Abstract
Bone is one of the most common target organs for cancer metastases which can frequently result in fractured or cracked bones and spinal cord compression. Here we review recent information regarding the use of high-intensity focussed ultrasound (HIFU) and other forms of thermal ablation for the pain palliation of bone metastases. High-intensity focussed ultrasound is a non-invasive and effective method for pain palliation and does not have cumulative toxicity effects when used. Similarly, radiofrequency-ablation effectively treats bone metastasis pain but is limited to the placement of hardware for radiofrequency targeting. The effectiveness of thermally ablative techniques is generally limited by the maximum volume that can be ablated and the precision of image-guidance, and it has been concluded that ablative techniques may produce synergistic effects if used in conjunction with standard forms of care. Included is a discussion of the development of HIFU, its mechanism of operation, recent clinical studies using image-guided HIFU, the limitations of HIFU, and a comparison to other ablative techniques such as radiofrequency ablation and cryotherapy. These innovative technologies are reaching clinical adoption as new methods for the treatment of bony metastases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Metastasis is one of the complications of cancer that has increased the need for effective forms of palliative treatment. In particular, with better local control of disease, the number of cases of bone metastases has risen, resulting in many negative side effects and impairments for patients. Bone metastases are discovered frequently, occurring in up to 70 % of patients with advanced prostate or breast cancer [1]. Among patients with bone metastases, 50–75 % experience severe pain [2]. Development of bone metastases along the spine is common, frequently resulting in spinal cord compression, vertebral compression fractures, and complications associated with the proper functioning of the nervous system. Malignant spinal cord compression can create sensory deficits, loss of mobility and paralysis [2]. Given this, there is a high demand to safely relieve the symptoms of bone metastases in patients as well as increase their survival rate and quality of life.
Various treatment modalities have been used in the palliation of bone metastases including radiotherapy, surgical resection, chemotherapy, vertebroplasty, kyphoplasty, or a combination of these approaches. However, it is not always possible to treat all patients with these approaches and alternate modalities must be considered. High-intensity focussed ultrasound (HIFU) is a technique that relies on the same principles as diagnostic ultrasound [3], but has been adapted for use in the palliative treatment of metastases. This modality leaves tumour-surrounding, healthy cells undamaged and minimizes side effects associated with treatment. Moreover, it is non-invasive, functions without ionizing radiation, has a relatively short procedure time, and can be more easily and willingly repeated than other treatments [4]. In 1942, high-intensity ultrasound beams were used in the first therapeutic trial but the technology did not progress much further due to a lack of real-time imaging as well as some physical barriers [3]. Recently, the field has greatly progressed with the development of systems such as Magnetic Resonance-guided HIFU (MRgFUS) and Ultrasound-guided HIFU (USgFUS), and these techniques have become practical modalities used to ablate tissues in solid tumours while simultaneously acquiring procedural measurements.
2 Development of HIFU
The development of HIFU began in the mid-twentieth century with the use of high-intensity ultrasound beams for treatment of neurological disorders in humans. Since then, HIFU has proven to be very effective in thermal ablation of solid tumours in the breast and prostate gland, and has continued to show promising results in the management of secondary tumours.
2.1 First Users of Ultrasound Therapy
It was known in the 1800s that the concept of piezoelectricity meant that charge could be generated when pressure was applied to a material. Transducers ultimately used in ultrasound imaging relied on reverse piezoelectricity and made use of the conversion between electrical energy and mechanical energy [5], permitting echo waves from responding tissues to provide diagnostic information. In 1938, Raimar Pohlman, who had developed an imaging method using acoustic lenses, demonstrated a therapeutic effect on human tissues using ultrasonic waves transmitted through acoustic lenses [5]. This was subsequently used to treat inflammatory conditions. These ultrasound waves, in the frequency region of 20 kHz to 2 MHz, were studied in 1942 to develop a technique known as focussed ultrasound [3]. Studied by John G. Lynn and Tracy J. Putnam in 37 animal models, high-frequency and short wavelength waves permitted the successful transfer of high doses of ultrasonic energy to brain areas with negligible damage to non-targeted tissue [5]. Interest in this continued when William and Francis Fry furthered this study in primate models by using a system of four transducers that delivered high-intensity focussed acoustic waves to confined tumour areas in brain ganglia. They noted a significant and lasting elevation of temperature in target tissues, with a minimal rise in temperature in surrounding cells [5]. This specificity proved to be one of the greatest advantages to ultrasound therapy and provided the motivation for further continued development.
Symptoms of neurological disorders, such as Parkinson’s disease, have been treated using high-intensity focussed ultrasound. However, visualization of brain tissue and image-guidance of therapy was critical in order to ascertain the appropriate clinical follow-up in patients, particularly when studying brain cortical regions beyond the cranium. A B-mode image-guided system was developed in the 1970s which allowed for two-dimensional visualization of ablation in cranial regions [5]. Since then, HIFU techniques were augmented in the 1990s with the combination of rapidly induced hyperthermia in tumour regions and image-guidance using advanced scanning techniques such as Magnetic Resonance Imaging (MRI) and Computed Tomo-graphy (CT). Image-guided investigations will be discussed further in Sect. 14.5.
2.2 Primary Tumour Ablation
A large number of clinical studies on primary solid tumours have conclusively demonstrated that HIFU ablation serves as a valid therapeutic option. Therapeutic trials have been completed on tumours in regions such as the breast, prostate gland, pancreas and liver, and studying these can have implications on our understanding of potential uses for HIFU in the treatment of metastatic sites.
One study treated over 1,000 patients in China with solid carcinomas using the HIFU system Chongqing Haifu [6]. The solid carcinomas included liver cancer, breast cancer, kidney cancer, pancreatic cancer and other primary malignancies. Feng et al. reported that within 1–2 weeks post-treatment, a distinct boundary was detectable in patients between the targeted and destroyed regions and viable tissue. The treated tissue included the tumour lesion, as well as a small 1.5–2.2 cm margin around the cancerous site. The visibility in follow-up images of a sharp boundary between damaged and viable cells has been a means of detecting the success of ablation. In another study using HIFU for treatment of hepatocellular carcinoma (HCC) after partial rib resection in 16 patients, complete tumour necrosis was achieved in 70 % of the lesions after the first HIFU treatment [7]. In the remaining lesions, HIFU treatment was performed a second time and complete tumour necrosis was visible in all tumours. Again, in a study of US-guided HIFU treatments in patients with advanced pancreatic cancer, eight patients’ pain symptoms were completely stopped with either one or two treatment sessions [8]. The possibility of retreatment and the capability of one to two treatments to achieve clinical goals make this a feasible alternative to other modalities. Finally, in a clinical study described by Zheng et al. on HIFU as a safe therapy for HCC adjacent to major hepatic veins, all 39 patients achieved complete tumour necrosis despite the close proximity of the lesions to major hepatic blood vessels. In follow-ups 24 ± 17 months after treatment, no major blood vessel injury was noted [9]. Models studying acoustics and thermal energy in fluids have indicated that this could be due to convective heat transfer and dissipation of heat through blood flow away from the vessel wall [10]. The low vulnerability of blood vessels to HIFU treatment has allowed for its use near such. These advantages have justified the expansion of HIFU ablation for pain palliation of metastatic tumours.
3 Mechanism Description of HIFU
There are various technological changes that have been made recently to enhance ultrasound equipment in order to facilitate modern image-guided therapy. Standard hardware and software components are described in this section as well as the physical changes seen in tumour composition after treatment.
