Abstract
Acupuncture is one of the most extensively studied complementary medicine modalities. The quality of acupuncture research has become increasingly better, due to refinement of research methodology and its dissemination among the researchers. In recent years, many randomized controlled trials have been reported on the application of acupuncture in cancer care. Here we review the studies deemed of high quality (Jadad scale 3 or above). The studies consist of randomized controlled trials of acupuncture on nausea, vomiting, hot flashes, xerostomia, pain, fatigue, mood-related symptoms and neutropenia. The most solid evidence came from studies of chemotherapy-related nausea and vomiting. Acupuncture has been repeatedly demonstrated to reduce nausea and vomiting in both the post-operative setting and the chemotherapy setting. Less strong evidence with mixed results was demonstrated in trials on hot flashes, xerostomia and post-operative pain, where acupuncture has shown benefit in some but not in other trials. There are insufficient number of trials of reasonable quality to evaluate other indications for acupuncture in cancer care. Serious adverse events are rare or non-existent among those trials. It would help our understanding of acupuncture if future studies take a “whole system” approach, taking into consideration of efficacy and effectiveness questions, and further explore the mechanistic aspect of acupuncture.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
15.1 Introduction
Acupuncture is a therapeutic modality in traditional Chinese medicine (TCM), developed over the millennia. Acupuncture treatment involves the placement of needles at selected points on the body, followed by manipulation with physical forces, heat, or, in modern times, electrical stimuli. According to TCM theory, vital energy (Qi or Chi in Chinese) flows throughout the body along channels called meridians. It was believed that the interruption or obstruction of the energy makes the individual vulnerable to illness. The insertion of needles at specific points along the meridian was thought to regulate the energy flow, which would produce therapeutic benefit.
Although the concepts of Qi and meridians are inconsistent with our current understanding of human anatomy and physiology, research in the past few decades supports the clinical effects of acupuncture. Recent neuroscience research suggests that it appears to work by modulating the nervous system. In large part due to such research, acupuncture has become increasingly integrated into mainstream cancer care in the Western medical practice setting. Most major comprehensive cancer centers and many community hospitals have an integrative medicine component that includes acupuncture treatment as a supportive care measure (Deng et al. 2006; Sagar 2008; Stone and Johnstone 2010).
There is no evidence that acupuncture has direct effects against cancer and it should not be used in efforts to treat the disease. However, clinical research shows that acupuncture can reduce many important physical and emotional symptoms commonly experienced by cancer patients, thereby improving patients’ quality of life. In this chapter, we review recent clinical trials that advance understanding of how to best use acupuncture in cancer care.
15.2 Methods
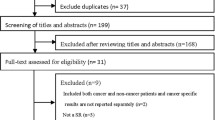
The National Institutes of Health pubmed.gov database was searched using the keywords “acupuncture” and “cancer” and adding the individual indications of “nausea”, “vomiting”, “hot flashes”, “xerostomia”, “pain”, “fatigue”, “neutropenia”, “ileus”, “lymphedema”, “dyspnea”, “breath”, “breathlessness”, “palliative” and “hospice,” limited to clinical trials published in the English language for the 5-year period from January 2007 through January 2012).
Methodological quality of trial design was evaluated using the Jadad scale, a widely employed five-item scoring measure for clinical trials (Jadad et al. 1996; Clark et al. 1999). Trials examined and discussed in detail had to be prospective and randomized with at least two experimental arms, and score a minimum of three points on the Jadad scale (trials with only single-blinding of either subjects or investigators were not awarded points for “double-blinding,” contrary to the practice of some other reviewers). Trials meeting these criteria were identified. Those that received less than three points or were not randomized were not mentioned. High quality trials that were already reviewed elsewhere were only described briefly. Clinical conditions and specific details of the acupuncture regimens were tabulated using the 2010 Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) , to ensure that reproducibility and theoretically sound rationale for treatment protocols was appropriately documented (MacPherson et al. 2010). All attempts were made to catalogue acupuncture points according to standardized WHO nomenclature (1990).
The majority of recent clinical trials that met the review criteria have focused on managing the complications of chemotherapy surgery or radiation in cancer patients, the most common indications were nausea and vomiting, hot flashes and pain. Other trials focused on xerostomia and various measures of quality of life , including fatigue, depression and insomnia . Other commonly researched cancer-related indications were not examined in any high quality randomized clinical trial in the past 5 years. These included lymphedema, dyspnea , hiccups and post-operative ileus. Overall, the most commonly studied single acupuncture point was Neiguan (PC6), most often for treatment of nausea and vomiting.
15.3 Acupuncture for Nausea and Vomiting-related to Cancer
The most recent Cochrane review regarding acupuncture for chemotherapy-induced nausea or vomiting was published in 2006. It examined eleven randomized controlled trials , concluding that electroacupuncture helps reduce chemotherapy-induced nausea and vomiting, and that self-acupressure can help prevent nausea. However, manual acupuncture apparently was not effective, and cutaneous electrical stimulation in the setting of antiemetic drug use did not demonstrate a significant impact (Ezzo et al. 2006). A more recent Cochrane review examining acupuncture for nausea and vomiting for post-operative patients, regardless of the presence or absence of cancer, was published in 2009. After reviews of 40 randomized controlled trials involving stimulation of the PC6 acupuncture point, the reviewers concluded that this intervention does prevent post-operative nausea and vomiting, although significant differences between PC6 stimulation and antiemetic medications was not clearly demonstrated (Lee and Fan 2009). Subsequent trials that specifically addressed acupuncture for cancer patients but not previously discussed in the above reviews, are mentioned below.
A randomized, partially blinded, placebo-controlled trial (Jadad score = 5) by Wang et al. (2010) used the PC6 acupoint to investigate the ability of transcutaneous electrode stimulation to prevent post-operative nausea and vomiting within 24 h of craniotomy. Particularly in post-craniotomy patients, nausea control is critical for preventing increases in intracranial pressure, arterial pressure, lung aspiration, dehydration, and disturbance of electrolytes and acid-base status. Up to 60% of post-craniotomy patients continue to experience post-operative nausea and vomiting despite use of antiemetic medications.
The included patients (n = 80) were age 20–60 with supratentorial cerebral tumors undergoing craniotomy (mostly for gliomas and meningiomas), with body mass index < 30 and no history of DM, smoking, motion sickness, or prior experience with electrodes or post-operative nausea and vomiting. True electrostimulation at 2 Hz alternating with 100 Hz was delivered to the right PC6 acupoint starting 30 min pre-operatively, continuing intra-operatively, and terminating six hours post-operatively. Sham control involved electrode placement at a non-acupoint on the dorsal forearm. All patients received pharmacological antiemetics, ondansetron and metoclopramide. Cumulative incidence of nausea at 24 h was significantly decreased by 40%, and the incidence of vomiting was decreased by 60% in the group randomized to electrostimulation of the PC6 acupoint.
This study was important not only because of the quality of its methodology and STRICTA reporting, but also because it demonstrated that a simple, non-puncturing acupoint intervention, administered by clinical staff untrained in acupuncture, was effective for nausea/vomiting control. It also demonstrated that pre-operative intervention at PC6 was extremely effective, whereas prior studies often found that post-operative stimulation at PC6 failed to produce adequate anti-emesis.
