Abstract
Purpose
Using 123I for diagnostic purposes avoids the risk of stunning for subsequent radioiodine treatment and affords an excellent image quality. In this study we assessed the role of 123I in comparison with 131I post-treatment imaging in patients with thyroid cancer.
Methods
We compared a total of 292 123I scans with their corresponding post-treatment 131I images. Patients received a therapeutic dose of 131I following diagnostic scanning with 50–111 MBq of 123I. All patients were in a hypothyroid state (>30 μIU/l) before radioiodine administration for either diagnostic or therapeutic purposes.
Results
In 228 out of 263 patients with a positive diagnostic scan, 123I whole-body scan findings were concordant with those of corresponding post-treatment 131I images (concordance rate 87%). However, there were 44 additional foci of abnormal uptake on post-treatment 131I scans in 22 discordant cases with no impact on therapeutic management of the patients. In 13 patients, there was at least one new site on post-treatment images that had been missed on pretreatment 123I images. Twenty-nine patients with a negative diagnostic scan were treated with 131I owing to a high serum thyroglobulin level (range 11.3–480 ng/ml). Radioiodine uptake sites were seen in eight post-treatment scans. In 21 pairs of whole-body scans, both the pre- and the post-treatment scan were negative (concordance rate 72.4%).
Conclusion
123I scanning is comparable to high-dose 131I post-treatment imaging in thyroid carcinoma patients, and 123I offers excellent image quality as a diagnostic agent. It avoids disadvantages such as stunning before treatment and delivery of a high radiation dose to patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iodine-131 possesses certain properties which makes it a unique radiopharmaceutical for the management of patients with thyroid cancer. It emits β-particles, is readily available, and has a low cost and a long half-life (8.02 days). It is the main agent for the ablation of residual thyroid tissue and the treatment of recurrent or metastatic differentiated thyroid carcinoma [1, 2]. However 131I has certain disadvantages as a diagnostic agent: The quality of the images generated with this radionuclide is suboptimal owing to its physical characteristics, such as high γ-energy. Furthermore, its β-emission decreases the success rate of treatment because of the stunning effect on functioning thyroid tissue if it is used before high-dose radioiodine treatment. Instead, 123I is considered an optimal agent for diagnostic purposes before therapy with 131I. It is a pure γ-emitter with no stunning effect on functioning thyroid cells and has a γ-energy of 159 keV, which is optimal for conventional scintillation cameras. It also delivers a lower radiation dose to patients owing to its relatively short half-life (13.3 h) and lacks β-particle emission [3–8].
In this study we assessed the performance of 123I as a diagnostic imaging agent in patients who were evaluated for either radioablation or treatment of persistent thyroid carcinoma, by comparison with the corresponding high-dose post-treatment 131I scans.
Materials and methods
Two hundred and ninety-two differentiated thyroid carcinoma patients (79 male, 213 female; age range 15–81 years, median 47) were included in the study. The histopathology was papillary in 284, Hürthle cell in six, and follicular in two. The patients had undergone total or near-total thyroidectomy 1 month to 12 years earlier and had a complete clinical examination and laboratory tests, including determination of thyroid stimulating hormone (TSH), thyroglobulin (Tg), and anti-thyroglobulin (TgAb) levels. A diagnostic 123I whole-body scan was performed to determine the residual thyroid tissue for radioablation after initial surgery and also to detect persistent disease in patients with an elevated serum Tg measurement during the surveillance period. The patients followed a low-iodine diet for about 1 week before radioiodine administration. Serum TSH levels were elevated (>30 μIU/l) before both 123I whole-body scanning and 131I treatment in each patient. The patients were given approximately 50–111 MBq of 123I, and anterior/posterior whole-body scans were obtained using a dual-head gamma camera (Picker 2000, Millennium-General Electric) 24 h later. The patients were divided into scan-positive and scan-negative groups according to 123I scan findings. In the scan-positive group, a therapeutic dose of 131I was administered orally (range 1,147–7,733 MBq; mean 3,829). The dose of 131I was determined empirically according to the clinical status, the histopathological report, and pretreatment scan findings. The dose of 131I ranged between 1,850 and 3,700 MBq if the disease was localized to the thyroid gland and the pretreatment 123I scan showed only focal uptake in the thyroid bed. If cervical lymph node metastases were present, the activity was between 3,700 and 5,550 MBq, and if there was evidence of distant metastases to the lungs or bone, approximately 7,400 MBq 131I was administered. In the scan-negative group, patients also received a therapeutic dose of 131I, ranging between 3,700 and 7,400 MBq (mean 5,500), owing to elevated serum Tg levels (>10 ng/ml).