3.1 Hardware and Software Components
Equipment for HIFU requires a signal generator, a power amplifier and a transducer [11]. HIFU transducers vary geometrically and electronically. Transducers can be concave and self-focussing or can be flat with an acoustic lens on top. Transducers can also be manipulated electronically and can be configured by having multiple piston transducers on a spherically focussed bowl [3]. When multiple transducers are used, the relative phases of transducer elements are different; this system is known as a phased-array transducer. This permits the acoustic beams to be guided in different directions due to their varying phases, which also can correct for some of the problems associated with lenses such as spherical aberration and distortion at the focal point. The signal generator creates the frequency and initial amplitude of the signal, which is then amplified [11]. The transducer vibrates as a result of the produced electric field and generates ultrasonic, high-frequency beams that converge with a fixed focus at the site of the lesion [3]. Transducer focal lengths can range with common focal lengths of 90, 130 and 160 cm [12], and treatment areas are around 3 mm wide and 10–12 mm long [13]. While many conventional transducers are physically moved against the area of treatment, phased-array ultrasonic treatment modalities are electronically controlled and do not require physical sweeping of the transducer [3].
The transducers and imaging systems are connected to a computer for tumour targeting and positioning guidance. Thermal maps and dose maps are created, which permit real-time visualization and feedback. When temperatures or doses reach certain limits, this is visible on the monitoring system and heating can be stopped [14].
3.2 Principle of Operation
HIFU creates a quick rise in temperature when acoustic power is delivered [10]. The intensity of HIFU ranges from 100 to 10,000 W/cm2 with compression pressures as high as 70 MPa and rarefaction pressures around 2 MPa [3]. The transducer permits, with electronic steering, the distribution of the energy over the external surface of the region of interest, but focuses the energy over a small area at the focal point so that tissue between the transducer and focal point remains undamaged [15]. Two major forms of tumour tissue damage can occur during treatment. The destruction of tissue and vasculature at the focal point and not in nearby regions is ideal, especially when treating regions of the body near the spinal cord. When tissue temperatures rapidly rise within seconds in the focal region, the destruction of the vasculature and cellular integrity occurs and necrotic lesions form; this results in irreversible cell death. The energy deposition is high enough to also cause protein denaturation, which can usually occur at temperatures higher than 43 °C [11]. Typically, during HIFU, temperatures above 56 °C for 1 s or temperatures of 65–100 °C for 0.5–1 s result in coagulative necrosis [16].
High-intensity focussed ultrasound can significantly disrupt the vascular elasticity and fibrin in tumour regions and can also result in mechanical effects such as acoustic cavitation [3]. Acoustic cavitation causes necrosis through a different means. Non-linear, high-amplitude pressure oscillations occur when the acoustic power is deposited. This creates gas bubbles that contract and expand rapidly, resulting in localized heat formation and tissue damage [11]. The oscillation of these gas bubbles can also generate an effect known as microstreaming, in which viscous tissue fluid moves rapidly. Friction generated by these viscous layers moving past each other leads to further heating and can potentially damage cell membranes [17]. This form of cell death is less predictable and more unstable than that above.
4 Assessment of Clinical Studies
Bone is one of the most common target organs for cancer metastases, followed by lung and liver as metastatic sites [18]. Bone metastases frequently results in sclerotic or fractured bones, or asymmetrical vertebral body collapse [19]. It can lead to hypercalcemia—the release of calcium into the blood stream—if bone resorption occurs. When bone metastases affect the bone marrow, blood cell levels may become abnormal. This can lead to anemia due to loss of red blood cells, frequent infections during periods of low white blood cells, or unusual bleeding patterns due to a lack of platelets. One of the most prominent symptoms is malignant spinal cord compression, which occurs when the tumour squeezes the spinal cord [20]. Among the 500,000 people in the United States who die from cancer annually, 12,700 will suffer from malignant spinal cord compression [2]. Malignant spinal cord compression can result in motor weakness (76–78 % of patients), autonomic dysfunction (40–64 %), or sensory loss (51–80 %) [21] and can cause neck and back pain, numbness, or difficulties with walking and posture [20]. Cauda equina syndrome can be another outcome as nerves at the end of the spinal cord are compromised due to spinal cord compression. The following discussion quantifies and analyzes the use of HIFU ablation for spine and bone metastases by comparing three clinical studies.
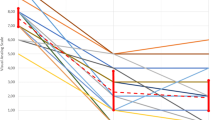
Liberman et al. studied patients with bone metastases using MRgFUS [22]. Thirty-six procedures were completed on 31 patients; 11 out of the 31 patients’ primary tumours were breast tumours and 18 out of the 31 metastatic sites were in the iliac bone, the uppermost pelvic bone. Spinal anesthesia was used during the procedure and the ultrasound transducer was a phased-array system. Mean treatment times were 66 min, ranging from 22 to 162 min. The average energy per sonication was 1,135 J, ranging from 440 to 1,890 J, with the number of sonications averaging 17.3 (range 8–32). Results of the study concluded that patients showed a decline in pain sensations, with a visual analog scale mean baseline score of 5.9 at the beginning of the study, a mean of 3.8 3 days after treatment, and a mean of 1.8 3 months after the study (p < 0.003). It was also noted that 67 % of patients reduced their opioid medication intake. This study suggests that the pain improvement could be due to denervation of local bone and a consequent reduction in pain sensation caused by heat denaturation of the periosteal layer, in addition to the reduction of pain-causing pressure by ablation of tumour tissue. This was suggested since bone absorption of acoustic energy is up to 50 times greater than soft tissue tumours. The lower thermal conductivity and higher absorption rate of bone permit the use of lower energy levels and destroys less periosteum. Twenty-five of the 31 patients participated in a follow-up assessment 3 months later and of these, 50 % reported a VAS score of 0, indicating that there was an equal partial and complete response in these patients. However, with a larger patient group and a longer follow-up time, further analysis could be completed with regard to pain palliation. While the source of the pain could be derived from various origins as the patients were ill with several metastases, the study was useful in determining whether or not some pain palliation can be possible from focussed ultrasound surgery.
A study reported by Li et al. compared the use of HIFU in 25 patients with malignant bone tumours at either primary or metastatic sites. The treatment was guided by B-mode ultrasonography and testing was conducted using biomarkers, contrast-enhanced MRI and PET-CT, both before and after HIFU treatment, using 99mTc-methane-diphosphonate (99mTc-MDP). Out of the 25 patients, five underwent two HIFU sessions each and two patients underwent three HIFU sessions each. The primary tumours (osteosarcomas) were situated at the femur, tibia, humerus, scapula, pubis and rib. The metastatic bone tumours had varying primary tumour sites such as hepatic sarcomas, lung sarcomas and colorectal sarcomas. The tumour blood vessels targeted had a diameter of less than 200 μm and the metastatic bone tumours had an average volume of 277.23 cm3. Mean treatment time was 231 +/− 173 min, with a range from 28 to 648 min. In patients with primary bone tumours, 4–6 weeks of chemotherapy was administered prior to receiving HIFU treatment and 10–20 days following HIFU treatment patients received an additional 2–4 weeks of chemotherapy (intravenous methotrexate/vincristine, doxorubicin, and cisplatin). Adjuvant chemotherapy was given to patients with metastatic bone tumours if deemed necessary. Table 14.1 summarizes the findings.