A randomized, double-blinded pragmatic trial of true vs sham acupuncture (n = 215, Jadad score = 5) at the PC6 point was undertaken by Enblom et al. (2012) to investigate the effect of acupuncture on treating radiation-induced nausea . Patients were at least 18 years of age, with various cancer diagnoses (i.e. gynecologic, anal, rectal, colonic, gastric, pancreatic, testicular), planned radiation of greater than 800 cm3 and 25 Gy dose to the abdomen, without any acupuncture treatment ever for emesis or for any other indication in the past year, and without any persistent emesis or antiemetic treatment in the 24 h preceding the start of radiotherapy. The primary outcome measurement was number of patients with at least one episode of nausea. Ultimately, there was no statistically significant difference between the true and sham groups, although patients in both groups subjectively reported that they felt the treatment that they had received was effective (92–95% in the true group, 94–96% in the sham group).
Hence an additional analysis was published by Enblom et al. (2011) comparing true vs sham acupuncture against a third usual care group (i.e. a pragmatic and efficacy trial, Jadad score = 3) to investigate the degree to which non-specific anti-emetic effects are invoked during acupuncture used to treat radiation-induced nausea. This study was only partially randomized in that randomization occurred within an acupuncture group (i.e. to true or sham), but both the acupuncture and usual care groups were selected, apparently without randomization, from two partially overlapping populations of patients. Non-randomization led to the standard care cohort having significantly more men than the acupuncture cohort, more patients with testicular tumors, and fewer patients consuming antiemetics, serotonin-receptor antagonists, or corticosteroids. Nausea was assessed daily in the true/sham acupuncture cohort, and only once (after radiation) in the usual care group. Although nausea intensity was significantly lower in the true and sham acupuncture groups vs the usual care group, there were no statistical differences between the true and sham groups in terms of nausea frequency/intensity, vomiting or use of antiemetics in the preceding 24 h or week (at the time of questioning). However, patients’ expectation of nausea was significantly correlated with actual development of nausea. Of note, a significant 30% cost savings per patient was also observed when comparing an equivalent number of acupuncture (true or sham) sessions to daily use of 8 mg of serotonin-receptor antagonists throughout a full course of radiation therapy .
An interesting variation of PC6 stimulation was examined by You et al. (2009) in a randomized, non-blinded trial (Jadad score = 3) examining treatment of cancer-related emesis using a combination of manual acupuncture plus simultaneous pyridoxine (vitamin B6) 50 mg injection into the PC6 acupoints themselves, vs manual acupuncture alone vs pyridoxine 50 mg intramuscular injection twice daily for 21 days. Patients receiving acupuncture alone and acupuncture plus B6 injections were treated every other day for ten sessions. This study was conceived because pyridoxine has been demonstrated to be an inexpensive and effective treatment for cancer-related nausea/vomiting. Included patients (n = 142) were age 45–65 with stage 2–3 ovarian cancer , with mild-moderate nausea/vomiting, and utilizing an identical chemotherapy and antiemetic drug regimen, with no history of hepatitis or other gastrointestinal disease, mental illness, lymphedema or active infection. This trial demonstrated that, over the 21-day duration of the trial, subjects in the combination of acupuncture plus pyridoxine injections at PC6 group had significantly fewer total episodes of emesis per person and more emesis-free days than did subjects in either of the single-intervention groups.
A randomized, non-blinded, usual care-controlled crossover trial (Jadad score = 3) was recently performed by Gottschling et al. (2008) in pediatric cancer patients to investigate the utility of individualized acupuncture regimens in managing chemotherapy-induced nausea and vomiting. Most commonly employed points in these individualized regimens included PC6, Zusanli (ST36), Zhongwan (CV12) and Hegu (LI4). Included patients (n = 23) were age 6–18 with “solid malignant tumors” (the majority being Ewing’s sarcoma and rhabdomyosarcoma) but without cerebral metastasis and with no prior acupuncture in the past 6 months, who were scheduled to receive at least three identical and consecutive chemotherapy courses with drugs that are considered “highly emetogenic.” Patients who did not experience nausea and/or vomiting during the first course of chemotherapy were excluded from participation, and those who did were randomized to receive either acupuncture or usual care with standing prophylactic 5-HT3 antagonists (i.e. ondansetron, tropisetron) as well as additional rescue antiemetics (i.e. dexamethasone, phenothiazines) during the second course of chemotherapy. For the third course of chemotherapy (each course is separated by at least 2 weeks) patients from the acupuncture group were switched to the usual care group, and vice versa.
While undergoing acupuncture, patients required significantly less phenothiazines as rescue antiemetics (though dexamethasone usage was not significantly different) and had significantly less episodes of retching or emesis . The only adverse effect noted was pain from needling (17%) and while six patients either died, stopped chemotherapy or were lost to follow-up, 71% of the remaining patients requested continuation of acupuncture for antiemesis when this option was offered at the conclusion of the study. This trial was significant because it demonstrated both safety and tolerability, and efficacy of acupuncture for treatment of cancer-related nausea/vomiting in pediatric patients. However, the publication’s limited report of treatment details based on STRICTA criteria renders it difficult to examine critically or reproduce.
15.4 Acupuncture for Cancer-related Hot Flashes
15.4.1 Breast Cancer
Three recent review articles, including a Cochrane review, discussed nine randomized controlled trials examining acupuncture for treating hot flashes related to breast cancer, and concluded that evidence to date is not convincing that acupuncture is effective for this indication (Chao et al. 2009; Lee et al. 2009a; Rada et al. 2010). Four of the reviewed trials were performed within the 5-year scope of this chapter. The lone study showing clear benefit from acupuncture was an efficacy trial by Hervik and Mjaland (2008) (n = 59, Jadad score = 3) studying true vs sham acupuncture in post-surgical patients treated with tamoxifen, which showed significant improvement in both daytime and nighttime hot flash frequency in the true acupuncture group over 22 weeks (subsequent follow-up at 2 years is discussed below) (Hervik and Mjaland 2009). One efficacy trial by Deng et al. (2007) (n = 72, Jadad score = 5) demonstrated hot flash reduction with both true and sham acupuncture involving several acupuncture points, though no statistically significant difference was noted between groups.
A pragmatic trial by Frisk et al. (2008) (n = 45, Jadad score = 3) compared electroacupuncture (points unspecified) over 12 weeks with estrogen/progesterone hormone therapy for 24 months, and claimed that, while both treatments significantly reduced hot flash symptoms, hormone therapy was “more effective” than electroacupuncture at decreasing hot flash frequency and impact, although no inter-group statistical significance was cited (further analysis of other parameters was published later, see below). Notably, this trial represented a substudy of the larger Swedish HABITS trial that ultimately was discontinued because it showed higher rates of breast cancer recurrence in breast cancer patients treated with hormone therapy, with the final recommendation that hormone therapy be avoided in such patients (Holmberg et al. 2008).
Finally, results from a pragmatic trial by Walker et al. (2010) (n = 50, Jadad score = 2 with no mention of randomization method) comparing acupuncture to venlafaxine , an anti-depressant , showed that both therapies significantly reduced hot flashes, and although there was no statistical inter-group difference, acupuncture reportedly produced none of the venlafaxine-associated adverse effects, and more beneficial side effects , such as improvement in energy, clarity of thought, sex drive and overall sense of well-being. Following publication of these review articles, additional studies examining acupuncture for hot flashes in breast cancer were published and are discussed below.
