Abstract
Ewing’s sarcoma family of tumors (ESFT) is a malignant tumor of bone and soft tissue in children and adolescents that is characterized by molecular alterations that most commonly involve the EWS gene on chromosome 22. It is an aggressive tumor, with metastases present at diagnosis in 20–25% of cases. Modern treatment regimens for localized disease have resulted in significant improvement in survival. However, the presence of metastasis is associated with mortality in 70–80% of patients. New insights into the pathogenesis and proliferative mechanisms of human cancers have led to the identification of a number of proteins acting as messenger molecules and modulators of tumor growth. Targeting these molecules in ESFT has the potential effect of controlling tumor growth. This chapter summarizes the current research on molecular pathogenesis, proliferation pathways and new investigational pharmacologic agents that are under development in the race for the cure of this malignancy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vascular Endothelial Growth Factor
- Proliferation Pathway
- Altered Copy Number
- Alveolar Rhabdomyosarcoma
- High Vascular Endothelial Growth Factor Expression
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Ewing’s sarcoma family of tumors (ESFT) is an aggressive malignancy that affects the growing bones and soft tissues of children and young adults. It is regarded as the second most common sarcoma of bone and commonly affects children in the second decade of life. It constitutes about 3% of all pediatric malignancies and 40% of pediatric bone cancers. The disease, which is predominantly seen in Caucasians and is rare in other races, is not predisposed to by any environmental or familial factor, and does not have any known association with any syndrome or genetic disease. The median age at diagnosis is 15 years and approximately three cases occur each year per one million Caucasian patients younger than 21 years (Paulussen et al. 2001). Although ESFT is a primary bone cancer, a substantial proportion of these tumors arise from extraskeletal sites. Patients with extraskeletal ESFT have a higher mean age, but also have a bimodal distribution, being more commonly found in those older than 35 years and less than 5 years compared with skeletal tumors (Applebaum et al. 2011).
ESFT presents with pain and later a swelling from a localized mass that appears on imaging studies as a destructive diaphyseal bony lesion that also extends to the soft tissues. The pelvic bones, long extremities and ribs are, in decreasing frequency, the most commonly affected sites. However this tumor can arise in any bone or soft tissue location in the human body, including deep seated visceral organs. Patients may also present with nonspecific signs because of tumor location or with general signs of inflammation such as fever, anemia and leukocytosis. No blood, serum, or urine test can specifically identify ESFT. Serum and urine catecholamine levels are always normal (Bernstein et al. 2006).
Patients may also present with metastasis that can occur in 20–25% of cases before diagnosis. ESFT metastasizes most commonly to the lungs, bone and bone marrow. The presence of metastasis is the most important prognostic factor and patients with metastatic tumor have poor survival. About 30–40% of those with localized disease and 80% with metastatic disease die as result of disease progression (Bacci et al. 2007).
Molecular Insights into Tumor Pathogenesis
The term “Ewing’s sarcoma family of tumors” is coined to describe closely related group of tumors that were previously considered separate entities: Ewing’s sarcoma, peripheral primitive neuroectodermal tumor and Askin tumor. These tumors exhibit similar histologic, immunophenotypic and molecular signatures and hence grouped as one family. Histologically they are characterized by a “small round blue cell” morphology (Fig. 21.1) that may also reveal limited neural and/or epithelial differentiation. The cell of origin is not definitively known but is probably a primitive mesenchymal cell or neuroectodermal stem cell that has retained some ability for multi-lineage differentiation. Recent evidence has suggested that the cell of origin may actually be a bone marrow associated mesenchymal stem cell (MSC) that undergoes transformation from a spindle cell morphology to a rounded cell that is characteristic of ESFT (Riggi et al. 2005; Lin et al. 2011).