Significant conclusions can be drawn from comparing the results of HIFU treatment on these primary and metastatic bone tumours. These findings indicate that patient ratings of pain significantly decreased after treatment and the majority of patients had either a complete or partial response as opposed to a moderate response, stable or progressive disease. It is noteworthy to point out that the overall response rate was 9.6 % higher when treating with HIFU on primary bone tumours than on metastatic bone tumours. Moreover, the 0 % survival rate 3 and 5 years following treatment to metastatic bone tumours differs, as expected, from the 69.2 % and 38.5 % 3 and 5 years after treatment, respectively, on primary bone tumours. With these treatments four of the metastatic patients developed a low-grade fever of around 37.5–38.4 °C, however, their body temperatures returned to normal within 3–5 days. In addition, 1–5 days following HIFU therapy, targeted areas showed swelling which disappeared entirely within 1 week after treatment. Prior to HIFU treatment, six patients were noted to have venous skin enlargement, but examination following treatment revealed that four patients were entirely asymptomatic, one patient displayed a decrease in swelling and one patient’s symptoms remained unchanged. Four to six weeks after HIFU, responsive primary and metastatic tumours were cold lesions (on radionuclide scans) and displayed reduced contrast agent uptake.
In these treatments, the high absorption of tumour-laden bone and the lower chance of retransmission of acoustic energy results in a high efficiency in converting HIFU acoustic energy into heat. The uniform distribution of therapeutic dose created by HIFU and its ability to treat various tumour shapes expands its possibility to create necrosis in many different tumours. Overall, the use of HIFU on metastatic bone tumours did display improved symptoms and limb function. This study showed that the use of HIFU and chemotherapy might be synergistic, and similar to the first study, suggests that possible denervation at the periosteum contributed to the results, as well as reduction in tumour mass and spinal pressure.
A study documented by Gianfelice et al. used MRgFUS on 11 patients with a total of 12 metastatic lesions [23]. Here, patients had previously undergone chemotherapy and radiation therapy, and the received HIFU treatment for pain and symptom reduction. In these patients with bone metastases, primary tumours existed in the breast, kidney, lung and liver, with breast tumour sites in 5 out of the 11 patients. Bone lesions treated included the ilium, scapula, clavicle and ischium, with 7 of the 12 lesions within the ilium. The number of sonications ranged from 12 to 18 and treatment time ranged from 28 to 103 min. Using a visual analog score pain scale, the mean score of 6.0 before treatment was reduced to a mean of 0.5 3 months after treatment, which is a decrease of 92 % (p < 0.01). Pain was clearly reduced at 14 days and pain medication usage also declined. Seven patients no longer required use of analgesics, and the remaining four patients had a 50 % or greater reduction in analgesic use.
No serious adverse effects related to treatment were observed. All osteolytic lesions demonstrated some thinning of the nearby bone cortex, but no patients were noted to have severe cortical destruction. There was some necrosis noted in the medullary component of bones, which were attributed to the thinning of overlying bone, consequently decreasing its absorption and permitting the transmission of thermal energy to the inner bone. In order to assess the effect of repeat treatment, one individual underwent two separate HIFU treatments many days apart, and another had two adjacent metastatic sites treated in the same HIFU session. Repeat treatment showed no increase in morbidity or cumulative effects. It is important to note during procedures whether lesions are osteolytic or osteoblastic as this factor significantly contributes to the analysis of any post-treatment bone sclerosis and thus, the efficacy of HIFU.
Taken together, these studies contribute to the validation of HIFU as a non-invasive method of tumour ablation. Mean-treatment time was longer in the ultrasound-guided study than in either of the magnetic resonance-guided studies, and the lower end of these treatment ranges approximates the treatment time for radiotherapy [24]. The second study demonstrates that HIFU promotes longer survival in patients with primary malignant bone tumours as opposed to those with metastatic bone tumours, which should be taken into account when treating patients with differing stages of cancer. Studies of surgical resection show that this course of treatment better promotes long-term survival than HIFU in patients with bony metastases [25]. Although preservation of the integrity of the nervous system is one of the objectives when treating metastases, studies indicate that local denervation of the bone periosteum can reduce pain sensation. This contributes to greater pain palliation with HIFU as peristeal denervation occurs in conjunction with coagulative necrosis of the tumour region. Malignant bone tumours radically alter the integrity of cortical bone and result in differences between the acoustic characteristics of normal bone and tumour-affected bone, which must be taken into account when treating these tumours with modalities such as HIFU.
5 Image-Guided HIFU
Image-guidance is a critical component to treatments, at all stages of a patient’s HIFU procedure. Real-time feedback is essential during sonications and the specifications of sonications can only be realized during patient-specific treatment with image-guidance for genemetric and temperature-controlled feedback. Specifically, imaging is necessary pre-treatment for tumour evaluation and protocol planning, immediately before treatment for patient and system positioning, during treatment to monitor thermal effects, and post-treatment to evaluate the success of the treatment. This section outlines advantages and disadvantages of MR- and US-guided HIFU (Fig. 14.1).
Interaction of software and hardware components in an MR-guided HIFU system [61]
5.1 Magnetic Resonance Imaging (MRI) Guidance
Imaging with MRI provides high anatomical resolution and high sensitivity in tumour delineation which allows for accurate treatment planning [26]. Magnetic resonance imaging –compatible ultrasound therapy transducers can be embedded in the patient MRI-tables to facilitate the use of the MR system. Transducers are often situated in water baths and coupled to patients via gel pads in order to eliminate the interference of the acoustic energy with air and increase the signal-to-noise ratio [23]. Transducers in MR-guided systems use piezo-composite materials to ensure MR compatibility with the magnetic field generated within the bore [27]. During MRgFUS procedures, transducer positioning is computer-controlled and is accomplished using a hydraulic system [28]. Linear actuators are hydraulically-driven and short pulses of pressure create motion that is step-wise and allows for precise transducer positioning [28]. MR images are taken during each sonication, which is a few seconds in duration, and then temperature and spatial maps are created and displayed. Processing of images, transferring of data, and the development of quantitative measurements often take about 10 s [28] (Fig. 14.2).
MRgFUS system showing the transducer and the positioning system and the ultrasonic energy converging at the focal point. The transducer is embedded in the patient table to facilitate the use of MRI [22]
Guidance with MRI allows for beam path visualization as well as tumour targeting in the sagittal, axial and coronal planes [29]. Transient tissue temperature can be measured using MRI due to the relationship between applied power and the proton resonant frequency (PRF) [30]. Health care professionals using MRI-guidance with HIFU have been able to detect damage past the targeted tissue due to both linear (frictional) ablation and unstable, non-linear forms of ablation (cavitation and streaming) and to adjust treatment accordingly [31]. This can be imposed on anatomical MRI images to detect regions where cell temperatures have reached toxic levels and to assess tissue damage thresholds [26]. Magnetic resonance imaging can also effectively display the boundary between untreated regions and those with coagulation necrosis [12]. Although MR systems are expensive and the initial apparatus can cost upwards of 1 million dollars [23], they provide immediate feedback during treatment permitting temperature and dose monitoring. Thermometry with magnetic resonance detects soft tissue temperatures around the targeted site, but the temperature of bone cannot be detected due to the lack of a PRF shift that is temperature-sensitive [22].
For the purposes of treatment, MRgFUS permits the shape of the focal volume to be modulated using spatial and temporal control [31]. Recent studies have shown an improvement in necrotic tumour volume by image-guided FUS as well as less energy propagation far from the target site, in comparison to regular sonications, with the energy level the same in both cases [31]. Magnetic responance-guidance allows for controlled, localized damage when treating tumours in close proximity structures that absorb large quantities of acoustic energy.
In the Liberman et al. study using MRgFUS on bony metastases[22], the phased-array Exablate® 2000 system by InSightec Ltd. (Haifa, Israel) was used in conjunction with a 1.5 T MRI scanner (General Electric, U.S.A.). Pretreatment MRI images were used to identify the targeted region. When patients were positioned on the tables, the position and sonication pathway were checked using T2-weighted (water-suppressed) fast spin-echo MR images. Patient treatment plans were personalized to eliminate damage to surrounding, non-targeted tissues. At the end of each treatment, T1-weighted (fat-suppressed) contrast-enhanced MR images were taken to ensure tumour ablation and minimal damage to surrounding tissues. Three months following treatment, T1- and T2-weighted MR images were repeated, showing no signs of long-lasting damage to the surrounding tissues. The successful results were confirmed in CT images taken 3 months later, which showed some calcification near the targeted tissues.