Serum Tg was measured by Nichols immunochemiluminometric assay (ICMA) in TgAb-negative specimens (Nichols Institute Diagnostics, San Juan Capistrano, CA, USA). The measurements of Tg with a TgAb-positive serum were performed by a radioimmunoassay method developed by USC Endocrine Services Laboratory, University of Southern California, Los Angeles. Resistance to TgAb interference was conferred by use of a high-affinity polyclonal rabbit antibody together with extensive purification of the 125I-labeled Tg tracer.
Pre- and post-treatment whole-body scans were obtained within a time interval of 6–8 days (mean 7.2 days). For the purposes of this study we compared the pretreatment 123I scans with the corresponding 131I post-treatment images. The concordance rate between pretreatment 123I diagnostic and post-treatment 131I scans was calculated as: (number of concordant scans/total number of scans)×100.
This study was approved by the institutional review board of the University of Pennsylvania School Medicine.
Results
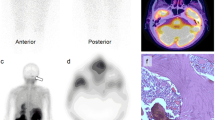
In the diagnostic scan-positive group, 228 out of 263 pretreatment 123I scans were identical with the corresponding post-treatment 131I scans. We noted 631 foci of increased radioiodine uptake consistent with functioning thyroid residual tissue or persistent disease on the pretreatment 123I scans. Of these, 599 lesions (94.9%) were located in the thyroid bed and neck, representing mainly residual tissue or locoregional disease infiltration via lymphatics. Other sites of radioiodine uptake were the lungs (18 lesions, 2.85%), bone (eight lesions, 1.26%), and mediastinum (six lesions, 0.09%). The post-treatment 131I scans showed more abnormal findings than the diagnostic images (Table 1). However, in eight patients, the total number of iodine uptake sites in the neck (six patients) and the lungs (two patients) was lower on post-treatment scans than on the pretreatment 123I scans (Fig. 1). Also, in 15 patients the intensity of the lesions was less on the post-treatment scans than on the pretreatment images (Fig. 2).
A 23-year-old patient with thyroid papillary carcinoma and multiple metastatic lesions to the lungs was examined with both 123I and 131I. More lesions are seen on the 123I scans (a) because of the superior spatial resolution of the images generated with this radiotracer compared to that of the post-therapy 131I scans (b)
We noted an additional 64 lesions in 35 patients on the post-treatment scans which were not seen on the pretreatment 123I images (Fig. 3). Of these 35 patients, 22 had additional foci at sites already imaged on pretreatment scans. However, in 13 patients (5%) additional foci on the post-treatment scans were at sites not seen on pretreatment 123I images. Serum Tg levels ranged between 1 and 300 ng/ml (median 9 ng/ml) in this group of patients. These new, additional lesion sites were noted in the lungs (eight lesions in six patients), bone (eight lesions in four) and mediastinum (four lesions in three patients). Therefore the administered dose of 131I would have been altered only in these 13 patients by knowledge of these additional sites. Thus, the clinically relevant concordance rate in this group of patients appeared to be 95%.
