Abstract
Even though more than 100 years have passed since the first description of the use of central blocks in children (Bier, 1899, Tyrell-Gray, 1909), there are still new and important things to learn within this particular field of anesthesia. Therefore, to perform safe and effective regional anesthesia in infants and children, a solid knowledge of the age-related pharmacology of both local anesthetics and their adjuncts is an absolute prerequisite. Although not as extensive as in adults, the published literature within the field of clinical pharmacology of local anesthetics and their adjuncts in infants and children is quite substantial at this point in time.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 12.1 Drugs and Clinical Pharmacology of Central Blocks in Infants and Children
Even though more than 100 years have passed since the first description of the use of central blocks in children (Bier, 1899, Tyrell-Gray, 1909), there are still new and important things to learn within this particular field of anesthesia. Therefore, to perform safe and effective regional anesthesia in infants and children, a solid knowledge of the age-related pharmacology of both local anesthetics and their adjuncts is an absolute prerequisite. Although not as extensive as in adults, the published literature within the field of clinical pharmacology of local anesthetics and their adjuncts in infants and children is quite substantial at this point in time.
To avoid redundant publications and the repetition of already published material within this field, I have refrained from producing yet another text on this topic. Instead, the current chapter provides a synopsis of the current knowledge and incorporates the reproduction of a review article by Professor Jean-Xavier Mazoit, titled Local Anesthetics and their Adjuncts, which was recently published in Pediatric Anesthesia (http://onlinelibrary.wiley.com/doi/10.1111/j.1460-9592.2011.03692.x/pdf). This has been made possible by the kind permission of Professor Mazoit, the editor-in-chief Neil Morton, and by Wiley-Blackwell Publishing Ltd. For information on the toxicity aspects, the reader is referred to another review from the same themed issue of Pediatric Anesthesia [1] (works cited in paragraph 12.1 have been kept separately in the first group of references listed at the end of the chapter).
Following the publication of the review article reproduced herein, further information and discussion has been published with regard to the use of ketamine as an adjunct in newborns and infants. Thus, in rodent experiments, Walker and colleagues have been able to show that the application of clinically relevant doses of intrathecal ketamine in young rodents does result in apoptosis of spinal neurons as previously shown for cortical neurons [2]. This is in sharp contrast to findings from similar studies for morphine and clonidine, both appearing to be associated with a comfortable margin of safety with regard to programmed spinal cord cell death [3, 4]. Based on these findings, a recent editorial in the British Journal of Anaesthesia questioned the use of ketamine as an adjunct to caudal and epidural blocks in newborns and infants and instead recommended the use of clonidine in a situation when an adjunct drug is deemed necessary in this age group [5]. Therefore, the key points are:
-
1.
Due to the reduced toxicity risk compared to racemic bupivacaine, the regular use of ropivacaine or levobupivacaine is advocated in infants and children (with the exception of intrathecal blockade).
-
2.
There is little evidence for the efficacy of the use of opioids as adjuncts to central blocks in children (with the exception of preservative-free morphine). Within this context, it should also be remembered that opioids, apart from being associated with a risk of respiratory depression, are also associated with a number of less serious but still very distressing side effects (e.g., postoperative nausea and vomiting, pruritus, urinary retention, and interference with gastrointestinal motility) [6].
-
3.
For a single-injection caudal block in children above 1 year of age, the use of ketamine appears the most effective adjunct in prolonging the duration of the block.
-
4.
Clonidine is associated with a good safety profile and can be used as an adjunct drug in all age groups. It can also be used as an adjunct for both central and peripheral nerve blocks [7].
-
5.
The use of adjuncts other than preservative-free solutions of clonidine, ketamine, and morphine must still be seen as experimental and should not be used routinely [8].
When reading the review by Professor Mazoit which follows, the reader should be mindful of a typographical error. With regard to the dosing of the lipid rescue, mL (milliliters) rather than mg (milligrams), should have been used throughout. The initial dose of Intralipid is 2–5 mL/kg-1 and can be repeated up to a total of 10 mL/kg-1, rather than 10 mg/kg-1.
2 12.2 Local Anesthetics and Their Adjuncts: A Review Article by Jean-Xavier Mazoit
Local anesthetics (LA) block propagation of impulses along nerve fibers by inactivation of voltage-gated sodium channels, which initiate action potentials [1]. They act on the cytosolic side of phospholipid membranes. Two main chemical compounds are used, amino esters and amino amides. Amino esters are degraded by pseudocholinesterases in plasma. Aminoamides are metabolized exclusively by the liver. Only amide LAs will be considered in this article.
