Abstract
Acupuncture within an oncology setting carries specific risks and potential benefits that may be attained through needling of soft, mostly superficial tissue. This chapter brings up-to-date clinical and basic research. It is divided in one session where the contra-indications of needling are discussed and few sessions regarding it’s use for specific side effects of cancer therapy as well as its probable mechanisms of action. To this point, acupuncture has been studied and applied for management of pain and specific oncologic treatment side-effects, namely post-chemotherapy nausea and vomiting , aromatase-inhibitor related arthralgia , hot flashes secondary to hormonal blockage, oncological fatigue, xerostomia and chemotherapy induced peripheral neuropathy. Clinical research has faced serious difficulties mostly influenced by small sample sizes and mixed protocols regarding different point selection. Nevertheless, a few high quality papers have been able to provide some reassuring evidence of substantial benefits especially within the patients’ referred quality of life aspects. Although the mechanisms of action are not completely unveiled yet, this is a promising field for acupuncture research and practice with much interest from the specialised media as well as from the general public.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cancer
- Oncology
- Neoplasm
- Nausea
- Vomiting
- Neuropathy
- Aromatase-inhibitor related arthralgia
- Hot flashes
- Fatigue
- Xerostomia
- Chemotherapy
1 Introduction
Acupuncture use within the field of oncology has been experiencing a steady growth in the last decade, shown by recent surveys among cancer patients of great cancer centers around the world and also by the increasing amount of research papers published in the scientific media.
Currently, this is a promising field of research with many published studies in scientific periodicals investigating the possible benefits of this traditional art of healing for cancer patients.
Interesting enough, acupuncture use remains within the realms of complementary medicine and its application serves, as adjunct therapy for optimizing the symptom control in this specific population, a very special group of patients that must endure a constellation of bothersome symptoms, be it from the underlying disease or from its aggressive treatment regimen.
It is not uncommon for patients to visit the cancer center where they are being treated 3–5 times a week in order to be submitted to therapies, medical consultations, medical imaging and blood exams. Usually they comply with every assignment with little room for discussion once the majority of them are terrified with the oncological diagnosis.
To add a complementary therapy may help with the overall well-being but it may also consume otherwise precious down time with family and friends.
Being a complementary therapy implies that the risk-benefit ratio has to be fully accessed on a shared decision basis with the patient. This should happen in order to establish priorities and targets for symptom control as well as to exclude futile procedures that may prevent other more meaningful actions to be taken.
As in every other field of medicine , the patients must be aware of the possible benefits and limitations of acupuncture , they have to understand the amount of time and money that will be invested, the possible adverse events and compare those to the beneficial outcomes that may be reached. The resulting ratio must be of significant importance for the patients.
To clarify the above mentioned, let us analyze two cases that may be seen not so eventually in practice:
56 years old woman who was diagnosed with breast cancer one year ago in a screening mammography. She was submitted to biopsy, neoadjuvant chemotherapy, underwent total mastectomy with axillary lymph node extraction, local radiotherapy and finally was put on hormonal blockage with tamoxifen.
She is now a “cancer survivor”, enduring post-mastectomy pain that prevents her to raise her arm higher than her chest and suffers from hot flashes that wake her up 5 times each night soaking wet from perspiration due to the hormonal blockage that is supposed to last at least 5 more years.
She has been trying to regain her upper limb functionality with physiotherapy and occupational therapy but the pain she feels prevents her to advance in the treatments although the pain medicine regimen is optimized. She is also not a candidate to hormonal treatment for the hot flashes and the currently available pharmacotherapies (serotonin re-uptake inhibitors and gabapentin) have not helped her.
This patient would be a great candidate for acupuncture since such pain and hot flashes could be relieved to some extent according to recently published research and she should be referred to a licensed acupuncturist to discuss such possibilities.
Now a second case, a 42 years old man who has a background of drug abuse (namely Ketamine and Ecstasy), suffered an ischemic stroke fifteen years ago without any identifiable cause at the time, which resulted in minor loss of motor strength in the right leg. A few months back, he presented with a deep venous thrombosis in such leg as well as dyspnea, which was first attributed to a possible pulmonary thromboembolism but initial pulmonary images refuted this hypothesis and suggested pneumonia.
Unfortunately, that did not resolve under usual antibiotic therapy and latter was diagnosed as a locally advanced small cell lung cancer with bone metastasis to the lumbar vertebrae. During this investigation he was also diagnosed with acquired immunodeficiency syndrome (AIDS) with low CD4 count and high viral load.
He is now under aggressive chemotherapy treatment, is scheduled to receive local lumbar radiotherapy, and uses enoxaparin for anticoagulation and antiretroviral medication.
Although he suffers from lumbar pain due to the bone metastasis it does subsides with the use of non-steroidal anti-inflammatories. Even if he chooses to search treatment for his pain with acupuncture , once he’s had a previous good experience with it, the risk-benefit ratio is poorly acceptable since the possibilities of bleeding, infections and loss of precious time are far greater than the eventual benefit of reducing the amount of anti-inflammatory drugs that he needs to control his pain.
Exposing the risk-benefit rational in each setting should help attain a shared decision whether or not to undertake the acupuncture treatment, and in order to do so, one must be aware of the current knowledge in the field.
2 Clinical Application
2.1 Contra-Indications and Cautions When Needling a Cancer Patient
Neutropenia
Neutropenia is a condition where the absolute neutrophil count (ANC) drops below 1500 per mm3. This is associated with a higher risk of developing an infection either viral or bacterial, the lower the ANC the greater the risk.
In the oncology setting the neutropenia is usually caused by the chemotherapy, but it can also be due to radiotherapy that impairs the bone marrow production (i.e. radiotherapy to the chest that reaches the sternum bone marrow) or in critical cases where the bone marrow is invaded by metastatic cancer cells.
When due to chemotherapy it is usually transient, its beginning and duration can be predicted according to the drug that is being used so the needling can be postponed.
Mild neutropenia (ANC between 1500 and 1000 per mm3) is still an acceptable scenario for needling but moderate to severe neutropenia (ANC below 1000 per mm3) carries an important risk of spontaneous development of febrile conditions and needling should be refrained once any bruise to the skin might facilitate a local organism to initiate an infection.
Thrombocytopenia
Thrombocytopenia is a condition where the platelets count fall below 150.000 platelets per mm3. Platelets are an important coagulation factor specially when dealing with needle punctures once platelets stop bleeding by binding together to form plugs in blood vessel injuries.
Platelets count below 100.000 per mm3 demands a cautious superficial needling and a 5 min observation after the removal of the needles is advised. Below 50.000 per mm3 the risk of uncontrolled bleeding increases to the point where needling becomes contra-indicated.
Anticoagulation Therapy or Coagulation Disorders
Anticoagulation therapy is not uncommon within the oncology population since it is an important measure to prevent and treat deep vein thrombosis as well as pulmonary thromboembolisms.
Coagulation disorders may be present in cancer patients due to anticoagulation factors produced or even normal coagulation factors impaired by neoplasms products, usually a coagulation laboratory test that measures prothrombin and activated partial thromboplastin times (PT and aPTT) showing a PT with a International Normalized Ratio (INR) lower than 2.0 and a aPTT faster than 60 s are enough to provide a certain safety for needling.
Warfarin is usually administered in situations where long-term anticoagulation is warranted and the intensity of its action can be measured through PT expressed in terms INR. Cautious superficial needling and a 5 min observation after the removal of the needles is advised in patients receiving warfarin that present with an INR between 1.0 and 2.0. Further alteration of PT may pose a threat of high volume bruise formations and needling should be avoided.
Enoxaparin is very common in practice and other newly available medications like Xarelto are rapidly becoming mainstream practice. These substances also present laboratory tests that can measure its action but they vary from drug to drug, so a very reliable indication of safety for needling is the objective sought with the prescribing of such drugs. A prophylactic prescription regimen is a safe needling situation whereas a treatment prescription regimen (i.e. established deep vein thrombosis or pulmonary thromboembolism) contra-indicates deep needling.
Lymphedema
Patients submitted to lymph node extraction or those presenting lymph node metastasis may develop lymphedema. These situations impair the normal lymph circulation slowing the drainage from limbs and the normal reaction to local infections. Limbs with lymphedema must not be needled and alternative points located elsewhere should be used to prevent local complications. Although a high quality pilot study (Cassileth et al. 2013) suggested that needling limbs with lymphedema is actually safe, this unfortunately has not been replicated so far and is still not considered mainstream practice (Fig. 1).
Tumor Sites and Bone Metastasis
Local needling is dangerous and must be avoided as tumors produce chaotic blood vessel formations. Bleeding may become uncontrollable and local infections may be difficult to treat.
Bone metastasis, especially to vertebrae may generate instability and local muscles can be tense in order to maintain stability, needling these local muscles may further increase the instability, risk of fractures and even medullar compression and therefore should be avoided.
