Abstract
Policymakers are increasingly designing policies that encourage patient choice and therefore mobility across providers. Since prices are regulated (fixed) in most countries, providers need to compete on quality to attract patients. This chapter reviews the current theoretical and empirical literature on patient choice and quality competition in health markets. The theoretical literature identifies key factors affecting incentives to provide quality. These include: altruistic motives, cost structure, number of providers, demand responsiveness, GP gatekeeping, degree of specialization, profit constraints and soft budgets. We also review the theoretical literature on choice across different countries (e.g. within the EU) or regions within the same countries. The chapter reviews selected empirical studies that investigate whether demand responds to quality and waiting times, the role of patient’s mobility and the effect of competition on quality.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
JEL Classification
1 Introduction
Policymakers are increasingly designing policies that encourage patient choice and therefore mobility across providers (hospitals and in some case general practitioners (GPs)). For example, in the English National Health Service (NHS) greater information on measures of hospital quality such as mortality rates, readmission rates, and infection rates are now available on government sponsored websites and patients now have the right to choose any NHS hospital rather than being restricted to hospitals contracting with their local health authority.
When prices are regulated as they are in most countries, health care providers need to compete on quality to attract patients. Patient choice is a pre-requisite for pro-competition policies to improve quality. If patients can freely move among providers then hospitals may have an incentive to compete on quality. The degree to which demand responds to variations in quality plays therefore a critical role. To facilitate choice, policy makers increasingly publish comparative information on health care providers, including measures of the quality such as adjusted mortality and readmission rates. However, patients’ choices are also influenced by family doctors and specialists. Family doctors often act as gatekeepers, referring patients to hospitals and specialists who are responsible for diagnosis and treatment. Given the asymmetry of information between doctors and patients, it is not obvious that stimulating choice will have any effect on actual demand.
This chapter reviews the theoretical and empirical literature on patient choice and quality competition in health markets. The theoretical literature summarized in Sect. 2 focuses on key factors that drive incentives to provide quality and how they relate to choice and competition. These include: altruistic motives, cost structure, number of providers, demand responsiveness, GP gatekeeping, degree of specialization, profit constraints and soft budgets. We also review the limited theoretical literature on patients’ choice across providers in different countries (e.g. within the EU) or municipalities within the same countries. In Sect. 3 we review selected empirical studies that investigate whether demand responds to quality and waiting times (a negative form of quality), and whether competition affects quality. The latter can be seen as an indirect test of whether providers respond to changes in the degree of patient choice.
2 Theory
The effects of patient choice and competition on health care provider behavior are the subject of an extensive theoretical literature.Footnote 1 Here, we focus on the literature that studies this relationship in health care systems where prices are regulated and thus not determined in the market. We therefore do not discuss the literature on patient choice and competition under variable prices, where each provider can set prices constrained only by the demand function it faces or where prices are the result of a bargaining procedure between the purchaser of health services (a private or a public insurer) and the hospital (Barros and Martinez-Giralt 2012).
Most countries regulate prices for health care services. For example, in the English National Health Service under the Payment by Results (PbR) system hospitals are paid a price for each patient which is based on the patient’s diagnoses and treatments. The system is similar to the Diagnosis Related Groups system introduced for payments for Medicare patients in the US in the early eighties, variants of which have been adopted subsequently.
It is often claimed that under a fixed-price regime, more patient choice and thus competition lead to higher quality. The intuition is that with fixed prices hospitals can attract more patients only by raising their quality. With more patient choice among hospitals, demand will be more responsive to quality, thereby increasing the additional revenue from raising quality. Formal economic models show that this intuition is correct if (i) more patient choice does increase the responsiveness of demand to quality, (ii) providers are profit maximizer, (iii) the marginal cost of additional patients is constant, (iv) the profit margin (price minus marginal cost) is positive, and (v) providers meet whatever demand is generated by their choice of quality (Ma and Burgess 1993; Gaynor 2006; Gaynor and Vogt 2003).
Thus suppose that the hospital chooses quality \( q \) to maximize profit
where \( p \) is the fixed price, \( X(q;\theta ) \) is demand (which equals its output) and higher quality increases demand \( (X_{q} > 0) \), and \( C \) is cost and depends both on output and quality (\( C_{X} > 0 \), \( C_{q} \) \( > 0 \), \( C_{qq} > 0 \)). \( \theta \) is parameter which measures the degree of patient choice and therefore the responsiveness of demand with respect to quality: \( X_{q\theta } > 0 \). \( T \) is a lump-sum payment from the third party payer. We assume for simplicity that patients’ co-payments are set to zero. The choice of quality satisfies the first order condition
Quality is increased by patient choice if it increases the marginal profit from quality i.e. if
Patient choice makes demand more responsive to quality (\( X_{q\theta } > 0 \)), but it could increase or reduce the demand for a particular hospital (\( X_{\theta }\, \lessgtr \, 0 \)), depending on whether the hospital had higher quality than its competitors, the geographical distribution of patients, and the details of the patient choice policy. Thus a sufficient condition for patient choice policy to increase quality for all providers is that the profit margin (\( p - C_{X} \)) is positive, and that the marginal cost of treating an extra patient is not affected by quality, either directly (\( C_{Xq} \equiv C_{qX} = 0 \)) or indirectly (\( C_{XX} X_{q} = 0 \)).
The incentive to increase quality is stronger, the larger the profit margin. Increasing the regulated price will increase the marginal net profit from higher quality and so will increase quality: the quality supply function is increasing in the regulated price.
In most prospective payment schemes, such as the DRG-pricing schemes and the English PbR scheme, the regulated price is related to the average cost. This implies that the profit margin (price minus marginal cost) will be larger for procedures characterized by large fixed costs and low marginal costs. The profit margin will be positive for hospitals operating at volumes where marginal cost is constant or decreasing. The profit margin will also be greater if the prospective price computation includes investment/capital costs (whether this is the case varies across countries). In some countries, like Norway, the fixed price is a proportion (40–60 %) of the average cost. In this case it is not obvious that the profit margin is positive. If the profit margin is negative, then the financial incentive to increase quality will be negative: providers will wish to reduce quality but will be constrained by sanctions from quality regulators and the threat of malpractice suits from patients. Increases in competition in this case will not increase quality.
2.1 Health care Provider Objectives
The extent to which health care providers respond to competition and patient choice depends on who is taking decisions which affect quality, their preferences, and who is the “residual claimant” (i.e., who has control over any financial surplus). In the English NHS almost all providers offering care to NHS patients are public: they have no shareholders. However, they are subject to financial targets which require them to break even or earn a financial surplus to be reinvested in providing services. Thus they will take the financial consequence of decisions about quality into account.