2.1 12.2.1 Pharmacokinetics
Local anesthetics (LAs) are small molecules with molecular weights ranging from 220 to 288 [2]. They contain an aromatic ring, an intermediate chain (amide group), and a hydrophilic residue with a tertiary amine. They are weak bases with pKas between 7.6 (mepivacaine) and 8.1 (bupivacaine and ropivacaine). At a pH of 7.40, 60-85% of the molecules are ionized and diffuse in hydric compartments. LAs are also soluble in lipids and then easily cross cell membranes. Bupivacaine is ten times more liposoluble than lidocaine; ropivacaine is four times as soluble as lidocaine (partition coefficient from XlogP) (Table 12.1). With the exception of lidocaine, all amide LAs possess an asymmetric carbon. Although the physiochemical properties (pKa, distribution coefficient) of the isomers are identical, the enantiomers have different affinities for the biological effectors (channels, receptors, proteins) [3]. Ropivacaine and levobupivacaine are pure S-(−) enantiomers. LAs are marketed as hydrochloride salts in water at pH of 4–5 to prevent them from precipitation [4]. Plain solutions of amide LAs are preservative-free; only epinephrine-containing solutions include metabisulfite.
2.1.1 12.2.1.1 Binding to Blood Components
Amide LAs distribute in red cells (20-30% depending on the hematocrit) and bind to serum proteins [2, 5]. Like most weak bases, amide LAs bind to both a1-acid glycoprotein (AGP) and to human serum albumin (HSA). The stereospecificity of this binding is insignificant, at least on a clinical point of view [6]. Despite its low concentration in serum (< 1 g/L-1 in adults), AGP is the major protein that binds LAs. AGP concentration is very low at birth and progressively increases during the first year of life [5, 7]. It is why neonates and young infants have a much higher free fraction of LAs than adults. AGP is an acute phase protein, and its concentration increases rapidly in inflammatory states like in the postoperative period [7]. LAs also bind to HSA, but with a very low affinity. It is only because HSA is the most abundant protein in serum that its binding capacity is significant.
2.1.2 12.2.1.2 Absorption
After applying topical anesthesia to the upper airway, LAs are rapidly absorbed. This may induce toxicity, particularly in young children. This is why it is important to use nozzles that deliver no more than 10 mg with each squeeze [8]. The EMLA (Eutectic Mixture of Local Anesthetics) cream is absorbed in significant amounts in premature babies and neonates [9]. The cream contains prilocaine, which produces methemoglobinemia in neonates and infants, especially if they are also treated with trimethoprim-sulfamethoxazole [10]. The efficacy of the cream has been questioned in premature babies because of a high skin blood flow [9].
After injection, amide LAs have a bioavailability of one (metabolism is exclusively hepatic) [11]. They bind to tissues, which delays their absorption. This delay varies depending on the site of injection. In adults, 3 h after an epidural injection, only 70% of a dose of lidocaine and 50% of a dose of bupivacaine or of ropivacaine are absorbed, which are safety factors [11]. From adult studies, it is clear that the speed of drug absorption decreases from head to foot and from the thoracic to the caudal portion of the epidural space. Lidocaine and bupivacaine concentrations peak about 30 min after caudal or lumbar injection in infants and adults [5, 12–17]. The Tmax for ropivacaine is much longer in infants than in children [18, 19] and possibly in children than in adults [18–26]. CYP1A2, which metabolizes lidocaine and ropivacaine, is immature before 4–7 years of age [27].
Levobupivacaine is principally metabolized by the CYP3A4/7, which has full enzymatic capacity by the age of 1 year [28].
2.1.3 12.2.1.3 Distribution
The volume of distribution of LAs at steady state (Vss) is slightly < 1 L/kg-1 (Table 12.2) [5, 11–26]. Because of delayed drug absorption leading to the ‘flip-flop’ effect,Footnote 1 terminal half-lives and volumes calculated after non-intravenous (i.v.) routes of administration are markedly overestimated [11, 20, 29–31]. Only total body clearance of the drug is measured accurately following extravascular administration (but sampling must take place over a prolonged period of time). It is highly probable that LAs distribute in a larger volume in neonates and in infants than in adults, thus preventing high serum drug concentrations from occurring after a single injection, but not following several injections. The volume of distribution of ropivacaine is smaller than that of bupivacaine in adults and probably in pediatric patients [2].
2.1.4 12.2.1.4 Elimination
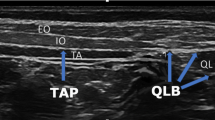
All amide LAs are metabolized by the liver cytochrome P450 enzymes. Bupivacaine is predominantly metabolized into pipecoloxylidide (PPX) by CYP3A4/7 [28]. Ropivacaine is predominantly metabolized to 3’- and 4’-OH-ropivacaine by CYP1A2 and to a minor extent to PPX by CYP3A4 [27]. These enzymes are not fully mature at birth and have important differences in their developmental expression. Contrary to lidocaine, bupivacaine and ropivacaine have a relatively low hepatic extraction ratio (0.30-0.35) and are considered rate limited for their elimination. Thus, the intrinsic hepatic clearance and the free fraction are the major determinants of total clearance. After surgery, serum AGP concentrations increase, which increases protein binding. A parallel decrease in total clearance is observed [7]. However, this only leads to a resetting in total serum concentration, and the unbound concentration remains constant. Bupivacaine clearance is low at birth and increases slightly during the first 6–9 months of life (Fig. 12.1). is also low in neonates and infants, increases during the first 2–6 years of life [19]. This is likely the cause of the delayed ropivacaine Cmax observed in the younger patients after caudal injection.
