Abstract
Breast reconstruction in previously irradiated patients is a difficult challenge for the surgeon owing to the lack of specific data for the use of less aggressive techniques such implant-based reconstruction in these cases. Flaps remain the primary option, although for some very well selected patients, implants can achieve satisfactory results with low rates of short-term and long-term complications. The purpose of this chapter is to establish an algorithm for breast reconstruction after recurrence of breast cancer in patients who have previously undergone breast-conserving surgery and radiotherapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Oncoplastic surgery
- Breast reconstruction
- Breast cancer
- Breast implants
- Latissimus dorsi
- Transverse rectus abdominis myocutaneous flap
- Radiotherapy
1 Introduction
Radiotherapy is an essential step in breast-conserving therapy (BCT) [1]. Unfortunately, it is also a significant additional risk for any technique of reconstruction when there is a true local recurrence or a second tumor in the same breast, and the patient is eligible for mastectomy. After BCT, the use of implants is controversial because of the damaging effects of radiotherapy on soft tissues. A large risk of implant loss, high rates of wound complications, and capsular contracture when radiotherapy accompanies breast reconstruction have been reported in previous series. Today, the use of implants remains a relative contraindication when there has been previous breast irradiation.
Despite being related to a decrease in the mortality and local recurrence rates in breast cancer patients, chronic radiotherapy can cause endarteritis, which leads to a less vascularized bed. It is potentially damaging if further intervention is necessary because ischemia alters the local resistance to infection. Furthermore, the reduced lymphatic drainage, resulting from actinic lymphangitis, favors the accumulation of fluids. Finally, many patients develop a certain degree of breast fibrosis a few months after the end of radiotherapy, which impedes the expansion of the tissue with temporary or definitive expanders. Because of these factors, autologous flaps are generally indicated for previously irradiated breast cancer patients.
The purpose of this chapter is to establish an algorithm for breast reconstruction after recurrence of breast cancer in patients who have previously undergone BCT and radiotherapy.
2 Implants
A high percentage of capsular contractures and postoperative complications in reconstruction with implants when adjuvant radiotherapy is used have been reported. Owing to a more intensive inflammatory response, there are reports of pain, distortion, and capsular contracture in approximately 30 % of patients during long-term follow-up. There are also reports of implant displacement, implant exposure, poor aesthetic outcomes, and high rates of implant removal [2–13]. In a study done in Switzerland among 107 patients who underwent mastectomy with immediate breast reconstruction, followed for a minimum period of 2 years, 20.6 % developed capsular contracture. This rate was significantly higher for irradiated breasts (41.7 %) than for nonirradiated breasts (14.5 %) (p = 0.01). In another reported series of 77 patients who underwent two-stage tissue expander and implant reconstruction, 55 patients (71 %) received adjuvant radiotherapy. Eight patients with an ipsilateral recurrence had been previously irradiated at the time of the conservative treatment and the remaining ones were irradiated for the first time after placement of the expander. The complications appeared to be related to radiotherapy (14 % in the nonirradiated patients and 51 % in the irradiated ones; p = 0.006). Complications occurred in five of the eight previously irradiated patients (62.5 %) and in 23 of the 47 patients irradiated after reconstruction (49 %). All of the most serious complications (class 3) were found in patients who received radiotherapy. It was suggested by the authors that there is need for more studies regarding immediate breast reconstruction in previously irradiated patients in order to establish selection criteria before this option is undertaken [10].
For 15 years, Benacci [11] followed 57 patients who underwent salvage mastectomy for local breast cancer recurrence. Nine patients in this group underwent breast reconstruction with a tissue expander/implant, involving placement of ten prostheses. Of those three patients, six had significant complications, including inability to fully expand the tissue expander secondary to a tight overlying skin envelope in two of them (20 %), wound infection requiring implant removal in one patient (10 %), significant capsular contracture (Baker 3) in 20 % of the patients, and tissue expander extrusion in one patient. Four reconstructions required an unplanned surgical revision (expander replacement, implant exchange, and capsulectomy). In this select group of patients who underwent salvage mastectomy and afterwards two-stage surgery, 60 % of attempted reconstructions resulted in either a significant complication or unfavorable aesthetic outcomes.
More recently this paradigm—to not use implants when radiotherapy has been used or is planned—was challenged by reports of good to excellent results in breast reconstruction despite the previous use of radiotherapy or its application after reconstruction [5, 13]. However, as long as some authors describe favorable experiences of reconstruction after radiotherapy, others are still opposed to that procedure.