There is even a possibility of local tumor spread induced by local needling as reported by a Taiwanese team from the Changhua Christian Hospital (Tseng et al. 2011) describing an event of post-acupuncture cutaneous spread of metastatic breast cancer after the puncture of a tender cervical mass that was probably deemed an “Ashi point” but, in reality, was a metastatic mass.
Prosthesis
Some patients present with metallic endoprosthesis due to bone metastasis that was removed or even due to fractures. These locations should not be needled once local infections would be very difficult to treat and could even need surgical intervention for removal of infected material (Table 1).
3 The Use of Acupuncture in Specific Side Effects of Usual Cancer Care
Nausea and Vomiting
Chemotherapy induced emesis (CIE) is one of the most acute distressing side-effects of cancer treatment, it can happen in up to 80% of patients with significant effects on quality of life and possible complications like metabolic derangements, dehydration, nutritional deficiency, esophageal tears and eventually may limit one’s tolerance to comply with the chemotherapy regimen (Fernández-Ortega et al. 2012).
Although the use of plural antiemetic medication regimens have been able to reduce the incidence of vomiting , nausea remains as one of the most severe side effects experienced by those undergoing Chemotherapy (Coates et al. 1983).
A few risk factors for CIE have been identified, for example female sex and previous history of motion sickness (de Boer-Dennert et al. 1997), as well as characteristics related to the treatment regimen like dosage and frequency.
The major subtypes of CIE are:
-
Acute: onset of nausea and vomiting within minutes to hours after administration of chemotherapy and resolving within 24 h
-
Delayed: occurs 24 h or later after administration of chemotherapy
-
Anticipatory: occurs before chemotherapy administration; thought to be an indicator of previous poor control of nausea and vomiting
-
Breakthrough/refractory: nausea and vomiting that occur despite appropriate prophylaxis; requires the use of rescue medications.
Current medication available to control CIE includes 5-HT3 receptor antagonists (i.e. Ondansetron), NK1 receptor antagonists (i.e. Aprepitant), Corticosteroids (i.e. Dexamethasone), Dopamine receptor antagonists (i.e. Metoclopramide) and eventually Benzodiazepines, Olanzapine and more recently Cannabinoids.
Acupuncture has been deemed useful for nausea and vomiting control for a long time now and in 1998, a National Institutes of Health consensus panel reported acupuncture was effective in controlling postoperative pain and chemotherapy-related nausea and vomiting (NIH Consensus Conference 1998). Despite being far from establishing itself as standard treatment, acupuncture for nausea/vomiting is a safe treatment that can relieve distress and may be an option for patients who do not achieve significant symptom control with medications listed above.
Of notice, Electroacupuncture for Control of Myeloablative Chemotherapy-Induced Emesis: A Randomized Controlled Trial (Shen 2000) is a high quality study with a low risk of bias that examined the antiemetic effects of electroacupuncture (EA) on breast cancer patients admitted to hospital wards that were receiving myeloablative chemotherapy.
The study consisted of 104 patients divided in 3 groups, all patients received the same triple pharmacological agents for emesis management, which included prochlorperazine, lorazepam and diphenhydramine hydrochloride. These medications were started 1 h prior to chemotherapy and were continued until 48 h after the last chemotherapy infusion. Rescue medications that were available to all patients included additional prochlorperazine, lorazepam, and diphenhydramine, as well as metoclopramide and droperidol.
The EA group (37 patients) received two sessions per day during 5 consecutive days, needles were placed on PC 6 and ST 36 with initial manipulation searching for DeQi, then the electrodes were connected (negative on PC 6 and positive on ST 36), Electrical frequency was delivered over 2–10 Hz, 0.5–0.7 ms duration pulse width, under a variable direct current output with square wave-form balanced alternating polarity of less than 26 mA for 20 min (Figs. 2 and 3).
The “placebo” group (33 patients) received minimal needling meaning that the needles were placed subcutaneously and without stimulation near the sites of LU 7 and GB 34, electrodes were connected and the machine would generate the same audiovisual effects but no electrical stimulus during 20 min.
The Medication group (34 patients) only received the medication regimen described above.
The number of emesis episodes per person along the 5 days of intervention was counted and the median was 5 episodes for the EA group, 10 episodes for the Minimal Needling group and 15 episodes for the pharmacotherapy alone group.
Statistical analysis showed that the EA group had significantly fewer emesis episodes than the minimal needling group or the pharmacotherapy alone group. Also, the minimal needling group had significantly fewer emesis episodes than the pharmacotherapy alone group.
This stands as a very strong evidence of acupuncture value in post-chemotherapy nausea and vomiting prevention.
4 Probable Mechanisms of Action—Nausea and Vomiting
The consensus points for treating nausea and vomiting are PC 6 and ST 36, although PC 6 neuroanatomical and specific molecular profile correlation to this perceived effect is unclear, some hypothesis have been formulated for the effectiveness of ST 36.
Cheng (2009) postulated that ST 36 needling may elicit a potent somato-autonomic reflex and thus modulate gastric activity once this has been shown by Sato and Schmidt (1987) and Sato (1997) where the stimulation of the muscles in the hindpaw of anaesthetised rats increased gastric vagal efferent nerve activity and increased gastric motility. To further establish this hypothesis, Cheng KJ present us the study (Wang et al. 2007) on the regulation of gastric activity by acupuncture at ST36 where the vagus nerve implication is clear once a bilateral vagotomy essentially abolishes the effect.
Somato-parasympathetic reflex is a possible mechanism of Nausea and Vomiting control effect. Needling would generate the somatic sensory stimulation that is conducted by the muscle afferent fibres to the medullary reflex center, and eventually the efferent parasympathetic nerves that innervate the stomach elicit the gastric response.
Hot Flashes
Hot Flashes (HFs), also referred to as Vasomotor symptoms are a sensation of heat flushing over the body surface, often accompanied by heart palpitations, spontaneous sweating, nausea, dizziness, mood and sleep disturbances. HFs usually happens a few times per day and night but some patients may present as many as hourly episodes lasting from 3 to 20 min. These symptoms may persist for years and can affect work, social activities, concentration, energy levels, and overall quality of life.
HFs are a common complaint among cancer patients specially those that underwent surgical castration and hormone therapy. Although quite frequent, 80% of women receiving Tamoxifen present those symptoms, only about 21% of the patients receive treatment for such ailment.
Despite the exact mechanism being unknown, It has been suggested that HFs due to hormonal changes may be related to a reduced concentration of b-endorphin in the hypothalamus, which leads to a drop in the set point of the thermoregulation center and increased release of calcitonin gene–related peptide, a potent vasodilator.
In general practice the usual care would be hormone replacement therapy but in the context of estrogen receptor–positive cancer this is not advisable and the options are narrowed to antidepressants and gabapentin which may present some relief but may also cause unpleasant side effects as nausea, drowsiness, dizziness, dry mouth, or headache.
Many cancer patients turn to integrative practices to help manage hot flashes and acupuncture is often prescribed.
The most recent systematic review of the use of acupuncture for the management of HFs in cancer patients (Garcia et al. 2015) identified 8 high quality RCTs. All studies showed significant within-group improvement from the baseline to the end of treatment for true acupuncture which is an important finding since spontaneous improvement is not likely once 50% of women with breast cancer report HFs lasting 10 years after menopause. Although the major concern regarding this particular review is the fact that none of the included trials presented a low Risk Of Bias preventing the achievement of definitive conclusions, the analyzed studies present some interesting strategies to treat this particular condition.
Characteristics of Studies Included
Psychological well-being improves in women with breast cancer after treatment with applied relaxation or electro-acupuncture for vasomotor symptom (Nedstrand et al. 2006).
Investigators used Electroacupuncture (EA) on a standard set of points for 30 min twice a week for 2 weeks then once a week for 10 more weeks.
EA | BL23 BL32 | GV20 | BL15 | HT7 | SP6 | SP9 | LR3 | PC6 |
Actually EA was performed on BL23 and BL32 with 2 Hz, the other points were only manually stimulated.
The control group was submitted to weekly 60 min applied-relaxation sessions for 12 weeks.
This paper had a small number of subjects (n = 38) and performed a long period of follow-up (6 months) with vasomotor symptoms being recorded daily and mood and psychological well-being scales applied during follow-up visits.
Results showed no significant differences were between groups. Both showed a significant decrease in number of HFs/24 h as well as a significant psychological well-being increase from the baseline in both groups.
This paper suggests that both interventions may be of benefit and further investigations could contribute to develop such strategies.
Two modes of acupuncture as a treatment for hot flushes in men with prostate cancer —a prospective multicenter study with long-term follow-up (Frisk et al. 2009).
This paper opted to further investigate the same point selection described in the previous study but this time the comparison was between manual and electroacupuncture, besides the fact that this was a study conducted in men. Two groups were differentiated only regarding the presence or absence of electrostimulation on BL23 and BL32. Sessions happened twice a week for 2 weeks and then once a week for 10 more weeks.