Gianfelice et al. reported the use of MRgFUS for painful bone metastases [23]. Unenhanced T1-weighted MR imaging and gadolinium enhanced T1-weighted MR imaging were completed prior to treatment (Fig. 14.3). Researchers said that this was completed to ensure that patients could be treated with MRgFUS and to create a baseline image when comparing treatment images. Images that were T2-weighted were taken on the treatment day, and T1-weighted imaging was completed 1–3 months following treatment. These images demonstrated an average decrease of 49.8 % in tumour volume, from 33.3 cm3 to 16.6 cm3. Imaging completed 3 months after treatment on nine of the 11 patients indicated a tumour increase in one patient (14 %), no change observed in two patients (0 %), and a decrease in tumour size in six patients by an average of 44 %, compared to the 1-month study. Unenhanced CT-imaging in nine patients confirmed that five patients (56 %) had increased bone density at the site of their osteolytic metastases. In general, the constant use of MRI is not harmful to patients and provides results that are useful in studying tumour volume at all stages of treatment, delineating between cases with successful and unsuccessful ablation procedures.
A patient from the study done by Gianfelice et al. [23] contrast-enhanced T1-weighted MR images pre-treatment (left) and post-treatment (right) show the medullary component of the osteolytic metastasis of the left iliac bone and the necrotic lesion
5.2 Ultrasound (US) Guidance
Ultrasound-guided HIFU systems, such as Ablatherm and Sonablate devices, use ultrasonic transducers for both imaging and treatment. When soft tissues are heated, the resulting echo pulses of acoustic energy travel back to the transducer and are used for detection of tissue response. Hyper-echoes are detected in B-mode ultrasonography [14]. They are believed to be created either when tissues boil due to cavitation or from bubbles generated during cavitation at the focal point [29]. In addition, since HIFU destroys tumour cells and vasculature, forms of ultrasound such as Doppler ultrasound can be used to detect changes in blood flow (perfusion) that occur during tissue damage subsequent to HIFU treatment. This cannot be done with other forms of imaging such as MRI or CT [32] (Fig. 14.4).
CT scan image showing the needle electrode placement into a metastatic tumour site at the rib. [45]
Other versions of image guidance such as USgFUS are still under development as they do not directly provide information about thermometry or elastography. Pulse-echo ultrasonic guidance is not always useful for imaging thermal damage because the ultrasonic backscattering coefficients of the ablated and non-ablated regions are not significantly different [10]. Some studies have attempted to use microwave-induced thermoacoustic tomography (TAT), which uses non-ionizing radiation to study the energy deposition in soft tissues. This imaging modality ideally produces images with high resolution due to the short wavelength of thermoacoustic waves as well as good contrast because of the differences in microwave absorption rates in various tissues [10]. Ultrasound-guided systems are relatively inexpensive compared to MR-guided systems and create high-resolution images, however they are still being modified as they do not confer all the advantages of other imaging modalities.
In a recent review [33], researchers compared studies in Chinese databases using USgFUS and MRgFUS on various benign and malignant tumours including bone metastatic sites. They concentrated on adverse events resulting from treatment and the extent to which these events depended on the site of the tumour and the system being used. Device-related side effects were not noted in the palliative treatment of bone metastasis with MRgFU. They noted that 21 % (46/224) of the patients with bone tumours that had received USgFUS had suffered adverse events, the most common being skin burns, fractures and nerve injuries (p = 0.0003). However, researchers attributed this to the location of the disease and the vulnerability of sensitive structures near the region of interest. More research is needed to determine the applicability of USgFUS to bone metastases.
6 Limitations and Risks Associated With HIFU
Some limitations associated with HIFU are related to the ability of various tissue types and organs to absorb acoustic energy. Acoustic energy cannot propagate through air- or gas-filled organs such as the bowel or lungs. Appropriate beam path planning and determination of an acoustic window is necessary in order to visualize the way in which acoustic energy will reach targeted tissues without suffering interference from other structures. Furthermore, patients can be anesthetized or given breath-hold devices so that organs do not move during treatment and alter the beam path [34], although anesthesia often increases the length of hospital stays [31]. Bone, cartilage, and other calcified tissues absorb large amounts of ultrasonic energy [31], thus appropriate thermal dose calculations must be made when studying the focal regions of targeted tissues for different patients [26].
One study developed a numerical model to conclusively demonstrate that due to convective cooling and acoustic streaming, the temperature buildup near large blood vessels can be smaller than that expected. Large blood vessels reduce the temperature at their boundaries and thus affect the lesion size and the volumetric shape of tissue affected by ultrasonic energy [35]. These factors must be taken into account when calculating expected results from thermal ablation.
As discussed in the clinical studies summarized earlier, patients are susceptible to certain side effects from HIFU treatment. A study conducted of patients who had undergone HIFU to bone tumours noted various side effects experienced as a result of the treatment including skin burns, local nerve injuries, fractures, infections, epiphyseal separation, alkaline phosphatase (ALP) elevation, hemoglobinuria or ruptures [33]. In a separate study by Li et al. [18], 12 patients were noted to have suffered from first-degree burns which faded within 2 weeks; two patients reported second-degree burns which faded without scarring within 4 weeks after treatment, and; three patients were without sensation in the limb affected with osteosarcoma during HIFU treatment, but regained feeling following treatment. In addition, some patients experienced short-lasting fevers.
7 Comparison to Other Ablative Treatment Modalities
High-intensity focussed ultrasound has apparent advantages over some of the commonly used treatment modalities for bone metastases. HIFU is not limited by cumulative effects or tumour-resistance as is external beam radiation therapy (EBRT). Although EBRT is the standard of care, it delivers ionizing radiation to a patient with inevitable cumulative dose effects. Some tumours are radio-resistant, which is why EBRT has a success rate of 70–80 % [36]. Radiation has also been shown to induce nausea and vomiting in some patients [2].
Surgical interventions have been used in patients; however, invasive methods put the patients at risk of developing infections and are limited in their application for bony metastases. Other ablative techniques aside from HIFU have advantages and disadvantages that closely reflect those of HIFU. In order to permit comparison, this section discusses clinical studies in which radiofrequency ablation, cryotherapy, laser-induced interstitial thermotherapy and microwave ablation have been used for pain palliation for bone metastases.
7.1 Radiofrequency Ablation
Radiofrequency ablation (RFA) is a minimally invasive ablative technique used to eliminate cancerous cells. In percutaneous RFA, a needle electrode is inserted into the tumour and high-frequency, alternating electrical currents are passed through the electrode which generates heat and destroys the cancerous cells at the region of interest. Needle electrodes can be single electrodes or hollow electrodes that contain multiple retractable electrodes for treatment [37]. Target temperatures are around 100 °C and ablations last between 5 and 15 min [38]. Water-cooling systems are sometimes added to needle electrodes and thermocouples are used to monitor temperatures adjacent to lesion sites. RFA is completed with the assistance of MRI, US, CT or other forms of guidance but depends on electrode insertion. Table 14.2 and the following discussion explain the results and significance of clinical studies performed to assess the use of RFA on bone metastases.