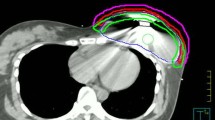
In a previous unpublished series from the Breast Unit of Hospital Nossa Senhora das Graças in Curitiba (Brazil), three cases were reported of one-stage breast reconstruction in patients who had previously undergone a quadrantectomy followed by radiotherapy and had local recurrence. All of them underwent skin-sparing mastectomy followed by one-stage immediate breast reconstruction with anatomic profile implants. After an average follow-up of 16 months, no evidence of capsular contracture was noticed, the aesthetic results were stable, and the patients did not have early or late complications. The authors suggest that the success in these patients could be due to the association of a selection of the patients with no breast fibrosis after radiotherapy and the use of anatomic implants smaller than the original size of the irradiated breast. Immediate breast reconstruction with implants in this well-selected group of patients needs to be tested in a large series in order to confirm these preliminary results [12] (Fig. 42.1).
3 Flaps
The description in 1977 of the latissimus dorsi (LD) musculocutaneous flap for breast reconstruction introduced another important option for autologous tissue reconstruction in patients after mastectomy [14]. Until the description of the transverse rectus abdominis muscle (TRAM) flap in 1982 [15], use of autologous tissue for reconstructions was closely linked with breast implants. The TRAM flap provided a relatively easy technique for acquiring ample tissue for shaping and skin coverage in most reconstructions. When a large amount of skin replacement is required, it is the preferred technique.
Complications in previously irradiated patients ranged from a mastectomy defect with minimal radiation changes to frank skin necrosis. Coverage is the primary purpose for the latter group, and the reconstructive operation becomes an aesthetic procedure in the former. For the reconstructive surgeon, there are two major areas of concern after radiotherapy:
-
1.
The recipient bed
-
2.
The flap’s vascular pedicle
Breast reconstruction with a TRAM flap after radiotherapy is reasonable and should remain the first choice for most patients, although multivariable logistic regression analysis showed both obesity and prior radiotherapy to be associated with an increased risk of fat necrosis [16].
The bipedicled flap should be used when possible to allow there to be sufficient tissue for reconstruction after resection of the irradiated recipient site and provide improved blood supply to a vascular impoverished recipient bed [16]. However, using a bipedicled flap in the irradiated patient does not prevent the occurrence of fat necrosis. The rate of fat necrosis suggests some compromised blood flow to the subcutaneous fat, possibly from partial obstruction of the internal mammary artery.
The largest review of irradiated patients undergoing TRAM flap reconstructions supports previous histologic studies that large vessel damage from radiation is rare and not prohibitive for using pedicles for flaps [16]. Moreover, Kroll et al. [17], using four independent observers, compared 82 patients with a history of previous chest-wall irradiation with 202 nonirradiated patients in order to determine whether prior irradiation was associated with more frequent complications. Both groups underwent LD and TRAM flap breast reconstruction. The complication rate in the irradiated group was 39 versus 25 % in the nonirradiated group (p = 0.03). In the irradiated group, complications were more frequent with the LD flap (63 %) than with the TRAM flap (33 %; p = 0.063), but this was not statistically significant.
Although only irradiated groups were evaluated, Schuster et al. [18] in a study with patient questionnaires found higher satisfaction rates with TRAM flap reconstructions than with LD flaps or implants in previously irradiated patients (Fig. 42.2).
Preoperative (a–c) and postoperative (d–g) views of a 59-year-old patient with an extensive local recurrence after breast-conserving therapy 4 years earlier in the left breast. d–g Twelve months after one-stage breast reconstruction with a bipedicled transverse rectus abdominis myocutaneous flap and contralateral breast reduction for symmetry
4 Effects of Radiation on the Decision for Immediate Breast Reconstruction
Issues concerning breast reconstruction in patients who have had or may potentially require radiotherapy include:
-
Effect of radiotherapy on soft tissues
-
Timing of irradiation in the patient presenting with breast cancer
-
Choice of a breast reconstruction option that will produce the optimal long-term cosmetic outcome.
The effects of radiation on wound healing are extensive and well known, although the specific causes remain a matter of speculation. Early response is characterized by dry or moist desquamation, dependent on the response of the host to the dose. The chronic phase is characterized by fibrosis, loss of elasticity, and in some circumstances a susceptibility to breakdown and ulceration [19].
An analysis of 277 consecutive LD breast reconstructions performed in 243 patients was published recently [20], with one-third of the reconstructions being immediate reconstructions. The mean age at reconstruction was 50.4 years. The mean follow-up was 47 months, and 3.6 % of patients developed Baker grade III capsular contracture requiring capsulotomy. Chemotherapy provided a protective effect (p = 0.0197) against capsular contracture formation. Previous radiotherapy had no significant influence on symptomatic capsule formation. Therefore, the conclusion was that use of textured, cohesive-gel silicone implants, combined with a standardized surgical approach, could reduce complications in the short-term and the long-term postoperative period, independent of radiotherapy.