Bupivacaine plasma concentrations measured in two groups of infants receiving continuous bupivacaine infusion by the caudal route for postoperative analgesia. Dosing was calculated to maintain steady concentrations in the older patients (> 9 months old). The bupivacaine concentrations increased with infusion time in the younger infants (< 4 months old), thus demonstrating that clear-ance was markedly lower in the younger patients. Reproduced from Luz G, Innerhofer I, Bachmann B et al. Bupivacaine plasma concentrations during continuous epidural anesthesia in infants and children. Anesth Analg 1996; 82: 231–234. February 1, Lippincott Williams & Wilkins [78]
Concentrations leading to toxicity are largely unknown. In adult volunteers, the threshold of toxicity is about 0.2-0.3 mg/L-1 of unbound bupivacaine and 0.4-0.6 mg/L-1 of unbound ropivacaine or levobupivacaine [32–35]. Neonates and infants seem to be more prone to develop toxicity [36, 37] because of a higher serum free fraction, a lower clearance, and an increased susceptibility to cardiac toxicity. During prolonged administration of LAs for postoperative pain relief, it is assumed that the intrinsic unbound clearance is unaffected during the whole period of administration and the unbound concentration reaches a steady level 12–18 h after the initiation of infusion. Because of the inflammatory process leading to increased serum binding capacity, the plasma concentrations of total (levo) bupivacaine and ropivacaine tend to increase postoperatively during more than 2–4 days.
2.2 12.2.2 Pharmacodynamics
Local anesthetics block the propagation of impulses along nerve fibers because of the inactivation of voltage-gated sodium channels. LAs cross membranes as free bases (unionized). Inside the cells, they become ionized and bind to specific amino acids within the channel pore, thus mechanically blocking the pore [1]. LAs also block potassium and calcium channels at slightly higher drug concentrations than those needed to block sodium channels [38, 39]. Voltage-gated potassium channels initiate repolarization in the nerve. In the myocardium, some of these channels [including the human ether-a-go-go related gene (hERG) channel] are responsible for genetically induced arrhythmias, such as the long-QT, short- QT, or Brugada syndromes. These channels are blocked by LA concentrations just slightly higher than those needed to block sodium channels [38, 39]. Unlike the central nervous system (CNS) and heart, peripheral nerves only express a small number of potassium channels. Both sodium and potassium channel blockades are stereospecific [38–40]. The S enantiomers induce less block than R enantiomers. LAs bind to the myocardial ryanodine receptor and L-type calcium channels [41, 42], but it is unclear if blockade of these channels affect the cardiotoxicity of long-lasting LAs.
Nerve fibers are either myelinated or unmyelinated. After initial depolarization, the sodium channels become unreceptive to stimulation (refractory period), which prevents backward propagation of impulses. The action potential of unmyelinated fibers propagates continuously.
Myelin insulates myelinated fibers, and this layer is interrupted regularly by the nodes of Ranvier. The sudden depolarization of the node induces an electrical field, which extends to 2–3 nodes. Action potentials “jump” rapidly from one node to the next. Because the distance between nodes is greater in heavily myelinated fibers (there are 3–4 nodes per cm in Aa fibers and 20–30 nodes per cm in Ad fibers), the conduction velocity is faster in motor than in small sensory fibers and faster in small sensory fibers than in high threshold fibers that conduct pain signals [43]. Small unmyelinated or lightly myelinated fibers-the fibers that conduct pain signals-are blocked by lower concentrations of drug and during a longer period of time than heavily myelinated fibers. Myelinization begins during the third trimester of pregnancy and is incomplete at birth. After birth, myelinization increases rapidly and is almost complete by 3–4 years of age [44, 45]. In rats, the nodes of Ranvier are fully mature at 2–3 weeks of age. Interestingly, the internode distance is similar between 2-week-old and adult rats. This may explain why infants and young children need larger volumes per kg of LAs than older children or adults (Fig. 12.2) [46].
Duration of sciatic nerve motor block in infant rats according to the dose of bupivacaine used. Rats aged 5 days had a prolonged block as compared to the other two groups. Twoweek-old rats had a similar duration of block as compared to 10-week-old rats despite an 8–10 times difference in body weight: The same dose gave the same duration of block likely because the internode distance is fixed after the age of 1–2 weeks [drawn from the data of Kohane DS, Sankar WN, Shubina M et al. Sciatic nerve blockade in infant, adolescent, and adult rats: a comparison of ropivacaine with bupivacaine. Anesthesiology 1998; 89: 1199–1208. November, Lippincott Williams & Wilkins [46]
Fortunately, the concentration of LA needed to cause the block is lower. Surprisingly, infants require larger doses of LAs for spinal anesthesia, and the duration of the spinal block is shorter. Some authors have attributed this difference to larger volumes and a more rapid turnover of cerebrospinal fluid (CSF) in neonates and infants than in older children and adults. However, MRI studies have shown that the CSF volume and CSF turnover are lower in neonates and infants than in children and adults [47, 48]. The major factor responsible for this short effect seems to depend on the number of nodes of Ranvier blocked because the distance between nodes is fixed soon after birth [44, 45].