A follow-up study published by Hervik and Mjaland (2010) (n = 82, Jadad score = 3 for previous design) re-evaluated patients from their initial 2008 efficacy trial (Hervik and Mjaland 2009) 2 years after completing true vs sham acupuncture treatment for post-surgical and tamoxifen-related hot flashes (Hervik and Mjaland 2010). Questionnaires soliciting open-ended thoughts about their breast cancer diagnosis and treatment were sent to living patients from the 2008 trial cohort, and to 31 additional women who were “treated and followed up in an identical manner to those included originally” . Twenty eight of 61 respondents commented about hot flashes and acupuncture treatment. Of those who had been randomized to true acupuncture, 15 described positive experiences both during and after acupuncture treatment and ten stated that hot flashes were still “fewer and milder” than they were prior to the acupuncture treatment administered 2 years earlier, compared to only one patient from the sham acupuncture group. Among the sham group patients, nine women reported ongoing severe hot flashes at the 2-year follow-up interval, four stated that acupuncture had been ineffective, and one mentioned that acupuncture had been unpleasant. Limitations of the study include the fact that no statistical analysis of these qualitative results was performed, and an additional cohort of 31 patients was added who were not formally followed in the previous 2008 trial. However, these subjective results suggest that true acupuncture, if demonstrated to outperform sham acupuncture with statistical significance, may indeed induce long-lasting benefits that persist even for 2 years.
Frisk et al. (2012) (n = 45) published a re-analysis of their initial 2008 trial of electroacupuncture vs hormone therapy (Frisk et al. 2008) to examine other subjective measures of quality of life, sleep quality, distress level, and general well-being (Frisk et al. 2012). Modest but statistically significant improvement in these parameters was demonstrated in both the electroacupuncture and hormone therapy groups, although no statistically significant superiority of electroacupuncture was observed. These results are in accord with the original 2008 study’s primary outcome measure of hot flash reduction. However, the authors make the case that, as closure of the HABITS trial renders hormone therapy a dubious first-line agent for treating hot flashes and associated symptoms in breast cancer patients, electroacupuncture may be considered an alternative of comparable efficacy that is perhaps better tolerated and safer than hormone therapy .
A randomized, single-blinded, sham-controlled efficacy trial (2010) (n = 84, Jadad score = 3) was published by Liljegren et al. (2010) examining the effect of true vs sham acupuncture on hot flashes in breast cancer, using a number of points. Included patients were age 36–80, at least one year following last menstruation, with history of completed medical and surgical treatment for breast cancer without recurrence, on adjuvant tamoxifen for at least two months, not on any other adjuvant chemotherapy or radiation, with significant vasomotor symptoms and with no acupuncture treatment within six months of the study . Although nighttime sweating alone was significantly improved in the true acupuncture group, no significant difference was observed in the primary outcome measures of hot flashes and sweating frequencies at one week after completion of the experimental course. Additionally, there were no significant differences between the groups in levels of follicle-stimulating hormone, luteinizing hormone , estradiol, progesterone, sex hormone-binding globulin, prolactin or testosterone.
15.4.2 Prostate Cancer
A recent review article discussed six studies investigating acupuncture for the treatment of hot flashes in prostate cancer patients (Lee et al. 2009b). Only one of the included trials was randomized and with a high quality Jadad score above 1, and conducted within the past five years. This trial, conducted by Frisk et al. (2009) (n = 31, Jadad score = 5), compared electroacupuncture vs traditional acupuncture at multiple points, for treating hot flashes in patients with prostate cancer. Patients had undergone castration therapy with either surgical or medical (i.e. gonadotropin-releasing hormone analogues) interventions. In brief, both groups demonstrated significant reduction in hot flashes following 12 weeks of treatment, although no significant difference was found between the electroacupuncture and traditional acupuncture groups. The authors recommended further investigation with sham or placebo controls, or with a usual care group.
15.5 Acupuncture for Xerostomia in Cancer Patients
A recent acupuncture neuroimaging study by Deng et al. (2008a) noted that acupuncture delivered with twisting manual stimulation at the Erjian (LI2) acupuncture point on the non-dominant side produced a distinct pattern of brain activation on fMRI that was not reproduced with sham acupuncture stimulation, and a corresponding significant increase in saliva secretion as compared to sham stimulation, with salivary flow measured at the bilateral parotid glands. These empiric objective findings suggest that acupuncture can be a useful modality for treating the complication of xerostomia that is often noted in cancer patients undergoing radiation treatment at the head and neck. A recent review by O’Sullivan and Higginson (2010) discussed three randomized trials examining acupuncture as treatment for radiation-induced xerostomia (RIX) in patients with head and neck cancer , and concluded that evidence to date was still inconclusive, yet justified further investigation of this modality. One of these trials was published in 1996 and falls outside of the timeframe of this review (Blom et al. 1996). One small, randomized, single-blind efficacy trial by Cho et al. (2008) (n = 12, Jadad score = 2 with no definite description of withdrawals or dropouts) examined true vs sham acupuncture at multiple points in patients with head and neck cancer following radiotherapy, noting significantly higher salivary flow rates and improved quality of life in the true acupuncture group after 6 weeks of treatment. A third randomized, non-blinded pragmatic trial by Pfister et al. (2010) (n = 58, Jadad score = 3) was extensively reviewed by multiple review papers (Capodice 2010; Lu and Rosenthal 2010; O’Sullivan and Higginson 2010). It investigated weekly acupuncture at multiple points (including LI2) vs usual care for xerostomia in patients who had undergone neck dissection for cancer at least three months prior to the study. Statistically significant improvement in xerostomia as measured on the Xerostomia Inventory, as well as pain and functional status as measured by the Constant-Murley scale, was noted in the acupuncture group as compared to the control group.
One other study was located during our literature search, which was not yet reviewed elsewhere. A randomized, non-blinded pragmatic trial of acupuncture vs usual care was recently undertaken by Meng et al. (2012) (n = 86, Jadad score = 3) to investigate the utility of acupuncture administered prior to and on the same days as radiation treatments for preventing RIX in patients with nasopharyngeal carcinoma . Included patients were over 18 years of age, with nasopharyngeal carcinoma but anatomically intact parotid and submandibular glands and no suspected or confirmed salivary duct closure, Zubrod performance status of 0–2, no history of xerostomia, no planned intensity-modulated radiation therapy, no bleeding disorder or anticoagulant use, no history of stroke or spinal cord injury, no saliva-modulating drug use in the preceding 30 days or during the study, and no contraindications for acupuncture at any of the studied acupuncture points. Seven weeks of acupuncture, three times each week, was performed. Statistically significant improvement in xerostomia and quality of life , as measured on the Xerostomia Questionnaire and the MD Anderson Symptom Inventory-Head and Neck, was noted starting at week 3, and persisted for 6 months. Additionally, significantly higher unstimulated salivary flow rates in the acupuncture group were noted from weeks 3–11, and significantly higher stimulated salivary flow rates were noted from week 7 through 6 months. This publication was important in that it was the first high-quality trial of its kind to demonstrate the preventive effects of acupuncture administered concurrent with active radiation therapy , indicated that future trials with larger sample sizes and a variety of control arms should be undertaken.