The diagnosis of Ewing’s sarcoma family tumor is suspected from the presence of the characteristic small round cell morphology on conventional H&E stains and is confirmed by the diffuse membranous immunohistochemical positivity for CD99. Molecular methods that detect the presence of EWS-FLI1 fusion gene by reverse transcription polymerase chain reaction (RT-PCR) are also important in confirming the diagnosis
The primary genetic event that drives this cellular malignant transformation is a chromosomal translocation that involves EWS, a gene located in chromosome 22q12 (Riggi et al. 2008). EWS is fused to the DNA binding domain (DBD) of one of five ETS family transcription factors, that include FLI1, ERG, ETV1, ETV4, and FEV (Arvand and Denny 2001). Ewing’s sarcoma family tumors (ESFT) are commonly associated with the chromosomal translocation t (11;22) (q24;q12) that generates the EWS-FLI1 fusion gene in >85% of cases and EWS-ERG in 5–10% of cases. In the remainder, EWS is fused to other ETS members such as ETV1, ETV4, or E1AF (Giovannini et al. 1994). The evidence, that the induction of EWS-FLI1 and other chimeric EWS/ETS proteins in mesenchymal progenitor cells is the primary initiation genetic event in the tumorigenicity of ESFT, comes from in vitro studies on MSC lines. There was a change of morphology and immunophenotype of the MSC (positive for CD10, CD13 and vimentin) to a rounded cells that have the morphologic and immunophenotypic features of ESFT with upregulation of CD54, CD99, CD117 and CD271. The malignant transformation of the MSC towards ESFT is accompanied by ability of the cells to have invasive properties (Miyagawa et al. 2008).
EWS-FLI1 fusion protein is a transcription factor that can bind DNA and cause altered expression of down-stream genes. EWS-FLI1 interacts with the transcription factor CBP and results in promoter interactions with the AP-1 (fos/jun) transcription complex and is thus important for transcriptional regulation of several genes that mainly influence the production of cell cycle proteins, growth factors and apoptosis molecules. There is up-regulation of MYC, IGF1, GLI1, TOPK, NKX2.2, DAX1, EAT-2, EZH2, MK-STYX, PLD2, MMP-3, FRINGE, ID2, and CCND1 along with repression of TGFBR2 and CDKN1A (Jedlicka 2010). It has also been suggested that other mutations may occur in conjunction with EWS-FLI1 oncogenetic transformation in a cooperative mechanism that allows for cell growth and proliferation (Lin et al. 2011). Comparative genomic hybridization studies have revealed the presence of altered copy number of numerous other genes including gains and deletions (Toomey et al. 2010). Gene expression studies have also yielded valuable information regarding gene signatures and their differences in localized versus metastatic disease (Pinto et al. 2011).
Pathologic Diagnosis
Details of tumor pathogenesis and biologic characteristics have led to valuable information that is also used in the pathologic diagnosis of this tumor. Currently, the diagnosis of ESFT is achieved through combination of histology and results of ancillary tests. The histology is that of an undifferentiated cellular tumor that may have overlapping features with other small round cell tumors, particularly solid alveolar rhabdomyosarcoma, lymphoblastic lymphoma or undifferentiated neuroblastoma. The tumor is composed of diffuse sheets of small cells with central nuclei and scant cytoplasm. The nuclei are round to oval with smooth contours and inconspicuous nucleoli and exhibit a low mitotic rate. The small amount of cytoplasm may appear clear or vacuolated due to accumulation of glycogen that can be identified with the periodic acid shift (PAS) special stain. Immunohistochemical tests are widely used to arrive at the diagnosis and help exclude other tumors in the differential diagnosis. Immunohistochemical stain with antibodies against CD99 reveal a diffuse membranous staining that is characteristic for ESFT (Fig. 21.1). An immunohistochemical test for Fli1, the partner in EWS-FLI1 translocation, can also be used in the diagnosis of ESFT and yields a nuclear staining pattern. Combination of histologic morphology and characteristic positive staining with PAS, CD99 and/or Fli1 is highly sensitive and specific for the diagnosis of ESFT (Pinto et al. 2011). Molecular testing to detect the characteristic chromosomal translocations is helpful to confirm the diagnosis. These molecular translocations can be detected by RT-PCR on fresh, frozen or paraffin-embedded formalin-fixed tissue (Fig. 21.1). The EWS (also called EWSR1) gene can also be detected by fluorescent in situ hybridization using specific probes (Lewis et al. 2007). In less than 5% of cases, characteristic EWS-ETS translocations are not identified and hence, gene sequencing of the EWS gene may confirm the diagnosis if necessary.