2.2.1 12.2.2.1 Effects on the Central Nervous System and Cardiovascular System
Like all inhibitors of sodium channels, LAs possess anticonvulsive effects at low dosage, which is why lidocaine is still used to treat intractable epilepsy in neonates and infants [49]. At higher doses, LAs induce convulsions and coma. However, the therapeutic ratio is low. In similar concentrations to those that cause convulsions, long-lasting LAs can induce cardiac arrhythmias. With the exception of nodal conduction, which depends on calcium channels, conduction in the heart depends on sodium channels. LAs prolong the refractory period, but the balance between the increase in effective refractory period and the decrease in the ventricular conduction velocity does not favor LAs. Long-lasting LAs, like bupivacaine, profoundly decrease ventricular conduction velocity [50–52]. This phenomenon is markedly amplified by tachycardia-it is the phasic block. Because neonates and infants have higher heart rates than adults, they are likely more sensitive to LA-induced blocks than adults. LAs also impair myocardial contractility but without any stereospecificity [52]. The S enantiomers (ropivacaine and levobupivacaine) have mild vasoconstrictive properties.
2.2.2 12.2.2.2 Stereospecificity
Mepivacaine, prilocaine, bupivacaine, and ropivacaine have an asymmetric carbon. Protein binding, pharmacokinetics, and nerve blocks have little stereoselectivity, which is why levobupivacaine has almost the same blocking properties as its racemic counterpart. In the heart, the effect on cardiac conduction is stereospecific (ropivacaine and levobupivacaine induce much less block than their corresponding R (+) enantiomer or the racemic mixture), whereas contractility is unaffected by stereoselectivity [51, 52].
LAs have anti-inflammatory properties and inhibit platelet aggregation [53], decrease leukocyte priming and the production of free radicals [54–56]. Systemically administered lidocaine has antinociceptive effects, particularly on neuropathic pain [57]. Consequently, LAs are now used preoperatively to prevent postoperative hyperalgesia in adults [58]. Interestingly, LAs can prevent and even treat complex regional pain syndrome in adults and children by limiting the neuropathic inflammatory processes [59, 60].
2.2.3 12.2.2.3 Toxicity of Local Anesthetics
At the site of injection, the minimum concentration required to produce a nerve blockade is 300–1500 μM for lidocaine and 100–500 μM for bupivacaine [61]. These concentrations (in the millimolar range) impair mitochondrial function and may be responsible for the observed nerve and muscle toxicity. Care should be taken when regional anesthesia is provided for eye surgery in adults, for children with myopathies (bupivacaine is an in vitro model of Duchene’s myopathy), and perhaps for children with mitochondrial cytopathy [62, 63]. With that respect, the site of injection for central blocks is far from any muscle.
After both local and regional anesthesia, neurological or cardiac toxicity related to excessive blood concentration may occur [64, 65]. Because of their low protein binding and intrinsic clearance, infants are more prone to LA toxicity than adults. General anesthesia may conceal the early signs of LA toxicity in children. In addition to pharmacokinetic factors, the rapid heart rate of children may increase the risk of cardiac toxicity induced by LA toxicity. Ropivacaine and levobupivacaine [S-())-enantiomers] are less toxic than racemic bupivacaine [32–35]. Even if toxic events occur with ropivacaine, small doses of epinephrine should produce rapid recovery. Impaired ventricular conduction is the primary manifestation of LA toxicity. QRS widening, bradycardia, and torsades de pointe are followed by either ventricular fibrillation and/or asystole [65]. The slight decrease in myocardial contractility caused by LAs is usually not a major problem. Treatment includes oxygenation, cardiac massage, and epinephrine, which is given in small incremental boluses beginning with 1–2 μg/kg-1 [66]. If ventricular fibrillation persists, defibrillation (2–4 J/kg-1) is performed. Although resuscitation measures must be initiated immediately, the specific treatment of LA toxicity is rapid administration of Intralipid (Kabivitrum Inc., Stockholm, Sweden). Numerous case reports have shown that rapid bolus injections of a lipid emulsion reverse the toxic effects of LAs [66–69]. Because 1 mole of Intralipid (Kabivitrum Inc.) binds > 3000 times more molecules of bupivacaine than a mole of buffer, the volume of distribution suddenly increases [70]. The recommended dose of 20% Intralipid (Kabivitrum Inc.) for pediatric patients is 2–5 mL/kg-1 by i.v. bolus. If cardiac function does not return, this dose (up to 10 mg/kg-1) is repeated. The lipid emulsion decreases LA elimination; thus, the cardiac effects may recur later.
2.2.4 12.2.2.4 Adjuvants
Adjuvants are often used to prolong the duration of analgesia.