15.6 Acupuncture for Pain in Cancer Patients
Acupuncture appears to be a promising treatment for pain unrelated to cancer, with a review of recent Cochrane reviews published by Lee and Ernst (2010) discussing good evidence demonstrating that the modality is helpful for at least some types of pain (i.e. peripheral joint osteoarthritis, migraine treatment and prophylaxis, neck pain, low back pain), though they mentioned that definitive evidence has not yet been produced regarding some other pain indications (i.e. rheumatoid arthritis, shoulder pain, lateral elbow pain). The most recent Cochrane review by Paley et al. (2011b) examining acupuncture specifically for cancer pain in adults described only three high-quality randomized controlled trials for this indication, though a high-quality trial by Mehling et al. (2007) was also briefly mentioned. Of the three trials discussed, one was conducted in 1998 and one in 2003, which are effectively outside of the time scope of this chapter (Dang and Yang 1998; Alimi et al. 2003). The other trial cited from 2008 was not published in the English language, thus causing it to fall outside of the boundaries of this chapter, as well (Chen et al. 2008). Another recent review of acupuncture for cancer pain by Hopkins Hollis (2010) identified two of the above studies mentioned studies from the Paley Cochrane review (Dang and Yang 1998; Alimi et al. 2003), an older study from 1986 (Xia et al. 1986) and a more recent study from 2007 (Minton and Higginson 2007) examining electroacupuncture for neuropathic pain that was not peer-reviewed, but rather published as a letter to the editor. Both of these review articles concluded that evidence is currently insufficient to accurately judge whether acupuncture is helpful for cancer pain.
However, another review article by Capodice (2010) has in fact identified several other recent, high-quality trials examining acupuncture for cancer-related pain that were not mentioned in the Paley Cochrane review or the Hopkins Hollis review, and even concluded that acupuncture should be “recommended as a complementary therapy if pain is poorly controlled and may offer utility as a primary treatment for cancer-related pain” based on the “significant body of research” from these studies, with a level 1A recommendation. One high-quality randomized efficacy trial conducted by Crew et al. (2010) (n = 43, Jadad score = 5) compared true vs sham acupuncture at multiple body and auricular acupuncture points for the treatment of aromatase inhibitor-associated joint pain in women with stage 1–3 estrogen receptor-positive breast cancer, taking medications such as anastrozole, letrozole, or exemestane. Individualization of additional points according to the primary joint(s) involved was allowed, with the core protocol based on an earlier pilot study by the same principal author (Crew et al. 2007). Significant superiority of pain reduction at 6 weeks was observed in the true acupuncture group was noted, according to validated measures of cancer-related pain, as well as various indices of pain traditionally associated with osteoarthritis and rheumatoid arthritis (Crew et al. 2010) . This trial was also favorably reviewed by Lu and Rosenthal (2010) and the initial pilot study was also reviewed positively by Chao et al. (2009) in their broad review of acupoint stimulation for the treatment of various adverse events in breast cancer patients.
Regarding post-operative cancer pain, two high-quality randomized studies have been reviewed by Capodice, including the Pfister trial for acupuncture for pain and xerostomia following neck dissection (Pfister et al. 2010), which has been reviewed extensively (Capodice 2010; Lu and Rosenthal 2010; O’Sullivan and Higginson 2010) and which was discussed in our xerostomia section above. The other such trial reviewed by Capodice includes a randomized, single-blind, sham-controlled efficacy trial by Deng et al. (2008b) (n = 162, Jadad score = 3) of intradermal needle studs at multiple true acupuncture points vs sham points for treatment of post-thoracotomy pain in patients with cancer requiring thoracotomy . Ultimately, no significant difference in pain scores between groups was noted at post-operative day 30. This negative finding was thought to be possibly related to lack of electrical stimulation, short depth of needle stud insertion, and acupuncture point selection, variables which were all different in previous prospective trials that had demonstrated adequate post-operative pain relief in patients undergoing thoracotomy and intra-abdominal surgery (Kotani et al. 2001; Wong et al. 2006).
Mehling et al. (2007) conducted another randomized, non-blinded pragmatic clinical trial (n = 150, Jadad score = 3) examining a combination of acupuncture and Swedish massage vs usual care for post-operative cancer pain, as well as mood symptoms and nausea/vomiting in a heterogeneous cancer patient population. This trial was reviewed in detail by Lu et al. (2008) and partially reviewed for its breast cancer subgroup by Chao et al. (2009) as well as briefly mentioned in the Cochrane review of acupuncture for cancer pain in adults by Paley et al. (2011b). Included patients were at least 18 years old and underwent surgery requiring at least 48 h of inpatient admission for procedures such as mastectomy or reconstructive breast surgery (for breast cancer), abdominal surgery (for intestinal or liver cancer), pelvic surgery (for ovarian, uterine or cervical cancer ), urologic surgery (for cancer of the testicles, prostate, bladder or kidneys) and surgery for head and neck cancer . A 2:1 randomization scheme of intervention to usual care group was employed, to attempt to increase study attractiveness for enrollment purposes, which is expected to slightly decrease statistical power without compromising the overall impact of the study (Dumville et al. 2006). The combination of acupuncture points used on post-operative days 1 and 2 (i.e. LI4, Sanyinjiao (SP6) and various auricular points for pain, PC6 and ST36 for nausea, LI4, Taichong (LR3) and Yintang (EX-HN3) for anxiety, as well as 30 min Swedish massage sessions, ultimately produced significant reduction in pain scores by post-operative day 3 in the intervention group, though significant reduction as compared to the usual care control group was only achieved in the urologic cancer subgroup. Significant improvement in mood was also observed in comparison to the control group (see below), though no significant improvement in nausea/vomiting was observed with this particular intervention.
Regarding other forms of cancer-related pain , such as pain from metastatic disease, cancer-induced bone pain and neuropathic pain , no peer-reviewed, high-quality prospective randomized trials examining acupuncture as treatment have been located in the English language within the past 5 years (Robb et al. 2008; Capodice 2010; Hopkins Hollis 2010; Paley et al. 2011a,b).
15.7 Acupuncture for Fatigue in Cancer Patients
Evidence continues to accumulate that elucidates the multifactorial nature of fatigue often experienced by cancer patients undergoing treatment, as well as the potential of acupuncture as a therapeutic modality for this indication (Johnston et al. 2007a,b). Several high-quality clinical trials, albeit mostly pilot studies, were published in the past 5 years in order to examine the effectiveness of acupuncture for cancer-related fatigue .