A 24-year-old woman with thyroid papillary carcinoma. The pretreatment 123I scan was negative (serum Tg 24 ng/ml) (a) but focal uptake was noted in the mediastinum on whole-body 131I scanning performed at approximately the 7th day of treatment (b). A metastatic lymph node at the junction of the right subclavian (SC) and brachiocephalic (BC) arteries was apparent on ultrasound (arrow) (c)
In the diagnostic scan-negative group of 29 patients, 123I scans showed no sites of abnormal uptake in spite of the elevated serum Tg levels. Serum Tg levels ranged between 11.3 and 480 ng/ml (median 76 ng/ml) in this group. In the same population, 21 patients showed no pathological uptake on pre- and post-treatment radioiodine whole-body scans (concordance rate 72.4%). Post-treatment 131I scans were positive in eight patients and revealed 12 additional sites: eight in the thyroid bed and neck, three in the mediastinum, and one in the lung (Fig. 4). In this group of patients, serum Tg levels ranged between 20.6 and 306 ng/ml (median 94 ng/ml).
Discussion
Iodine-123 is a pure γ-emitter and has a relatively short half-life of 13.3 h. It delivers a 100-fold lower radiation dose than the low-dose diagnostic 131I scan to the functioning thyroid cells and avoids stunning. In recent years the clinical role of 123I imaging in differentiated thyroid carcinoma patients has been investigated and the results have been compared with those of either diagnostic or post-treatment 131I scans. These reports have indicated optimal sensitivity for 123I in differentiated thyroid carcinoma for diagnostic purposes, detecting recurrences and distant metastases.
In this study, the results of pretreatment 123I diagnostic scans were comparable to those of post-treatment 131I imaging. In 228 of the 263 patients in the diagnostic scan-positive group, the pretreatment 123I scan and corresponding post-treatment scan yielded concordant findings regarding the number of lesion sites (concordance rate 86.7%). Of the 35 remaining patients with discordant findings, 22 showed additional lesions on the post-treatment 131I scans (17 in the thyroid bed/neck, three in the lung/mediastinum, and two in the bone) which would not have altered the therapeutic dose. Therefore, it can be assumed that, in these patients, the pretreatment 123I scans were in concordance with the corresponding post-treatment 131I scans. Thus the concordance rate increased to 95%. By comparison, in a group of 238 patients, Alzahrani et al. reported a concordance rate of 97.2% [9].
It has been reported that post-treatment whole-body scans are more sensitive than pretreatment whole-body scans and detect additional metastatic foci in the bone, mediastinum, and lungs in approximately 10% of patients [10]. In our study, a total of 64 additional foci were seen in 35 patients (9%). However, a change in clinical management may only occur upon the detection of a new focus in a new location images. The detection of an additional lesion on post-treatment whole-body images has no clinical impact on patient management if foci have previously been imaged at that site on pretreatment scanning. Only 13 (5%) of our patients had new foci on post-treatment scanning at sites not seen on the diagnostic 123I scans, i.e. in these patients the pretreatment evaluation underestimated the disease.
Metastatic lesions in the lungs can usually be seen clearly on pretreatment 123I scans because of the superior resolution of this agent. Patients with iodine-avid lung metastases have a better prognosis than those with lesions in the bone [11–13]. Determination of metastases in the lung on a pretreatment 123I scan enables administration of a relatively high 131I dose for treatment.
In certain cases with a considerable radioiodine concentration in metabolically active residual thyroid or tumor tissue, low-dose diagnostic scans and even high-dose post-treatment scans may fail to show all of the lesions. The less iodine-avid metastases, to either the lung or the bone, can be missed, and they can be subsequently detected after complete ablation of the dominant foci. In our study, ten lesions detected on pretreatment scans in eight patients were not clearly visualized on post-treatment scans owing to intense activity in adjacent tissues. Exact localization of lesions, especially in the neck, may have a clinical impact on the management of patients when surgery is considered.
