Abstract
Dyslipidemia is considered to be one of the main heart risk factors, affecting the endothelial vascular function, which can be non-invasively investigated by ultrasound flow-mediated dilation (US-FMD). However, US-FMD comes at a high-cost and is operator-dependent. In this paper, the effect of dyslipidemia on the photoplethysmogram (PPG) signal recorded from collateral index fingers is investigated following a previous study where it was shown that results similar to that of US-FMD can be replicated by the PPG. Two groups, consisting of 30 healthy subjects free from any risk factors and 30 subjects who have only dyslipidemia as risk factor were respectively considered. The percent change in the AC (peak-to-peak) values versus time of the PPG after flow release following 4 min of brachial artery blockage (reactive hyperemia) was obtained (PPG-FMD). Results indicate that a very simple morphological feature allows for a significant (p < 0. 00001) discrimination between the control and pathologic groups.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
47.1 Introduction
Atherosclerosis is one of the main major causes of cardiovascular disease (CVD). Several risk factors such as smoking, high blood pressure, diabetes and high level of the cholesterol in the blood (dyslipidemia) may lead to developing atherosclerosis. An index which is capable to assess atherosclerosis using vascular endothelial dysfunction would therefore be beneficial to early diagnosis.
47.1.1 Vascular Endothelial Dysfunction
Atherosclerosis causes a dysfunction in the endothelium cells action; therefore evaluation of the endothelial function plays an important role in its early detection. Anatomically, the vascular wall is composed of three layers: the Intima, which is the nearest to the lumen and affected by blood flow. The second layer (Media) includes smooth muscle cells and the third layer is Adventitia. Endothelial cells are located in the Intima, the interior surface of the vascular wall. Because of their strategic location (contact with blood), endothelial cells play a critical role in various vascular functions such as controlling the thrombosis by their anticoagulant and antithrombotic surface, interactions of leukocyte and platelet with vessel wall and regulation of vascular tone and growth [1].
The endothelium maintains vascular homeostasis by establishing a balance between endothelium derived relaxing (such as Nitric Oxide – NO) and constricting factors. Any change in this balance makes the vasculature susceptible to vasoconstriction as well as leukocyte adherence, platelet activation, mitogenesis, pro-oxidation, thrombosis, impaired coagulation, vascular inflammation, and atherosclerosis [2]. The measurement of flow mediated dilation (FMD) has been established as an effective method to evaluate endothelial dysfunction [3, 4]. This technique (described in the next section) evaluates the ability of the vascular bed to self-regulate its tone and control the blood flow in response to either a physical or pharmacologic stimuli.
47.1.2 Flow Mediated Dilation
In this technique, a sphygmomanometric cuff is used to occlude the blood flow in (usually) the brachial artery (BA) by cuff inflation to suprasystolic pressure causing ischemia in the lower arm. Consequently, the vessels below the occlusion dilate through a self-regulated function. After 4–5 min of occlusion, the pressure is suddenly released leading to reactive hyperemia which causes shear stress on the inner wall (Intima) of the blocked BA. Subsequently, the BA is dilated due to the release of vasodilators. The diameter of the BA is measured from high-resolution longitudinal ultrasound B-mode images. As various factors affect FMD (such as temperature, food, drugs and sympathetic stimuli), subjects have to fast for at least 8 h without using any vasoactive medications for at least four half-lives, caffeine, high fat foods, vitamin C and tobacco and finally should be studied in a temperature controlled room [5, 8].
Unfortunately the above method proves to be expensive due to the equipment involved, prone to errors requiring an experienced operator [9].
More recently, another non-invasive method based on photoplethysmography [9] (PPG) has been developed. PPG is a signal reflecting pressure waves generated by the function of peripheral vascular arteries due to heart contraction. Dynamic blood volume changes due to the pulses are detected by a photoelectric probe placed on the finger tip (finger PPG) or ear lobes, among other sites. During systole, blood volume is increased due to the heart ventricle’s contraction and as a result, light transmission through the peripheral vasculature is reduced and vice-versa during the diastole [11].
PPG pulse amplitude changes due to flow-mediated dilation in the index finger are recorded following a 4 min brachial artery occlusion (PPG-FMD). As PPG reflects blood volume changes in the micro vascular bed of tissue [10], this means that PPG is affected by the occlusion.
The investigated risk factors were obesity, diabetes, hypertension and hypercholesterolemia [12]. Considering the effects of those risk factors, it was found that PPG-AC curves followed closely the US-FMD responses (good correlation) except for subjects who had more than one risk factor. In the present study the focus is on one risk factor only: dyslipidemia [9], and how PPG-FMD data is influenced by this single risk factor is investigated in the next sections.
47.2 Methods
47.2.1 Data Acquisition
The source of the raw database is from Universiti Kebangsaan Malaysia [9] (UKM). As factors such as temperature, food, drug, caffeine and sympathetic stimuli affect vascular flow-mediated vasodilation, each subject had adhered to a strict diet protocol before experimentation.
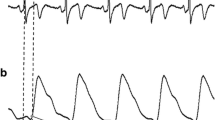
There are three steps for data acquisition: before occlusion, during occlusion and after cuff deflation as shown in Fig. 47.1.