In most health care providers the decision making process is complex. In hospitals some decisions affecting quality are made at hospital level: hospitals invest in better machinery, medical equipment, or better trained staff. Other decisions, particularly on treatment of patients, are made by individual doctors and nurses who, in many systems of the NHS type, are typically paid a fixed salary, as opposed to fee for service, or a share of profits. We may expect the financial incentive to respond to increased competition by raising quality will be diluted if those who take decisions affecting quality do not receive any financial benefit from higher quality.
In the health economics literature, it is recognized that doctors may not be entirely selfish (McGuire 2000): they care about their income and effort, but they are also motivated in part by an altruistic concern for patients’ health. Alternatively, the hospital’s objectives can be viewed as the result of bargaining between managers (who are more concerned with financial constraints and targets) and doctors who are more directly concerned with patient wellbeing. It is therefore common in the health economics literature to assume that providers act as if they were maximizing a weighted sum of profits and benefits for the patients.
Brekke et al. (2011) show that with semi-altruistic providers there is an a priori ambiguous relationship between increased patient choice and quality provision. A simplified version of their model illustrates the main point.
The total benefit to the patients who are treated by the provider is \( B\left( {X(q;\theta ),q} \right) \), with \( B_{X} > 0 \) and \( B_{q} > 0 \). Higher quality increases patient benefit in two ways: it increases the benefit for each patient treated and it increases the number of patients treated. Suppose that the provider chooses quality to maximize a weighted sum of profit and patient benefit
where \( \alpha > 0 \) is a parameter measuring the degree of provider altruism. Quality is chosen so that
The square bracketed term in (5) is total benefit from higher quality and is positive, so that an altruistic provider will choose a higher level of quality than a pure profit maximizer. Indeed the altruistic provider chooses quality such that \( \pi_{q} (q;\theta ) \) \( < \,0 \) which could result in the provider operating where the profit margin (\( p - C_{X} \)) is negative: it treats patients on whom it makes a financial loss.
The effect of increased patient choice on the marginal utility of quality is
In general the sign of \( u_{q\theta } \) is unclear and the effect of patient choice on a profit maximizing provider does not indicate its effect on an altruistic provider. If the marginal costs of output and quality are constant with respect to output and \( B_{qX} = 0 = B_{XX} \) then we can ignore the effect of patient choice on demand (\( X_{\theta } \)) and
In this case, increased patient choice has two potentially offsetting effects on the incentives for quality provision. On the one hand, a more quality-responsive demand increases each provider’s incentive to reduce quality if \( p{\kern 1pt} < C_{X} \) in order to induce financially unprofitable patients to choose other providers (first term in (7)). On the other hand, altruism means that the provider wants to increase \( q \) to attract more patients and increase patient benefit.
Brekke et al. (2011) show that, depending on the size of the two effects, more competition may increase or reduce quality. A similar type of reasoning applies when hospitals compete on waiting times as opposed to quality, where waiting times can be thought of a negative form of quality (Brekke et al. 2008). More competition can lead to higher waiting times when demand is more responsive. Providers have an incentive to increase waiting times to avoid unprofitable patients.
As an additional special case, suppose that the provider cares only about the average quality so that \( B_{X} = 0 \). Then, it is still the case that for sufficiently high altruism, providers are willing to choose a quality provision where they make a financial loss by treating an additional patient. In such case, for sufficiently high altruism, a more responsive demand unequivocally leads to lower quality. Providers choose \( q \) to deter rather than to attract patients.
2.2 Profit Constraints
Hospital care is mainly provided by non-profit and public providers. Thus, large parts of health care services are offered by providers that cannot distribute profits. In publicly-funded health care markets financial surpluses can generally not be distributed in cash to those who makes decisions about provider quality. In such markets it might be more reasonable to model health care providers as being subject to a constraint on profit distribution, where alternative ways of distributing profits (e.g., through perquisites) imply a utility loss relative to distribution in cash. This is the approach taken by Brekke et al. (2012a), who show that the presence of such distribution constraints could severely alter provider incentives with respect to quality. We can incorporate such an approach in the simple example above by assuming that the value of financial profits for the provider is discounted by a factor \( \delta \in \left( {0,1} \right) \).
When investigating the role of profit constraints, it is important to distinguish whether the direct cost of quality are monetary or non-monetary. We therefore now interpret the cost function \( C(X(q,\theta ),q) \) as the monetary cost of quality and \( \varphi (q) \) as the non-monetary cost of providing quality (quality effort disutility), with \( \varphi^{\prime} (q) > 0 \) and \( \varphi^{\prime\prime} (q) > 0 \).
The condition for optimal quality provision, (5), then becomes
It is useful to investigate some special cases. Suppose that there is no altruism and non-monetary costs are also absent (\( \alpha = \varphi (q) = 0 \)). Then the discounting of profits has no effect on quality. The constraint on profit distribution acts like a tax on profits. It reduces both the marginal benefit and the marginal cost of quality, so that the optimal level of quality remains unaffected.
Consider now the case where there is still no altruism but costs are also non-monetary. The provider chooses quality to equate the marginal profit with the marginal non-monetary cost of quality. In this case, profit distribution constraints reduce the marginal profit, and therefore the incentive to provide quality. They also reduce the effect on quality of an increase in the responsiveness of demand to quality (\( \theta \)).
With semi-altruistic providers, the optimally chosen quality level balances the marginal net profit and the marginal altruistic benefit with the marginal non-monetary cost of quality. A constraint on profit distribution now reduces the importance of the marginal profit from quality (\( (1 - \theta )\pi_{q} \)) in determining quality. If the marginal effort cost of quality \( \varphi^{\prime} (q) \) is smaller than the altruistic marginal benefit, then \( (1 - \theta )\pi_{q} \) is negative in (8) and an increase in \( \delta \) will reduce the overall marginal loss from higher quality and so increase quality. Conversely if the marginal effort cost of effort is greater than the altruistic marginal benefit, then greater profit constraints reduce quality.
2.3 Soft Budgets
An important feature of many health care systems, is that providers, especially publicly owned hospitals, face soft budgets with funders partially covering deficits or partially confiscating profits. Despite the importance of this topic, there are very few theoretical studies of how soft budgets influence the provision of health care.