On the other hand, Garusi et al. [21] evaluated the use of LD breast reconstruction after radiotherapy. They performed 63 LD flap with implant reconstructions between 2001 and 2007. All of them were performed in breast cancer recurrence cases after BCT and then total mastectomy. Baker grade III capsular contraction was observed in two cases (3.1 %). The rest were grade I or grade II and there were no grade IV contractures. They proposed that LD flap with implant reconstructions can be performed in irradiated breasts with a low capsular contracture rate.
The same European Institute of Oncology group [22] performed an interesting study addressing whether there is any difference in the evaluation of cosmesis according to the gender and specialization of the observer. Fifty-two photographs of patients who had undergone TRAM flap reconstruction for breast cancer were divided into three groups according to treatment (TRAM flap reconstruction alone, TRAM flap reconstruction and then radiotherapy, radiotherapy and then TRAM flap reconstruction), and were evaluated by 21 specialists, ten male and 11 female from different areas: radiotherapy, breast surgery, and plastic and reconstructive surgery. A significantly worse score was registered in the group who underwent TRAM flap reconstruction and then radiotherapy compared with the other groups.
In the last few years at the Department of Mastology and Breast Reconstruction of the Hospital de Cancer de Barretos, 45 autologous flap reconstructions were performed with or without radiotherapy. The LD flap was indicated in 29 cases, 10 % of them before radiotherapy, aiming to reshape large quandrantectomies. The comparison between the patients reconstructed before and after radiotherapy revealed unsatisfactory results in 66 % for the first group. TRAM flap reconstruction was performed in 16 patients. Poor results with flaps and implants occurred in 26.66 % of cases, the rate of capsular contracture being 52.2 % in irradiated patients versus 16 % in nonirradiated ones.
Regarding flap reconstruction, the quality of the skin at the recipient bed is important in the final decision and this must be explained to the patient. One suggestion is to avoid flap reconstruction before radiotherapy because of progressive loss of aesthetic results related to fibrosis. Complications after TRAM flap and LD flap reconstructions were more frequent in previously irradiated than in nonirradiated patients, probably because of radiation-induced damage to chest-wall skin. These differences are not enough to suggest that previous irradiation is a contraindication to breast reconstruction, but it is necessary to consider flap reconstruction as the first choice in most cases.
A recent meta-analysis selected 11 studies and a total of 1,105 patients and examined postoperative morbidity following immediate or delayed breast reconstruction combined with radiotherapy [23]. Use of autologous flaps resulted in less morbidity than implant-based reconstruction. Although the specific case of previous radiotherapy in BCT was not addressed, comparison of immediate versus delayed reconstruction with use of autologous flaps in irradiated patients after mastectomy did not produce statistically significant morbidity differences.
Cordeiro et al. [24], from Memorial Sloan-Kettering Cancer Center, in a timely article, retrospectively described their experience with immediate two-stage implant-based reconstruction in 121 patients who had previously undergone radiotherapy. They compared complications, aesthetic outcomes, and patient satisfaction with those for 1,578 patients who had undergone the same surgery but had not undergone radiotherapy. They reported a significantly higher incidence of postoperative early (29 vs. 15 %; p ≤ 0.001) and late complications in the irradiated group and a poorer aesthetic outcome. The most frequent early complication in both groups was mastectomy flap necrosis (18 vs. 7.7 %; p < 0.01). However, they concluded that with careful selection of the patients, implant-based breast reconstruction is acceptable, with a slightly higher incidence of grade III and grade IV capsular contracture (10.6 vs. 6.3 %; p = 0.2), and despite a higher incidence of postoperative complications. Patient satisfaction did not differ between the two groups, and most of the irradiated patients had good or very good results, whereas most of the nonirradiated patients had excellent results (p = 0.04).
A decision flowchart used in the Breast Unit of Hospital Nossa Senhora das Graças for this group of previously irradiated patients is shown in Fig. 42.3.
5 Conclusions
Breast reconstruction in previously irradiated patients is a difficult challenge for the surgeon owing to the lack of specific data for the use of less aggressive techniques in these cases. Flaps remain the primary option, although for some very well selected patients, implants can achieve satisfactory results with low rates of short-term and long-term complications.