The number of participants was once again small (n = 31) and as an improvement the outcomes also included a HF scale and dosing of Calcitonin gene-related peptide (CGRP) in the subjects 24 h urine samples besides the usual HF diaries.
Results showed that both groups attained significant reductions in number of HFs/24 h (74% for EA and 69% for Manual after 12 wk) as well as in the HF score (78% for EA and 73% for Manual after 12 wk).
Both EA and Manual acupuncture had a persistent significant effect over time maintaining effect up to 9 months after the start of treatment, CGRP urine measures did present a decrease but this was not statistically significant.
Although this paper lacks the presence of a placebo group on a non-treated group the authors claim that previous studies have shown that a placebo pill can contribute to a maximum of 20–30% decrease in the number of HF/24 h and wouldn’t last longer than 3 months whereas they saw a greater reduction with a longer period of effect contributing to the notion that the placebo effect wasn’t the main ingredient in this study.
Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients (Deng et al. 2007).
This study applied manual acupuncture on a standard set of points for 20 min twice a week for 4 weeks.
True acupuncture | GV14 | GB20 | BL13 | PC7 | HT6 | KI7 | ST36 | SP6 | Ear shenmen and sympathetic |
The control group was submitted to “Sham Acupuncture ” (SA) which consisted of nonpenetrating needles applied a few centimeters from TA points.
Again, the number of participants was restrained (n = 72) and this paper only analysed HF frequency as outcome.
Results showed that although no significant differences between groups were found, TA was associated with 0.8 fewer HFs/24 h than SA at week 6.
This paper raises the hypothesis that the acupuncture effect may have been be amplified had the treatment period been longer.
Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial (Hervik and Mjåland 2009).
The authors opted for manual acupuncture on a standard set of points for 20 min, twice a week for 5 weeks then once a week for 5 more weeks.
True acupuncture | CV4 | LR3 | GB20 | LU7 | KI3 | SP6 | PC7 | LR8 |
Control group was submitted to SA with superficial needling in non-acupuncture points.
Outcomes included number of HF/24 h and the Kupperman index a well-validated health score, follow-up was conducted up to 12 weeks.
Results implied a significant decrease in daytime and nighttime HFs in favor of TA (50% daytime and 60% at night) over SA (25% daytime and no reduction at night) the same was seen in the Kupperman Index with the TA group presenting a 44% reduction after treatment and the SA group remaining unchanged. Also the follow-up showed that for the SA group the minimal effects where gradually reversed while the TA group maintained response.
Despite its small sample size (n = 59), this study provides a nice insight into the potential role of acupuncture for HF control in women with breast cancer , the authors suggest that a individualized prescription of points according to TCM diagnostics could provide a greater effect.
Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant tamoxifen: a randomized controlled trial (Liljegren et al. 2012).
This paper investigated manual acupuncture on a standard set of points for 20 min twice a week for 5 weeks.
Bilaterally | SP6 | KI7 | ||
Unilaterally | LI4 | HT6 | LR3 | ST36 |
Control group with SA placing nonpenetrating needles on same meridian 1 cm from TA points.
Endpoints included HF frequency scale and circulating levels of estradiol, progesterone, testosterone, prolactin, follicle stimulating hormone (FSH), luteinising hormone (LH) and Sex hormone binding globulin (SHBG) measured before treatment and at 18 wk.
Both groups reported similar reductions in the HF scale but with significant between-group differences in favor of TA only for nighttime HFs. Also, the hormone levels remained unchanged.
Again, despite being the second largest study included in this review, the sample size remains modest (n = 84) and the question whether a more prolonged treatment regimen could provide better results is raised by the authors.
Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer : a randomized controlled trial (Walker et al. 2010).
The authors opted to use a tailored approach comprised of manual acupuncture on some core set of points plus points selected according to Traditional Chinese Medicine (TCM) theory, 30 min sessions twice a week for 4 weeks and then 8 weekly sessions.
Core points | BL23 | KI3 | SP6 | ||||||
Tailored points | GV14 | GV20 | GB20 | LU9 | LR3 | ST36 | CV6 | PC7 | HT7 |
Control group was medicated with Venlafaxine at 37.5 mg taken orally at bedtime for 1 wk followed by 75 mg at bedtime for 11 wk and follow-up was undertaken for 1 year.
Results showed that TA was as effective as venlafaxine and by 2 weeks after treatment, the venlafaxine group experienced significant increases in HFs, whereas HFs in the TA group remained low. The venlafaxine group experienced 18 occurrences of adverse effects (nausea, dry mouth, dizziness, and anxiety), whereas no adverse effects were reported in the TA group.
Albeit small in sample size (n = 50) this paper raises the opportunity to further encourage the use of this complementary treatment in face of the most common adopted pharmacological regimen.
Acupuncture relieves menopausal discomfort in breast cancer patients: A prospective, double blinded, randomized study (Bokmand and Flyger 2013).
This paper still remains with a modest sample size (n = 94) but in comparison to the previous studies attains an important improvement for the statistical analysis and investigates manual acupuncture on a standard set of points, with 15–20 min weekly sessions for 5 weeks only.
TA bilaterally | HT6 | KI3 | SP6 | LR3 |
The control group received SA on bilateral nonacupuncture points with superficial insertion. Also there was a third arm comprised of no acupuncture (Fig. 4).
The primary outcome was deemed “HF distress” on a visual analog scale (VAS) marked as a 0–10 logbook, also, plasma estradiol was measured right before and 30 min after the first treatment as well as at week 5. Follow-up was conducted up to 12 weeks (Fig. 5).
TA group showed better results for HF distress compared to SA or no acupuncture groups is this study. The TA group started to show improvements right after the second acupuncture session, which remained significant until the 12 wk follow-up. The estradiol plasma levels remained unchanged thus eliminating safety issues regarding the possibility of greater occurrence of breast cancer relapse related to acupuncture .
Conclusions
In light of the current published data and above mentioned strategies of treatment, to this author, seems like the use of a core set of points with Kidney and Qi enhancing properties allied with Heart and Liver harmonization points should be combined with a tailored selection of acupoints according to the patient’s most disturbing symptoms (i.e. night sweating, anxiety, mood and sleep disturbances, and so on) in order to provide the best possible acupuncture effect when controlling HFs.
5 Probable Mechanisms of Action—Hot Flashes
A hot flash frequently occurs in menopause and can be exacerbated by premature ovarian failure or estrogen deprivation resulting from cancer therapies.
The flashes in women are probably initiated by a sudden downward shift in the set point for the core body temperature in the thermoregulatory center, which seems to be affected by sex steroids and beta-endorphins.
Vasomotor symptoms have been shown to correlate with the decrease in estrogen production during the menopausal transition and with testosterone decreases after castration therapy in men with prostate cancer .
Also, Serum levels of serotonin are lower in postmenopausal women that associated with the reduced beta-endorphin concentrations could increase the release of noradrenaline causing sudden drops in the temperature set point in the hypothalamus eliciting inappropriate heat loss.
Acupuncture possibly modulates serotonin and noradrenalin activity in the central nervous system influencing the thermoregulatory center.
Calcitonin gene-related peptide (CGRP) is a potent vasodilator, and may be a proxy for beta-endorphin activity. Wyon et al. (2000) showed that plasma concentration of CGRP and neuropeptide Y (NPY) increases during a hot flush, and the urine excretion of CGRP seems to be reduced parallel to the reduction of hot flushes after acupuncture treatment.
In conclusion, acupuncture affects the beta-endorphin levels and also affects serotonin and noradrenalin activity in the central nervous system, besides that, a possible direct effect on regulating the release of CGRP could mediate the symptoms control seen in recent trials.
Aromatase Inhibitor Arthralgia
Breast cancer tissue has been shown to produce higher levels of estrogen, which then induces growth of breast cancer cells both in pre and post-menopausal women. Since aromatase plays a major role by catalyzing the final and rate-limiting step in estrogen biosynthesis, aromatase inhibitors (AIs) are used as first-line adjuvant therapy in post-menopausal women with hormone receptor-positive breast cancer .
When compared with Tamoxifen, which is a selective estrogen receptor modulator and unfortunately increases the risk of endometrial cancer and thromboembolism, AIs present with a less severe myriad of adverse events like hot flashes , vaginal dryness and headaches. However, 28–47% of patients receiving AIs experience musculoskeletal disorders and 5–25% of them discontinue therapy due to adverse effects.
To this date the exact etiology of these musculoskeletal symptoms is not well understood and this probably is what prevents an excellent management to be developed. Acupuncture has been shown to effectively increase the rate of musculoskeletal pain control (Vickers et al. 2012) and several trials have tested this treatment modality in breast cancer patients experiencing AIs related arthralgia.
The first systematic review of such trials (Chien et al. 2015) identified 5 high quality studies, 3 of them present favorable effects while the other 2 do not, meta-analysis of the results shows no statistically significant effects when compared with sham acupuncture .