Brekke et al. (2013a) analyze the incentives for hospitals to provide quality and expend cost-reducing effort when budgets are soft. They assume that demand is uncertain and that patients can choose which hospital to be treated at. In their model surpluses occur in the low demand state, whereas deficits occur in the high demand state. There are two reasons for this. First, providers cannot increase prices when demand is high (prices are regulated), and, second, they cannot turn down patients who demand treatment. Assuming providers maximize expected profits, the condition for optimal quality is then:
where \( \mu \) is the probability of the low-demand state (where \( X = X^{L} (q;\theta ) \)), \( \sigma \) is the share (or probability) of profit expropriation, and \( \beta \) is the share (or probability) of bailout. For a given level of cost-reducing effort, it is evident that profit confiscation reduces the providers’ quality incentives and bailout increases quality incentives. However, the effects of soft budgets on quality are ambiguous when providers can expend cost-containment effort (i.e., reduce \( C_{X} \)) to increase their profit margin.
The reason is that softer budgets reduce cost-containment effort, which in turn enhances the negative effect of profit confiscation on quality and counteracts the positive effect of bailouts on quality. Therefore, soft budgets can reduce quality if the effect on cost-containment effort is sufficiently pronounced. Brekke et al. (2013a) show that a higher degree of patient mobility (due to lower travel costs in their Hotelling framework), generally increases quality. A more responsive demand tends on one hand to reduce quality because the profit margin is negative in the high-demand state but on the other hand tends to increase quality because the profit margin is positive in the low-demand state. But the overall expected profit margin in equilibrium is positive and therefore quality increases with a more responsive demand.
2.4 Specialization
As well as competing on quality providers may specialize by attracting particular types of patient. By specializing, providers can reduce the competition they face in their specialist treatment. It is reasonable to assume that specialization is a longer term decision than quality investment. If so, decisions over quality and specialization should be modelled sequentially rather than simultaneously. This is the approach used by Brekke et al. (2006). In stage 1 providers choose the degree of specialization and in stage 2 the level of quality. Suppose that all providers in a market maximize profits (\( \alpha = 0 \)). In stage 2, the optimal quality level, for a given level of specialization \( s \), chosen by each provider is given by (see 5)
In a Hotelling spatial competition framework, greater specialization decreases demand responsiveness (\( X_{qs} < 0 \)) and therefore dampens incentives to provide quality (\( \partial q/\partial s < 0 \)). The marginal profit from \( s \) when it is chosen at stage 1, is
The optimal level of specialization is determined by the marginal cost saving from the effect of greater specialization on quality (second term) and the reduction in profit as market share falls (first term). The degree of specialization critically depends on the degree of convexity of costs with respect to quality. If convexity is high enough, the marginal cost saving due to the reduction in quality as specialization increases is less than the loss in profit as market share falls and so providers do not specialize. Conversely, if the degree of convexity is low, providers specialise to the maximum extent possible.
If there is an interior solution a higher price (\( p \)) will increase the marginal benefit of attracting patients and therefore intensify competition and specialization. A higher degree of patient mobility (\( \theta \)) will make demand more quality-responsive (i.e., increase the value of \( X_{q} \)) and therefore also intensify specialization. The increase in competition intensity following an increase in patient mobility is dampened, but not overturned, by incentives to specialize. Thus, an increase in patient mobility will lead to more specialization and higher quality in equilibrium.
Gravelle (1999) and Nuscheler (2003) investigate quality and provider location decisions (which we can interpret loosely as a type of specialization) when there are no barriers to entry. They find that patient mobility affects entry decisions through incentives for quality provision. Increased patient mobility makes demand more quality-responsive and leads to higher quality provision for a given number of providers. However, this reduces the profit of each provider and therefore reduces entry to the market. Thus, increased patient mobility leads to higher quality but a lower number of providers in equilibrium.
2.5 Information on Quality
The degree of patient mobility, and thus the incentive to compete on quality, may be enhanced by giving more accurate information about quality to patients, for example by publishing data on quality measures. Such information reduces the cost of quality comparisons among hospitals for GPs or patients. It seems intuitive that this would increase the responsiveness of demand to quality and hence increase the marginal profit from increasing quality. However, Gravelle and Sivey (2010) show that this argument is correct only when hospitals do not differ significantly in the quality they provide. If the difference between providers’ marginal cost of providing quality is large, then their quality differences will tend to be large. In such cases better information about quality may lead to lower quality. Demand at a hospital depends on the difference in quality between that hospital and a competing hospital, and on the distribution of the differences in the errors each patient makes when observing qualities at the two hospitals. Unless an individual patient’s errors in observing quality are perfectly correlated across hospitals, the distribution of the difference in errors for each patient is unimodal and centered on zero. For most patients the difference in their errors is small and few patients have large differences in errors. Thus the marginal revenue from improving quality is smaller, for both hospitals, when the true quality difference is large. Improving the accuracy of patient information makes it even less likely that they will have large differences in errors and thus reduces the marginal revenue from quality increases when the true quality difference is large. Thus if the initial quality difference is large better information will reduce marginal revenue from quality at both hospitals and thus reduce quality levels at both hospitals.
In a related study, Montefiori (2005) assumes that consumers can observe only noisy signals of quality, e.g. true quality with error term, and the error is normally distributed. He shows that patients’ utility is decreasing in the variance of the error term and that providers’ demand is a function also of the difference in the variance of the error term. He also shows that as long as the variance of the error term is the same across the two providers, the optimal quality incentives for the providers are not affected (since variances drop out from demand functions).
In Gravelle and Masiero (2000) GPs are paid by capitation (a fee for each patient registered in the practice). GPs compete on quality but quality is only imperfectly observed. They show that for a given capitation fee, the presence of imperfect information reduces the effect of a higher capitation fee on quality.
2.6 Gatekeeping
Another way to improve patients’ information about secondary care providers is to apply a gatekeeping system, where general practitioners act as gatekeepers to secondary care. Besides the cost containment argument, such a system is likely to ensure that potential patients get access to more accurate information about the characteristics (including quality) of secondary care providers.
Brekke et al. (2007) investigate how hospital quality competition is affected by the introduction of compulsory gatekeeping where every patient needs to have a referral to access a hospital specialist. In their two hospital model patients choose whether to consult a GP who can provide a diagnosis and information about which hospital is a better match for their diagnosis. The first order condition on quality is
where \( \lambda \) is the fraction of patients who consult a GP and \( 1 - \lambda \) is the fraction who directly approach the secondary care providers. Patients who consult GPs make an informed choice of providers and therefore this demand segment is responsive to quality (and specialization) differences. Those who do not consult a GP first are uninformed and choose providers randomly with probability 1/2. A gatekeeping system, which corresponds to setting \( \lambda = 1 \), may amplify or dampen competition depending on the relative size of two effects. On the one hand, competition is amplified by higher GP attendances, i.e., more patients get better recommendations on which provider to use, which makes demand more quality-responsive. On the other hand, incentives for quality competition can be dampened by improved accuracy in diagnosis, which reduces the relative importance of quality as a predictor for the best choice of secondary care provider.