Pathobiologic Proliferation Pathways
EWS-FLI-1 fusion and other dysregulated genes lead to over-expression of several cellular signaling pathways that mediate cellular proliferation and tumor growth. Insulin-growth factor pathway and its members, IGF1 and IGFR1 have been found to be over-expressed in ESFT cell lines and tissues (Scotlandi et al. 1996). This may explain the surge in ESFT incidence during the pubertal growth spurt. The ubiquitous PI3K-AKT pathway and its members are protein kinases that are also identified in ESFT, both in vivo and in vitro studies (Ahmed et al. 2011). NF-Kappa B is a transcription factor that regulates genes involved in inflammation and cell proliferation and dysregulation of NF-kappa B has been identified in ESFT cell lines (Ahmed et al. 2011). Similarly the vascular endothelial growth factor (VEGF) and its family of proteins play a role in tumor angiogenesis and proliferation and have been identified in ESFT cell lines and tissues (Nagano et al. 2010). The expression of these molecules and several other proliferation pathway members can be detected on human tumor tissues using conventional immunohistochemical techniques (Fig. 21.2).
CD99 is upregulated during the cellular malignant transformation of ESFT and is commonly used as an immunohistochemical marker for confirming the diagnosis of ESFT as shown above (Fig. 21.1). CD99 (also known as MIC2, and recognized by the antibodies 12E7, HBA71, and O13) is a 32-kDa integral membrane glycoprotein that plays a key role in several biological processes, including cell adhesion, migration, and apoptosis, maintenance of cellular morphology and regulation of intracellular membrane protein trafficking. However the function of CD99 in ESFT is currently unknown. There is some evidence that CD99 is required for ESFT transformation (Rocchi et al. 2010). CD99 can affect ESFT cell growth, tumorigenesis and metastatic ability and may prevent neural differentiation of tumor cells. CD99 may affect the modulation of several intracellular pathways, including PI3K/Akt and RAS/MAPK which are activated by EWS-FLI1. CD99 seems to inhibit the activation of ERK1/2 and thus counter-act the effect of EWS-FLI1 on MAPK pathway activation. There is evidence that CD99 knockdown inhibits Akt while increases ERK1/2 phosphorylation, which in turn seems to modulate the neural differentiation of ESFT tumor cells.
Several other related pathways and molecules such as C-kit, caveolin-1, and E-cadherin are over-expressed and play an indirect role in tumor cell proliferation through their interaction with main proliferative pathways. Similarly, basic fibroblast growth factor and receptor molecules and platelet-derived growth factor receptors are over-expressed in ESFT. Furthermore, basic fibroblast growth factor may cause stimulation of EWS-FLI1 fusion protein activity (Girnita et al. 2000; Bozzi et al. 2007). Targeting these proteins and other proliferation pathways by small interfering RNAs and monoclonal antibodies is the subject of fervent research in attempts to discover new therapies for ESFT tumors that are resistant to conventional treatment (McAllister and Lessnick 2005).
Current Treatment Regimens
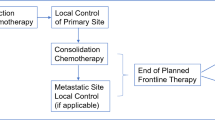
The current approach to treatment of Ewing’s sarcoma is a combination of chemotherapy, surgery and radiation. For localized disease, chemotherapy with compressed cycles of ifosfamide/ etoposide alternating with vincristine/ adriamycin/cyclophosphamide or VIDE (vincristine/ifosfamide/doxorubicin/etoposide) per the Euro-Ewing’s group, given prior to and post local control, is the standard of care. With this treatment regimen, the overall survival is approximately 70% (Ladenstein et al. 2010). Patients with metastatic disease have worse outcomes, though patients with isolated lung metastasis fare better, with overall survival ranging from 9 to 41%. Independent poor prognostic factors include presence of ≥ 2 bone metastases, primary tumor volume >200 ml, age older than 14, pulmonary metastasis and bone marrow metastasis (Ladenstein et al. 2010). The question of whether autologous transplant improves survival in patients with metastatic disease continues to be evaluated.
Novel Therapeutic Targets
Given the poor outcomes of patients with metastatic or high risk Ewing’s sarcoma, methods to improve outcomes have been the focus of extensive research. One area being explored is drug resistance and how to overcome it. Another large area of research, as alluded to previously, is targeted therapy. The targets of these therapies are some of the pathway members discussed previously that are over-expressed in ESFT. Several of these therapeutic targets are currently being evaluated in preclinical and/or early clinical trials (Table 21.1). Examples of such therapeutic targets and their applications in clinical trials are listed below.