Adrenaline (5 μg/mL-1 = 1/200,000) decreases bupivacaine Cmax, without affecting the time to peak concentration. In < 6-month-old infants, 2.5 μg/mL-1 1/400,000 epinephrine has been recommended [71]. However, the drug is less efficacious with long-acting S-())- enantiomers and has limited use with these solutions. Plain solutions of LAs must be used for penile, interdigital, and eye blocks. Adrenaline also slightly increases the duration of postoperative analgesia after caudal anesthesia. Clonidine 1–2 μg/kg-1, either i.v. or in the epidural space, prolongs the duration of caudal blocks [72]. Clonidine also enhances the efficacy of dilute long-acting agents (e.g., 0.1% ropivacaine). More than 2 g/kg-1 may lead to hypotension.
Clonidine is not recommended for infants < 3 months of age because it can cause apnea in this age group. It has been shown that clonidine injected i.v. has a similar effect than when epidurally injected [73].
Ketamine is also used as an adjuvant for epidural block [74]. The pure preservative-free S(+) ketamine is preferable because it is less toxic for the nervous structures than the racemic mixture. However, some authors recommend avoiding the use of ketamine because of its potential toxicity [75, 76]. The usual dose injected caudally is 1 and 0.5 mg/kg-1 for the S(+) and racemic ketamine, respectively.
Opioids are often used as adjuvants for epidural block. After 6–9 months of age, adding opioids to LAs prolongs epidural analgesia for up to 24 h. Hydrophobic agents (fentanyl, sufentanil) must be placed at the metameric level where the pain will occur [77]. Preservative-free morphine easily spreads rostrally and can be placed at a lower metameric level. The bolus dose of morphine is 25–30 μg/kg-1 in the epidural space, which is followed by a continuous infusion of 1 μg/kg-1/h-1. When continuous epidural administration of fentanyl or sufentanil is combined with LAs, the doses are 0.2 and 0.1 μg/kg-1/h-1, respectively. Morphine 5–10 μg/kg-1 can be used as the sole agent for spinal analgesia during general anesthesia. In case of urinary retention, naloxone 1 μg/kg-1 or nalbuphine 0.1 mg/kg-1 can be injected as an i.v bolus. An i.v. bolus of naloxone 1–2 μg/kg-1 followed by a continuous infusion of 1–2 μg/kg-1/h-1 is usually efficacious in case of pruritus.
Notes
- 1.
Because compartmental pharmacokinetics are based on the assumption of linearity, concentration is described by a sum of exponentials with the assumption that absorption is faster than distribution and distribution is faster than elimination. If absorption is longer than elimination, it is not possible to distinguish between the phases. In other words, if absorption continues during elimination, the terminal phase appears falsely prolonged.
References
Lönnqvist PA (2012) Toxicity of local anesthetic drugs: a pediatric perspective. Paediatr Anaesth 22:39–43
Walker SM, Westin BD, Deumens R et al. (2010) Effects of Intrathecal Ketamine in the Neonatal Rat: Evaluation of Apoptosis and Long-term Functional Outcome. Anesthesiology 113:147159
Westin BD, Walker SM, Deumens R et al. (2010) Validation of a Preclinical Spinal Safety Model: Effects of Intrathecal Morphine in the Neonatal Rat. Anesthesiology 113:183–199
Walker SM, Grafe M, Yaksh TL (2012) Intrathecal clonidine in the neonatal rat: dose-dependent analgesia and evaluation of spinal apoptosis and toxicity. Anest Analg 2012; in press
Lonnqvist PA, Walker SM (2012) Ketamine as an adjunct to caudal blockade in neonates and infants: is it time to re-evaluate? Br J Anaesth 2012; in press
Lonnqvist PA, Ivani G, Moriarty T (2002) Use of caudal-epidural opioids in children: still state of the art or the beginning of the end? Paediatr Anaesth 12:747–749.