2.7 Cost-Containment Effort
In the absence of cost reimbursement, any type of payment which does not vary with costs (for example a fixed budget or a prospective payment system like PbR) will give the appropriate incentive to keep costs down. If the provider is the residual claimant who has control over any surplus, the benefits from greater cost-reducing effort are equated to the marginal disutility from such effort.
The interaction between quality and cost-containment effort in the presence of patient choice has been analyzed by Brekke et al. (2012a) Assuming that providers are profit maximizers, we can write the optimal conditions for quality and cost-containment effort,
where \( C_{e} < 0 \) is the reduction in the treatment costs due to cost-containment effort, and \( G_{e} \) is the disutility from exerting such effort. We see that any effect of patient choice on cost-containment effort arises through the interaction with quality. If more patient choice increases quality, and cost-containment effort and quality are substitutes, i.e., \( \partial e^{ * } /\partial q < 0 \), then more patient choice may lead to lower cost-containment effort. This may be the case when doctor effort can be applied to improving quality of care for individual patients or to finding ways to reduce cost (for example choosing cheaper therapeutically equivalent drugs). Conversely \( \partial e^{ * } /\partial q > 0 \), if, for example, higher quality leads to higher volume of patients treated, which in turn may increase the marginal benefit from investing in cost-containment effort since the higher profit margin will apply to a larger volume of patients treated (Ma 1994).
2.8 Cream-Skimming
If providers can provide different levels of quality to different patients, then they might have an incentive to cream-skim, i.e., to increase the quality for profitable patients (where the profit margin is positive) and to ‘skimp’, i.e., to reduce the quality for non-profitable ones (where the profit margin is negative). These incentives may be strengthened in the presence of more intense competition (Ellis 1998). Therefore, if demand is more responsive to quality, providers have even stronger incentives to skimp on expensive patients and to cream-skim the inexpensive ones. Soft budgets will tend to dampen such incentives (Brekke et al. 2013a).
2.9 Interjurisdictional Mobility
A common feature of all the above-discussed analyses is that all health care providers in the market belong to the same health care jurisdiction. In other words, all patient mobility occurs within the same health care jurisdiction. However, in some countries patient mobility across different health care jurisdictions (regions) is an important issue (a prominent example is Italy). Furthermore, patient mobility across national borders is an increasingly important topic in Europe, particularly following recent changes in EU regulations which have strengthened patients’ rights to seek medical treatment in other member countries. Brekke et al. (2013b) have examined the implications for increased patient mobility across different health care jurisdictions on quality provision and welfare. They use a spatial competition framework with two regions, where health care quality is decided at regional level (to maximize regional welfare) and patients are allowed freely to choose between the providers in the two regions, which differ in their ability to provide high-quality health care.
They find that the effects of patient mobility on quality and welfare in the two regions depend crucially on the details of the transfer pricing scheme; i.e., the price paid by the exporting region (and received by the importing region) for patients who travel across borders to obtain health care. Any increase in quality tends to occur in the region that is the net importer of patients, while quality in the exporting region is reduced for any reasonable assumption regarding transfer pricing. However, with patient mobility across regions a larger share of the total population has access to higher-quality health care, so quality for the average patient may increase even if there is no increase in the amount of health care provided by either of the two regions. Allowing for cross-jurisdictional patient mobility also has different welfare effects in the two regions. Intuitively, a higher transfer price tends to favor the importing region at the expense of the exporting region. Importantly, even if allowing for patient mobility might constitute a Pareto improvement at the regional level, where both regions are (at least weakly) better off with mobility than without, such a policy tends always to have winners and losers at the individual patient level.
2.10 Dynamic Analysis
The above analyses use a static framework where providers play a one-shot game, and decisions on quality are made and are implemented in one period. Demand for health care tends to respond sluggishly to changes in quality provision. Because quality is not always easily observable and because of habits or trust in specific health care providers, patients may have sluggish beliefs about quality, which in turn will make demand adjustment sluggish. If a provider increases quality, sluggish beliefs about quality imply that it will take some time before the potential demand increase is fully realized. Therefore, demand may be less responsive when demand is more sluggish.
The implications of demand sluggishness for quality provision are analyzed in a differential-game dynamic setting by Brekke et al. (2012b) and Siciliani et al. (2013). They assume that actual demand vary over time as follows
where \( D\left( t \right) \) is actual demand in period \( t \), \( D^{ * } \left( t \right) \) is potential demand in period \( t \), and \( \gamma \in \left[ {0,1} \right] \) is an (inverse) measure of the degree of sluggishness in patients’ beliefs about provider quality. The higher is \( \gamma \), the less sluggish are these beliefs, and the faster is the demand response to quality changes.
In Brekke et al. (2012b) providers are assumed to be profit-maximizers. A lower degree of demand sluggishness will generally stimulate quality provision, regardless of the nature of competition between the providers. A less sluggish demand is analogous to an increase in responsiveness of demand which increases providers’ incentives to raise quality. However, the study shows that when providers are allowed to revise their investment decisions more frequently (which can be thought of as a more competitive environment compared to one where quality can be revised only after a long time gap), long-run quality may be lower if the marginal cost of treating a patient is increasing. This result arises because in a dynamic setting lower quality investment by one provider will induce a future reduction in quality investment by the other provider; in other words, quality levels are strategic complements over time. A similar results is derived in Brekke et al. (2010), where demand adjust instantaneously but quality is akin to a stock \( q(t) \) which increases over time \( t \) only if the investment in quality \( I(t) \) is higher than its depreciation rate: \( \partial q(t)/\partial t = I(t) - \delta q(t) \). Quality provision is found to be lower in the more competitive environment, where providers are allowed to revise their quality decisions more frequently.
This conclusion contrasts with the findings of Siciliani et al. (2013), who consider the case of partially altruistic health care providers. A reduction in demand sluggishness, for example through public policies that increase the degree of patient information, might lead to lower quality provision if the (exogenous) treatment price is sufficiently low. This result resembles the one found by Brekke et al. (2011) in a static setting (see Sect. 2.1) and the intuition is similar.
