Abstract
The optimum sequencing of breast reconstruction (BR) in patients receiving postmastectomy radiation therapy (PMRT) is controversial. A comprehensive search of published studies that examined postoperative morbidity following immediate or delayed BR with combined radiotherapy was performed. Medical (MEDLINE & EMBASE) databases were searched and cross-referenced for appropriate studies where morbidity following BR was the primary outcome measured. A total of 1,105 patients were identified from 11 appropriately selected studies. Patients undergoing PMRT and BR are more likely to suffer morbidity compared with patients not receiving PMRT (OR = 4.2; 95% CI, 2.4–7.2 [no PMRT vs. PMRT]). Reconstruction technique was also examined with outcome when PMRT was delivered after BR, and this demonstrated that autologous reconstruction is associated with less morbidity in this setting (OR = 0.21; 95% CI, 0.1–0.4 [autologous vs. implant-based]). Delaying BR until after PMRT had no significant effect on outcome (OR = 0.87; 95% CI, 0.47–1.62 [delayed vs. immediate]). PMRT has a detrimental effect on BR outcome. These results suggest that where immediate reconstruction is undertaken with the necessity of PMRT, an autologous flap results in less morbidity when compared with implant-based reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast conservation surgery provides excellent loco-regional control with improved quality of life when compared with mastectomy [1]. However, many patients still require mastectomy as the optimum therapeutic cancer procedure, and many opt to undergo immediate breast reconstruction [2]. It is therefore essential that an appropriate strategy be proposed regarding the timing of reconstruction and postoperative radiotherapy. The enthusiasm for post-mastectomy breast reconstruction aims to achieve good functional aesthetic outcome and maintain their quality of life, without negatively affecting the prognosis or detection of cancer recurrence [3].
The Danish Breast Cancer Cooperative Group, 82b and 82c, trials in conjunction with findings from the Canadian trial collectively demonstrate that patients randomised to receive post-mastectomy radiation have a lower 10-year rate of local regional recurrence and an additional survival advantage associated with post-mastectomy radiotherapy [4, 5]. Based on these, and similar studies, clear guidelines are available regarding the indications for post-mastectomy radiation which are large tumour size, direct involvement of the skin, and four or more metastatic axillary lymph nodes [6–8]. However, despite reducing loco-regional recurrences and increasing disease-free survival [9], post-mastectomy radiotherapy may negatively affect reconstruction outcome.
As a consequence, several studies demonstrated that immediate breast reconstructions in irradiated patients are associated with the potential for significant postoperative morbidity [10, 11]. As a result, breast reconstruction may be delayed until the final pathological results are available from the mastectomy specimen and the indication for radiotherapy can be established.
Immediate breast reconstruction without radiotherapy, offers enhanced aesthetic and safe oncological outcomes, is more cost-effective and provides a positive psychological effect [12–16]. Despite this, less than 20% of patients having a mastectomy have immediate breast reconstruction in the United States [2]. This may be because of patient choice or possibly apprehension on the part of the surgeon that radiotherapy maybe required postoperatively which potentially could compromise the reconstruction. Radiotherapy can cause unpredictable changes in all tissues and prosthetic materials [17]. It has a biphasic nature with the acute effects occurring over days to weeks and a delayed response, which can occur from months to years after completion of the therapy [18]. The acute phase usually involves acute inflammatory changes taht may lead to desquamation or even necrosis of tissue [19]. The delayed phase involves atrophy, fibrosis and inhibition of normal wound-healing mechanisms [19]. Furthermore, opponents of immediate breast reconstruction suggest it may alter chest wall anatomy and therefore distort the geometrics of the radiation field design leading to under/overdosing the targeted and underlying tissues [20, 21]. However, Strålman et al. demonstrated a loco-regional recurrence rate of 6% in 100 patients who had a mastectomy with immediate (implant/autologous) reconstruction followed by radiotherapy with a mean follow up of 108 ± 26 months. This suggests that there is no significant decrease in efficacy or delivery of radiation post-immediate implant or autologous reconstruction [22]. Furthermore, Huang et al. compared the incidence of local recurrence and distant metastasis of post-mastectomy radiotherapy for breast cancer patients with and without immediate TRAM flap reconstruction. They reported no statistical differences in the incidences of loco-regional recurrence or distant metastasis between the TRAM flap and the non-TRAM flap patients [23].