A few points are worth mentioning when analyzing this review, the studies included looked for a possible downregulating effect of acupuncture on the inflammatory status of the participants by measuring pro-inflammatory cytokines like IL and TNF-alpha in blood samples, the exact molecules analyzed as well as the measurement methods were not consistent, also, as noted before, the role of inflammation in this particular entity has not been fully clarified. Moreover, the treatments chosen were also not consistent with point selection varying greatly between studies. Finally, most of the included trials applied questionnaires of self-reported outcomes for end-point measurements. While the used instruments are valid and consistent they would better reflect an accurate measurement if more patients and treatment centers were included since these are inherent subjective.
Characteristics of Studies Included
Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer : pilot study (Oh et al. 2013).
This study was a small pilot study with 32 subjects divided in two groups, one where the subjects received real EA and another where they received SA
EA:
Day 1 | LI4 | LI11 | GB34 | ST40 | LR3 | GV20 | Shishencong | Baxie |
Day 2 | GB21 | TE5 | ST36 | SP6 | LR3 | GV20 | Shishencong | Baxie |
SA was performed with non-penetrating needles (Streitberger placebo needle) at the actual acupoints and the EA device was set to produce the same audiovisual stimuli as in the EA group but with no actual electrical current.
Patients received sessions 2 days a week for 6 consecutive weeks.
Outcomes were measured with 3 scales, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Brief Pain Inventory Short Form (BPI-SF) and Functional Assessment of Cancer Therapy-General (FACT-G). Also there was a handgrip strength test and serum dosage of C reactive protein and erythrocyte sedimentation rate.
Follow-up was conducted until 12 weeks.
Investigators were unable to identify any significant changes in the markers selected for this study although they do point a “trend” of better outcomes at week 12 for stiffness, physical function and total WOMAC and inflammatory markers at week 6.
A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors (Bao et al. 2013).
This study utilized yet another set of acupoints :
CV4 | CV6 | CV12 | LI4 | PC6 | GB34 | ST36 | KI3 | BL65 |
SA was performed with non-penetrating needles placed away from real acuponits.
This protocol was undertaken once a week for 8 weeks and follow-up was performed for 12 weeks.
Outcome measures were differences in change in Health Assessment Questionnaire Disability Index (HAQ-DI) and pain VAS scores from baseline, also there was an attempt to find valid biomarkers with the measurement of plasmatic concentrations of estrogen, cytokine profile and beta-endorphin.
Again, the number of participants was low (n = 51) with 4 dropouts, remaining 47 for the analysis. Both groups presented improved function but there was no statistical difference between groups.
Estradiol remained indetectable, result consistent with other protocol that investigated acupuncture for hot flashes (Bokmand and Flyger 2013). Interestingly the cytokine profile showed a significant reduction of IL-17 in both groups (IL-17 is a pro-inflammatory cytokine that has been linked to severity of rheumatoid arthritis and psoriasis) raising the hypothesis of clinical improvement through IL-17 modulation.
Pilot study of acupuncture for the treatment of joint symptoms related to adjuvant aromatase inhibitor therapy in postmenopausal breast cancer patients (Crew et al. 2007) and Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer (Crew et al. 2010).
This protocol opted for a combination of core body acupuncture points combined with core auricular acupuncture points plus a tailored set depending on the most symptomatic joint:
Body | TA5 | GB41 | GB34 | LI4 | ST41 | KI3 |
Auricular | Shen men | Kidney | Liver | Upper lung | Sympathetic | |
Shoulder | LI15 | TA14 | SI10 | |||
Wrist | TA4 | LI5 | ||||
Fingers | TA5 | SI3 | Baxie | LI3 | ||
Lumbar | GV3 | GV8 | BL23 | |||
Hip | GB30 | GB39 | ||||
Knee | SP9 | SP10 | ST34 |
SA consisted of superficial needling in non-acupoint sites
Sessions lasted for 30 min twice weekly over 6 weeks.
Outcome measures included Brief Pain Inventory Short Form (BPI-SF), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Modified Score for the Assessment of Chronic Rheumatoid Affections of the Hands (M-SACRAH) and the Functional Assessment of Cancer Therapy-General (FACT-G) at baseline, 3 and 6 weeks.
This study also had a small sample size (n = 51) with 38 subjects evaluated and results showed improvement in joint pain, stiffness, functional ability and physical well-being in the True Acupuncture group and no significant benefits on the SA group, this poor response to the placebo intervention may have been caused by insufficient blinding of subjects to their treatment assignment once 43% of patients in the SA group correctly guessed that they were on the control group.
A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use (Mao et al. 2014).
On this protocol, the investigators decided to use a tailored set of points depending on the most painful joints and at least four distant points were used to address constitutional symptoms such as depression/anxiety and fatigue. Also, the EA was according to the symptoms with two pairs of electrodes at the needles adjacent to the painful joint with 2 Hz stimulation. Sessions happened twice weekly for 2 weeks, then weekly for 6 more weeks (Table 2).
There were two other control groups, one was a wait list control group (WLC) and a SA group with the sham procedure performed with non-penetrating needles (Streitberger device) at non-acupoints and the EA device would be on a different channel than the ones connected to the needles.
Measures included the Brief Pain Inventory (Mendoza et al. 1999) with the change in pain severity score at week 8 of intervention compared to the baseline between EA and WLC as primary outcome, secondary outcomes included Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Quick Disability of Arm, Shoulder, Hand scale (DASH) and the Physical Performance Test (PPT). Follow-up was completed at 12 weeks.
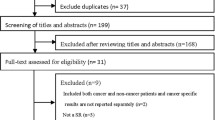
This study attempted a larger sample size with 159 patients screened for eligibility and 67 actually evaluated.
Results showed that the EA group had a significant greater decrease in the BPI severity score than the WLC at week 8. The EA group also had a statistically significant greater reduction in pain related interference score compared to the WLC group. Compared to baseline, the EA group experienced a 43.1% reduction in pain severity and a 52.6% reduction in pain-related interference at the end of the intervention period, results that remained significant at week 12.
Despite the impressive results, this study failed to find significant differences between EA and SA groups which could be explained by the somewhat small sample size, underpowered to difference between those groups. Also the authors suggest that maybe the follow-up period was to short to adequately find long-term potential separation of effects and complement raising the issue that maybe the non-penetrating needles are not as inert as a placebo procedure should.
6 Probable Mechanisms of Action—Aromatase-Inhibitor Arthralgia
Aromatase-inhibitor Arthralgia pathophysiology is unknown, estrogen deprivation has been temporally associated with this condition (Mao et al. 2011). Possibly, estrogen deprivation would decrease the generation of endogenous opioids , thereby leading to a lowered pain threshold. Mao J. J. then conducted an RCT (Mao et al. 2014) testing the hypothesis that Electroacupuncture (EA) would be able to restore the normal pain threshold since EA animal research demonstrated its clear physiological effect on the endogenous opioid system. This study revealed a significant effect when compared EA x usual care but failed to find differences between EA and Sham as reported earlier in this chapter.
Another possible mechanism would be the acupuncture effect on modulating the pro-inflammatory cytokines such as IL and TNF-alpha and, as previously mentioned, this was tested by a few investigators with Bao et al. (2013) being able to identify a reduction of IL-17 and a trend toward greater reduction in TNF-alpha (p = 0.095). This is very encouraging and future trials should focus on such analysis to reinforce the current evidence.
Cancer Related Fatigue
Fatigue is a subjective sensation of tiredness or even exhaustion that encompasses physical, psychological, emotional and cognitive activities and is not proportional to recent activities neither can be mitigated by adequate rest.
Cancer Related Fatigue is the most prevalent symptom of cancer patients being reported in up to 40% of individuals at diagnosis, 90% of those treated with radiation, and 80% of those under chemotherapy treatment (Hofman et al. 2007). It may start during treatment and increase in a cumulative manner, it may diminish when treatment is halted but some patients refer that it may last for years after cancer treatment is done.
This condition is often underreported, sometimes because patients feel that it is a standard condition of being sick, other times because survivors fear that it can indicate that the disease is relapsing and refrain from mentioning it so that the treatment and screening procedures won’t be re-started and also many doctors don’t actually investigate its presence since there is not much that can be offered for its treatment.
Nevertheless some treatable comorbidities may contribute to Cancer Related Fatigue (CRF) intensity like anemia, depression, anxiety, decreased ability to ingest food (nausea, vomiting, xerostomia), dyspnea and pain and must be addressed for optimal clinical management.
Treatment possibilities are antidepressants, mild psycho-stimulants, corticosteroids and erythropoietin. Non-pharmacological options includes diverse mind-body therapies and exercise. Although it may sound illogical to spend a fatigued one’s energy with exercise, a good body of evidence shows that it actually increases the well-being of patients suffering from cancer related fatigue (Kuchinski et al. 2009).
Acupuncture treatment for this condition has been tested since many patients turn to complementary medicine for symptoms that mainstream medicine can’t provide much relief.
A few RCTs have been conducted but once again the results have been mixed, as were the treatment protocols.