One previously reviewed, randomized, double-blinded , sham-controlled efficacy trial was executed by Balk et al. (2009) (n = 27, Jadad score = 5) to examine the utility of electroacupuncture at Taixi (KI3), SP6, LI4, ST36 and (Qihai) CV6) vs sham electroacupuncture for treating fatigue in women with localized cancer (predominantly breast cancer, but one woman with endometrial cancer) that had been treated using surgery , with or without chemotherapy. A trend towards greater improvement in fatigue in the true electroacupuncture group was observed, but the study was apparently underpowered to detect statistical significance, a criticism that was raised by others who reviewed this study (Deng 2009; Capodice 2010). Furthermore, the study groups were observed to have differences in baseline fatigue that were not stratified during randomization , and the trial’s method of double-blinding without actively seeking Deqi sensation was cited by its authors as a confounder that might diminish effect size of the true intervention. Additionally, a three-armed, randomized efficacy trial by Molassiotis et al. (2007) (n = 47, Jadad score = 3) was undertaken to investigate the effect of acupuncture vs true self-acupressure (at LI4, ST36 and SP6) vs sham self-acupressure on fatigue in patients who had completed chemotherapy for various types of cancer. This study was previously reviewed by Lu et al. (2008) as well as Escalante and Manzullo (2009) and demonstrated significant improvement in fatigue for the acupuncture and true self-acupressure groups, both after 2 weeks of treatment and persisting for 2 additional weeks following treatment completion. However, acupuncture was observed to be significantly more effective than either true or sham self-acupressure.
A more recent randomized, non-blinded, prospective feasibility study was conducted by Johnston et al. (2011) (n = 13, Jadad score = 3) to investigate the pragmatic value of acupuncture at multiple points (once weekly treatment for 8 weeks) and wellness education based on integrative medical and social cognitive theory (once weekly for the first 4 weeks) vs usual care in treating cancer-related fatigue . Included patients were female, aged 18–65, with no evidence of disease following completion of treatment for breast cancer, and with a fatigue score of > 4 on the Brief Fatigue Inventory (BFI). Exclusion criteria included any history of depression with score of > 10 on the Hospital Anxiety and Depression Score (HADS), anemia with hemoglobin level < 9 g/dL or hematocrit < 30%, decline in hemoglobin by more than 2 g/dL over the one month preceding the study, active treatment for anemia , or severe limitation in physical functioning (i.e. Karnofsky performance status (KPS) < 70); other potential causes of fatigue (i.e. hypothyroidism and hepatitis) were not criteria for exclusion. A combination of acupuncture and patient education was demonstrated to be beneficial for reducing by 66% according to BFI scores, though this effect did not reach statistical significance (p < 0.10), and changes in secondary outcomes of perceived cognitive impairment were not statistically significant. The lack of statistical significance can be attributed to the small sample size employed in this feasibility trial, and its non-blinded nature may have biased its results. However, the encouraging magnitude of fatigue reduction demonstrated by acupuncture and patient education in this study invites large-scale follow-up trials that are more adequately powered to detect statistical significance in this patient population.
Another recent pilot study employing a randomized, non-blinded pragmatic trial model was undertaken by Lim et al. (2011) (n = 20, Jadad score = 3) to examine the effect of weekly acupuncture vs supportive care guided by a palliative care nurse on multiple symptoms for cancer patients in palliative care . Included patients were age 31–81 with various types of cancer, undergoing palliative care and with at least three months of predicted lifespan remaining, and the interventions were delivered once weekly for 4 weeks. The acupuncture intervention was individualized based on patients’ symptoms, which were reassessed each week with the acupuncture point regimen adjusted accordingly. The nurse-led supportive care involved 20–30 min weekly meetings in which nurses discussed with the patient details regarding symptoms, medications and other therapies, dietary adjustments and medication scheduling changes, and offered emotional support. Improvement in various symptoms (including pain, tiredness, nausea, depression , anxiety , drowsiness, appetite, feeling of well-being and dyspnea) was noted in both groups after each session, with improvement largely persisting at 6 weeks following completion of the 4-week treatment period. No calculations were performed to determine whether any of these changes were statistically significant. However, this study confirmed the feasibility of examining both this particular individualized acupuncture model and the palliative care nurse meeting model in larger scale future clinical trials .
15.8 Acupuncture for Depression, Anxiety, Insomnia and Other Mood-related Symptoms in Cancer Patients
A randomized, non-blinded, fluoxetine-controlled trial (Jadad score = 3) of acupuncture for depression in 80 patients with malignancy , (with 30 pulmonary, 16 gastric and 14 colorectal cancer patients comprising the majority of tumor types) was undertaken (Feng et al. 2011). There was no placebo control, and no overt description of blinding. Primary outcome measures were change in depression score on the Self-rating Depression Scale (SDS) and Hamilton Depression Rating Scale (HAMD) , and change in sleep quality on the Pittsburgh Sleep Quality Index (PSQI). Inclusion criteria were age 18–75, baseline SDS > 50, HAMD > 7 and PSQI > 8, expected survival time > 3 months and absence of mental or intellectual disorders . Exclusion criteria were ongoing use of antidepressants , functional disorders of the heart, liver, kidney and spinal cord , dementia or low education level that precluded understanding of the questionnaires , or KPS < 30 (global assessment of function in cancer patients). Following 30 days of daily treatment with either acupuncture or fluoxetine 20 mg, the study authors reported significant improvement (p < 0.05) in all the measures of SDS, HAMD and PSQI in the acupuncture group. However, fluoxetine and other SSRIs usually require serial dose up-titration (maximal dose 80 mg for Fluoxetine) and a minimum of 4–5 weeks for maximal therapeutic efficacy to be achieved. Hence, a trial with longer follow-up duration and appropriate control dose titration should be attempted. Additionally, methodological reporting concerns regarding the nature of the acupuncture studied also render this study difficult to interpret or reproduce.
As mentioned above, the high-quality study by Mehling et al. (2007) investigating acupuncture and Swedish massage post-operatively for patients with various cancer types demonstrated a significant reduction in depression in comparison to the usual care group, as measured by the Profile of Mood States Short Form (POMS-SF) (Mehling et al. 2007; Lu et al. 2008; Chao et al. 2009). However, no significant improvement in anxiety between intervention and control groups was noted in the above study. The pilot study by Lim et al. (2011) for palliative care patients demonstrated improvement from acupuncture and palliative care nurse-led meetings in many domains of mood and psychological well-being (see above), though the study was not powered or designed to detect statistical significance in these parameters. Also as discussed above, the studies by Hervik and Walker (Hervik and Mjaland 2009, 2010; Walker et al. 2010) on acupuncture for reducing hot flash symptoms in breast cancer patients also showed a significant benefit on depression , sleep disturbance and other mood-related symptoms with adequate control of hot flashes .
15.9 Acupuncture for Chemotherapy-Induced Neutropenia
A randomized, blinded, sham acupuncture-controlled pilot study (Jadad score = 5) was undertaken to investigate the effects of acupuncture on leukopenia (WBC count), neutropenia (ANC count) and serum granulocyte-colony stimulating factor (G-CSF) levels in patients with ovarian cancer , which was the first sham-controlled trial of its kind (Lu et al. 2009). Post-chemotherapy neutropenia in gynecologic cancer patients often jeopardizes intended clinical outcomes by necessitating chemotherapy dose reduction, delayed treatment, inpatient hospitalization and the use of IV antibiotics. Current treatment with G-CSF and GM-CSF is expensive and includes adverse effects such as fever, bone pain , and the acceleration of possible myelodysplasia or acute myeloid leukemia . Patients in this study were over age 18, had newly diagnosed or recurrent ovarian cancer and were on myelo-suppressive chemotherapy (in 3-week cycles) but not on filgrastim or pegfilgrastim, with platelets > 100,000 cells/mL and ANC > 1,000 cells/mL, with regular use of acupuncture within 120 days of the study and no history of psychiatric or cardiac disorders, particularly those requiring a pacemaker.