Therefore, the objective of this meta-analysis is to examine the published evidence whether patients requiring post-mastectomy radiotherapy should have an immediate or delayed reconstruction and whether a prosthesis or autologous reconstruction is associated with the optimum outcome in terms of postoperative morbidity.
Methods
Identification of studies
MEDLINE and EMBASE were searched by entering the following in the searching algorithm: breast reconstruction AND surgery OR radiation AND (clinical trial OR randomized controlled trial OR double-blind OR single-blind OR random OR randomized OR placebo OR retrospective study OR prospective study). English was set as a language restriction. The latest search was performed on 1st January 2010. Two authors (M. Barry and M.R. Kell) independently examined the title and abstract of citations, the full texts of potentially eligible trials were obtained and disagreements were resolved by discussion.
Eligibility criteria
All trials, whether randomized or non-randomized prospective or retrospective, that examined the effects of radiotherapy on immediate or delayed breast reconstruction using either a prosthesis or autologous tissue were eligible (latissimus dorsi—LD or trasversus rectus abdominis muscle—TRAM). Case series or reports were not included. Studies where the data could not be accurately extracted were also excluded.
Data extraction and outcomes
The following information regarding each eligible trial was recorded: authors’ names, journal, patient numbers, timing and method of reconstruction, addition of radiotherapy and the postoperative complication rate. The primary end point of this meta-analysis was postoperative morbidity, including capsular contracture, fibrosis, fat necrosis and surgical site infections requiring removal of prosthesis/re-operation (see Tables 1, 2, 3 and 4).
Statistical analysis
For postoperative complications in each study, the odds ratio (OR) of the simple proportions of events was estimated with its variance and 95% CI. Heterogeneity between the ORs for the same outcome between studies was assessed using the χ2-based Q statistic [24]. Data were then combined across studies by the use of general variance methods with fixed and random effects models [14]. Analyses were conducted using StatsDirect version 2.5.6 (StatsDirect Ltd, Chesire, United Kingdom) and SPSS version 12.0 (SPSS, Inc, Chicago, IL). All statistical tests were two-tailed.
Results
Eligible studies
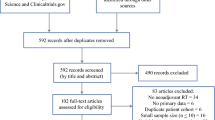
About 20 potentially eligible studies were identified that examined the effects of radiotherapy on immediate or delayed breast reconstructions. Because of low numbers (e.g. n < 15) or incomplete data set regarding postoperative morbidity, 9 studies were excluded from the meta-analysis. Of the 11 studies selected, 4 studies examined the effects of RT on immediate BR using implant or expanders and 4 studies examined the effects of RT on immediate BR using either a prosthesis or autologous flap. Finally, 3 remaining studies evaluated the effects of RT on immediate versus delayed autologous BR (see Fig. 1).
A total of 1,105 patients were identified from 11 selected studies [10, 11, 15, 22, 25–31]. These were subsequently divided into three cohorts for subgroup analyses. The first group (n = 424) were patients with immediate BR using a prosthesis alone with/without RT. The second subgroup (n = 380) compared patients with immediate autologous BR versus prosthesis alone in the presence of RT. The last subgroup analysis (n = 301) compared the effects of RT on immediate versus delayed autologous BR.
Postoperative complications in BR in the presence of RT
Patients undergoing PMRT and immediate BR (n = 196) are more likely to suffer morbidity when compared to patients not receiving PMRT (n = 229) (OR = 4.2; 95% CI: 2.4–7.2 [no PMRT vs. PMRT]; see Fig. 2). Finally, reconstruction technique was examined when PMRT was delivered after BR and this demonstrated that autologous reconstruction is the superior reconstruction technique in terms of postoperative morbidity (OR = 0.20; 95% CI: 0.1–0.4 [autologous vs. implant-based]; see Fig. 3). Postoperative morbidity was defined in terms of capsular contracture, infection, fat necrosis, fibrosis and the necessity to re-operate on the patient. The rates of these complications are displayed in Tables 1, 2 and 4. Interestingly, the effect of delaying BR until after PMRT had no significant effect on outcome (OR = 0.87; 95% CI: 0.47–1.62 [delayed vs. immediate]; see Fig. 4).