Acupuncture for cancer -related fatigue in patients with breast cancer : A pragmatic randomized controlled trial (Molassiotis et al. 2012) presents the largest RCT focused on investigating the benefits of acupuncture in CRF to date. It included 302 individuals with breast cancer randomly assigned to usual care (75) and to acupuncture plus usual care (227) (assignment of 1:3 respectively). This unusual disbalance between group sizes was justified due to a second phase in the study A randomized, controlled trial of acupuncture self-needling as maintenance therapy for cancer -related fatigue after therapist-delivered acupuncture (Molassiotis et al. 2013) where maintenance was done through self needling and acupressure. Statistical analyses deemed this a feasible design capable of detecting a 2-point change in scores. The primary outcome measure was the difference in general fatigue, as self-reported by patients with the baseline Multidimensional Fatigue Inventory (MFI) at 6 weeks (treatment completion). The MFI is a brief 20-item well-validated scale measuring general fatigue and the dimensions of physical and mental fatigue, activity, and motivation.
The acupuncture procedure per se consisted of weekly sessions of 20 min with manual acupuncture on standard points (LI 4, SP 6, ST 36) plus tailored points according to the acupuncturist’s discretion, no manipulation was allowed once the needles were placed. This was a multi-center study and involved 12 different practitioners. The results were significant and showed an impressive magnitude of effect (P < 0.001 and −3.11 from baseline score).
The main concern regarding this study was the lack of a placebo group plus the fact that the patients were not blinded to the group allocation. Since the main outcome was patient reported, this lack of concealment generates a high risk of bias jeopardizing the study findings.
There have been two other RCTs that were conducted recently and exhibited relatively high methodological quality.
Acupuncture for the treatment of post-chemotherapy chronic fatigue: A randomized, blinded, sham-controlled trial (Deng et al. 2013) compared manual acupuncture in standard points (CV 6, CV 4, KI 3, SP 6, ST 36, LI 11, HT 6 and auricular point “anti-depression”) with weekly sessions of 20 min for 6 weeks against Sham acupuncture with placebo needles placed a few millimeters away from true acupuncture points and meridians. The blinding was adequate and the main outcome was measured by the Brief Fatigue Inventory (BFI) (Mendoza et al. 1999). 74 patients were evaluated for the primary end-point (34 in the acupuncture group and 40 in the Sham acupuncture group), follow-up was attempted at 6 months after intervention but there was a huge loss of patients in this phase. Although there was a slight improvement in the questionnaires applied, this was not statistically significant and neither was the difference between groups. The conclusion of this study was that the treatment provided did not alleviate Post-chemotherapy Chronic Fatigue, the authors remark that the study was limited by the number of patients lost to follow-up and also that they cannot exclude the possibility that a more intensive treatment regimen may be more effective.
The effect of acupuncture on post-cancer fatigue and well-being for women recovering from breast cancer : a pilot randomised controlled trial (Smith et al. 2013) also attempted a randomized sham-controlled trial using sham acupuncture needles but this was a much smaller study since it was deemed a pilot study with 30 patients, 10 in the acupuncture group, 10 in the sham acupuncture group and 10 on wait list group. The intervention consisted of needling KI 3, KI 27, SP 6, ST 36, CV 4 and CV 6 plus tailored points at the acupuncturist’s discretion (maximum of 3 extra points), 20 min sessions with manual stimulation twice during this time, twice weekly session during the first 3 weeks and 3 more weeks with one weekly session (total of 9 sessions in 6 weeks). 3 questionnaires were used to measure the outcomes, one specific to fatigue, the BFI previously mentioned, plus two for general well-being, the Wellbeing questionnaire (W-BQ12) (Bradley 1994) and Measure Yourself Concerns and Wellbeing questionnaire (MYCaW) (Paterson et al. 2007). This feasibility study conclusions were deemed positive but the questionnaires findings only showed significant differences between groups at week 2 for the BFI (with loss of this difference in weeks 4 and 6), and for MYCaW at week 6. Once again, the indication that a more intense acupuncture treatment (i.e. 2 or more times a week) would be of greater effect was implied.
7 Probable Mechanisms of Action—Fatigue
The pathological mechanism of Chronic Fatigue Syndrome is still uncertain, major findings reported in Tang et al. (2015) include cerebral blood flow reduced in some brain regions, ventricular cerebrospinal fluid lactate and corticosteroid alterations combined with enhanced feedback of the hypothalamic-pituitary-adrenal (HPA) axis, as well as brain -derived neurotrophic factor (BDNF), serotonin and brain cytokines system distress.
Although there are various findings, none of them can explain the mechanism and clinical symptoms in this entity as well as in Cancer Related Fatigue and so far no specific mechanism of acupuncture action in this scenario has been minimally suggested.
Xerostomia
Xerostomia or dry mouth is a subjective feeling often associated to insufficient production of saliva to keep the mouth moist. This condition may present a myriad of discomfort encompassing difficult chewing, swallowing, tasting and talking, oral cavity ulcers or cracks, tooth decay, halitosis as well as make it difficult to wear dentures.
Radiation therapy to the head and neck as well as certain types of Chemotherapy, may cause damage to the salivary gland impairing its production of normal saliva. Chemotherapy generates xerostomia by making saliva thicker, which is an often reversible condition months after the treatment stops. Local radiation may destroy salivary glands diminishing it’s saliva output, some patients experience a normalization within the first year after radiotherapy but some may present xerostomia as a permanent condition.
Some medications commonly used by cancer patients such as antidepressants, muscle relaxants, diuretics and opioids may contribute to the dry mouth feeling and plausible alternatives must be considered when treating a patient with a severe case of xerostomia.
Usual management includes saliva substitutes also known as artificial saliva and mouth rinses with hyetellose, hyprolose or carmellose, physical methods to induce saliva production like chewing non-sugary gums, candy or even ice pellets. Medications that increase saliva output as pilocarpine and cevimeline are also an option but these may present some limiting side-effects, mostly systemic anti-cholinergic effects like nausea, dizziness, weakness, bladder dysfunction, rhinitis, headache, flushing, chills, and diaphoresis.
Acupuncture has been used in the management of radiation-induced xerostomia and a few trials have produced encouraging results both in the treatment and prevention of this condition.
Xerostomia Prevention
Randomized controlled trial of acupuncture for prevention of radiation-induced xerostomia among patients with nasopharyngeal carcinoma (Meng et al. 2012) is a very wise trial testing the use of acupuncture for prevention of xerostomia on patients undergoing radiotherapy compared with usual oral-hygiene care. The patients undergoing the acupuncture intervention (n = 40) were needled 3 times per week during the 7 week radiation period with a six-months follow-up, the points chosen were
Body | CV24 | LU7 | KI6 | LI4 |
Auricular | Shenmen | Point zero | Salivary gland 2’ | Larynx |
Except for CV 24 located in the midline, all points were treated bilaterally with the session lasting for 20 min. Subjects in the control group (n = 46) were under standard oral care, with no special education regarding prevention of xerostomia (Fig. 6).
The outcome measures selected were two specific questionnaires regarding Xerostomia and Head and Neck symptoms as well as salivary flow both spontaneous and induced (Fig. 7).
By week 3 of treatment the difference between the study groups began to be significant both on the questionnaires and on the induced salivary flow measurement, this difference reach it’s peak by week 7 and remained significant until 6 months after the end of radiotherapy suggesting that acupuncture is a valid resource for radiotherapy induced xerostomia prevention (Fig. 8).
Treatment
Few papers examined the effectiveness of xerostomia treatment with acupuncture , of notice Functional magnetic resonance imaging (fMRI) changes and saliva production associated with acupuncture at LI-2 acupuncture point : a randomized controlled study (Deng et al. 2008), have shown that salivary flow can be increased by needling LI 2 in healthy subjects and a recent literature review (Zhuang et al. 2012) identified 3 other studies of high quality methodology that are worth mentioning:
Acupuncture treatment of patients with radiation-induced xerostomia (Blom et al. 1996) this protocol included 38 subjects with 20 in the experimental group treated with classical acupuncture plus 18 in the control group with superficial acupuncture as placebo and treated patients twice a week for 12 weeks. The points chosen were diverse varying from 5 to 8 local and distal points (ST 3, ST 6, ST 5, GV 20, ST 7, SI 17, LI 18, PC 6, HT 7, ST 36, LR 3, LI 11, LI 10, LI 4, SI 3, SP 8, SP 3, SP 6, KI 7, KI 3, KI 5); 2 to 4 auricular points (Shenmen, Kidney Mouth, Stomach, Gl. Parotis, Sympathetic, Subcortex).
The outcomes were patient reported alleviation of symptoms and improvement in quality of life. Although salivary flow rates increased within group, this study failed to find a statistically significant difference between groups.
Manual acupuncture improved quality of life in cancer patients with radiation-induced xerostomia (Cho et al. 2008) this protocol was designed for a shorter period of treatment needling patients twice a week for 3 weeks on 5–8 local and distal points (ST 6, ST 36, LI 4, SP 6) and compared them to a group submitted to sham needling with the Streitberger device. This study had an extremely reduced sample size (n = 12) but questionnaire addressing problems in communicating, eating, sleeping, and daily functions showed positive results for the acupuncture group encouraging further investigations.