In a study conducted by Kashima et al. [39], internally-cooled electrodes were used and real-time CT fluoroscopy was used to place needle electrodes in patients. If the maximum tumour diameter was greater than 3 cm, cement was placed near the lesion site to prevent fractures. The technical success of this trial, defined by the correct placement of the needle electrode in the target tumour and successful completion of planned ablation, was 100 %. The 3-year survival rates and median survival lengths were low: 10 % and 17 months in the 12 patients with complete tumour ablation and 0 % and 6.5 months in 28 patients with incomplete tumour ablation (p < 0.04). Kashima et al. suggested that prognosis depends greatly on the number of bone metastasis sites as well as the stage of cancer. Many of these patients suffered from advanced cancer and 57 % of deaths of this patient population resulted from intrahepatic lesions. Transient nerve injury was only noted in one patient out of 40 (2.5 %) and this was improved after 1 week, however, metastases continued to invade the patient’s spinal cord. These researchers concluded that RFA is a safe therapeutic technique, but suggested that RFA is limited in its ability to ablate large tumour sizes and should perhaps be used as a part of a multidisciplinary approach. Callstrom et al. [40] agreed with this, suggesting that anti-osteoclast agents, bisphosphonates, chemotherapeutic agents or radiotherapy can have synergistic effects when used simultaneously with RFA.
In Goetz et al.’s multicenter study [38], researchers noted that one of the limitations of RFA is that the tip of the needle electrodes cannot spread out in osteoblastic metastases, thus metastases with an osteolytic component are best treated with this approach. Single ablations were performed on patients with lesions less than or equal to 3 cm in diameter, whereas multiple ablations were required for patients with lesions between 3 and 5 cm. For lesions greater than 5 cm, and the goal of treatment was to focus on the interface between bone and soft tissue. Opioid usage decreased at weeks 8 and 12 (p = 0.01), but this was not persistent at 24 weeks. While the RFA pain reduction results are significant, the use of opioids in patients prior to and during treatment suggests that other techniques could be helpful when used in conjunction with RFA treatment. Adverse events including second-degree burns at the electrode grounding pad, transient bowel and bladder incontinence and fracture of acetabulum after RFA at an acetubular lesion were noted in three patients. Another multicenter study [41] which used image-guided RFA of bony metastases also stated that patients with painful metastases in the sacrum or presacral region are limited in their options. Ablation of nerves near these areas must be avoided in order to prevent bowel or bladder incontinence.
Belfiore et al. [42] had selection criterion similar to the RFA trials above, and was used when radiotherapy and common therapeutic methods failed. In their study, nine lesions were treated with a single needle and another four with expandable electrodes. Imaging in 9 out of 12 patients showed large necrotic areas involving the tumour-bone interface, however, not all of these necrotic areas covered the entire osteolytic areas. Whereas two cases were successfully re-treated, three lesions greater than 3 cm in diameter at the humerus, scapula and iliac wing were re-treated at 1 month and did not show satisfactory tumour-bone ablation; RFA could not be used to ablate large lesions and tumour volume changes treatable were constrained by the capability of the RFA electrode. Additionally, in this study, a patient with sacral metastasis from rectal adenocarcinoma was further stabilized by cementoplasty. Toyota et al. [43] also demonstrated satisfactory pain reduction when combining cementoplasty and RFA in 17 patients.
Grönemeyer et al. demonstrated similar results [44]. Neurological function in patients measured on the Frankel scale was maintained in nine patients and improved in one patient. Despite this, four patients needed vertebroplasties and 3–5.5 mL of polymethyl methacrylate was used in these procedures. As well, researchers concluded that RFA treatments needed to be re-started if irritation occurred during heating near the spinal cord or sympathetic nerves. Thanos et al. [45] had no complications in their study; however multi-tined electrodes were used for all lesions. Seven-array, 2–3 cm multitined electrodes were used for lesions smaller than 3 cm and nine-array multitined electrodes were used for larger lesions. Larger lesions required oncologists to either treat with an increased number of electrodes and/or longer periods of time of energy deposition, both of which can result in longer treatment times.
Radiofrequency ablation, similar to HIFU, is valuable in its ability to significantly reduce pain sensations in patients in early and late-stage disease, post-treatment. Treatment with RFA is a repeatable procedure that also allows for tissue diagnosis during treatment [46]. This type of ablation usually reaches tumour sites a few millimeters around the needle electrode, but is not feasible in reaching distal areas [47]. It is limited in the tumour volume it can ablate; microscopic tumours and very large lesions are both difficult to treat with this modality [37]. Oncologists and researchers have created strict guidelines for patient selection of this treatment, requiring that patients undergoing RFA treatment have a pain sensation of greater than or equal to 4 on a 0–10 scale, have one or two focal sites, cannot have osteoblastic metastases, and are usually non-responders to chemotherapy and radiation therapy [38, 44, 45]. Treatment with RFA should not be used if lesions are located within 1 cm of major nerves, the spinal cord, bowel, or bladder [41]. This technique has been generally used for pain palliation in conjunction with vertebroplasties and cementoplasties to further strengthen patient skeletons, and is mainly useful for pain relief after traditional standards of care have not been useful.
7.2 Cryotherapy
One of the first uses of cryotherapy for bone tumours was in conjunction with orthopedic surgery to achieve minimal loss of bone and function [48]. Cryotherapy for bone metastases involves the use of a hollow metal probe that is placed through the skin to reach the tumour site. Pressurized gas in the probe is rapidly expanded resulting in cooling to temperatures around −100 °C within a few seconds. Freeze-thaw-freeze cycles are used to ablate tumours at such low temperatures. The frozen area is called an ice ball, and complete cell death can occur within about 3 mm internally to the ice ball margin [41]. Cellular necrosis is said to occur through a variety of possible mechanisms including the formation of intracellular ice crystals, membrane disruption, vasculature failure, protein denaturation, and changes in electrolyte concentration. Thawing further allows ice crystals to combine and disrupt cellular integrity, leading to cell death [48]. Multiple probes can be placed in a parallel arrangement at the tumour periphery in order to completely cover the tissue-bone interface in the case of bone metastases, but this usually increases the procedural time. Cryoablation is best performed with a well-insulated probe with a diameter of 11–17 gauge, and recently developed probes contain argon gas for freezing and helium gas for thawing [41]. Saline is sometimes used during treatments in order to prevent skin freezing. Care must be taken to minimize destruction of the bone cortex and periosteum. The following representative studies below used cryotherapy to treat bone metastases.
Tuncali et al. [49] achieved 89 % pain palliation and reported that cryoablation near sensitive structures such as major blood vessels is feasible and must be completed carefully in order to prevent adverse events. In only two patients, cryoablation of spinal and paraspinal metastases caused transient lower extremity tingling, numbness and weakness, which spontaneously resolved within 1 week. Some sensory deficits were noted after two presacral tumour sites were treated and these deficits were attributed to ablation of the sacral plexus branches. The patient in that study who received surgical placement of intramedullary rods was required to do so in order to stabilize bone and prevent fracture, post-treatment. Researchers also noted that MRI guidance was more useful than CT guidance because in CT images both tumour and ice balls are typically hypodense and not easily distinguishable. Guidance with MRI was also claimed to be more useful than ultrasound guidance because ultrasonic images cannot detect the entire circumference of the ice ball in one view, as can MRI. The report by Callstrom et al. [50] discussed their selection criteria and stated that patients chosen for treatment were required to have a 4 or greater on a BPI scale of 0–10 and be non-responders to conventional therapies. Pain palliation was successful, as seen in Table 14.3, and the eight patients who were prescribed narcotics prior to treatment noted a reduction in medication after cryotherapy. A direct correlation was noted between the number of probes and the size of the lesion; a mean of 2.8 ± 1.6 probes were used per treatment the larger the lesion, the greater number of probes used. Mean treatment time was 139 ± 53 min and with CT-guidance, treatment time was 185 ± 56 min. Callstrom et al. discussed that while the mean treatment time was 46 min longer in order to set up CT-guidance, CT images can be useful in showing the ice ball region and low-attenuating necrotic tissue (Fig. 14.5).