Data acquisition: (a) before occlusion to establish the baseline (b) occlusion which lasts 4 min (c), after cuff deflation (reactive hyperemia) 4 min (Adapted from study [9])
In the first step (a), PPG were simultaneously recorded from index fingers of both right and left hand for 3 min without any blockage in order to establish the baseline.
In the second step (b), the left hand PPG was the reference, and a blood-pressure cuff was used to create flow blockage (stimulus) in the brachial artery (BA) of the right arm. The cuff was inflated to the suprasystolic pressure (50 mmHg above the subject’s systolic blood pressure) inducing total arterial occlusion.
In the third step (c), after 4 min occlusion the flow was established again by rapid cuff deflation, followed by reactive hyperemia in the BA and subsequent dilation.
PPG signals were recorded from both hands [5, 9] during the whole process and the final sampling rate was 50 Hz. In this study, two groups of healthy and pathologic subjects consisting of 30 subjects in each group were considered. Healthy groups are without any history of heart diseases as well as heart risk factors. The pathological group consists of subjects have only dyslipidemia as a risk factor.
47.2.2 Signal Processing
MATLAB (The Math Works Inc.) and SPSS (SPSS Inc.) software were used for signal processing. PPG signals contain both DC and AC components: the DC is related to respiration, sympathetic nervous system activity and thermoregulation while AC parameter is referred to the cardiac synchronous changes with each heart beat in skin micro-vascular blood volume [13].
In this study, the focus is on the AC component of the PPG signal. PPG AC refers to the difference between the amplitudes of the valley and the peak of the same heart cycle in the PPG signal. For the first step the DC of the signal was removed and the AC value was extracted. As the PPG-AC curves were subject dependent, the next step was normalization.
It is assumed that the difference between the mean value (M) over 3 min of PPG AC of the left (L) and right (R) index fingers are equal before occlusion and after it. Therefore, the effect of hyperemia is removed from the baseline by Eq. (47.1) which computes the new baseline (M (R after )).
Equation (47.2) shows the normalized value for each subject based on its new baseline which we used as PPG %AC change.
After normalization based on the new baseline, features were extracted to compare two groups of healthy and pathologic subjects.
A common feature was needed to compare the plots with each other, to this end; a threshold was defined for each subject. It was referred to the percent of the peak value which is shown in Fig. 47.2. During processing threshold levels from 15% to 95% of the peak value by interval of 10% were tested.
Figure 47.2 shows a typical schematic of this behavior for both healthy and pathologic subjects, after normalization. It is clear that as a common behavior, the PPG %AC change rises to its peak value and then falls towards the baseline. For the healthy subjects, the graph shows a sharp slope in both directions whereas for the pathologic subjects the response is rather blunted.
47.2.3 Feature Definition
Two features were extracted from the PPG %AC. In a previous study [14] the threshold was placed at 35% of the graph’s peak, the time period between two cross points of the graph with threshold was measured as Time feature. The results of the t-test showed [14] that the mean of the two groups were significantly different (p-value is 4.4%). The present study was extended to extract other features as below:
-
Area under the curve (AUC) before the peak time but above the threshold line: depicted in Fig. 47.2 as A1. This feature reflects the increase in the micro vessels diameter.
-
AUC above the threshold after the peak but above the threshold line: depicted in Fig. 47.2 as A2. This feature reflects the decrease in the micro vessels diameter towards the baseline.
47.3 Results
Figure 47.3 shows a typical PPG %AC change for a subject in the healthy group whereas the origin of time indicates cuff deflation. The response increases and reaches the peak value during hyperemia at about 210 s, as a consequence of the stimulus on the vessel wall. Then the diameter goes back to its normal size. This phenomenon is similar to the very well known US-FMD response corresponding, but is obtained here through PPG %AC change. The two threshold values (15% and 85% of peak) are also shown as examples.
Figure 47.4 shows the same data for a subject who has dyslipidemia. As it can be seen, the curve reaches the peak but goes down with some delay compared to the healthy subject (Fig. 47.3). In other words the diameter of the vascular bed increases due to hyperemia but it does not return to its normal size as sharply as it occurred in healthy subjects. It was observed that in some subjects the trace did not even reach the baseline again.
For the first feature (A1: AUC starting from the cuff release point to the peak value), the mean value for pathologic subjects is generally higher than for healthy ones. This could be explained by the sharp changes of the PPG %AC change for the healthy subjects. It was found that by increasing the threshold to 85% of the peak value, a significant difference between the two groups could be seen (Fig. 47.5).
On the opposite, for the second feature (A2: AUC starting from the peak time up to the end), the value for healthy subjects is much more than pathologic subjects. A very significant difference (p < 10− 4) is obtained when the threshold is at 15% of the peak value. When the threshold is increased towards 85%, the difference becomes less (Fig. 47.6).
Figure 47.7 shows the ROC curve for both features A1 (with 85% threshold) and A2 (with 15% threshold).
The mean of the two groups were significantly different (T-test p-value of less than 0.3%) and the 95% confidence interval of the difference was from 1,058 to 4,723 for A1. Figure 47.5 shows the error plot for two groups for A1.