Lonnqvist PA (2012) Alpha-2 adrenoceptor agonists as adjuncts to Peripheral Nerve Blocks in Children-is there a mechanism of action and should we use them? Paediatr Anaesth 22:421–424
Lonnqvist PA(2005) Adjuncts to caudal block in children — Quo vadis? Br J Anaesth 95:431–433
References of the Review Article
Catterall WA (2002) Molecular mechanisms of gating and drug block of sodium channels. Novartis Found Symp 241:206–218
Mazoit JX, Dalens BJ (2004) Pharmacokinetics of local anaesthetics in infants and children. Clin Pharmacokinet 43:17–32
Nau C, Strichartz GR (2002) Drug chirality in anesthesia. Anesthesiology 97:497–502
Cartwright PD, Fyhr P (1988) The manufacture and storage of local anesthetics. Reg Anesth 13:1–12
Mazoit JX, Denson DD, Samii K (1988) Pharmacokinetics of bupivacaine following caudal anesthesia in infants. Anesthesiology 68:387–391
Mazoit JX, Denson DD, Samii K (1996) Pharmaisolated albumin and isolated alpha-1-acid glycoprotein. Differences between the two enantiomers are partly due to cooperativity. J Pharmacol Exp Ther 276:109–115
Meunier JF, Goujard E, Dubousset AM et al. (2001) Pharmacokinetics of bupivacaine after continuous epidural infusion in infants with and without biliary atresia. Anesthesiology 95:87–95
Sitbon P, Laffon M, Lesage V et al. (1997) Lidocaine plasma concentrations in pediatric patients after providing airway topical anesthesia from a calibrated device. Anesth Russell SC, Doyle E. A risk-benefit assessment of topical percutaneous local anaesthetics in children. Drug Saf 16:279–287
Taddio A, Ohlsson A, Einarson TR et al. (1998) A systematic review of lidocaine-prilocaine cream (EMLA) in the treatment of acute pain in neonates. Pediatrics 101:E1
Russell SC, Doyle E (1997) A risk-benefit assessment of topical percutaneous local anaesthetics in children. Drug Saf 16:279–287
Burm AGL (1989) Clinical pharmacokinetics of epidural and spinal anesthesia. Clin Pharmacokinet 16:283–311
Ecoffey C, Desparmet J, Berdeaux A et al. (1984) Pharmacokinetics of lidocaine in children following caudal anaesthesia. Br J Anaesth 56:1399–1402
Ecoffey C, Desparmet J, Berdeaux A et al. (2004) Bupivacaine in children: pharmacokinetics children under 2 years of age. Br J Anaesth 92:218–222
Chalkiadis GA, Eyres RL, Cranswick N et al. (2004) Pharmacokinetics of levobupivacaine 0.25% following caudal administration in children under 2 years of age. Br J Anaesth 92:218–222
Cortinez LI, Fuentes R, Solari S et al. (2008) Pharmacokinetics of levobupivacaine (2.5 mg/kg) after caudal administration in children younger than 3 years. Anesth Analg 107:11821184
Desparmet J, Meistelman C, Barre J et al. (1987) Continuous epidural infusion of bupiva- caine for postoperative pain relief in children. Anesthesiology 67:108–110
Lerman J, Nolan J, Eyres R et al. (2003) Efficacy, safety, and pharmacokinetics of levobupivacaine with and without fentanyl after continuous epidural infusion in children: a multicenter trial. Anesthesiology 99:1166–1174
Ala-Kokko TI, Partanen A, Karinen J et al. (2000) Pharmacokinetics of 0.2% ropivacaine and 0.2% bupivacaine following caudal blocks in children. Acta Anaesthesiol Scand 44:1099–1102
Lonnqvist PA, Westrin P, Larsson BA et al. (2000) Ropivacaine pharmacokinetics after caudal block in 1–8 year old children. Br J Anaesth 85:506–511
Emanuelsson BM, Persson J, Sandin S et al. (1997) Intraindividual and interindividual variability in the disposition of the local anesthetic ropivacaine in healthy subjects. Ther Drug Monit 19:126–131
Hansen TG, Ilett KF, Reid C et al. (2001) Caudal ropivacaine in infants: population phar- macokinetics and plasma concentrations. Anesthesiology 94:579–584
McCann ME, Sethna NF, Mazoit JX et al. (2001) The pharmacokinetics of epidural ropiva- caine in infants and young children. Anesth Analg 93:893–897
Bosenberg AT, Thomas J, Cronje L et al. (1998) Pharmacokinetics and efficacy of ropi- vavoxamine and ketoconazole as in vivo inhibitors. Clin Pharmacol Ther 64:484–491
Rapp HJ, Molnar V, Austin S et al. (2004) Ropivacaine in neonates and infants: a population pharmacokinetic evaluation following single caudal block. Pediatr Anesth 14:724–732
Berde CB, Yaster M, Meretoja O et al. (2008) Stable plasma concentrations of unbound ropi- vacaine during postoperative epidural infusion for 24–72 hours in children. Eur J Anaesthe- siol 25:410–417
Dalens B, Ecoffey C, Joly A et al. (2001) Pharmacokinetics and analgesic effect of ropivacaine following ilioinguinal/iliohypogastric nerve block in children. Paediatr Anaesth 11:415–420
Arlander E, Ekstrom G, Alm C et al. (1998) Metabolism of ropivacaine in humans is mediated by CYP1A2 and to a minor extent by CYP3A4: an interaction study with fluvoxamine and ketoconazole as in vivo inhibitors. Clin Pharmacol Ther 64:484–491