13-gauge cryotherapy needle with ice ball at the end [49]
A final study on cryotherapy compared different forms of treatment for renal cell carcinoma with bone metastases. Kollender et al. [51] compared 29 cases of wide surgical excision, 25 cases of marginal excision and adjunctive cryotherapy using liquid nitrogen, and two cases of amputation. In treated patients, 91 % had significant pain relief and no difference in pain control, and function was noted in those with wide surgical excision versus those with marginal excision and cryotherapy. However, four lesions recurred; three within the lesions treated with marginal excision and cryosurgery and only one from a metastatic site treated with wide excision. Despite this, it was stated that cryotherapy is advantageous around weight-bearing joints as joint surfaces are preserved after treatment.
In general, ice balls created during cryotherapy are visible as low-attenuation regions in CT and MR images. Cryotherapy can treat lesions with larger diameters in a single session, such as 8 cm diameter lesions [41], relative to the small diameters treatable by RFA. Radio-frequency ablation and cryotherapy, similar to HIFU, are minimally invasive techniques that are not limited by cumulative dose effects, are useful in pain palliation, and should be considered in combination with other modalities.
7.3 Laser-Induced Interstitial Thermotherapy, Microwave Ablation, Alcohol Ablation
In laser-induced interstitial thermotherapy (LITT), the frequently used laser is Nd: YAG (neo-dymium yttrium aluminum garnet), with a wavelength of 1,064-nm, or laser diodes are used with wavelengths of 980 or 805 nm [52]. Necrosis occurs when heating is induced by a coherent, monochromatic Nd: YAG generated light that passes through a fiber-optic tip at the tumour site [53]. Cooled applicators are used as in RFA to prevent carbonization at the probe tip and to expand the diameter of the necrotic lesion [53]. Lasers operate at a power of 5–10 W for 10–15 min [54]. A study by Papini et al. used percutaneous laser ablation to treat two patients with unresectable bony metastases from thyroid carcinoma. One case had tumour 90 % ablated after two sessions of treatment and the other 80 % ablated after two sessions. Increase in performance status, tumour volume decrease 3 months post-treatment, and reduction in analgesics were all noted. Laser-induced interstitial thermotherapy works similarly to other ablative techniques and must be monitored for temperature control, tissue impedance, applicator positioning, and in order to minimize damage to nearby structures [52].
Microwave ablation is another form of percutaneous thermal ablation which uses electromagnetic waves with a frequency of around 1 GHz to create oscillations in water molecules [55]. As the water molecules align their dipole moments with an alternating electric field, tissue temperature rises, resulting in necrosis. Microwave ablation is advantageous over RF ablation because it not does require the use of grounding pads and has higher ablation temperatures and shorter treatment times [55]. Moreover, unwanted heating in major structures with high impedance is reduced because electrical currents are not used.
Percutaneous ethanol ablation is another method of percutaneous tumour ablation whereby needles are inserted into tumours and alcoholization causes dehydration and tissue necrosis. Vascular thrombosis and tissue ischemia also result which contribute to necrosis, and it has been suggested that this can also achieve pain palliation for bone metastases. Nonetheless, alcohol ablation is an unpredictable form of ablation due to a random distribution of ethanol when injected [56].
8 Future Directions
High-intensity focussed ultrasound and other thermally ablative techniques used to treat bony metastases represent innovative alternatives to the treatment of skeletal metastases. These techniques have been used primarily in palliative settings to control pain and also attempt to reduce the onset of further tumour growth in patients. Research continues in these fields in the hopes of enhancing both the technological and clinical aspects of thermally ablative modalities.
8.1 Technological Improvements
HIFU technology is being refined in its real-time imaging capability for anatomical guidance and thermometry, transducer design, and modes of energy transfer [3]. Adequate treatment monitoring continues to be developed in the areas of thermometry, elastography, and radiation force imaging [14]. Acoustic radiation force impulse (ARFI) imaging provides further information on the mechanical properties of tissue, more so than that provided by US-guidance [14], and may be useful for monitoring HIFU treatments. This modality functions because of the energy deposition in soft tissue when acoustic energy passes through it. This energy creates a transfer of momentum during wave reflection that acts in the direction of ultrasound propagation. The displacement of the soft tissue is known as the radiation force, which presents information to the user about tissue types [17]. In vitro animal studies on elastography have been completed and researchers have concluded that elastographic depictions of lesions are useful in studying types of tissue damage and the treated volume [57]. Further research is needed, incorporating both thermometry and elastography measurements in image-guidance.
Precise positioning of transducers and applicator probes is also required in order to adequately target the region of interest. Guidance with CT is often used in ablative techniques to guide percutaneous injection of needle electrodes and probes. Probes are continually becoming smaller and fiber-optic tips are on the order of a few hundred micrometers and are thus difficult to detect with imaging. Fiber stoppers can be used, but technological improvement in this field are currently underway in order to develop better forms of guidance for probe insertion [52]. Transducer technology is being improved upon and a more recently developed transducer type is known as a CMUT, a capacitive micromachined ultrasonic transducer. This type of transducer is created using silicon micro-machinery and changes in capacitance are what create signal transduction and were discussed in a study using MRgFUS, and appeared to allow for fabrication flexibility, diminished acoustic beam loss, and efficient beam transmission. Heating from CMUT’s was monitored using MRI and heated a HIFU phantom by 19 °C in 5 mins. This transducer type is relatively new and is being tested on surfaces such as gel phantoms before being tried in clinical settings [58]. Phased-array ultrasonics are also useful in treating different regions of total tumour volumes without having to re-position the transducer, and this can reduce total treatment times. Similarly, transducers with annular arrays and cylindrical 2D arrays have been developed for experimental purposes to further study the alteration of the focal point during treatment without moving the transducer itself [59]. In addition, an in vitro and animal study was completed in 2010 to assess the use of a robotic system to setup the ultrasonic transducer to target a focal site [60]. New technologies still need to be tested in clinical settings and devices must gain approval before being introduced for therapeutic use.
8.2 Clinical Research
In theory, HIFU treatment of bone metastases promotes prolonged survival by reducing structural damage to the bone cortex and only ablating up until the tissue-bone interface. This minimizes bone destruction in comparison to widely invasive techniques such as surgery, and with minimal damage to the bone surface, HIFU allows for faster bone healing after treatment [36]. In spite of this, long-term survival rates in the studies discussed have been low and are in large part due to the advanced stages of cancer that patients are suffering from. Clinically, ablative techniques are being developed to determine ways to treat multiple metastatic sites but should also find better use as a primary treatment for tumours, minimizing surgery and radiation needed. Considerable work is also being done to determine how the effect of HIFU ablation can be enhanced when used with adjuvant radiation therapy, chemotherapy or cementoplasty [61–71]. The injection of microbubbles is also being studied as a novel way to augment the success of tumour ablation by increasing heating at the focal point [59].
Presently, HIFU, radiofrequency ablation, cryotherapy and other ablative modalities are useful in treating skeletal metastases, but are limited by technological and clinical constraints. These therapies are as useful as the ability of transducers and probes to cause significant thermal effects on tumours and can only be used with adequate guidance. As most of these bony metastatic sites are close to nervous system structures and important vasculature, serious negative repercussions can result if ablative techniques are unsuccessful. Further investigation is needed to deduce whether thermal ablation for the pain palliation of bone metastases produces adequate results on its own or concurrently with more standard forms of care.