3 Empirical Evidence
There are two main empirical approaches to examining the relationship between patient choice and quality of care. The first approach is to test the fundamental assumption that patients choice is influenced by quality and providers with higher quality have a higher demand. Here, quality is an explanatory variable. The second approach tests whether more competition (as measured, for example, by the number of competitors or the Herfindhal index) affects quality. More competition should imply that the demand is more responsive to quality, and therefore competing providers have a stronger incentive to raise quality. Here, quality is the dependent variable.
3.1 Patient Choice and Quality
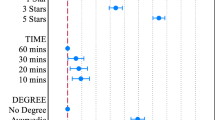
One of the key steps in the argument that greater competition, with fixed prices, can lead to higher quality is that the choice of a hospital by patients (or their GP advisors) is influenced by its quality relative to that of other available hospitals. Thus by improving quality, relative to other hospitals, a hospital can attract more patients and thereby increase its revenue. The papers are summarized in Table 1. We do not limit the papers to those for markets where price is regulated since we are interested in whether quality affects demand, holding other factors constant, rather than whether competition affects quality.
The analysis is usually conducted for patients in need of a specific treatment (i.e. coronary bypass, PTCA, kidney transplant, cataract surgery, hip replacement). Most of the studies suggest that, after controlling for other factors such as patient characteristics and distance, the probability of a hospital being chosen increases with measures of quality, though the demand elasticities with respect to quality are generally small.
Three of the 12 studies are set in the English NHS (Beckert et al. 2012; Gaynor et al. 2011; Sivey 2008) and are in line with the other, mainly US, studies (Folland 1983; Luft et al. 1990; Burns and Wholey 1992; Hodgkin 1996; Tay 2003; Ho 2006; Howard 2005; Pope 2009). Allowing for waiting times, distance, and patient characteristics, Beckert et al. (2012) and Gaynor et al. (2011) find that higher quality leads to increased demand and Sivey (2008) finds demand increases with quality though not in all his specifications.
Most of the papers model the choice of individuals among hospitals using either conditional logit or mixed logit. The conditional logit model can be motivated within a random utility framework (McFadden 1974). Assume that the utility of patient \( j \) choosing hospital \( i \) is \( U_{ji} = \beta d_{ji} + \gamma q_{i} + \varepsilon_{ji} \) where \( d_{ji} \) is the distance between patient’s \( j \) residential address and hospital \( i \) address, \( q_{i} \) is the quality of hospital \( j \) (e.g. mortality rates, readmission rates, waiting times) and \( \varepsilon_{ji} \) is the unobserved component of utility. If \( \varepsilon_{ji} \) are iid and follow type 1 extreme value distribution, then the probability of patient \( j \) choosing hospital \( i \) out of a total of \( N \) hospitals is given by:
Conditional logit models make the strong assumption that the probability of choosing hospital A rather than hospital B (\( p_{jA} /p_{jB} \)) is not affected by the characteristics of other hospitals. Thus the relative probabilities of choosing A over B when the choice set includes hospital C which has the same characteristics as B are assumed to be the same as when the choice set does not include C. But it seems more plausible that patients who would have chosen C will switch to B in its absence so that the proportion choosing A will fall.
Mixed logit models do not impose this restriction and also allow for the possibility that the effects of hospital characteristics on choice vary with unobservable characteristics of patients. The conditional logit model allows the effects of hospital characteristics on choice to vary only with observable characteristics of patients. The mixed logit model is computationally more demanding than the conditional logit model. Tay (2003) shows that the conditional logit underestimates the effect of distance on hospitals’ choice.
One of the problems in estimating the effects of hospital quality on choice is that measured hospital quality may depend on the mix of patients at the hospital and the mix of patients may depend in part on quality. Thus, for instance, measured quality is lower if the hospital attracts sicker patients and sicker patients care more about true quality, then the effect of quality on demand will be underestimated. Thus it is important to use measures of quality which allow for the effects of patient characteristics on quality. The papers do this in few ways. First, they may use a standardized quality measure for a hospital calculated as the ratio of actual quality to the quality which would be expected at the hospital given its patients mix. Second, individual patient quality can be regressed on patient characteristics and a hospital dummy and the estimated hospital effect is used as the measure of quality. Both methods are improved by using richer data on individual patients to estimate hospital quality. Third, as in Sivey (2012), demand is first estimated as a function of waiting time, distance and a hospital dummy variable capturing all unobserved hospital factors, and then the hospital effect regressed on hospital characteristics including quality. It is argued (Murdoch, 2006) that this procedure prevents the under-estimation of standard errors which arises if quality measures are entered directly in the demand model. Fourth, to control for time-invariant unobserved heterogeneity (such as the case mix) some studies use panel data including hospital fixed-effects (for example Hodgkin 1996; Tay 2003; Sivey 2012). The approach relies on variations in quality over time to identify an effect on demand. Sivey (2012) for example finds that while cross-sectional results suggest, that higher waiting times lead to an increased probability of hospital choice, panel data results suggest the opposite with higher waiting time reducing the probability of the choice. The counterintuitive cross-sectional results may be explained by unobserved heterogeneity, with hospitals with higher clinical quality attracting higher demand and therefore being characterised by longer waiting times and a higher probability of choice.
A second problem arises in systems, like the NHS, where hospital waiting times adjust to equate demand and supply. Higher treatment quality will lead to longer waiting times if the hospital does not increase the number of patients treated.
Thus waiting times should be included in the demand model because they affect demand and may be correlated with quality. Gaynor et al. (2011) also allow for the possibility that waiting time for coronary bypass (CABG) is correlated with unobserved aspect of CABG quality by using waiting times for other procedures in the same hospital as an instrumental variable for CAGB waiting time. Sivey (2008) estimates a model of waiting time for individual patients including patient characteristics and a hospital dummy and then calculates the waiting time for a hospital as the median of the estimated waiting times. This procedure removes any bias arising from the individual patient quality and waiting times being correlated with unobserved patient characteristics. Beckert et al. (2012) use a hospital level average waiting time which assumes that there are no unobserved hospital level quality measures affecting demand which are also correlated with waiting times.
One way for policy makers to influence the demand responsiveness to quality is to publish information on relative performance, such as risk-adjusted mortality and readmission rates for specific conditions such as CABG. There is evidence from the US that report cards can influence choice and hospitals’ market shares in the expected direction. The studies often use a natural-experiment set up since reports cards were introduced in some US states but not in others. For example, Cutler et al. (2004) show that hospitals with high mortality rates experience a 10 % reduction in coronary bypasses but this is not the case for hospitals with low mortality rates.