We believe that use of 123I for diagnostic purposes both avoids the stunning effect and reduces the level of radiation exposure to patients (especially important in young women of child-bearing age). However, recurrent or metastatic thyroid carcinoma with a slow radioiodine metabolism might not be able to concentrate an adequate amount of radioiodine to be seen with 123I, which has a relatively shorter half-life. On the other hand, whole-body scanning performed several days after the administration of high-dose 131I allows visualization of such lesions.
In 15 patients the lesion intensity was less on post-treatment 131I scans than on 123I scans, as assessed by visual inspection. It should be noted that stunning of iodine-avid tissue with 123I and 131I is dose dependent. Hilditch et al. reported stunning of thyroid tissue in 15 of 16 patients after administration of a dose of 200 MBq [14]. In our study the maximum dose of 123I administered was 111 MBq—a relatively low dose to cause stunning. Another possible explanation for the aforementioned observation is that lesions with relatively high iodine turnover may be seen with minimal activity or may completely disappear on post-treatment whole-body imaging performed several days after treatment despite having been clearly visible on pretreatment 123I scans. On subsequent surveillance imaging of these patients, the lesions were not present.
Patients with thyroid carcinoma, an elevated serum Tg level, and a negative diagnostic radioiodine scan present a therapeutic dilemma [15, 16]. Alzahrani et al. reported that 46% of post-treatment scans became positive, delineating areas of radioiodine uptake that were not apparent on pretreatment 123I scans. It should be noted that the tumor volume and the degree of radioactivity concentration by the lesion are also major factors influencing the visualization of these lesions. Furthermore, progressive dedifferentiation of the thyroid cancer cells results in reduced radioiodine uptake. Occasionally even in the same patient, different metastatic tumor tissues may exhibit varying degrees of metabolic activity owing to variation in tumor differentiation. In our study, 29 thyroid carcinoma patients with elevated Tg levels of more than 10 ng/ml had negative pretreatment 123I scans. Post-treatment 131I whole-body scans were positive in only eight of these patients (27.6%), showing eight lesions in the thyroid bed and neck, three in the mediastinum, and one in the lung (Fig. 4). Schlumberger et al. reported that lung metastases were demonstrated on post-treatment scans in about 50% of patients who were treated with high doses of 131I owing to a high Tg level and had normal chest X-rays [17]. The remaining 21 pairs of whole-body scans, i.e. both the pre- and the post-treatment scan, failed to show any functioning lesions. The concordance rate of the pre- and post-treatment scans was 72.4%.
We conclude that 123I is an excellent diagnostic agent for whole-body scanning in patients with thyroid carcinoma. The imaging results are comparable to those generated with post-treatment 131I scans. Accordingly, this radiopharmaceutical can be used to visualize residual thyroid tissue and recurrent/metastatic differentiated thyroid carcinoma and to assess the extent of disease without the stunning effect that is frequently noted after the administration of 131I as a diagnostic agent.
Its cost is an issue that prevents 123I from being available on a routine basis. However, it is actually no more expensive than some other radiopharmaceuticals, including FDG, which is being increasingly used to image patients with suspected metastatic thyroid cancer. In the near future, the cost of 123I will become modest as more institutions establish a cyclotron and start delivering it. Finally, none of those patients with a negative diagnostic and a positive post-treatment scan had a serum Tg level of <20.6 ng/ml, and this value can serve as a cut-off level above which the post-treatment scan is more likely to be positive.
References
Tsang RW, Brierly JD, Simpson WJ, Panzarella T, Gospodarowicz MK, Sutchliffe SB. The effects of surgery, radioiodine and external radiation therapy on the clinical outcome of patients with differentiated thyroid carcinoma. Cancer 1998;82:375–88.
Coburn M, Teates D, Wanebo HJ. Recurrent thyroid cancer. Role of surgery vs. radioactive iodine. Ann Surg 1994;219:587–95.
Park HM. The stunning effect in radioiodine therapy of thyroid cancer. In: Freeman L, editors. Nuclear medicine annals. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. p 49–67.