Acupuncture was administered just prior to and until the end of chemotherapy #2. The study was conducted from the beginning of week 3 (one week prior to starting chemotherapy cycle #2, which is the predicted nadir of WBC/ANC count for cycle #1) to the end of week 6 (end of chemotherapy cycle #2, one week after the predicted WBC/ANC nadir for cycle #2). Significantly lower incidence of severe leukopenia (i.e. grade 2–4) was observed in the true acupuncture arm at the end of cycle #2 (i.e. 30 vs 90% in the sham arm), and the median leukocyte value at this time was significantly higher than that of the control arm (i.e. 8,600 cells/mL vs 4,800 cells/mL). A higher median leukocyte nadir, neutrophil nadir and recovering ANC were observed in the true group, but this trend did not reach statistical significance. Although a fourfold increase in G-CSF levels was noted in the true group at the beginning of cycle #2 (after three acupuncture sessions), this difference was not significant, and no further G-CSF differences were noted at the end of cycle #2 (Lu et al. 2009). This trial was remarkable as a pilot study because of its high quality of both methodological design and STRICTA reporting, and its results suggest that larger scale trials should be undertaken to further investigate the possible benefits of acupuncture on the immune system response during chemotherapy.
15.10 Discussion
In summary, applying rigorous criteria to evaluate the quality of acupuncture clinical trials, we found the most solid evidence came from studies of chemotherapy-related nausea and vomiting. Less strong and mixed evidence was demonstrated in trials on hot flashes, xerostomia and post-operative pain. There are not a sufficient number of trials of reasonable quality to evaluate other indications for acupuncture in cancer care.
As the majority of these trials were published prior to the publication of the new STRICTA guidelines in 2010, it is expected that many of these earlier trials would not conform to the reporting practices encouraged by the STRICTA criteria. However, we also expect that many more trials in the future will observe these reporting criteria, as familiarity with the STRICTA guidelines increases among acupuncture researchers. It is our hope that increased use of these criteria will expand the generalizability and reproducibility of future study results.
Price et al. (2011) have commented on the fact that reporting of acupuncture rationale has yet to be standardized and varies widely from paper to paper, even in the face of increasing conformity to STRICTA reporting guidelines. Design, execution and reporting acupuncture rationale in further clinical trial publications is mandatory to appropriately differentiate among different modes, styles and depths of needle stimulation in order to avoid inappropriate grouping of disparate acupuncture styles during systematic reviews and meta-analysis . And of course, general issues for all acupuncture trials remain regarding methodological variation (i.e. point selection, frequency of treatment, acupuncture style, operator skill and ancillary stimulation modalities such as manual force, moxibustion, electricity and massage), an incomplete understanding of the physiologic mechanisms through which the acupuncture encounter and the needles themselves exert their effects, the non-inert nature of sham acupuncture (as invoked by mechanoreceptor stimulation of even gentle touch such as is employed in Japanese styles) and the apparently larger non-specific effect size of acupuncture and other procedures (i.e. surgery, other devices or manual manipulations) in comparison to placebo pills used in drug trials. Such challenges may well continue to represent the most difficult obstacles to overcome in terms of future clinical trial design and distillation of evidence that will ultimately help guide clinical practice and reduce the suffering of patients with cancer.
The 2007 Society for Acupuncture Research (SAR) international symposium on acupuncture research was attended by 300 acupuncture researchers, practitioners, students, funding agency personnel, and health policy analysts from 20 countries (Park et al. 2008). Among the presentations and discussions, two paradoxes emerged. First, a number of well-designed clinical trials found that true acupuncture is superior to usual care, but did not significantly outperform sham acupuncture . Second, although many experimental studies showed that the mode of needling is associated with various physiological effects, whether these changes influence therapeutic outcomes in clinical trials is unclear. A White Paper was issued to identify gaps in knowledge underlying the paradoxes and proposes strategies for their resolution through translational research (Langevin et al. 2011). We endorse the recommendations in the White Paper that future research should focus on a “whole systems” approach and on mechanistic studies. The studies may incorporate consideration of efficacy and effectiveness and may include qualitative measures.
References
WHO. (1990). A standard international acupuncture nomenclature: Memorandum from a WHO meeting. Bulletin of the World Health Organization, 68, 165–169.
Alimi, D., Rubino, C., Pichard-Leandri, E., Fermand-Brule, S., Dubreuil-Lemaire, M. L., Hill, C. (2003). Analgesic effect of auricular acupuncture for cancer pain: A randomized, blinded, controlled trial. Journal of Clinical Oncology, 21, 4120–4126.
Balk, J., Day, R., Rosenzweig, M., Beriwal, S. (2009). Pilot, randomized, modified, double-blind, placebo-controlled trial of acupuncture for cancer-related fatigue. Journal of the Society for Integrative Oncology, 7, 4–11.
Blom, M., Dawidson, I., Fernberg, J. O., Johnson, G., Angmar-Mansson, B. (1996). Acupuncture treatment of patients with radiation-induced xerostomia. European Journal of Cancer Part B, Oral Oncology, 32B, 182–190.
Capodice, J. L. (2010). Acupuncture in the oncology setting: Clinical trial update. Current Treatment Options in Oncology, 11, 87–94.
Chao, L. F., Zhang, A. L., Liu, H. E., Cheng, M. H., Lam, H. B., Lo, S. K. (2009). The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: A systematic review. Breast Cancer Research and Treatment, 118, 255–267.
Chen, Z. J., Guo, Y. P., Wu, Z. C. (2008). Observation on the therapeutic effect of acupuncture at pain points on cancer pain. Zhongguo Zhen Jiu, Chinese Acupuncture and Moxibustion, 28, 251–253.
Cho, J. H., Chung, W. K., Kang, W., Choi, S. M., Cho, C. K., Son, C. G. (2008). Manual acupuncture improved quality of life in cancer patients with radiation-induced xerostomia. Journal of Alternative and Complementary Medicine, 14, 523–526.
Clark, H. D., Wells, G. A., Huet, C., Mc Alister, F. A., Salmi, L. R., Fergusson, D., Laupacis, A. (1999). Assessing the quality of randomized trials: Reliability of the Jadad scale. Controlled Clinical Trials, 20, 448–452.
Crew, K. D., Capodice, J. L., Greenlee, H., Apollo, A., Jacobson, J. S., Raptis, G., Blozie, K., Sierra, A., Hershman, D. L. (2007). Pilot study of acupuncture for the treatment of joint symptoms related to adjuvant aromatase inhibitor therapy in postmenopausal breast cancer patients. Journal of Cancer Survivorship, 1, 283–291.
Crew, K. D., Capodice, J. L., Greenlee, H., Brafman, L., Fuentes, D., Awad, D., Yann Tsai, W., Hershman, D. L. (2010). Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. Journal of Clinical Oncology, 28, 1154–1160.
Dang, W., Yang, J. (1998). Clinical study on acupuncture treatment of stomach carcinoma pain. Journal of Traditional Chinese Medicine, 18, 31–38.