Mukamel et al. (2005) also finds that higher mortality rates reduce surgeons’ market shares. Dranove and Sfekas (2008) find that hospitals with bad reports have a smaller market share but only after accounting for the prior beliefs of the patients: i.e. the market share changes (upwards or downwards) only if the report cards convey information which suggests different quality from that which patients previously expected based on reputation and advice from family doctors. However, report cards may also induce providers to select patients and by avoiding more severe patients (at higher risk of mortality) as evidenced by Dranove et al. (2003).
3.2 Hospital Competition
Most studies on the relation between competition and quality are based on US experiences, but in recent years a number have used English data. The evidence from the US is generally mixed. When prices are fixed (as they are under Medicare in the US), Kessler and McClellan (2000) and Kessler and Geppert (2005) find that a positive effect of competition on quality in the US, Gowrinsankaran and Town (2003) find a negative effect, Shen (2003) finds mixed results, and Shortell and Hughes (1988) and Mukamel et al. (2001) find no effect. Recent evidence from England suggests that competition increases quality when prices are fixed (Cooper et al. 2011; Gaynor et al. 2010; Bloom et al. 2011a).Footnote 2
The basic empirical approach within a cross-sectional framework is:
where \( q_{i} \) is the quality provided by hospital \( i \), \( c_{i} \) is a measure of competition, and \( x_{i} \) is a vector of control variables. Quality is typically measures by mortality rates for patients admitted with acute myocardial infarction (AMI) (heart attacks) though occasionally other measures are used. The use of AMI mortality for emergency admissions as a quality measure is justified by its correlation with other measures of quality expected to influence demand for elective care. Competition is typically measured as the number of providers within a catchment area (e.g. 30 min travel time, 40 km) or the Herfindahl–Hirschman index (HHI) which is the sum of the providers’ squared market shares. Markets with higher HHIs are interpreted as less competitive.
An observed cross-sectional association between competition and hospital quality does not prove that competition affects quality. For example:
-
(i)
if higher quality hospitals disproportionately attract patients who are sicker and if the quality measure fails to allow appropriately for differences in casemix, and the competition measure is based on market shares, then the observed association between measured quality and measured competition will overestimate the effect of competition on true quality;
-
(ii)
if hospital competition is measured using hospitals’ shares of patients treated in an area and patient choice of hospital is influenced by quality, then higher quality hospitals will have greater market shares and will appear to be in less competitive markets, thereby underestimating the effect of competition;
-
(iii)
when competition is measured in terms of the numbers of alternative providers, there may be factors (such as population density or size) which influence both the entry/exit decisions of providers and the quality decisions of providers in the market.
A number of strategies are available to increase the likelihood that an observed association is evidence of causality.
-
(i)
Rich set of covariates. Including covariates which plausibly affect quality reduces the risk of omitted variable bias. In the studies of competition and quality this suggests in particular the need to allow for patient characteristics affecting measured quality i.e. for thorough casemix adjustment. Casemix adjustment by including age, gender etc. as explanatory variables is more flexible than first directly or indirectly standardizing quality with respect to age, gender etc.
-
(ii)
Predicted market shares. Some competition measures are based on patterns of use of providers, as in the Herfindahl–Hirschman index. But observed patterns of use reflect the quality of providers since quality affects patient choice. Thus a provider with higher quality will have larger market share and higher HHI and the estimated effect of competition (smaller HHI) on quality will be under-estimated. Kessler and McClellan (2000) therefore suggest that the HHI is calculated on predicted market shares that arise from estimates based on a demand model of the type described in Sect. 3.1 which includes distance as the key explanatory and which does not contain hospital quality or other hospital variables correlated with quality.
-
(iii)
Instrumental variables for competition: variables which are correlated with competition but which are not correlated with unobservable factors affecting quality. For example, Bloom et al. (2011a) use the political marginality of an area as an instrument for the competing number of hospitals, arguing that decisions on closing or merging hospitals will be affected by political considerations (public hospitals are less likely to be closed in marginal constituencies) is used which are independent of the quality a hospital. In their study on the effect of competition on management quality they have 2005/2006 cross-sectional data for 100 trusts (about 61 % of all NHS trusts). The key measure of competition is the number of hospitals within a 30 km radius. They find that increasing the number of rival providers by three increases the index of management quality by more than a standard deviation, which implies a 6 % reduction in AMI mortality rates.
-
(iv)
Difference in differences: compare changes in quality over time for providers which had different changes in competition. The obvious way to implement this strategy is compare hospitals where rivals entered or left with those where the set of rivals was unchanged. Alternatively, one can argue that competition depends both on market structure (numbers of rivals or market shares) and on national competition policy and that changes in national policy lead to different changes in effective competitive pressures for providers depending on their market structure. The methodology of difference-in-difference relies on the assumption of common trends: quality would have changed at the same rate for providers with different number of competitors in the absence of the change in structure or competition policy. If the trends differ, then the estimated effect of greater competition will be biased upwards if quality improves more rapidly in more competitive areas. It is possible, as in Cooper et al. (2011), to allow differential trends in the high and low competition groups of hospital and to test if the change in policy affected the trend one group compared to the other.
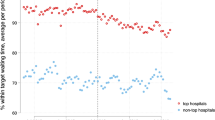
Cooper et al. (2011) estimates the effect of competition on AMI mortality rates during a period (2002–2008) when prices were fixed. The analysis uses data from 227 hospital sites as opposed to data aggregated at Trust level (therefore allowing for Trusts with multiple sites). They assume that the introduction of the Patient Choice policy from 2005 onward led to an increase in competition and that this led to an increase in effective competition which was greater in areas with more providers. Competition was measured using market shares based on predicted rather than actual demand. They estimate a difference-in-difference model and find that the introduction of Patient Choice policy was associated with a bigger reduction in AMI mortality in more competitive areas. AMI mortality fell by 0.31 % points per year faster in areas where competition was more intense by one standard deviation of their market structure indicator.