References
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMra030831. Accessed 30 July 2012
Saghal A, Chow E, Merrick J et al (2010) Bone and brain metastases: advances in research and treatment. Nova Science Publishers, New York
Zhou YF (2011) High intensity focused ultrasound in clinical tumor ablation. World J Clin Oncol 2(1):8–27. doi:10.5306/wjco.v2.i1.8
Beerlage HP (1999) High-Intensity Focused Ultrasound (HIFU) followed after one to two weeks by radical retropubic prostatectomy: results of a prospective study. J Urol. Doi: 10.1016/S0022-5347(05)68361–9
Jagannathan J, Sanghvi NT, Crum LA et al (2009) High-Intensity focused ultrasound surgery of the brain: part 1-A historical perspective with modern applications. Neurosurgery 64(2):201–210. doi:10.1227/01.NEU.0000336766.18197.8E
Wu F, Wang ZB, Chen WZ et al (2004) Extracorporeal high intensity focused ultrasound ablation in the treatment of 1038 patients with solid carcinomas in China: an overview. Ultrason Sonochem 11(3–4):149–154. doi:10.1016/j.ultsonch.2004.01.011
Zhu H, Zhou K, Zhang L et al (2008) High intensity focused ultrasound (HIFU) therapy for local treatment of hepatocellular carcinoma: role of partial rib resection. Eur J Radiol 72(1):160–166. doi:10.1016/j.ejrad.2008.07.003
Wu F, Wang ZB, Zhu H et al (2004) Feasibility of US-guided high-intensity focused ultrasound treatment in patients with advanced pancreatic cancer: initial experience. Radiology 236(3):1034–1040. doi:10.1148/radiol.2362041105
Zhang L, Zhu H, Jin C et al (2008) High-intensity focused ultrasound (HIFU): effective and safe therapy for hepatocellular carcinoma adjacent to major hepatic veins. Eur Soc Radiol 19(2):437–445. doi:10.1007/s00330-008-1137-0
Jin X, Xu Y, Wang LV et al (2004) Imaging of high-intensity focused ultrasound-induced lesions in soft biological tissue using thermoacoustic tomography. Med Phys 32(1):5–11. doi:10.1118/1.1829403
Dogra VS, Zhang M, Bhatt S (2009) High-intensity focused ultrasound (HIFU) therapy applications. MD Consult 4(3):307–321. doi:10.1016/j.cult.2009.10.005
Wu F, Chen WZ, Bai J et al (2002) Tumor vessel destruction resulting from high-intensity focused ultrasound in patients with solid malignancies. Ultrasound Med Biol 28(4):535–542. doi:10.1016/S0301-5629(01)00515-4
Illing R, Emberton M (2006) Sonablate-500: transrectal high-intensity focused ultrasound for the treatment of prostate cancer. http://www.focus-surgery.com/Documents/Future%20Drugs%20Article%202006.pdf Accessed 30 July 2012
Hwang JH Current status of HIFU therapy for treatment of benign and malignant tumors of the abdomen, pelvis, and bone. http://www.aapm.org/meetings/amos2/pdf/59-17287-39310-375.pdf. Accessed 30 July 2012
Foster RS, Bihrle R, Sanghvi N et al (1994) High-intensity focused ultrasound for the treatment of benign prostatic hypertrophy. Sem Urol. http://www.focus-surgery.com/Documents/High-Intensity%20Ultrasound%20for%20the%20Treatment%20of%20BPH.pdf. Accessed 30 July 2012
Halpern EJ (2005) High-intensity focused ultrasound ablation: will image-guided therapy replace conventional surgery? Radiology 235(2):659–667. doi:10.1148/radiol.2352030916
Khokhlova T, Hwang J (2011) HIFU for palliative treatment of pancreatic cancer. J Gastrointest Oncol 2(3):175–184. doi:10.3978/j.issn.2078-6891.2011.033
Li C, Zhang W, Fan W et al (2010) Noninvasive treatment of malignant bone tumors using high-intensity focused ultrasound. Cancer 116(16):3934–3942. doi:10.1002/cncr.25192
(2012) Bone metastasis. Novartis Oncol. http://www.novartisoncology.com/files/cancer-resource-center/what-is-cancer/Bone-Metastasis-english.pdf. Accessed 30 July 2012
(2012) Bone metastasis. University of Michigan Comprehensive Cancer Center. http://www.cancer.med.umich.edu/cancertreat/tissue_bone/bonesymptoms.shtml. Accessed 30 July 2012
Mirjana R, Kovac V (2008) Malignant spinal cord compression. Radiol Oncol 42(1):23–31. doi:10.2478/v10019-007-0035-4
Liberman B, Gianfelice D, Inbar Y et al (2008) Pain palliation in patients with bone metastases using MR-guided focused ultrasound surgery: a multicenter study. Ann Surg Oncol 16(1):140–146. doi:10.1245/s10434-008-0011-2
Gianfelice D, Gupta C, Kucharczyk W et al (2008) Palliative treatment of painful bone metastases with MR imaging-guided focused ultrasound. Radiology 249(1):355–363. doi:10.1148/radiol.2491071523
(2012) Local treatments for bone metastases. Am Cancer Soc http://www.cancer.org/treatment/understandingyourdiagnosis/bonemetastasis/bone-metastasis-treating-local-treatments. Accessed 30 July 2012
Durr HR, Muller PE, Lenz T et al (2002) Surgical treatment of bone metastases in patients with breast cancer. Clin Orthop Relat Res 396:191–196
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10(6):787–800. doi:10.1016/j.bbr.2011.03.031
Grull H, Langereis S (2012) Hyperthermia-triggered drug delivery from temperature-sensitive liposomes using MRI-guided high intensity focused ultrasound. J Control Release 161(2):317–327. doi:10.1016/j.jconrel.2012.04.041
Huber PE, Jenne JW, Raster R et al (2001) A new noninvasive approach in breast cancer therapy using magnetic resonance imaging-guided focused ultrasound surgery. Cancer Res 61:8441–8447
(2012) MR guided focused ultrasound: what is it? InSightec. http://www.insightec.com/MRgFUS-Technology.html. Accessed 30 July 2012
Liberman L, Bracero N (2005) Breast MRI: diagnosis and intervention. Springer, New York
Kopelman D, Papa M (2007) Magnetic resonance-guided focused ultrasound surgery for the noninvasive curative ablation of tumors and palliative treatments: a review. Ann Surg Oncol 14(5):1540–1550. doi:10.1245/s10434-006-9326z
Fan CH, Liu HL, Huang CY et al (2012) Detection of intracerebral hemorrhage and transient blood-supply shortage in focused-ultrasound-induced blood-brain barrier disruption by ultrasound imaging. Ultrasound Med Biol 38(8):1372–1382. doi:10.1016/j.ultrasmedbio.2012.03.013
Yu T, Luo J (2011) Adverse events of extracorporeal ultrasound-guided high intensity focused ultrasound therapy. PloS ONE 6(12). Doi: 10.1371/journal.pone.0026110
Kennedy JE, Harr GR, Cranston D (2003) High intensity focused ultrasound: surgery of the future? Br Ins Radiol 76:590–599. doi:10.1259/bjr/17150274
Solovchuk M, Sheu TWH, Thiriet M et al Effect of acoustic streaming on tissue heating due to high-intensity focused ultrasound. http://arxiv.org/ftp/arxiv/papers/1111/1111.2908.pdf. Accessed 30 July 2012
(2012) Bone metastases. Focused ultrasound foundation. http://www.fusfoundation.org/Bone-Mets-Pain/bone-metastases. Accessed 30 July 2012
(2012) Radiofrequency ablation of liver tumors. Radiology Info. http://www.radiologyinfo.org/en/info.cfm?pg=rfaliver. Accessed 30 July 2012