Deng, G. (2009). Acupuncture for fatigue during radiation therapy: Points made. Journal of the Society for Integrative Oncology, 7, 1–3.
Deng, G., Vickers, A., Simon Yeung, K., Cassileth, B. R. (2006). Acupuncture: Integration into cancer care. Journal of the Society for Integrative Oncology, 4, 86–92.
Deng, G., Vickers, A., Yeung, S., D’Andrea, G. M., Xiao, H., Heerdt, A. S., Sugarman, S., Troso-Sandoval, T., Seidman, A. D., Hudis, C. A., Cassileth, B. (2007). Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. Journal of Clinical Oncology, 25, 5584–5590.
Deng, G., Hou, B. L., Holodny, A. I., Cassileth, B. R. (2008a) Functional magnetic resonance imaging (fMRI) changes and saliva production associated with acupuncture at LI-2 acupuncture point: A randomized controlled study. BMC Complementary and Alternative Medicine, 8, 37.
Deng, G., Rusch, V., Vickers, A., Malhotra, V., Ginex, P., Downey, R., Bains, M., Park, B., Rizk, N., Flores, R., Yeung, S., Cassiletha, B. (2008b). Randomized controlled trial of a special acupuncture technique for pain after thoracotomy. The Journal of Thoracic and Cardiovascular Surgery, 136, 1464–1469.
Dumville, J. C., Hahn, S., Miles, J. N., Torgerson, D. J. (2006). The use of unequal randomisation ratios in clinical trials: A review. Contemporary Clinical Trials, 27, 1–12.
Enblom, A., Johnsson, A., Hammar, M., Onelov, E., Steineck, G., Borjeson, S. (2012). Acupuncture compared with placebo acupuncture in radiotherapy-induced nausea—a randomized controlled study. Annals of Oncology, 23, 1353–1361.
Ernst, E., Lee, M. S. (2010). Acupuncture for palliative and supportive cancer care: A systematic review of systematic reviews. Journal of Pain and Symptom Management, 40, e3–5.
Escalante, C. P., Manzullo, E. F. (2009). Cancer-related fatigue: The approach and treatment. Journal of General Internal Medicine, 24, S412–S416.
Ezzo, J. M., Richardson, M. A., Vickers, A., Allen, C., Dibble, S. L., Issell, B. F., Lao, L., Pearl, M., Ramirez, G., Roscoe, J., Shen, J., Shivnan, J. C., Streitberger, K., Treish, I., Zhang, G. (2006). Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database System Review, 2, CD002285.
Feng, Y., Wang, X. Y., Li, S. D., Zhang, Y., Wang, H. M., Li, M., Cao, K., Ye, Y. F., Zhang, Z. (2011). Clinical research of acupuncture on malignant tumor patients for improving depression and sleep quality. Journal of Traditional Chinese Medicine, 31, 199–202.
Frisk, J., Carlhall, S., Kallstrom, A. C., Lindh-Astrand, L., Malmstrom, A., Hammar, M. (2008). Long-term follow-up of acupuncture and hormone therapy on hot flushes in women with breast cancer: A prospective, randomized, controlled multicenter trial. Climacteric, 11, 166–174.
Frisk, J., Kallstrom, A. C., Wall, N., Fredrikson, M., Hammar, M. (2012). Acupuncture improves health-related quality-of-life (HRQoL) and sleep in women with breast cancer and hot flushes. Supportive Care in Cancer, 20, 715–724.
Frisk, J., Spetz, A. C., Hjertberg, H., Petersson, B., Hammar, M. (2009). Two modes of acupuncture as a treatment for hot flushes in men with prostate cancer—a prospective multicenter study with long-term follow-up. European Urology, 55, 156–163.
Gottschling, S., Reindl, T. K., Meyer, S., Berrang, J., Henze, G., Graeber, S., Ong, M. F., Graf, N. (2008). Acupuncture to alleviate chemotherapy-induced nausea and vomiting in pediatric oncology—a randomized multicenter crossover pilot trial. Klinische Padiatrie, 220, 365–370.
Hervik, J., Mjaland, O. (2009). Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Research and Treatment, 116, 311–316.
Hervik, J., Mjaland, O. (2010). Quality of life of breast cancer patients medicated with anti-estrogens, 2 years after acupuncture treatment: A qualitative study. International Journal of Women’s Health, 2, 319–325.
Holmberg, L., Iversen, O. E., Rudenstam, C. M., Hammar, M., Kumpulainen, E., Jaskiewicz, J., Jassem, J., Dobaczewska, D., Fjosne, H. E., Peralta, O., Arriagada, R., Holmqvist, M., Maenpaa, J. (2008). Increased risk of recurrence after hormone replacement therapy in breast cancer survivors. Journal of the National Cancer Institute, 100, 475–482.
Hopkins Hollis, A. S. (2010). Acupuncture as a treatment modality for the management of cancer pain: The state of the science. Oncology Nursing Forum, 37, E344–E348.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., McQuay, H. J. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials, 17, 1–12.
Johnston, M. F., Xiao, B., Hui, K. K. (2007a). Acupuncture and fatigue: Current basis for shared communication between breast cancer survivors and providers. Journal of Cancer Survivorship, 1, 306–312.
Johnston, M. F., Yang, C., Hui, K. K., Xiao, B., Li, X. S., Rusiewicz, A. (2007b). Acupuncture for chemotherapy-associated cognitive dysfunction: A hypothesis-generating literature review to inform clinical advice. Integrative Cancer Therapies, 6, 36–41.
Johnston, M. F., Hays, R. D., Subramanian, S. K., Elashoff, R. M., Axe, E. K., Li, J. J., Kim, I., Vargas, R. B., Lee, J., Yang, L., Hui, K. K. (2011). Patient education integrated with acupuncture for relief of cancer-related fatigue randomized controlled feasibility study. BMC Complementary and Alternative Medicine, 11, 49.
Kotani, N., Hashimoto, H., Sato, Y., Sessler, D. I., Yoshioka, H., Kitayama, M., Yasuda, T., Matsuki, A. (2001). Preoperative intradermal acupuncture reduces postoperative pain, nausea and vomiting, analgesic requirement, and sympathoadrenal responses. Anesthesiology, 95, 349–356.
Langevin, H. M., Wayne, P. M., Macpherson, H., Schnyer, R., Milley, R. M., Napadow, V., Lao, L., Park, J., Harris, R. E., Cohen, M., Sherman, K. J., Haramati, A., Hammerschlag, R. (2011). Paradoxes in acupuncture research: Strategies for moving forward. Evidence-Based Complementary and Alternative Medicine, 2011, 180805.
Lee, A., Fan, L. T. (2009). Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database System Review, 2, CD003281.
Lee, M. S., Kim, K. H., Choi, S. M., Ernst, E. (2009a). Acupuncture for treating hot flashes in breast cancer patients: A systematic review. Breast Cancer Research and Treatment, 115, 497–503.
Lee, M. S., Kim, K. H., Shin, B. C., Choi, S. M., Ernst, E. (2009b). Acupuncture for treating hot flushes in men with prostate cancer: A systematic review. Supportive Care in Cancer, 17, 763–770.