The results show that the mean of the two groups were significantly different (T-test p-value of less than 0.01%) and 95% confidence interval of the difference was from − 19,589 to − 10,610 for A2. Figure 47.6 shows us the error plot for two groups.
The result of the last two features shows that for the pathologic subjects the vessels diameter cannot come back to its normal size compared to healthy subjects. Table 47.1 lists out the characteristics of the test variables.
47.4 Conclusion
Following brachial arterial blockage, the percent AC change in the PPG signal undergoes through a very typical cycle. Dyslipidemic subjects show a significant difference in the shape of this signal which was investigated in this paper. A simple morphological feature and a low-cost setup have allowed a significant discrimination to take place.
The physiological reason for this observed phenomenon requires further study. Evidence suggests that in healthy subjects – with a normal vascular function control – the behavior of the vessel diameters after hyperemia differs from pathologic subjects where this function seems to be altered. A larger population and other risk factors should be studied to eventually reach a useful index assisting physicians in their diagnostic of the vascular health.
References
Celermajer, D.S.: Endothelial dysfunction: Does it matter? Is it reversible. J. Am. Coll. Cardiol. 30(2):325–33 (August 1997)
Verma, S., Anderson, T.J.: Fundamentals of endothelial function for the clinical cardiologist. J. Am. Heart Assoc. Circulat. 105:546–549 (2002)
Meyer, B., Mörtl, D., Strecker, K., Hülsmann, M., Kulemann, V., Neunteufl, T., Pacher, R., Berger, R.: Flow-mediated vasodilation predicts outcome in patients with chronic heart failure. J. Am. Coll. Cardiol. 46(6):1011–1018 (2005)
Anderson, E.A., Mark, A.L.: Flow-mediated and reflex changes in large peripheral artery tone in humans. J. Am. Heart Assoc. Circulat. 79:93–100 (1989)
Corretti, M.C., Anderson, T.J., Benjamin, E.J., Celermajer, D., Charbonneau, F., Creager, M.A., Deanfield, J., Drexler, H., Gerhard- Herman, M., Herrington, D.: Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery – a report of the international brachial artery reactivity task force. J. Am. Coll. Cardiol. 39: 257–265 (2002)
Su, W., Cheng, S., Hsu, T., Ho, W.: Abnormal flow-mediated vasodilation in normal-tension glaucoma using a noninvasive determination for peripheral. Invest. Ophthalmol. Visual Sci. 47(8):3390–3394 (August 2006)
Kao, Y.H., Mohler, E.R., Arger, P.H., Sehgal, C.M.: Brachial artery: measurement of flow-mediated dilation with cross sectional US-technical validation. J. Radiol. 228(3):895–900 (2003)
Leeson, P., Thorne, S., Donald, A., Mullen, M., Clarkson, P., Deanfield, J.: Non-invasive measurement of endothelial function: effect on brachial artery dilatation of graded endothelial. J. Heart 78:22–27 (1997)
Zahedi, E., Jaafar, R., Mohd Ali, M.A., Mohamed, A.L., Maskon, O.: Finger photoplethysmogram pulse amplitude changes induced by flow mediated dilation. Physiol. Measure. 29(5):625–637 (2008)
Allen, J.: Photoplethysmography and its application in clinical physiological measurement. J. Physiol. Measure. 28:1–39 (2007)
Crabtree, V.P., Smith, P.R.: Physiological models of the human vasculature and photoplethysmography. Electron. Syst. Con. Division Res. (2003)
Zaheditochai, M., Jaafar, R., Zahedi, E.: Non-invasive techniques for assessing the endothelial dysfunction: ultrasound versus photoplethysmography. Proceedings of International Conference of Biomedical Engineering 23:65–68 (2009)
Allen, J., Oates, C.P., Lees, T.A., Murray, A.: Photoplethysmography detection of lower limb peripheral arterial occlusive disease: a comparison of pulse timing, amplitude and shape characteristics. J. Physiol. Measure. 26:811–821 (2005)
Zaheditochai, M., Zahedi, E., Mohd Ali, M.A.: Effect of dyslipidemia on photoplethysmography flow mediated dilation. World Congress Engineering, pp. 1881–1884 (2009)
Acknowledgement
The authors would like to thank Universiti Kebangsaan Malaysia for supporting this work under the University Research Grant UKM-AP-TKP-07–2009.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media B.V.
About this chapter
Cite this chapter
Zaheditochai, M., Zahedi, E., Ali, M.A.M. (2010). Effect of Dyslipidemia on a Simple Morphological Feature Extracted from Photoplethysmography Flow Mediated Dilation. In: Ao, SI., Gelman, L. (eds) Electronic Engineering and Computing Technology. Lecture Notes in Electrical Engineering, vol 60. Springer, Dordrecht. https://doi.org/10.1007/978-90-481-8776-8_47
Download citation
DOI: https://doi.org/10.1007/978-90-481-8776-8_47
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-90-481-8775-1
Online ISBN: 978-90-481-8776-8
eBook Packages: EngineeringEngineering (R0)