Ewing’s Sarcoma-FLI1
Due to EWS-FLI1’s role in the pathogenesis of Ewing’s sarcoma there has been a lot of interest in targeting EWS-FLI1 itself, but unfortunately it has proven difficult to move these therapies from bench to bedside due to the pharmacokinetics of these targeting agents (Herrero-Martin et al. 2011). Extensive work has also been done looking at blocking downstream targets and to inhibiting binding of transcription proteins to EWS-FLI1. An example of downstream targeting work is that De Vito et al. (2011) performed on the miRNA expression in human mesenchymal stem cells and ESFT cell lines. This work demonstrated a difference in the miRNA signature and revealed a decrease in let-7a expression in ESFT cell lines compared to mesenchymal stem cells, thus implicating let-7a as a potential treatment target. Mice with Ewing’s sarcoma treated with let-7a miRNA had a decrease in tumor burden along with a change in gene expression. This implies that let-7a miRNA plays a significant role in Ewing’s sarcoma, and can also be a target for Ewing’s sarcoma therapy (De Vito et al. 2011).
Another way to target EWS-FLI1 is to target the proteins that are involved in its transcription. YK-4-279 blocks RNA helicase A binding to EWS-FLI1 and thus induces apoptosis in ESFT cell lines. This treatment has led to inhibition of growth in xenograft mouse models (Erkizan et al. 2009). YK-4-279 has been evaluated in a clinical trial at the University of Texas MD Anderson Cancer Center (Subbiah and Anderson 2011). Another very promising downstream target that is being tested in clinical trials is poly(ADP-ribose) polymerase (PARP 1). Brenner et al. (2012) published data demonstrating that EWS-FLI increases PARP 1 expression which in turn promotes more EWS FLI expression. Xenograft Ewings sarcoma models demonstrated sensitivity to PARP 1 inhibitors. This sensitivity is further increased when PARP 1 inhibitors are combined with Temazolamide.
Vascular Endothelial Growth Factor (VEGF)
The pathogenesis of Ewing’s sarcoma is partly contributed to by blood vessel formation. There are two specific processes that are part of blood vessel formation: angiogenesis and vasculogenesis. Angiogenesis is the growth of new vessels off of preexisting vessels and vasculogenesis refers to the initial formation of the vasculature. Production of vascular endothelial growth factor (VEGF) and engagement of its receptors is thought to contribute to the development of new vessels in Ewing’s sarcoma (Stewart and Kleinerman 2011). EWS-FLI1 also contributes to vessel production as it upregulates production of VEGF-A mRNA and protein levels (Nagano et al. 2010). In a preclinical trial using an ESFT model it was noted that VEGF was produced and secreted in 6/6 ESFT cell lines tested. High VEGF expression was also noted in 18 of 30 patients’ tumor samples. Expression of VEGF correlated with microvessel density (MVD) (Dalal et al. 2005). High expression in tumor samples also correlated with patient’s survival. Patients with high level of expression had decreased survival compared to those with low level of expression (Ahmed et al. 2011).
Preclinical studies have demonstrated that by blocking VEGF A production (with a VEGF-A-targeted siRNA) (Nagano et al. 2010) and inhibiting VEGF with an antibody (rhuMAb) (Dalal et al. 2005) there is significant tumor shrinkage. These preclinical studies, along with others, have led to the use of anti-angiogenesis/vasculogenesis agents in phase 1 trials. Despite the evidence that antivascular therapy has efficacy, it is likely not going to be curative alone. In future studies, it will be important to evaluate how antivascular agents improve outcomes in combination with traditional chemotherapy or other targeted therapy (Stewart and Kleinerman 2011).
Insulin Growth Factor Receptor (IGFR)
It has been shown that most ESFT tumor cells express an increased level of the insulin growth factor- 1 receptor (IGF-1R) or insulin growth factor- 2 receptor (IGF-2) ligands (Grimberg and Cohen 2000). The IGF-1R is a tetrameric tyrosine kinase receptor which is seen in both normal and neoplastic cells. The activation of IGF-1R is by the engagement of growth factor ligands IGF-1 and IGF-2, which then results in the autophosphorylation of these receptors. There are six IGF binding proteins which serve to regulate the activity of the IGF-1R by either promoting or inhibiting signaling by the binding of these IGF ligands in the circulation (Grimberg and Cohen 2000). The IGF-1R converts extracellular signaling intracellularly, which then mediates the proliferation, growth and survival of cells. Activation of the IGF-1R leads to activation of several signaling pathways, such as the phosphatidylinositol 3 phosphate kinase/Akt/mammalian target of rapamycin (mTOR) pathway. When activated, these pathways may lead to the promotion of an oncogenic phenotype. There has been evidence that the IGF-R1 signaling is critical in the biology of the ESFT. It has also been shown that malignant transformation by the pathognomonic EWS-FLI1 fusion gene is dependent on IGF-1R (Toretsky et al. 1997). The EWS-FLI1 fusion gene also promotes the activation of the IGF-R1 by downgrading the expression of the insulin growth factor binding protein-3 (IGFBP-3). There have been several studies demonstrating that drugs targeting the IFG-R1 inhibitors may elicit growth arrest in Ewing’s sarcoma cells in xenograft models (Scotlandi et al. 2005).