Leger FA, Izembart M, Dagousset F, Barritault L, Baillet G, Chevalier A, et al. Decreased uptake of therapeutic doses of I-131 after 185 MBq I-131 diagostic imaging for thyroid remnants in differentiated thyroid carcinoma. Eur J Nucl Med 1998;25:242–6.
Mandel SJ, Shankar LK, Benard F, Yamamoto A, Alavi A. Superiority of I-123 compared with I-131 scanning for thyroid remnants in patients with differentiated thyroid cancer. Clin Nucl Med 2001;26 1:6–9.
Yaakob W, Gordon L, Spicer KM, Nitke SJ. The usefulness of I-123 whole-body scans in evaluating thyroid carcinoma and metastases. J Nucl Med Technol 1999;27:279–81.
Shankar LK, Yamamoto AJ, Alavi A, Mandel SJ. Comparison of I-123 scintigraphy at 5 and 24 hours in patients with differentiated thyroid cancer. J Nucl Med 2002;43:72–6.
Gerard SK, Cavalieri RR. I-123 diagnostic thyroid tumor whole-body scanning with imaging at 6, 24 and 48 hours. Clin Nucl Med 2001;27:1–8.
Alzahrani AS, Bakheet S, Al Mandil M, Al-Hajjaj A, Almahfouz A, Al Haj A. I-123 isotope as a diagnostic agent in the follow-up of patients with differentiated thyroid cancer: a comparison with post I-131 therapy whole-body scanning. J Clin Endocrin Metab 2001;86:5294–300.
Sherman SI, Tielens ET, Sostre S, Wharam MD Jr, Ladenson PW. Clinical utility of post-treatment radioiodine scans in the management of patients with thyroid carcinoma. J Clin Endocrinol Metab 1994;78:629–34.
Schlumberger M, Tubiana M, De Vathaire F, Hill C, Gardet P, Travagli JP, et al. Long-term results of treatment of 283 patients with lung and bone metastases from differentiated thyroid carcinoma. J Clin Endocrin Metab 1986;63:960–7.
Sisson JC, Giordano TJ, Jamadar DA, Kazerooni EA, Shapiro B, Gross MD, et al. I-131 treatment of micronodular pulmonary metastases from papillary thyroid carcinoma. Cancer 1996;78:2184–92.
Samuel AM, Rajashekharrao B, Shah DH. Pulmonary metastases in children and adolescents with well-differentiated thyroid cancer. J Nucl Med 1998;39:1531–6.
Hilditch TE, Dempsey MF, Bolster AA, McMenemin RM, Reed NS. Self-stunning in thyroid ablation: evidence from comparative studies of diagnostic I-131 and I-123. Eur J Nucl Med Mol Imaging 2002;29:783–8.
Pacini F, Lippi F, Formica N, Elisei R, Anelli S, Ceccarelli C, et al. Therapeutic doses of I-131 reveal undiagnosed metastases in thyroid cancer patients with detectable serum thyroglobulin levels. J Nucl Med 1987;28:1888–91.
Pineda JD, Lee T, Ain K, Reynolds JC, Robbins J. Iodine-131 therapy for thyroid cancer patients with elevated thyroglobulin and negative diagnostic scan. J Clin Endocrinol Metab 1995;80:1488–92.
Schlumberger M, Arcangioli O, Piekarski JD, Tubiana M, Parmentier C. Detection and treatment of lung metastases of differentiated thyroid carcinoma in patients with normal chest X-rays. J Nucl Med 1988;29:1790–4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Urhan, M., Dadparvar, S., Mavi, A. et al. Iodine-123 as a diagnostic imaging agent in differentiated thyroid carcinoma: a comparison with iodine-131 post-treatment scanning and serum thyroglobulin measurement. Eur J Nucl Med Mol Imaging 34, 1012–1017 (2007). https://doi.org/10.1007/s00259-006-0341-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-006-0341-x