Acupuncture for pain and dysfunction after neck dissection: results of a randomized controlled trial (Pfister et al. 2010) larger in size (n = 58), also opted for a shorter period of treatment consisted of once a week for 4 weeks with needling on standard distal points (LI 4, SP 6, GV 20) and auricular shenman, plus various customized points and compared this group with a group submitted to “usual care”. The main outcome was not the xerostomia but Xerostomia Inventory was the secondary outcome measurement chosen and it showed a significant improvement in the intervention group.
Nevertheless this particular review (Zhuang et al. 2012) considered that the potential bias and great variation between study protocols prevented them to “positively identify the therapeutic effect of acupuncture for radiation-induced xerostomia”. They consider that the xerostomia should be analysed as being a yin deficiency syndrome specially stomach and kidney yin according to TCM as well as the radiation pathogenic factor as toxic heat and in being so they suggest the following treatment regimen:
-
Local points: ST 4, ST 6, ST 7, CV 23, CV 24;
-
Distal points: LI 2, LI 4, LI 11, PC 6, LU 7, ST 36, KI 3, KI 5, KI 6, SP 6, LR 3;
-
Auricular points: Shenmen, Point zero, Salivary gland.
8 Probable Mechanisms of Action—Xerostomia
Possible mechanisms of action have been identified in this particular setting, (Deng et al. 2008) fMRI study showed central nervous system imaging changes (activation of the insula and adjacent operculi) during acupuncture at LI2 with consequent saliva production. Also it is suggested that autonomic changes induced by needle manipulation inducing specific de-qi sensations might be mediated through the central nervous system.
Also the release of neuropeptides that stimulate the salivary glands and increase blood flow like CGRP (afore mentioned) and vasoactive intestinal polypeptide has been shown by Dawidson et al. (1997, 1998) in the saliva of xerostomia patients submitted to acupuncture .
These findings indicate that a central nervous system activation inducing saliva production together with a local increment of vasodilator and salivation stimulator peptides would be a plausible mechanism of Xerostomia mitigation by acupuncture .
Chemotherapy Induced Peripheral Neuropathy
Chemotherapy induced peripheral neuropathy (CIPN) is a common side effect resulting from nerve damage after exposure to certain Chemotherapy agents such as platinum compounds, taxanes, vinca alkaloids and also to newer agents such as bortezomib and thalidomide.
The clinical presentation may consist of a diverse array of symptoms such as persistent loss of feeling perceived as numbness or less ability to sense pressure and temperature, pain that may be constant or intermittent with characteristics of shooting or stabbing pain, burning, tingling or electric-shock like. This may impair manual abilities and increase the odds of stumbling or tripping while walking. Severe cases may present difficult swallowing, constipation, urinary retention and blood pressure changes. Usually the symptoms start farthest away from the head and tend to move closer over time, in most cases the changes will begin in the feet then later on in the hands. Some patients have symptoms that last for a short period of time but the symptoms may also persist for a long time and some patients refer that it never actually goes away.
Trials for prevention of CIPN with Vitamin E, Calcium and magnesium, anti-depressants, anti-seizure drugs and glutathione have yield mixed results and more studies are needed to provide any conclusion, strategies like reduced chemotherapy doses, longer periods of infusion and fractioned doses may be tried in order to reduce the risk of CIPN.
Acupuncture has been tested in the treatment of CIPN in various trials with different point combinations in order to address the most bothersome symptoms.
A recent review (Brami et al. 2015) identified 4 recent high quality trials:
Chemotherapy-induced peripheral neuropathy in cancer patients: a four-arm randomized trial on the effectiveness of electroacupuncture (Rostock et al. 2013) compared EA versus hydroelectric bath, daily vitamin B, or daily placebo capsules in 60 patients over a 3 weeks, with additional follow-up at 12 weeks. Points chosen were:
LR3 | SP9 | GB41 | GB34 | LI4 | LI11 | SI3 | HT3 |
EA was applied with 50 Hz during 15 min consisting of a combination of rectangular currents and high amplitude waves. This study had a major fall back due to baseline symptoms being far less intense than expected and significant changes between groups were not found.
Acupuncture for chemotherapy-induced peripheral neuropathy (CIPN): A pilot study using neurography (Schroeder et al. 2012), compared acupuncture for 10 weeks plus best medical care (BMC) vs. BMC only in patients with various cancer types and chemotherapy regimens. Intervention patients received a standard 10-week treatment on:
ST34 | EX-LE 12 (at the tip of the toes) | EX-LE 8 (at the web of the toes) |
Needles were inserted bilaterally for 20 min. Nerve conduction studies were used to evaluate possible changes and a ±2 m/s change in sural nerve conduction velocity (NCV) from initial assessments was considered significant. Although small in sample size, five out of six patients treated with acupuncture showed a significant mean NCV improvement after 6 months.
A Pilot Study of Acupuncture in Treating Bortezomib-Induced Peripheral Neuropathy in Patients With Multiple Myeloma (Bao et al. 2014) with 27 multiple myeloma patients with moderate to severe bortezomib-induced peripheral neuropathy were submitted to 10 weeks of manual acupuncture beginning with twice a week for 2 weeks, followed by once a week for four weeks and then once every other week for 4 more weeks. The points selected were bilateral ear points (shen men, point zero, and 2 additional auricular acupuncture points where electrodermal signal was detected), bilateral body acupuncture points LI 4, TA 5, LI 11, ST 40, and Ba Feng, the subjects experienced significantly reduced neuropathic pain and improved functions measured by specific questionnaires but cytokines analyses showed no significant changes, nerve conduction velocity studies did provide changes but these were not correlated to the subjective changes perceived by the patients (Fig. 9).
Electroacupuncture for thalidomide/bortezomib-induced peripheral neuropathy in multiple myeloma: a feasibility study (Garcia et al. 2014) demonstrated that EA was safe and possibly effective in treating thalidomide/bortezomib-induced peripheral neuropathy in 19 multiple myeloma patients with significant improvements in questionnaire scores and objective timed function tests such as fall risk, walk, postural stability, button and coin tests. The acupuncture treatment consisted of needling LI 4, SI 3, Baxie 2, Baxie 3, LR 3, SP 6, GB 42, ST 36, Bafeng 2, Bafeng 3, GV 20, CV4, and CV6, electrical stimulation was applied bilaterally as follows: from LI 4 (negative) to SI 3 (positive) and from LR 3 (negative) to GB 42 (positive) at 2–100 Hz for 20 min over a 9-week period of 20 acupuncture sessions at 2–3 times weekly (Fig. 10).
To this point, some high quality trials have yielded positive results in patient reported outcomes and even on neuronal conductions studies, but the accumulated body of evidence is still far from ideal to reach any definitive conclusion.
9 Probable Mechanisms of Action—Chemotherapy Induced Peripheral Neuropathy (CIPN)
The exact pathophysiology of CIPN is unclear. It generally is regarded as a consequence of the disruption of axoplasmic microtubule mediated transport, distal axonal degeneration, mitochondrial damage and direct damage to the sensory nerve cell bodies of the dorsal root ganglia (DRG) as described by Podratz et al. (2012). The DRG neurons seem to lack a vascular barrier, being more exposed to the neurotoxic effects of chemotherapy.
A few experimental models have yielded possible mechanisms through which acupuncture could affect the pain threshold and overall sensibility in CIPN.
Kim et al. (2004) demonstrated that Electroacupuncture (EA) acts through mu and delta but not kappa opioid receptors in mechanical allodynia and Sun et al. (2005) reported that cold allodynia can be reduced in rats treated with EA through the mediation of spinal alfa2-adrenergic receptors. Lau et al. (2008) investigated the role of EA on COX2 in rat spinal cord after spinal nerve ligation showing its action of downregulating COX2 expression. Somers and Clemente (2009) applied EA at the ST 36, which reduced the mechanical allodynia in a neuropathic model and normalized the expression profile of hypothalamic proteins identified as being involved in inflammatory processes, metabolism and signal transduction. Ko et al. (2002) examined such mechanisms of acupuncture in yet another model in rats at the molecular level by cDNA microarray analysis and found an increased expression of 68 genes which in turn could be returned to normal after treatment with EA. Such genes were involved in signal translation, gene expression, and nociceptive pathways. The same study also found a 50% decrease in the expression of the sigma opioid receptor in the neuropathic pain model, which also returned to normal after acupuncture .
The above mentioned findings correlate to the poor clinical response of neuropathic pain to opioids seen in practice, and the analgesic action of acupuncture in neuropathic pain could be that of normalizing the opioid receptor expression while increasing the release of endogenous opioid peptides.
10 Concluding Remarks
Acupuncture use within the oncological patient setting is a very promising therapeutic approach for symptom control especially for cancer survivors that endure lasting sequelae from aggressive treatment and disease.