Discussion
It is evident from the results that an immediate BR using a prosthesis only in the presence of RT is associated with an increased risk of postoperative complications (OR = 4.2; 95% CI: 2.4–7.2 [no PMRT vs. PMRT]). This is supported by the study of Aschermann et al. [32] who conducted a retrospective review of 104 patients (123 breasts) underwent mastectomy followed by implant breast reconstruction. They demonstrated that complications requiring prosthetic device removal or replacement, as well as total complications, were more frequent in breasts that received radiation than breasts that did not (18.5% vs. 4.2% for complications requiring prosthetic removal or replacement, P ≤ 0.025, and 40.7% vs. 16.7% for total complications, P ≤ 0.01) [32]. On analysis of Tables 1 and 5, it is apparent that patients with immediate implant-based reconstructions receiving radiotherapy have significantly greater incidences of complications compared to those who did not receive radiotherapy.
Immediate breast reconstruction following a skin-sparing mastectomy has a number of advantages over the delayed reconstruction. First, it provides a more enhanced aesthetic result because of preservation of the infra-mammary fold, allowing a more natural appearance and there is also the option to adjust the position of the scar [14]. More importantly, for the patient, it provides enormous psychosocial benefits by restoring femininity and improving vitality, sexuality and quality of life [14]. In the absence of implants, immediate breast reconstruction has a very favourable morbidity profile even when exposed to adjuvant radiotherapy [23]. Moreover, it is oncologically safe with an acceptable local recurrence rate [23]. Despite this, advocates of delayed breast reconstruction suggest that there are two main problems with immediate breast reconstruction in the presence of radiotherapy. First, radiation therapy can adversely affect the cosmetic outcome and cause increased postoperative complications [33]. Second, immediate breast reconstruction can impair the efficacy and delivery of radiotherapy [33]. Autologous reconstructions have a more predictable response than implants to radiotherapy; however, the exact sequencing of this therapy is contentious. Kronowitz et al. [34] suggested the concept of the delayed-immediate breast reconstruction as a potential solution. This involves placing a tissue expander at the time of a skin-sparing mastectomy and waiting for the final pathological results of the specimen. If radiotherapy is not required, an immediate reconstruction is proposed and if radiotherapy is required, a delayed reconstruction is advised. Unfortunately, this requires two operations that are associated with significant psychological and cost implications.
McKeown et al. [35] demonstrated that patient satisfaction with cosmetic outcome was similar between patients undergoing immediate and delayed reconstruction (autologous LD) plus radiotherapy. Interestingly, they also noted that most patients in retrospect preferred an immediate reconstruction [35]. In a prospective study by Thomson et al. [12] that assessed 73 women post-immediate implant–assisted LD or autologous LD reconstruction with or without radiotherapy, there was no difference between the groups in terms of overall cosmetic outcome as determined by the patients. When a panel of independent cosmetic assessors reviewed the photographic evidence at different intervals over a defined time period, they concluded that although radiotherapy had an adverse effect on aesthetic outcome (P = 0.0002), this was more obvious in the implant-assisted LD group [12].
Kroll and colleagues [36] reviewed 1,384 free-flap procedures performed for reconstruction of the breast or of head and neck defects. They assessed the effects of prior irradiation of the recipient site on the incidence of total flap loss which were more common in flaps transferred to previously irradiated sites [36]. It is evident from this study (Tables 4 and 6) that exposure of an autologous flap to radiotherapy increases the postoperative complication rates irrespective of whether an immediate or delayed reconstruction is performed (30.1% vs. 32.1%, respectively).
The potential limitations of this study are that patient selection criteria for either prosthetic-based or autologous BR were poorly defined and may have differed between centres and time periods. There was also variation in the RT treatments used in terms of both dose and use of a boost. It is possible that the incidence of postoperative BR complication rates varies with the dose of RT used and this could not be assessed in our analysis.
