocr-Relat Cancer 18:S27–S51
Van Vliet EI, Hermans JJ, De Ridder MA et al (2012) Tumor response assessment to treatment with [177Lu-DOTA0, Tyr3]ocreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors: differential response of bone versus soft-tissue lesions. J Nucl Med 53:1359–1366
Wymenga LF, Boomsma JH, Groenier K et al (2001) Routine bone scans in patients with prostate cancer related to serum prostate-specific antigen and alkaline phosphatase. Brit J Urol 88:226–230
Thurairaja R, McFarlane J, Traill Z et al (2004) State-of-the-art approaches to detecting early bone metastasis in prostate cancer. Brit J Urol 94:268–271
Hirobe M, Takahashi A, Hisasue SI et al (2007) Bone scanning—who needs it among patients with newly diagnosed prostate cancer? Jpn J Clin Oncol 37:788–792
Lawrentschuk N, Davis I, Bolton D et al (2006) Positron emission tomography and molecular imaging of the prostate: an update. Brit J Urol 97:923–931
Fogelman I, Cook G, Israel O et al (2005) Positron emission tomography and bone metastases. Semin Nucl Med 35:135–142
Schirmeister H, Glatting G, Hetzel J et al (2001) Prospective evaluation of clinical value of planar bone scan, SPECT and 18F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med 42:1800–1804
Oyen WJ, Withes JA, Corstens FH (2001) Nuclear medicine techniques for the diagnosis and therapy of prostate carcinoma. Eur Urol 40:294–299
Behesti M, Vali R, Waldenberger P et al (2008) Detection of bone metastases in patients with prostate cancer by F-18 fluorocholine and F-18 fluoride PET-CT: a comparative study. Eur J Nucl Med Mol Imaging 35:1766–1774
Coleman RE, Rubens RD (1987) The clinical course of bone metastases from breast cancer. Br J Cancer 55:61–66
Hamaoka T, Madewell JE, Podologg DA et al (2004) Bone imaging in metastatic breast cancer. J Clin Oncol 22:2942–2953
Krishnamurthy GT, Tubis M, Hiss J et al (1977) Distribution pattern of metastatic bone disease. A need for total body skeletal image. JAMA 237:2504–2506
Brar HS, Sisley JF, Johnson RH (1993) Value of preoperative bone and liver scans and alkaline phosphatase in the evaluation of breast cancer patients. Am J Surg 165:221–223
Yeh KA, Fortunato L, Ridge JA et al (1995) Routine bone scanning in patients with T1 and T2 breast cancer: a waste of money. Ann Surg Oncol 2:319–324
Libshitz HI, Hortobagyi GN (1981) Radiographic evaluation of therapeutic response in bony metastases of breast cancer. Skeletal Radiol 7:159–165
Cook GJ, Houston S, Rubens R et al (1998) Detection of bone metastases in breast cancer by 18FDG PET: differing metabolic activity in osteoblastic and osteolytic lesions. J Clin oncol 16:3375–3379
Marom EM, McAdams HP, Eramus JJ et al (1999) Staging non-small cell lung cancer with whole-body PET. Radiology 212:803–809
Fiebrich HB, Brouwers AH, Kerstens MN et al (2009) 6-[F-18]Fluoro-L-dihydoxyphenylalanine positron emission tomography is superior to conventional imaging with 123I-metaiodobenzylguanidine scintigraphy, computer tomography, and magnetic resonance imaging in localizing tumors causing catecholamine excess. J Clin Endocrinol Metabol 94:3922–3930
Witjes CD, Verhoef C, Kwekkeboom DJ et al (2013) Is bone scintigraphy indicated in surgical work-up for hepatocellular carcinoma patients? J Surg Res 181(2):256–261
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Glaudemans, A.W.J.M., Signore, A. (2014). Nuclear Medicine Imaging Modalities: Bone Scintigraphy, PET-CT, SPECT-CT. In: Vassiliou, V., Chow, E., Kardamakis, D. (eds) Bone Metastases. Cancer Metastasis - Biology and Treatment, vol 21. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7569-5_5
Download citation
DOI: https://doi.org/10.1007/978-94-007-7569-5_5
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7568-8
Online ISBN: 978-94-007-7569-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)