To this date, high quality acupuncture research has been limited to a few centers of excellence and even though it is difficult to find protocols that have been re-tested in order to increase the level of evidence accumulated so far.
It is important that future research use the published experiences in order to avoid primary mistakes when designing a new trial and take notice of the plausible mechanisms of action so that more specific outcome measurement can be undertaken.
Future perspectives indicate further study in acupuncture regulation of pro-inflammatory cytokines, vasodilator peptides and the correlation between the endogenous opioid system and the serotonin-noradrenalin equilibrium.
Abbreviations
- AIs:
-
Aromatase Inhibitors
- AIDS:
-
Acquired immunodeficiency syndrome
- ANC:
-
Absolute neutrophil count
- aPTT:
-
Activated partial thromboplastin time
- BDNF:
-
Brain -Derived Neurotrophic Factor
- BMC:
-
Best Medical Care
- CIE:
-
Chemotherapy induced emesis
- CIPN:
-
Chemotherapy induced peripheral neuropathy
- EA:
-
Electroacupuncture
- CRF:
-
Cancer Related Fatigue
- h:
-
Hours
- HFs:
-
Hot Flashes
- HPA:
-
Hypothalamic-Pituitary-Adrenal
- HRT:
-
Hormone replacement therapy
- i.e.:
-
in example
- IL:
-
Interleukins
- INR:
-
International Normalized Ratio
- MFI:
-
Multidimensional Fatigue Inventory
- Min:
-
Minutes
- PT:
-
Prothrombin
- SA:
-
Sham Acupuncture
- TA:
-
True Acupuncture
- TNF-alpha:
-
Tumor Necrosis Factor alpha
- wk:
-
Week
References
Bao T, Cai L, Giles JT, Gould J, Tarpinian K, Betts K, … Stearns V (2013) A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 138(1):167–174. https://doi.org/10.1007/s10549-013-2427-z
Bao T, Goloubeva O, Pelser C, Porter N, Primrose J, Hester L, … Badros AZ (2014) A pilot study of acupuncture in treating Bortezomib-induced peripheral neuropathy in patients with multiple myeloma. Integr Cancer Ther 13(5):396–404. https://doi.org/10.1177/1534735414534729
Blom M, Dawidson I, Fernberg JO, Johnson G, Angmar-Mânsson B (1996) Acupuncture treatment of patients with radiation-induced xerostomia. Eur J Cancer Part B Oral Oncology. https://doi.org/10.1016/0964-1955(95)00085-2
Bokmand S, Flyger H (2013) Acupuncture relieves menopausal discomfort in breast cancer patients: a prospective, double blinded, randomized study. Breast 22(3):320–323. https://doi.org/10.1016/j.breast.2012.07.015
Bradley C (1994) The well-being questionnaire. In: Bradley C (ed) Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Harwood Academic Publishers, Chur, pp 89–109
Brami C, Bao T, Deng G (2015) Natural products and complementary therapies for chemotherapy-induced peripheral neuropathy: a systematic review. Crit Rev Oncol/Hematology. https://doi.org/10.1016/j.critrevonc.2015.11.014
Cassileth BR, Van Zee KJ, Yeung KS, Coleton MI, Cohen S, Chan YH, Hudis CA (2013) Acupuncture in the treatment of upper-limb lymphedema: results of a pilot study. Cancer 119(13):2455–2461. https://doi.org/10.1002/cncr.28093
Cheng KJ (2009) Neuroanatomical basis of acupuncture treatment for some common illnesses. Acupunct Med 27(2):61–64. https://doi.org/10.1136/aim.2009.000455
Chien T-J, Liu C-Y, Chang Y-F, Fang C-J, Hsu C-H (2015) Acupuncture for treating aromatase inhibitor-related arthralgia in breast cancer: a systematic review and meta-analysis. J Altern Complement Med 21(5):251–260. https://doi.org/10.1089/acm.2014.0083
Cho JH, Chung WK, Kang W, Choi SM, Cho CK, Son CG (2008) Manual acupuncture improved quality of life in cancer patients with radiation-induced xerostomia. J Altern Complement Med (New York, NY) 14(5):523–526. https://doi.org/10.1089/acm.2007.0793
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, Tattersall MHN (1983) On the receiving end-patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol 19(2):203–208. https://doi.org/10.1016/0277-5379(83)90418-2
Crew KD, Capodice JL, Greenlee H, Apollo A, Jacobson JS, Raptis G, … Hershman DL (2007) Pilot study of acupuncture for the treatment of joint symptoms related to adjuvant aromatase inhibitor therapy in postmenopausal breast cancer patients. J Cancer Survivorship Res Pract 1(4):283–291. https://doi.org/10.1007/s11764-007-0034-x
Crew KD, Capodice JL, Greenlee H, Brafman L, Fuentes D, Awad D, Hershman DL (2010) Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol Off J Am Soc Clin Oncol 28(7):1154–1160. https://doi.org/10.1200/JCO.2009.23.4708
Dawidson I, Angmar-Mansson B, Blom M, Theodorsson E, Lundeberg T (1997) Sensory stimulation (acupuncture) increases the release of calcitonin gene-related peptide in the saliva of xerostomia sufferers. Neuropeptides. https://doi.org/10.1016/s0143-4179(98)90083-x
Dawidson I, Angmar-Mansson B, Blom M, Theodorsson E, Lundeberg T (1998) Sensory stimulation (acupuncture) increases the release of vasoactive intestinal polypeptide in the saliva of xerostomia sufferers. Neuropeptides. https://doi.org/10.1016/s0143-4179(98)90083-x
De Boer-Dennert M, de Wit R, Schmitz PI, Djontono J, v Beurden V, Stoter G, Verweij J (1997) Patient perceptions of the side-effects of chemotherapy: the influence of 5HT3 antagonists. Br J Cancer. https://doi.org/10.1038/bjc.1997.507
Deng G, Hou BL, Holodny AI, Cassileth BR (2008) Functional magnetic resonance imaging (fMRI) changes and saliva production associated with acupuncture at LI-2 acupuncture point: a randomized controlled study. BMC Complement Altern Med 8(37):1–7. https://doi.org/10.1186/1472-6882-8-37
Deng G, Chan Y, Sjoberg D, Vickers A, Yeung KS, Kris M, … Cassileth B (2013) Acupuncture for the treatment of post-chemotherapy chronic fatigue: a randomized, blinded, sham-controlled trial. Support Care Cancer 21(6):1735–1741. https://doi.org/10.1007/s00520-013-1720-z
Deng G, Vickers A, Yeung S, D’Andrea GM, Xiao H, Heerdt AS, … Cassileth B (2007) Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. J Clin Oncology Off J Am Soc Clin Oncol 25(35):5584–5590. https://doi.org/10.1200/jco.2007.12.0774
Fernández-Ortega P, Caloto MT, Chirveches E, Marquilles R, Francisco JS, Quesada A, … Llombart-Cussac A (2012) Chemotherapy-induced nausea and vomiting in clinical practice: impact on patients’ quality of life. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. https://doi.org/10.1007/s00520-012-1448-1
Frisk J, Spetz A-C, Hjertberg H, Petersson B, Hammar M (2009) Two modes of acupuncture as a treatment for hot flushes in men with prostate cancer–a prospective multicenter study with long-term follow-up. Eur Urol 55(1):156–163. https://doi.org/10.1016/j.eururo.2008.02.002
Garcia MK, Cohen L, Guo Y, Zhou Y, You B, Chiang J, … Wang M (2014) Electroacupuncture for thalidomide/bortezomib-induced peripheral neuropathy in multiple myeloma: a feasibility study. J Hematol Oncol 7:41. https://doi.org/10.1186/1756-8722-7-41
Garcia MK, Graham-Getty L, Haddad R, Li Y, McQuade J, Lee RT, … Cohen L (2015) Systematic review of acupuncture to control hot flashes in cancer patients. Cancer 121(22):3948–3958. https://doi.org/10.1002/cncr.29630
Hervik J, Mjåland O (2009) Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Res Treat 116(2):311–316. https://doi.org/10.1007/s10549-008-0210-3
Hofman M, Ryan JL, Colmar F-M, Pascal J-P, Morrow GR, Figueroa-Moseley CD, … Morrow GR (2007) Cancer-related fatigue: the scale of the problem. The Oncologist, 12 Suppl 1(suppl 1):4–10. https://doi.org/10.1634/theoncologist.12-s1-4
Kim JH, Min BIl, Na HS, Park DS (2004) Relieving effects of electroacupuncture on mechanical allodynia in neuropathic pain model of inferior caudal trunk injury in rat: mediation by spinal opioid receptors. Brain Res. https://doi.org/10.1016/j.brainres.2003.11.045
Ko J, Na DS, Lee YH, Shin SY, Kim JH, Hwang BG, … Park DS (2002) cDNA microarray analysis of the differential gene expression in the neuropathic pain and electroacupuncture treatment models. J Biochem Mol Biol