Finally, in addition to selecting the appropriate timing of radiotherapy and reconstruction, appropriate patient selection is also paramount to consistently obtain successful outcomes. A BMI of less than 30 is associated with a better outcome in all reconstructive surgical procedures [37]. A history of smoking and diabetes is also poor prognostic indicators for myocutaneous flap viability [38]. Patient selection for reconstruction was not stated in many of the studies involved in this meta-analysis and therefore could not be included.
Conclusion
Post-mastectomy radiation, irrespective of the method of reconstruction, increases the incidence of postoperative complications; however, this study has demonstrated that in this setting, an autologous flap offers a more favourable outcome in terms of morbidity than expander/implant reconstruction. There is a paucity of high-quality conclusive data regarding the correct sequencing of breast reconstruction and radiotherapy. The majority of studies involve small numbers of patients in single centres with retrospective analysis. Multicenter randomised controlled trials with longer follow-up times and better specified parameters are necessary to validate any future strategies regarding the optimum timing of radiotherapy and breast reconstruction. Unfortunately, these studies are difficult to perform, as it is difficult to ethically justify demanding that patients undergo an immediate versus a delayed reconstructive procedure because of a randomisation process. Therefore, in the absence of level-I evidence, the current data suggest that immediate breast reconstruction with PMRT may be undertaken though morbidity is higher with either immediate or delayed technique. The timing and effect of radiotherapy on breast reconstruction must be discussed to ensure informed opinion and consent of the patient. The patients’ expectations, preferences, motivations and their level of understanding should be explored to enhance postoperative satisfaction and quality of life [39].
References
Fisher B, Anderson S, Bryant J et al (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Eng J Med 347:1233–1241
Chevray PM (2008) Timing of breast reconstruction: immediate versus delayed. Cancer J 14(4):223–229
Meretoja TJ, von Smitten KA, Leidenius MH, Svarvar C, Heikkila PS, Jahkola TA (2007) Local recurrence of stage 1 and 2 breast cancer after skin sparing mastectomy and immediate breast reconstruction in a 15 year series. Eur J Surg Oncol 33:1142–1145
Overgaard M, Hansen PS, Overgaard J et al (1997) Postoperative radiotherapy in high risk premenopausal women with breast cancer who receive adjuvant chemotherapy. N Engl J Med 337:949–955
Ragaz K, Jackson SM, Le N et al (1997) Adjuvant radiotherapy and chemotherapy in node positive premenopausal women with breast cancer. N Engl J Med 337:956–962
Recht A, Edge SB, Solin LJ et al (2001) Postmastectomy radiotherapy: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol 19:1539–1569
Harris JR, Halpin-Murphy P, McNeese M et al (1999) Consensus statement on postmastectomy radiation therapy. Int J Radiat Oncol Biol Phys 44:989–990
Rutqvist LE, Rose C, Cavallin-Ståhl E (2003) A systematic overview of radiation therapy effects in breast cancer. Acta Oncol 42(5–6):532–545
Truong PT, Woodward WA, Bucholz TA (2006) Optimizing locoregional control and survival for women with breast cancer: a review of current developments in postmastectomy radiation. Expert Rev Anticancer Ther 6:205–216
Wong JS, Ho AY, Kaelin CM, Bishop KL, Silver B, Gelman R, Harris JR, Hergrueter CA (2008) Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J 14(1):49–54
Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM (2004) Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys 59(4):1080–1087
Thomson HJ, Potter S, Greenwood RJ, Bahl A, Barker J, Cawthorn SJ, Winters ZE (2008) A prospective longitudinal study of cosmetic outcome in immediate latissimus dorsi breast reconstruction and the influence of radiotherapy. Ann Surg Oncol 15(4):1081–1091 Epub 26 Jan 2008
Miller MJ, Rock CS, Robb GL (1996) Aesthetic breast reconstruction using a combination of free transverse rectus abdominis musculocutaneous flaps and breast implants. Ann Plast Surg 37(3):258–264