Recently there have been several clinical trials using monoclonal antibodies against the IGFR-1 receptor. So far the results of these trials have not been as promising as expected (Ho and Schwartz 2011; Subbiah and Anderson 2011). There are current trials that are designed to improve the efficacy of IGF-R1 inhibitors by combining them with other targeted therapy involved in the pathway, such as mTOR inhibitors (Subbiah and Anderson 2011).
The Mammalian Target of Rapamycin (mTOR)
The mammalian target of rapamycin (mTOR) is a serine-threonine kinase that controls cap-dependent translation. It plays an integral role in the regulation of multiple signaling pathways that control cellular growth, division, metabolism and angiogenesis (Bjornsti and Houghton 2004). mTOR is activated in response to nutritional and environmental conditions and plays a role in the transduction of proliferative signals mediated through the phosphoinositide-3-kinase (PI3K)/Akt pathway. mTOR and members of the PI3K-AKT pathway are identified in ESFT, both in vivo and in vitro studies (Ahmed et al. 2011).
Rapamycin is a macrocyclic lactone antibiotic, and the first compound to demonstrate specific mTOR inhibition. Deforlimus (also known as AP23573) is a non-prodrug analog of rapamycin that has also been shown to have mTOR activity inhibition. mTOR inhibition may have direct effects on cancer cell proliferation and survival, or indirectly by inhibition of the hypoxia inducible factor 1α (HIF1α) which reduces tumor induced vascular endothelial growth factors (VEGF) (Faivre et al. 2006). Rapamycin has demonstrated in multiple tumor models an anti-angiogenic activity through decreasing the density of vessels. The anti-angiogenic activity of rapamycin has been linked to a decrease in the production of VEGF and inhibition of vascular endothelial cells to stimulation by VEGF (Guba et al. 2002).
In both adult and pediatric cancer cell lines, including those derived from rhabdomyosarcoma, neuroblastoma, glioblastoma, osteosarcoma, and Ewing’s sarcoma, rapamycin has resulted in inhibition of cell growth (Bjornsti and Houghton 2004; Mateo-Lozano et al. 2003). mTOR inhibitors are currently being studied as single agents or part of combination therapy in the treatment of solid tumors and specifically for Ewing’s sarcoma in combination with IGF-R1 inhibitors (Subbiah and Anderson 2011).
In conclusion a better understanding of the pathogenesis of Ewing’s sarcoma has led to the development of new targeted therapies for this disease. Targeted therapies may be combined with current chemotherapeutic regimens to improve outcomes. The incorporation of other targeted therapies to prevent resistance is the next step in the cure of this malignancy.