Kuchinski AM, Reading M, Lash AA (2009) Treatment-related fatigue and exercise in patients with cancer: a systematic review. Medsurg Nurs 18(3):174–180. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd = Retrieve&db = PubMed&dopt = Citation&list_uids = 19591364\nhttp://media.proquest.com/media/pq/classic/doc/1753658261/fmt/pi/rep/NONE?hl = &cit%3Aauth = Kuchinski%2C + Anne-Marie%3BReading%2C + Maria%3BLash%2C + Ayhan + Aytek
Lau WK, Chan WK, Zhang JL, Yung KKL, Zhang HQ (2008) Electroacupuncture inhibits cyclooxygenase-2 up-regulation in rat spinal cord after spinal nerve ligation. Neuroscience. https://doi.org/10.1016/j.neuroscience.2008.06.016
Liljegren A, Gunnarsson P, Landgren B-M, Robéus N, Johansson H, Rotstein S (2012) Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant tamoxifen: a randomized controlled trial. Breast Cancer Res Treat 135:791–798. https://doi.org/10.1007/s10549-010-1283-3
Mao JJ, Su HI, Feng R, Donelson ML, Aplenc R, Rebbeck TR, … DeMichele A (2011) Association of functional polymorphisms in CYP19A1 with aromatase inhibitor associated arthralgia in breast cancer survivors. Breast Cancer Res 13(1):R8. https://doi.org/10.1186/bcr2813
Mao JJ, Farrar JT, Bruner D, Zee J, Bowman M, Seluzicki C, … Xie SX (2014) Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: a randomized trial - appendix. Cancer 120(23):3744–3751. https://doi.org/10.1002/cncr.28917
Mao JJ, Xie SX, Farrar JT, Stricker CT, Bowman MA, Bruner D, Demichele A (2014) A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer 50(2):267–276. https://doi.org/10.1016/j.ejca.2013.09.022
Meng Z, Garcia MK, Hu C, Chiang J, Chambers M, Rosenthal DI, … Cohen L (2012) Randomized controlled trial of acupuncture for prevention of radiation-induced xerostomia among patients with nasopharyngeal carcinoma. Cancer 118(13):3337–3344. https://doi.org/10.1002/cncr.26550
Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL (1999) The rapid assessment of fatigue severity in cancer patients: use of the brief fatigue inventory. Cancer 85(5):1186–1196. https://doi.org/10.1002/(SICI)1097-0142(19990301)85:5%3c1186:AID-CNCR24%3e3.0.CO;2-N
Molassiotis A, Bardy J, Finnegan-John J, Mackereth P, Ryder DW, Filshie J, Richardson A (2012) Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. J Clin Oncol 30(36):4470–4476. https://doi.org/10.1200/JCO.2012.41.6222
Molassiotis A, Bardy J, Finnegan-John J, Mackereth P, Ryder WD, Filshie F, Richardson A (2013) A randomized, controlled trial of acupuncture self-needling as maintenance therapy for cancer-related fatigue after therapist-delivered acupuncture. Ann Oncol 24(6):1645–1652. https://doi.org/10.1093/annonc/mdt034
Nedstrand E, Wyon Y, Hammar M, Wijma K (2006) Psychological well-being improves in women with breast cancer after treatment with applied relaxation or electro-acupuncture for vasomotor symptom. J Psychosom Obstet Gynecol. https://doi.org/10.1080/01674820600724797
NIH Consensus Conference (1998) Acupuncture JAMA 280:1518–1524
Oh B, Kimble B, Costa DSJ, Davis E, McLean A, Orme K, Beith J (2013) Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: pilot study. Acupunct Medicine J Br Med Acupunct Soc 31(3):264–271. https://doi.org/10.1136/acupmed-2012-010309
Paterson C, Thomas K, Manasse A, Cooke H, Peace G (2007) Measure yourself concerns and wellbeing (MYCaW): an individualised questionnaire for evaluating outcome in cancer support care that includes complementary therapies. Complement Ther Med 15(1):38–45. https://doi.org/10.1016/j.ctim.2006.03.006
Pfister DG, Cassileth BR, Deng GE, Yeung KS, Lee JS, Garrity D, … Vickers AJ (2010) Acupuncture for pain and dysfunction after neck dissection: results of a randomized controlled trial. J Clin Oncology Off J Am Soc Clin Oncol 28(15):2565–2570. https://doi.org/10.1200/jco.2009.26.9860
Podratz JL, Knight AM, Ta LE, Staff NP, Gass JM, Genelin K, … Windebank AJ (2012) Cisplatin induced Mitochondrial DNA damage in dorsal root ganglion neurons. Neurobiol Dis 41(3):661–668. https://doi.org/10.1016/j.nbd.2010.11.017.cisplatin
Rostock M, Jaroslawski K, Guethlin C, Ludtke R, Schröder S, Bartsch HH (2013) Chemotherapy-induced peripheral neuropathy in cancer patients: a four-arm randomized trial on the effectiveness of electroacupuncture. Evid-Based Complement Altern Med eCAM 2013:349653. https://doi.org/10.1155/2013/349653
Sato A, Schmidt RF (1987) The modulation of visceral functions by somatic afferent activity. Jpn J Physiol. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3302431
Sato A (1997). Neural mechanisms of autonomic responses elicited by somatic sensory stimulation. Neurosci Behav Physiology. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9353786
Schroeder S, Meyer-Hamme G, Epplée S (2012) Acupuncture for chemotherapy-induced peripheral neuropathy (CIPN): a pilot study using neurography. Acupunct Med J Br Med Acupunct Soc. https://doi.org/10.1016/j.dza.2012.06.009
Shen J (2000) Electroacupuncture for control of myeloablative chemotherapy-induced emesis: a randomized controlled trial. JAMA J Am Med Assoc 284(21):2755–2761. https://doi.org/10.1001/jama.284.21.2755
Smith C, Carmady B, Thornton C, Perz J, Ussher JM (2013) The effect of acupuncture on post-cancer fatigue and well-being for women recovering from breast cancer: a pilot randomised controlled trial. Acupunct Med J Br Med Acupunct Soc 31:9–15. https://doi.org/10.1136/acupmed-2012-010228
Somers D, Clemente F (2009) Contralateral high or a combination of high-and low-frequency transcutaneous electrical nerve stimulation reduces mechanical allodynia and alters dorsal horn. J Pain. Retrieved from http://www.sciencedirect.com/science/article/pii/S1526590008007372
Sun KK, Min BIl, Ji HK, Byung GH, Gi YY, Dong SP, Heung SN (2005) Individual differences in the sensitivity of cold allodynia to phentolamine in neuropathic rats. Eur J Pharmacology. https://doi.org/10.1016/j.ejphar.2005.08.030
Tang L-W, Zheng H, Chen L, Zhou S-Y, Huang W-J, Li Y, Wu X (2015) Gray matter volumes in patients with chronic fatigue syndrome. Evid Based Complement Altern Med eCAM 2015:380615. https://doi.org/10.1155/2015/380615
Tseng HS, Chan SE, Kuo SJ, Chen DR (2011) Acupuncture-related rapid dermal spread of breast cancer: a rare case. J Breast Cancer 14(4):340–344. https://doi.org/10.4048/jbc.2011.14.4.340
Vickers A, Cronin A, Maschino A (2012) Acupuncture for chronic pain: individual patient data meta-analysis. DtschE Z Für…. Retrieved from http://www.sciencedirect.com/science/article/pii/S0415641212006364
Walker EM, Rodriguez AI, Kohn B, Ball RM, Pegg J, Pocock JR, … Levine RA (2010) Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: a randomized controlled trial. J Clin Oncology Off J Am Soc Clin Oncol 28(4):634–640. https://doi.org/10.1200/jco.2009.23.5150
Wang JJ, Liu XD, Qin M, Chen LW, Qiu JY, Duan L, … Huang YX (2007) Electro-acupuncture of Tsusanli and Shangchuhsu regulates gastric activity possibly through mediation of the vagus-solitary complex. Hepato Gastroenterol 54(78):1862–1867
Wyon YA, Spetz AC, Theodorsson GE, Hammar ML (2000) Concentrations of calcitonin gene-related peptide and neuropeptide Y in plasma increase during flushes in postmenopausal women. Menopause 7(1):25–30. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10646700
Zhuang L, Yang Z, Zeng X, Zhua X, Chen Z, Liu L, Meng Z (2012) The Preventive and therapeutic effect of acupuncture for radiation-induced xerostomia in patients with head and neck cancer: a systematic review. Integr Cancer Ther. https://doi.org/10.1177/1534735412451321
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
D’Alessandro, E. (2019). Acupuncture in Oncology. In: Xia, Y. (eds) Translational Acupuncture Research. Springer, Cham. https://doi.org/10.1007/978-3-030-16089-0_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-16089-0_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16087-6
Online ISBN: 978-3-030-16089-0
eBook Packages: MedicineMedicine (R0)