Kroll SS, Marchi M (1991) Immediate reconstruction: current status in cancer management. Tex Med 87:67–72
Spear SL, Ducic I, Low M, Cuoco F (2005) The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg 115(1):84–95
Dean C, Chetty U, Forrest AP (1983) Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet 1:459–462
Bloomer WD, Hellman S (1975) Normal issue responses to radiation therapy. N Engl J Med 293:80–83
Fajardo LF, Berthrong M (1978) Radiation injury in surgical pathology: part I. Am J Surg Pathol 2:159–199
Fajardo LF (1989) Morphologic patterns of radiation injury. Front Radiat Ther Oncol 23:75–84
Kronowitz SJ, Robb GL (2004) Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg 114(4):950–960
Buchholz TA, Kronowitz SJ, Kuerer HM (2002) Immediate breast reconstruction after skin-sparing mastectomy for treatment of advanced breast cancer: radiation oncology considerations. Ann Surg Oncol 9:820–821
Strålman K, Mollerup CL, Kristoffersen US, Elberg JJ (2008) Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol 47(4):704–708
Huang CJ, Hou MF, Lin SD et al (2006) Comparison of local recurrence and distant metastases between breast cancer patients after postmastectomy radiotherapy with and without immediate TRAM flap reconstruction. Plast Reconstr Surg 118(5):1079–1086
Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127:820–826
Tallet AV, Salem N, Moutardier V et al (2003) Radiotherapy and immediate two stage breast reconstruction with a tissue expander and implant: complications and aesthetic results. Int J Radiat Oncol Biol Phys 57(1):136–142
Krueger EA, Wilkins EG, Strawderman M et al (2001) Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 49(3):713–721
Cordeiro PG, Pusic AL, Disa JJ et al (2004) Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 113(3):877–881
Whitfield GA, Horan G, Irwin MS et al (2009) Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 Gray in 15 fractions. Radiother Oncol 90:141–147
Jhaveri JD, Rush SC, Kostroff K, Derisi D, Farber LA, Maurer VE, Bosworth JL (2008) Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys 72(3):859–865
Williams JK, Carlson GW, Bostwick J 3rd, Bried JT, Trimble J, Mackay G (1997) The effects of radiation treatment after TRAM flap breast reconstruction. Plast Reconstr Surg 100(5):1153–1160
Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL (2001) Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 108(1):78–82
Ascherman JA, Hanasono MM, Newman MI, Hughes DB (2006) Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg 117(2):359–365
Motwani SB, Strom EA, Schechter NR, Butler CE, Lee GK, Langstein HN, Kronowitz SJ, Meric-Bernstam F, Ibrahim NK, Buchholz TA (2006) The impact of immediate breast reconstruction on the technical delivery of postmastectomy radiotherapy. Int J Radiat Oncol Biol Phys 66(1):76–82
Kronowitz SJ, Hunt KK, Kuerer HM, Babiera G, McNeese MD, Buchholz TA, Strom EA, Robb GL (2004) Delayed-immediate breast reconstruction. Plast Reconstr Surg 113(6):1617–1628
McKeown DJ, Hogg FJ, Brown IM, Walker MJ, Scott JR, Weiler-Mithoff EM (2009) The timing of autologous latissimus dorsi breast reconstruction and effect of radiotherapy on outcome. J Plast Reconstr Aesthet Surg 62(4):488–493 Epub 11 Feb 2008
Kroll SS, Robb GL, Reece GP, Miller MJ, Evans GR, Baldwin BJ, Wang B, Schusterman MA (1998) Does prior irradiation increase the risk of total or partial free-flap loss? J Reconstr Microsurg 14(4):263–268
Chang DW, Wang B, Robb GL et al (2000) Effect of obesity on flap and donor site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg 105:1640–1648
Chang DW, Reece GP, Wang B (2000) Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 105:2374–2380
Saulis AS, Mustoe TA, Fine NA (2007) A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: comparison of three common procedures. Plast Reconstr Surg 119:1669–1678
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barry, M., Kell, M.R. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat 127, 15–22 (2011). https://doi.org/10.1007/s10549-011-1401-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1401-x