References
Ahmed AA, Sherman AK, Pawel BR (2011) Expression of therapeutic targets in Ewing sarcoma family tumors. Hum Pathol 43(7):1077–1083
Applebaum MA, Worch J, Matthay KK, Goldsby R, Neuhaus J, West DC, DuBois SG (2011) Clinical features and outcomes in patients with extraskeletal Ewing sarcoma. Cancer 117:3027–3032
Arvand A, Denny CT (2001) Biology of EWS/ETS fusions in Ewing’s family tumors. Oncogene 20:5747–5754
Bacci G, Balladelli A, Forni C, Longhi A, Serra M, Fabbri N, Alberghini M, Ferrari S, Benassi MS, Picci P (2007) Ewing’s sarcoma family tumours. Differences in clinicopathological characteristics at presentation between localised and metastatic tumours. J Bone Joint Surg Br 89:1229–1233
Bernstein M, Kovar H, Paulussen M, Randall RL, Schuck A, Teot LA, Juergens H (2006) Ewing’s sarcoma family of tumors: current management. Oncologist 11:503–519
Bjornsti MA, Houghton PJ (2004) The TOR pathway: a target for cancer therapy. Nat Rev Cancer 4:335–348
Brenner JC, Feng FY, Han S, Patel S, Goyal SV, Bou-Maroun LM, Liu M, Lonigro R, Prensner JR, Tomlins SA, Chinnaiyan AM (2012) PARP-1 inhibition as a targeted strategy to treat Ewing’s sarcoma. Cancer Res 72:1608–1613
Bozzi F, Tamborini E, Negri T, Pastore E, Ferrari A, Luksch R, Casanova M, Pierotti MA, Bellani FF, Pilotti S (2007) Evidence for activation of KIT, PDGFRa, and PDGFRb receptors in the Ewing sarcoma family of tumors. Cancer 109:1638–1645
Dalal S, Berry AM, Cullinane CJ, Mangham DC, Grimer R, Lewis IJ, Johnston C, Laurence V, Burchill SA (2005) Vascular endothelial growth factor: a therapeutic target for tumors of the Ewing’s sarcoma family. Clin Cancer Res 11:2364–2378
De Vito C, Riggi N, Suva ML, Janiszewska M, Horlbeck J, Baumer K, Provero P, Stamenkovic I (2011) Let-7a is a direct EWS-FLI-1 target implicated in Ewing’s sarcoma development. PLoS One 6:e23592
Erkizan HV, Kong Y, Merchant M, Schlottmann S, Barber-Rotenberg JS, Yuan L, Abaan OD, Chou TH, Dakshanamurthy S, Brown ML, Uren A, Toretsky JA (2009) A small molecule blocking oncogenic protein EWS-FLI1 interaction with RNA helicase A inhibits growth of Ewing’s sarcoma. Nat Med 15:750–756
Faivre S, Kroemer G, Raymond E (2006) Current development of mTOR inhibitors as anticancer agents. Nat Rev Drug Discov 5:671–688
Giovannini M, Biegel JA, Serra M, Wang JY, Wei YH, Nycum L, Emanuel BS, Evans GA (1994) EWS-erg and EWS-FLI1 fusion transcripts in Ewing’s sarcoma and primitive neuroectodermal tumor with variant translocations. J Clin Invest 94:489–496
Girnita L, Girnita A, Wang M, Meis-Kindblom JM, Kindblom LG, Larsso O (2000) A link between basic fibroblast growth factor (bFGF) and EWS/FLI-1 in Ewing’s sarcoma cells. Oncogene 19:4298–4301
Grimberg A, Cohen P (2000) Role of insulin-like growth factors and their binding proteins in growth control and carcinogenesis. J Cell Physiol 183:1–9
Guba M, von Breitenbuch P, Steinbauer M, Koehl G, Flegel S, Hornung M, Bruns CJ, Zuelke C, Farkas S, Anthuber M, Jauch KW, Geissler EK (2002) Rapamycin inhibits primary and metastatic tumor growth by antiangiogenesis: involvement of vascular endothelial growth factor. Nat Med 8:128–135
Herrero-Martin D, Fourtouna A, Niedan S, Riedmann LT, Schwentner R, Arvee DN (2011) Factors affecting EWS-FLI1 activity in Ewing’s sarcoma. Sarcoma 2011:352580
Ho AL, Schwartz GK (2011) Targeting of insulin-like growth factor type 1 receptor in Ewing sarcoma: unfulfilled promise or a promising beginning? J Clin Oncol 29:4581–4583
Jedlicka P (2010) Ewing Sarcoma, an enigmatic malignancy of likely progenitor cell origin, driven by transcription factor oncogenic fusions. Int J Clin Exp Pathol 3:338–347
Ladenstein R, Potschger U, Le Deley MC, Whelan J, Paulussen M, Oberlin O, Van den Berg H, Dirksen U, Hjorth L, Michon J, Lewis I, Craft A, Jürgens H (2010) Primary disseminated multifocal Ewing sarcoma: results of the Euro-EWING 99 trial. J Clin Oncol 28:3284–3291