Goetz MP, Callstrom MR, Charboneau W et al (2004) Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol 22(2):300–306. doi:10.1200/JCO.2004.03.097
Kashima M, Yamakado K, Takaki H et al (2010) Radiofrequency ablation for the treatment of bone metastases from hepatocellular carcinoma. Am J Roentgenol 194(2):536–541. doi:10.2214/AJR.09.2975
Callstrom MR, Charboneau JW, Goetz MP (2002) Painful metastases involving bone: feasibility of percutaneous CT- and US-guided radio-frequency ablation. Radiology 224:87–97. doi:10.1148/radiol.2241011613
Callstrom MR, Charboneau W (2007) Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Int Radiol 10(2):120–131. doi:10.1053/j.tvir.2007.09.003
Belfiore G, Tedeschi E, Ronza FM et al (2008) Radiofrequency ablation of bone metastases induces long-lasting palliation in patients with untreatable cancer. Singapore Med J 49(7):565–570
Toyota N, Naito A, Kakizawa H et al (2005) Radiofrequency ablation therapy combined with cementoplasty for painful bone metastases: initial experience. Cardiovasc Interv Radiol 28(5):578–583. doi:10.1007/s00270-004-0208-0
Gronemeyer DHW, Schirp S, Gevargez A (2002) Image-guided radiofrequency ablation of spinal tumors: preliminary experience with an expandable array electrode. Cancer J 8(1):33–39
Thanos L, Mylona S, Galani P et al (2008) Radiofrequency ablation of osseous metastases for the palliation of pain. Skeletal Radiol 37:189–194. doi:10.1007/s00256-007-0404-5
Maciunas RJ (1998) Advanced techniques in central nervous system metastases. The American Association of Neurological. Surgeons, Illinois
Gray L (2012) Single-session ablation relieves misery of cancer that has spread to the bones. University of Washington. http://www.washington.edu/news/2012/04/02/single-session-ablation-relieves-misery-of-cancer-that-has-spread-to-the-bones/. Accessed 30 July 2012
Bickels J, Meller I, Malawer M (2001) The biology and role of cryosurgery in the treatment of bone tumors. In: Musculoskeletal cancer surgery, 1st edn. Kluwer Academic, New York
Tuncali K, Morrison PR, Winalski CS et al (2007) MRI-guided percutaneous cryotherapy for soft tissue and bone metastases: initial experience. Am J Roentgenol 189(1):232–239. doi:10.2214/AJR.06.0588
Callstrom MR, Atwell TD, Charboneau JW et al (2006) Painful metastases involving bone: percutaneous image-guided cryoablation- prospective trial interim analysis. Radiology 241:572–580. doi:10.1148/radiol.2412051247
Kollender Y, Bickels J, Price WM et al (2000) Metastatic renal cell carcinoma of bone: indications and technique of surgical intervention. J Urol 164:1505–1508
Groenemeyer DHW, Schirp S, Gervargez A (2002) Image-guided percutaneous thermal ablation of bone tumors. Acad Radiol 9:467–477
Gebauer B, Tunn PU (2006) Thermal ablation in bone tumors. Cancer Res 167:135–146
Papini E, Bizzarri G, Baroli A, et al Percutaneous laser ablation of unresectable bone metastases from poorly differentiated thyroid carcinoma. Hormones http://www.hormones.gr/445/article/article.html. Accessed 30 July 2012
Boss A, Dupuy D, Pereira PL (2008) Microwave ablation. Med Radiol 21–28:S69–S83. doi:10.1007/978-3-540-68250-9_3
Gangi A, Buy X (2010) Percutaneous bone tumor management. Semin Int Radiol 27(2):124–236. doi:10.1055/s-0030-1253511
Kallel F, Stafford RJ, Price RE (1999) The feasibility of elastographic visualization of HIFU-induced thermal lesions in soft tissues. Ultrasound Med Biol 25(4):641–647. doi:10.1016/S0301-5269(98)00184-7
Wong SH, Watkins RD, Kupnik M et al. (2008) Progress in development of HIFU CMUTs for use under MR-guidance. http://www-kyg.stanford.edu/khuriyakub/opencms/Downloads/08_Wong_2_ISTU.pdf. Accessed 30 July 2012
Illing R, Emberton M (2006) Sonablate-500: transrectal high-intensity focused ultrasound for the treatment of prostate cancer. Future Drugs Ltd. doi:10.1586/17434440.3.6.717
Krafft AJ, Jenne JW, Maier F et al (2010) A long arm for ultrasound: a combined robotic focused ultrasound setup for magnetic resonance-guided focused ultrasound surgery. Int J Med Phys Res Prac 37(5):2380–2394. doi:10.1118/1.3377777
Hynynen K, Freund WR, Cline HE et al (1996) A clinical, noninvasive, MR-Imaging-monitored ultrasound surgery method. Radiographics 16:185–195
Lim LC, Rosenthal MA, Maartens N et al (2004) Management of brain metastases. Int Med J 34(5):270–278. doi:10.1111/j.1444-0903.2004.00579.x
Arnone P, Chen W, Orsi F et al (2010) High intensity focused ultrasound ablation: a new therapeutic option for solid tumors. Health Reference Center. http://go.galegroup.com.ezproxy.library.ubc.ca/ps/i.do?action=interpret&id=GALE|A250737554&v=2.1&u=ubcolumbia&it=r&p=HRCA&sw=w&authCount=1. Accessed 30 July 2012
Orgera G, Curigliano G, Krokidis M et al (2010) High-intensity focused ultrasound effect in breast cancer nodal metastasis. Cardiovasc Int Radiol 33(2):447–449. doi:10.1007/s00270-010-9824-z
Uchida T, Nakano M, Hongo S et al (2011) High-intensity focused ultrasound therapy for prostate cancer. Int J Urol 19(3):187–201. doi:10.1111/j.1442-2042.2011.02936.x
(2012) High intensity focused ultrasound (HIFU) for the treatment of prostate cancer. community connect medical policy. http://www.cchmedicalpolicies.com/medicalpolicies/policies/mp_pw_a053507.htm. Accessed 30 July 2012
Hynynen K, Pomeroy O, Smith DN et al (2001) MR imaging-guided focused ultrasound surgery of fibroadenomas in the breast: a feasibility study. Radiology 219(1):176–185
Suh JH, Chao ST, Vogelbaum MA (2009) Management of brain metastases. Current Neurol Neurosci Rep 9:223–230
Wu F, Wang Z-B, Chen W-Z, Zhu H (2005) Non-invasive ablation of high intensity focused ultrasound for the treatment of patients with malignant bone tumors. J Bone Joint Surg Br 87-B(4)
Rabkin BA, Zderic V, Vaezy S (2005) HIFU-induced hyperecho in ultrasound images, cavitation activity and thermal behaviour. AIP Conf Proc 754:43–46. doi:10.1063/1.1901596
Du ZH, Zang J, Tang ZD et al (2010) Experts’ agreement on therapy for bone metastases. Orthop Surg 2(4):241–253. doi:10.111/j.1757-7861.2010.00095.x
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Halani, S., Coccagna, J., Chow, E., Hynynen, K., Czarnota, G.J. (2014). High-Intensity Focussed Ultrasound and Radio-Frequency Ablation for Bone Metastasis Treatment. In: Vassiliou, V., Chow, E., Kardamakis, D. (eds) Bone Metastases. Cancer Metastasis - Biology and Treatment, vol 21. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7569-5_14
Download citation
DOI: https://doi.org/10.1007/978-94-007-7569-5_14
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7568-8
Online ISBN: 978-94-007-7569-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)