Gaynor et al. (2011) use a similar methodology, also arguing that the introduction of Patient Choice increased competition more for hospitals in markets with a more competitive structure and using predicted demand to calculate market shares. They use two years of data: 2003 and 2007. The sample includes 130 hospitals (trusts) in 2003 and 121 in 2007. They find that hospitals which had a 10 % higher Herfindahl index (i.e. faced less competition) in 2003 had a smaller (by 2.9 %) decrease in AMI mortality rates between 2003 and 2007. There is a similar association for overall mortality rates, though the effect is quantitatively smaller. Hospitals facing less competition in 2003 also had an increase in overall length of stay between 2003 and 2007 relative to providers facing more competition in 2003.Footnote 3
4 Conclusions
Patient choice and mobility across providers (such as hospitals and GPs) are likely to become permanent features of health systems in several countries. This chapter has focussed on the theoretical and empirical literature on patient choice and quality competition when prices are regulated. The theoretical literature suggests that more choice increases quality if providers are profit maximizers and the marginal cost is constant. The results are less clear-cut when providers are altruistic and the marginal cost of treatment is increasing. For sufficiently high altruism, providers may be willing to work at a negative profit margin and more choice may then reduce quality. We have also outlined that profit constraints may dampen incentives to compete on quality but, if providers are altruistic, may contribute to increase the relative weight given to patients so that the overall effect on quality is indeterminate. Hospitals may also dampen incentives to compete on quality by specializing. When considering patients mobility across different regions (or countries) transfer pricing schemes between the importing and exporting regions play a critical role to align regions’ incentives. The empirical literature generally confirms that demand responds to quality and waiting times though demand elasticities are generally low. Recent empirical studies mainly from the US and the UK generally confirm that more competition among hospitals is positively related to quality.
Notes
- 1.
- 2.
See Gaynor (2006), Gaynor and Town (2011), and Propper (2012), for a detailed review of the literature. When prices are variable and endogenously determined, the evidence from the US finds a positive relationship between competition and quality in Sari (2002), Gowrisankaran and Town (2003), and Abraham et al. (2007). However, in England Propper et al. (2004) and Burgess et al. (2008) find a significant (though small) negative relationship for a period in which hospital prices were not centrally regulated.
- 3.
References
Abraham, J. M., Gaynor, M., & Vogt, W. B. (2007). Entry and competition in local hospital markets. Journal of Industrial Economics, 2, 265–288.
Barros, P. P., & Martinez-Giralt, X. (2012). Models of negotiation and bargaining in health care. In A. Jones (Ed.), The Elgar companion to health economics (pp. 231–239). Cheltenham: Edward Elgar.
Beckert, W., Christensen, M., & Collyer, K. (2012). Choice of NHS-funded hospital services in England. Economic Journal. doi: 10.1111/j.1468-0297.2012.02496x.
Bevan, G., & Skellern, M. (2011). Does competition between hospitals improve clinical quality? A review of evidence from two eras of competition in the English NHS. British Medical Journal, 343, d6470.
Bloom, N., Propper C., Seiler S., & Van Reenen, J. (2011a). The impact of competition on management quality: Evidence from public hospitals, CEP Discussion Paper N. 983.
Bloom, N., Cooper, Z., Gaynor, M., Gibbons, S., Jones, S., McGuire, A., et al. (2011b). In defence of our research on competition in England’s national health service. The Lancet, December 17/24/31:2064–2065.
Bloom, N., Cooper, Z., Gaynor, M., Gibbons, S., Jones, S., McGuire, A., et al. (2012). A response to Pollock et al (2011). http://www.bristol.ac.uk/cmpo/publications/other/cpresponse.pdf.
Brekke, K. R., Nuscheler, R., & Straume, O. R. (2006). Quality and location choices under price regulation. Journal of Economics and Management Strategy, 15, 207–227.
Brekke, K. R., Nuscheler, R., & Straume, O. R. (2007). Gatekeeping in health care. Journal of Health Economics, 26, 149–170.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2008). Competition and waiting times in hospital markets. Journal of Public Economics, 92, 1607–1628.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2011). Hospital competition and quality with regulated prices. Scandinavian Journal of Economics, 113, 444–469.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2012a). Quality competition with profit constraints. Journal of Economic Behavior and Organization, 84, 642–659.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2013a). Hospital competition with soft budgets. Mimeo, Braga, Portugal.
Brekke, K. R., Cellini, R., Siciliani, L., & Straume, O. R. (2010). Competition and quality in regulated markets: A differential-game approach. Journal of Health Economics, 29, 508–523.
Brekke, K. R., Cellini, R., Siciliani, L., & Straume, O. R. (2012b). Competition in regulated markets with sluggish beliefs about quality. Journal of Economics and Management Strategy, 21, 131–178.
Brekke, K. R., Levaggi, R., Siciliani, L., & Straume, O. R. (2013b). Patient mobility, health care quality and welfare. Mimeo, Bergen, Norway.
Burgess, S., Propper, C., & Gossage, D. (2008). Competition and quality: Evidence from the NHS internal market 1991–9. The Economic Journal, 118, 138–170.
Burns, L. R., & Wholey, D. R. (1992). The impact of physician characteristics in conditional choice models for hospital care. Journal of Health Economics, 11, 43–62.
Cooper, Z., Gibbons, S., Jones, S., & McGuire, A. (2011). Does hospital competition save lives? Evidence from the English patient choice reforms. Economic Journal, 121(554), F228–F260.
Cutler, D., Huckman, R., & Landrum, M. B. (2004). The role of information in medical markets: An analysis of publicly reported outcomes in cardiac surgery. American Economic Review, 94, 342–346.
Dranove, D., Kessler, D., McLellan, M., & Satterthwaite, M. (2003). Is more information better? The effects of ‘report cards’ on health care providers. Journal of Political Economy, 111(3), 555–588.
Dranove, D., & Sfekas, A. (2008). Start spreading the news: A structural estimate of the effects of New York hospital report cards. Journal of Health Economics, 27(5), 1201–1207.
Ellis, R. (1998). Creaming, skimping and dumping: Provider competition on the intensive and extensive margins. Journal of Health Economics, 17(5), 537–555.
Folland, S. T. (1983). Predicting hospital market shares. Inquiry, 20, 34–44.
Gaynor, M. (2006). What do we know about competition and quality in health care markets? Foundations and Trends in Microeconomics, 2(6), 441–508.
Gaynor, M., & Vogt, W. B. (2003). Competition among hospitals. RAND Journal of Economics, 34, 764–785.
Gaynor, M., Moreno-Serra R., & Propper, C. (2011). Death by market power: Reform, competition and patient outcomes in the national health service, CMPO Working Paper No. 10/242.
Gaynor, M., Propper, C., & Seiler, S. (2010). The effect of patient choice. Evidence from recent NHS reforms. cep.lse.ac.uk/conference_papers/10-05-2010/seiler.pdf.