Gantenbein M, Attolini L, Bruguerolle B et al. (2000) Oxidative metabolism of bupivacaine into pipecolylxylidine in humans is mainly catalyzed by CYP3A. Drug Metab Dispos 28:383–385
Burm AG, van der Meer AD, van Kleef JW et al. (1994) Pharmacokinetics of the enantiomers of bupivacaine following intravenous administration of the racemate. Br J Clin Pharmacol 38:125–129
Burm AGL, Vermeulen NPE, Van Kleef JW et al. (1987) Pharmacokinetics of lidocaine and bupivacaine in surgical patients following epidural administration. Simultaneous investigation of absorption and disposition kinetics using stable isotopes. Clin Pharmacokinet 13:191–203
Burm AG, Stienstra R, Brouwer RP et al. (2000) Epidural infusion of ropivacaine for postoperative analgesia after major orthopedic surgery: pharmacokinetic evaluation. Anesthesi- ology 93:395–403
Scott DB, Lee A, Fagan D et al. (1989) Acute toxic ity of ropivacaine compared with that of bupivacaine. Anesth Analg 69:563–569
Knudsen K, Beckman Suurküla M, Blomberg S et al. (1997) Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth 78:507–514
Bardsley H, Gristwood R, Baker H et al. (1998) A comparison of the cardiovascular effects of levobupivacaine and rac-bupivacaine following intravenous administration to healthy volunteers. Br J Clin Pharmacol 46:245–249
Stewart J, Kellett N, Castro D (1995) The central nervous system and cardiovascular effects of levobupivacaine and ropivacaine in healthy tricular myocytes. Circulation 92:3014–3024
Maxwell LG, Martin LD, Yaster M (1994) Bupivacaine-induced cardiac toxicity in neonates:successful treatment with intravenous phenytoin. Anesthesiology 80:682–686
Hubler M, Gabler R, Ehm B et al. (2010) Successful resuscitation following opivacaine-in- duced systemic toxicity in a neonate. Anaesthesia 65:1137–1140
Longobardo M, Delpon E, Caballero R et al. (1998) Structural determinants of potency and stereoselective block of hKv1.5 channels induced by local anesthetics. Mol Pharmacol 54:162–169
Gonzalez T, Arias C, Caballero R et al. (2002) Effects of levobupivacaine, ropivacaine and bupivacaine on HERG channels: stereoselective bupivacaine block. Br J Pharmacol 137:1269–1279
Valenzuela C, Snyders DJ, Bennett PB et al. (1995) Stereoselective block of cardiac sodium channels by bupivacaine in guinea pig ventricular myocytes. Circulation 92:3014–3024
Komai H, Lokuta AJ (1999) Interaction of bupivacaine and tetracaine with the sarcoplasmic reticulum Ca2+ release channel of skeletal and cardiac muscles. Anesthesi- ology 90:835–843
Zapata-Sudo G, Trachez MM, Sudo RT et al. (2001) Is comparative cardiotoxicity of S()) and R(+) bupivacaine related to enantio- mer-selective inhibition of L-type Ca(2+) channels? Anesth Analg 92:496–501
Raymond SA, Thalhammer JG, Strichartz GR (1989) Axonal excitability: endogenous and exogenous modulation, in Dimitrijevic Ed Altered sensation and Pain. Recent Achievement in Restorative Neurology, Vol 3, Karger Basel 1990, cited by Raymond SA and Strichartz GR. The long and short of differential block (Editorial). Anesthesiology 70:725–728
Vabnick I, Novakovic SD, Levinson SR et al. (1996) The clustering of axonal sodium channels during development of the peripheral nervous system. J Neurosci 16:4914–4922
Rasband MN, Trimmer JS (2001) Developmental clustering of ion channels at and near the node of Ranvier. Dev Biol 236:5–16
Kohane DS, Sankar WN, Shubina M et al. (1998) Sciatic nerve blockade in infant, adolescent, and adult rats: a comparison of ropivacaine with bupivacaine. Anesthesiology 89:1199–1208
Greitz D, Hannerz J (1996) A proposed model of cerebrospinal fluid circulation: observations with radionuclide cisternography. AJNR Am J Neuroradiol 17:431–438
Wachi A, Kudo S, Sato K (1989) Characteristics of cerebrospinal fluid circulation in infants as detected with MR velocity imaging. Acta Anaesthesiol Scand 33:385–388
Booth D, Evans DJ (2004) Anticonvulsants for neonates with seizures. Cochrane Database Syst Rev 4:CD004218
de La Coussaye J, Brugada J, Allessie MA (1992) Electrophysiologic and arrhythmogenic- effects of bupivacaine. A study with high-resolution ventricular epicardial mapping in rabbit hearts. Anesthesiology 77:32–41
Mazoit JX, Decaux A, Bouaziz H et al. (2000) Comparative ventricular electrophysiologic effect of racemic bupivacaine, levobupivacaine, and ropivacaine on the isolated rabbit heart. Anesthesiology 93:784–792
Simon L, Kariya N, Edouard A et al. (2004) Effect of bupivacaine on the isolated rabbit heart: developmental aspect on ventricular conduction and contractility. Anesthesiology 101:937–944
Odoom JA, Sturk A, Dokter PWC et al. (1989) The effects of bupivacaine and pipecoloxy- lidide on platelet function in vitro. Acta Anaesthesiol Scand 33:385–388