A., Lekander, M., Hammar, M., Johnsson, A., Onelov, E., Ingvar, M., Steineck. G., Borjeson, S. (2011). Getting the grip on nonspecific treatment effects: Emesis in patients randomized to acupuncture or sham compared to patients receiving standard care. PloS One, 6, e14766.
Liljegren, A., Gunnarsson, P., Landgren, B. M., Robeus, N., Johansson, H., Rotstein, S. (2010). Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant tamoxifen: A randomized controlled trial. Breast Cancer Research and Treatment, doi:10.1007/s10549–010-1283–3.
Lim, J. T., Wong, E. T., Aung, S. K. (2011). Is there a role for acupuncture in the symptom management of patients receiving palliative care for cancer? A pilot study of 20 patients comparing acupuncture with nurse-led supportive care. Acupuncture in Medicine, 29, 173–179.
Lu, W., Dean-Clower, E., Doherty-Gilman, A., Rosenthal, D. S. (2008). The value of acupuncture in cancer care. Hematology/Oncology Clinics of North America, 22, 631–648.
Lu, W., Matulonis, U. A., Doherty-Gilman, A., Lee, H., Dean-Clower, E., Rosulek, A., Gibson, C., Goodman, A., Davis, R. B., Buring, J. E., Wayne, P. M., Rosenthal, D. S., Penson, R. T. (2009). Acupuncture for chemotherapy-induced neutropenia in patients with gynecologic malignancies: A pilot randomized, sham-controlled clinical trial. Journal of Alternative and Complementary Medicine, 15, 745–753.
Lu, W., Rosenthal, D. S. (2010). Recent advances in oncology acupuncture and safety considerations in practice. Current Treatment Options in Oncology, 11, 141–146.
MacPherson, H., Altman, D. G., Hammerschlag, R., Youping, L., Taixiang, W., White, A., Moher, D. (2010). Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. Journal of Evidence-Based Medicine, 3, 140–155.
Mehling, W. E., Jacobs, B., Acree, M., Wilson, L., Bostrom, A., West, J., Acquah, J., Burns, B., Chapman, J., Hecht, F. M. (2007). Symptom management with massage and acupuncture in postoperative cancer patients: A randomized controlled trial. Journal of Pain and Symptom Management, 33, 258–266.
Meng, Z., Garcia, M. K., Hu, C., Chiang, J., Chambers, M., Rosenthal, D. I., Peng, H., Zhang, Y., Zhao, Q., Zhao, G., Liu, L., Spelman, A., Palmer, J. L., Wei, Q., Cohen, L. (2012). Randomized controlled trial of acupuncture for prevention of radiation-induced xerostomia among patients with nasopharyngeal carcinoma. Cancer, 118, 3337–3344.
Minton, O., Higginson, I. J. (2007). Electroacupuncture as an adjunctive treatment to control neuropathic pain in patients with cancer. Journal of Pain and Symptom Management, 33, 115–117.
Molassiotis, A., Sylt, P., Diggins, H. (2007). The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: A randomised controlled trial. Complementary Therapies in Medicine, 15, 228–237.
O’Sullivan, E. M., Higginson, I. J. (2010). Clinical effectiveness and safety of acupuncture in the treatment of irradiation-induced xerostomia in patients with head and neck cancer: A systematic review. Acupuncture in Medicine, 28, 191–199.
Paley, C. A., Bennett, M. I., Johnson, M. I. (2011a). Acupuncture for cancer-induced bone pain? Evidence-Based Complementary and Alternative Medicine, 2011, 671043.
Paley, C. A., Johnson, M. I., Tashani, O. A., Bagnall, A. M. (2011b). Acupuncture for cancer pain in adults. Cochrane Database System Review, 1, CD007753.
Park, J., Linde, K., Manheimer, E., Molsberger, A., Sherman, K., Smith, C., Sung, J., Vickers, A., Schnyer, R. (2008). The status and future of acupuncture clinical research. Journal of Alternative and Complementary Medicine, 14, 871–881.
Pfister, D. G., Cassileth, B. R., Deng, G. E., Yeung, K. S., Lee, J. S., Garrity, D., Cronin, A., Lee, N., Kraus, D., Shaha, A. R., Shah, J., Vickers, A. J. (2010). Acupuncture for pain and dysfunction after neck dissection: Results of a randomized controlled trial. Journal of Clinical Oncology, 28, 2565–2570.
Price, S., Long, A. F., Godfrey, M., Thomas, K. J. (2011). Getting inside acupuncture trials—exploring intervention theory and rationale. BMC Complementary and Alternative Medicine, 11, 22.
Rada, G., Capurro, D., Pantoja, T., Corbalan, J., Moreno, G., Letelier, L. M., Vera, C. (2010). Non-hormonal interventions for hot flushes in women with a history of breast cancer. Cochrane Database System Review, 9, CD004923.
Robb, K. A., Bennett, M. I., Johnson, M. I., Simpson, K. J., Oxberry, S. G. (2008). Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults. Cochrane Database System Review, 3, CD006276.
Sagar, S. M. (2008). Acupuncture as an evidence-based option for symptom control in cancer patients. Current Treatment Options in Oncology, 9, 117–126.
Stone, J. A., Johnstone, P. A. (2010). Mechanisms of action for acupuncture in the oncology setting. Current Treatment Options in Oncology, 11, 118–127.
Walker, E. M., Rodriguez, A. I., Kohn, B., Ball, R. M., Pegg, J., Pocock, J. R., Nunez, R., Peterson, E., Jakary, S., Levine, R. A. (2010). Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: A randomized controlled trial. Journal of Clinical Oncology, 28, 634–640.
Wang, X. Q., Yu, J. L., Du, Z. Y., Xu, R., Jiang, C. C., Gao, X. (2010). Electroacupoint stimulation for postoperative nausea and vomiting in patients undergoing supratentorial craniotomy. Journal of Neurosurgical Anesthesiology, 22, 128–131.
Wong, R. H., Lee, T. W., Sihoe, A. D., Wan, I. Y., Ng, C. S., Chan, S. K., Wong, W. W., Liang, Y. M., Yim, A. P. (2006). Analgesic effect of electroacupuncture in postthoracotomy pain: A prospective randomized trial. The Annals of Thoracic Surgery, 81, 2031–2036.
Xia, Y. Q., Zhang, D., Yang, C. X., Xu, H. L., Li, Y., Ma, L. T. (1986). An approach to the effect on tumors of acupuncture in combination with radiotherapy or chemotherapy. Journal of Traditional Chinese Medicine, 6, 23–26.
You, Q., Yu, H., Wu, D., Zhang, Y., Zheng, J., Peng, C. (2009). Vitamin B6 points PC6 injection during acupuncture can relieve nausea and vomiting in patients with ovarian cancer. International Journal of Gynecological Cancer, 19, 567–571.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Deng, G., Seto, D., Cassileth, B. (2012). Recent Clinical Trials of Acupuncture for Cancer Patients. In: Cho, W. (eds) Acupuncture and Moxibustion as an Evidence-based Therapy for Cancer. Evidence-based Anticancer Complementary and Alternative Medicine, vol 3. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4833-0_15
Download citation
DOI: https://doi.org/10.1007/978-94-007-4833-0_15
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4832-3
Online ISBN: 978-94-007-4833-0
eBook Packages: MedicineMedicine (R0)