Gaynor, M., & Town R. (2011). Competition in health care markets. In M. V. Pauly, T. G. McGuire, P. P. Barros (Eds.), Handbook of health economics (Vol 2). Elsevier, Amsterdam.
Gowrisankaran, G., & Town, R. (2003). Competition, payers, and hospital quality. Health Services Research, 38, 1403–1422.
Gravelle, H. (1999). Capitation contracts: Access and quality. Journal of Health Economics, 18, 315–340.
Gravelle, H., & Masiero, G. (2000). Quality incentives in a regulated market with imperfect competition and switching costs: Capitation in general practice. Journal of Health Economics, 19, 1067–1088.
Gravelle, H., & Sivey, P. (2010). Imperfect quality information in a quality-competitive hospital market. Journal of Health Economics, 29, 524–535.
Hodgkin, D. (1996). Specialized service offerings and patients’ choice of hospital: The case of cardiac catheterization. Journal of Health Economics, 15, 305–332.
Ho, K. (2006). The welfare effects of restricted hospital choice in the US medical care market. Journal of Applied Econometrics, 21, 1039–1079.
Howard, D. H. (2005). Quality and consumer choice in health care: Evidence from kidney transplantation. Topics in Economic Analysis and Policy, 5(1), 1349.
Kessler, D., & McClellan, M. (2000). Is hospital competition socially wasteful? The Quarterly Journal of Economics, 115, 577–615.
Kessler, D. P., & Geppert, J. J. (2005). The effects of competition on variation in the quality and cost of medical care. Journal of Economics and Management Strategy, 14(3), 575–589.
Luft, H. S., Garnick, D. W., Mark, D. H., Peltzman, D. J., Phibbs, C. S., Lichtenberg, E., et al. (1990). Does quality influence choice of hospital? JAMA, 263, 2899–2906.
Ma, C. A., & Burgess, J. F. (1993). Quality competition, welfare, and regulation. Journal of Economics, 58, 153–173.
Ma, C. A. (1994). Health care payment systems: Cost and quality incentives. Journal of Economics and Management Strategy, 3, 93–112.
McFadden, D. (1974). Conditional logit analysis of qualitative choice behaviour. In P. Zarembka (Ed.), Frontiers in econometrics (4, pp. 105–142). New York: Academic Press.
McGuire, T. (2000). Physician agency, In A. J. Culyer & J. P. Newhouse (Eds.), Handbook of health economics (Vol. 1). Amsterdam: Elsevier.
Montefiori, M. (2005). Spatial competition for quality in the market for hospital care. European Journal of Health Economics, 6, 131–135.
Mukamel, D., Zwanziger, J., & Tomaszewski, K. J. (2001). HMO penetration, competition and risk-adjusted hospital mortality. Health Services Research, 36, 1019–1035.
Mukamel, D. B., Weimer, D. L., Zwanziger, J., Gorthy, S. F., & Mushlin, A. I. (2005). Quality report cards, selection of cardiac surgeons, and racial disparities: A study of the publication of the New York state cardiac surgery reports. Inquiry, 41, 435–446.
Murdoch, J. (2006). Handling unobserved site characteristics in random utility models of recreation demand. Journal of Environmental Economics and Management, 51,1–25.
Nuscheler, R. (2003). Physician reimbursement, time consistency, and the quality of care. Journal of Institutional and Theoretical Economics, 159(2), 302–322.
OHE, (2012). Report of the Office of Health Economics Commission on Competition in the NHS. London: Office of Health Economics.
Pollock, A., Macfarlane, A., Kirkwood, G., Majeed, A., Greener, I., Morrelli, C., et al. (2011a). No evidence that patient choice in the NHS saves lives. The Lancet, 378, December 17/24/3, 2057–2060.
Pollock, A., Majeed, A., Macfarlane, A., Greener, I., Kirkwood, G., et al. (2011b). Authors’ reply. The Lancet, 378, December 17/24/31, 2065–2066.
Pope, D. (2009). Reacting to rankings: Evidence from “America’s best hospitals”. Journal of Health Economics, 28, 1154–1165.
Propper, C. (2012). Competition, incentives and the English NHS. Health Economics, 21, 33–40.
Propper, C., Burgess, S., & Green, K. (2004). Does competition between hospitals improve the quality of care? Hospital death rates and the NHS internal market. Journal of Public Economics, 88(7–8), 1247–1272.
Sari, N. (2002). Do competition and managed care improve quality? Health Economics, 11, 571–584.
Shen, Y.-S. (2003). The effect of financial pressure on the quality of care in hospitals. Journal of Health Economics, 22, 243–269.
Shortell, S. M., & Hughes, E. F. (1988). The effects of regulation, competition, and ownership on mortality rates among hospital inpatients. New England Journal of Medicine, 318, 1100–1107.
Siciliani, L., Straume, O.R., and Cellini, R. (2013). Quality competition with motivated providers and sluggish demand, Journal of Economic Dynamics and Control. 37, 2041–2061, forthcoming.
Sivey, P. (2008). The effect of hospital quality on choice of hospital for elective heart operations in England. Chapter 4 in The Economics of Patient Choice and Information in the National Health Service, Ph.D. Thesis. University of York, York.
Sivey, P. (2012). The effect of waiting times and distance of hospital choice for English cataract patients. Health Economics, 21, 444–456.
Tay, A. (2003). Assessing competition in hospital care markets: The importance of accounting for quality differentiation. RAND Journal of Economics, 34, 786–814.
Varkevisser, M., van der Geest, S., & Schut, F. (2010). Assessing hospital competition when prices don’t matter to patients: The use of time elasticities. International Journal of Health Care Finance and Economics, 9(4), 347–366.
Varkevisser, M., van der Geest, S., & Schut, F. (2012). Do patients choose hospitals with high quality ratings? Empirical evidence from the market for angioplasty in the Netherlands. Journal of Health Economics, 31, 371–378.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Italia
About this chapter
Cite this chapter
Brekke, K.R., Gravelle, H., Siciliani, L., Straume, O.R. (2014). Patient Choice, Mobility and Competition Among Health Care Providers. In: Levaggi, R., Montefiori, M. (eds) Health Care Provision and Patient Mobility. Developments in Health Economics and Public Policy, vol 12. Springer, Milano. https://doi.org/10.1007/978-88-470-5480-6_1
Download citation
DOI: https://doi.org/10.1007/978-88-470-5480-6_1
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5479-0
Online ISBN: 978-88-470-5480-6
eBook Packages: Business and EconomicsEconomics and Finance (R0)