Lewis TB, Coffin CM, Bernard PS (2007) Differentiating Ewing’s sarcoma from other round blue cell tumors using a RT-PCR translocation panel on formalin-fixed paraffin-embedded tissues. Mod Pathol 20:397–404
Lin PP, Wang Y, Lozano G (2011) Mesenchymal stem cells and the origin of Ewing’s sarcoma. Sarcoma 2011:2011
Mateo-Lozano S, Tirado OM, Notario V (2003) Rapamycin induces the fusion-type independent downregulation of the EWS/FLI-1 proteins and inhibits Ewing’s sarcoma cell proliferation. Oncogene 22:9282–9287
McAllister NR, Lessnick SL (2005) The potential for molecular therapeutic targets in Ewing’s sarcoma. Curr Treat Options Oncol 6:461–471
Miyagawa Y, Okita H, Nakaijima H, Horiuchi Y, Sato B, Taguchi T, Toyoda M, Katagiri YU, Fujimoto J, Hata J, Umezawa A, Kiyokawa N (2008) Inducible expression of chimeric EWS/ETS proteins confers Ewing’s family tumor-like phenotypes to human mesenchymal progenitor cells. Mol Cell Biol 28:2125–2137
Nagano A, Ohno T, Shimizu K, Hara A, Yamamoto T, Kawai G, Saitou M, Takiqami I, Matsuhashi A, Yamada K, Takei Y (2010) EWS/Fli-1 chimeric fusion gene upregulates vascular endothelial growth factor-A. Int J Cancer 126:2790–2798
Paulussen M, Fröhlich B, Jürgens H (2001) Ewing tumour incidence, prognosis and treatment options. Paediatr Drugs 3:899–913
Pinto A, Dickman P, Parham D (2011) Pathobiologic markers of the Ewing sarcoma family of tumors: state of the art and prediction of behaviour. Sarcoma 2011:856190
Riggi N, Cironi L, Provero P, Suva ML, Kaloulis K, Garcia-Echeverria C, Hoffmann F, Trumpp A, Stamenkovic I (2005) Development of Ewing’s sarcoma from primary bone marrow–derived mesenchymal progenitor cells. Cancer Res 65:11459–11468
Riggi N, Suva ML, Suva D, Cironi L, Provero P, Tercier S, Joseph JM, Stehle JC, Baumer K, Kindler V, Stamenkovic I (2008) EWS-FLI-1 expression triggers a Ewing’s sarcoma initiation program in primary human mesenchymal stem cells. Cancer Res 68:2176–2185
Rocchi A, Manara MC, Sciandra M, Zambelli D, Filippo Nardi F, Nicoletti G, Garofalo C, Meschini S, Astolfi A (2010) CD99 inhibits neural differentiation of human Ewing sarcoma cells and thereby contributes to oncogenesis. J Clin Invest 120:668–680
Scotlandi K, Benini S, Sarti M, Serra M, Loffini PL, Maurici D, Picci N, Manara MC, BaIdini N (1996) Insulin-like growth factor I receptor-mediated circuit in Ewing’s sarcoma/peripheral neuroectodermal tumor: a possible therapeutic target. Cancer Res 56:4570–4574
Scotlandi K, Manara MC, Nicoletti G, Lollini PL, Lukas S, Benini S, Croci S, Perdichizzi S, Zambelli D, Serra M, García-Echeverría C, Hofmann F, Picci P (2005) Antitumor activity of the insulin-like growth factor-I receptor kinase inhibitor NVP-AEW541 in musculoskeletal tumors. Cancer Res 65:3868–3876
Stewart KS, Kleinerman ES (2011) Tumor vessel development and expansion in Ewing’s sarcoma: a review of the vasculogenesis process and clinical trials with vascular targeting agents. Sarcoma 2011:165837
Subbiah V, Anderson P (2011) Targeted therapy of Ewing’s sarcoma. Sarcoma 2011:686985
Toomey EC, Schiffman JD, Lessnick SL (2010) Recent advances in the molecular pathogenesis of Ewing’s sarcoma. Oncogene 29:4504–4516
Toretsky JA, Kalebic T, Blakesley V, LeRoith D, Helman LJ (1997) The insulin-like growth factor-I receptor is required for EWS/FLI-1 transformation of fibroblasts. J Biol Chem 272:30822–30827
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Ahmed, A.A., Samuel, G., Fulbright, J.M. (2013). Ewing’s Sarcoma Family of Tumors: Targeting Molecular Pathways and the Race for a Cure. In: Hayat, M. (eds) Pediatric Cancer, Volume 4. Pediatric Cancer, vol 4. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6591-7_21
Download citation
DOI: https://doi.org/10.1007/978-94-007-6591-7_21
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6590-0
Online ISBN: 978-94-007-6591-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)