References
Early Breast Cancer Trialists’ Collaborative Group (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomized trials. Lancet 366:2087–2106
Thaylor CW, Horgan T, Dodwell D (2005) Oncological aspects of breast reconstruction. The Breast 14:118–130
Evans GR, Schusterman MA, Kroll SS et al (1995) Reconstruction and the radiated breast: is there a role for implants? Plast Reconstr Surg 96(5):1111–1115
Warren AG, Morris DJ, Houlihan MJ, Slavin SA (2008) Breast reconstruction in a changing breast cancer treatment paradigm. Plast Reconstr Surg 121:1116–1126
Perec I, Bucky LP (2008) Successful prosthetic breast reconstruction after radiation therapy. Ann Plastic Surg 60:527–531
Pittet B, Montandon D, Pittet D (2005) Infection in breast implants. Lancet Infect Dis 5(2):94–106
Behranwala KA, Dua RS, Ross GM, Ward A, A’Hern R (2006) The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconst Aesthetic Surg 59:1043–1051
Ascherman JA, Hanasono MM, Newman MI, Hughes DB (2006) Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconst Surg 117:359–365
Benediktson K, Perbeck L (2006) Capsular contracture around saline-filled and textured subcutaneously-placed implants in irradiated and non-irradiated breast cancer patients: five years of monitoring of a prospective trial. Brit J Plast Surg 59:27–34
Tallet AV, Salem N, Moutardier V, Ananian P, Braud A, Zalta R, Cowen D, Houvenaeghel G (2003) Radiotherapy and immediate two-stage breast reconstruction with a tissue expander and implant: complications and esthetic results. Int J Radiation Oncol Biol Phys 57:136–142
Benacci JC (2002) Implant breast reconstruction in the irradiated cancer patient. Curr Surg 59:21–27
Urban CA, Blaszkowski DS, Lima e Silva J et al. One-stage breast reconstruction with implants in previously irradiated patients. Revista Brasileira de Mastologia (in press)
McCormick B, Wright J, Cordeiro P (2008) Breast reconstruction combinated with radiation therapy: long-term risks and factors related to decision making. Cancer J 14:264–268
Schneider WJ, Hill HL Jr, Brown RG (1977) Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg 30:277–281
Scheflan M, Hartrampf CR, Black PW (1982) Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg 69:908–909
Williams JK, Bostwick J 3rd, Bried JT, Mackay G, Landry J, Benton J (1995) TRAM flap breast reconstruction after radiation treatment. Ann Surg 221:756–764; discussion 64–66
Kroll SS, Schusterman MA, Reece GP, Miller MJ, Smith B (1994) Breast reconstruction with myocutaneous flaps in previously irradiated patients. Plast Reconstr Surg 93:460–469; discussion 70–71
Schuster RH, Kuske RR, Young VL, Fineberg B (1992) Breast reconstruction in women treated with radiation therapy for breast cancer: cosmesis, complications, and tumor control. Plast Reconstr Surg 90:445–452; discussion 53–54
Schuster RH (1993) Breast reconstruction in women treated with radiation therapy for breast cancer. Plast Reconstr Surg 91:967
Hardwicke JT, Prinsloo DJ (2011) An analysis of 277 consecutive latissimus dorsi breast reconstructions: a focus on capsular contracture. Plast Reconstr Surg 128:63–70
Garusi C, Lohsiriwat V, Brenelli F et al (2011) The value of latissimus dorsi flap with implant reconstruction for total mastectomy after conservative breast cancer surgery recurrence. Breast 20:141–144
Leonardi MC, Garusi C, Santoro L et al (2010) Impact of medical discipline and observer gender on cosmetic outcome evaluation in breast reconstruction using transverse rectus abdominis myocutaneous (TRAM) flap and radiotherapy. J Plast Reconstr Aesthet Surg 63:2091–2097
Barry M, Kell MR (2011) Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat 127:15–22
Cordeiro PG, Snell L, Heerdt A, McCarthy C (2012) Immediate tissue expander/implant breast reconstruction after salvage mastectomy for cancer recurrence following lumpectomy/irradiation. Plast Rec Surg 129:341–349
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Italia
About this chapter
Cite this chapter
Urban, C., Zucca-Matthes, A.G., Vieira, R., Rietjens, M. (2013). Immediate Breast Reconstruction in Previously Irradiated Patients. In: Urban, C., Rietjens, M. (eds) Oncoplastic and Reconstructive Breast Surgery. Springer, Milano. https://doi.org/10.1007/978-88-470-2652-0_42
Download citation
DOI: https://doi.org/10.1007/978-88-470-2652-0_42
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2651-3
Online ISBN: 978-88-470-2652-0
eBook Packages: MedicineMedicine (R0)