Hollmann MW, Gross A, Jelacin N et al. (2001) Local anesthetic effects on priming and activation of human neutrophils. Anesthesiology 95:113–122
Beloeil H, Asehnoune K, Moine P et al. (2005) Bupivacaine’s action on the carrageenan induced inflammatory response in mice: cytokine production by leukocytes after ex-vivo stimulation. Anesth Analg 100:1081–1086
Leduc C, Gentili ME, Estèbe JP et al. (2002) Inhibition of peroxydation by local anesthetic in an inflammatory rat model with carrageenan. Anesth Analg 95:992–996
Rowbotham MC, Reisner-Keller LA, Fields HL (1991) Both intravenous lidocaine and morphine reduce the pain of postherpetic neuralgia. Neurology 41:1024–1028
Marret E, Rolin M, Beaussier M et al. (2008) Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg 95:1331–1338
Linchitz RM, Raheb JC (1999) Subcutaneous infusion of lidocaine provides effective pain relief for CRPS patients. Clin J Pain 15:67–72
Dadure C, Motais F, Ricard C et al. (2005) Con enantiomers on intracellular Ca2+ regulation in murine skeletal muscle fibers. Anesthesiology 102:793–798
Popitz-Bergez FA, Leeson S, Strichartz GR et al. (1995) Relation between functional deficit and intraneural local anesthetic during peripheral nerve block. A study in the rat sciatic nerve. Anesthesiology 83:583–592
Zink W, Missler G, Sinner B et al. (2005) Differential effects of bupivacaine and ropivacaine enantiomers on intracellular Ca2+ regulation in murine skeletal muscle fibers. Anesthesiology 102:793–798
Nouette-Gaulain K, Sirvent P, Canal-Raffin M et al. (2007) Effects of intermittent femoral nerve injections of bupivacaine, levobupivacaine, and ropivacaine on mitochondrial energy metabolism and intracellular calcium homeostasis in rat psoas muscle. Anesthesiology 106:1026–1034
Brown DL, Ransom DM, Hall JA et al. (1995) Regional anesthesia and local anesthetic induced systemic toxicity: seizure frequency and accompanying cardiovascular changes. Anesth Analg 81:321–328
Di Gregorio G, Neal JM, Rosenquist RW et al. (2010) Clinical presentation of local anesthetic systemic toxicity: a review of published cases, 1979 to 2009. Reg Anesth Pain Med 35:181–187
Weinberg GL (2010) Treatment of local anesthetic systemic toxicity (LAST). Reg Anesth Pain Med 35:188–193
Rosenblatt MA, Abel M, Fischer GW et al. (2006) Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest. Anesthesiology 105:217–218
Litz RJ, Popp M, Stehr SN et al. (2009) Successful lipid emulsions. Anesthesiology 110:380–386
Ludot H, Tharin JY, Belouadah M et al. (2008) Successful resuscitation after ropivacaine and lidocaine-induced ventricular arrhythmia following posterior lumbar plexus block in a child. Anesth Analg 106:1572–1574
Mazoit JX, Le Guen R, Beloeil H et al. (2009) Binding of long-lasting local anesthetics to lipid emulsions. Anesthesiology 110:380–386
Flandin-Bléty C, Barrier G (1995) Accidents following extradural analgesia in children. The results of a retrospective study. Paediatr Anaesth 5:41–46
Jamali S, Monin S, Begon C et al. (1994) Clonidine in pediatric caudal anesthesia. Anesth Analg 78:663–666
Hansen TG, Henneberg SW, Walther Larsen S et al. (2004) Caudal bupivacaine supplemented with caudal or intravenous clonidine in children undergoing hypospadias repair: a doubleblind study. Br J Anaesth 92:223–227
De Negri P, Ivani G, Visconti C et al. (2001) How to prolong postoperative analgesia after caudal anaesthesia with ropivacaine in children: S-ketamine versus clonidine. Paediatr Anaesth 11:679–683
Braun S, Gaza N, Werdehausen R et al. (2010) Ketamine induces apoptosis via the mitochondrial pathway in human lymphocytes and neuronal cells. Br J Anaesth 105:347–354
Eisenach JC, Yaksh TL (2003) Epidural ketamine in healthy children - what is the point? Anesth Analg 96:626
Lejus C, Surbled M, Schwoerer D et al. (2001) Postoperative epidural analgesia with bupi- vacaine and fentanyl: hourly pain assessment in 348 paediatric cases. Paediatr Anaesth 11:327–332
Luz G, Innerhofer I, Bachmann B et al. (1996) Bupivacaine plasma concentrations during continuous epidural anesthesia in infants and children. Anesth Analg 82:231–234
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Italia
About this chapter
Cite this chapter
Lönnqvist, PA. (2013). Drugs and Clinical Pharmacology of Central Blocks in Infants and Children. In: Astuto, M. (eds) Pediatric Anesthesia, Intensive Care and Pain: Standardization in Clinical Practice. Anesthesia, Intensive Care and Pain in Neonates and Children. Springer, Milano. https://doi.org/10.1007/978-88-470-2685-8_12
Download citation
DOI: https://doi.org/10.1007/978-88-470-2685-8_12
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2684-1
Online ISBN: 978-88-470-2685-8
eBook Packages: MedicineMedicine (R0)