Abstract
Gastroesophageal reflux disease (GERD) is a common condition in gastroenterology practice. Classical techniques like endoscopy and 24-h pH-metry are often used to diagnose patients with symptoms related to GERD. Although these techniques have been useful over the years both for diagnosis and therapeutic guidance, there are still many patients with typical or atypical GERD symptoms with normal endoscopy and pH-metry who do not respond adequately to anti-secretory therapy. 24-h impedance combined with pH is a new technique and currently considered as the gold standard for diagnosis of GERD. It offers greater sensitivity for the detection of all reflux episodes, and allows us to establish their nature (liquid, gas, mixed), composition (acidic, non-acidic), and clearance. This chapter describes basic principles, technique, interpretation, and clinical application of 24-h pH impedance monitoring.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Gastroesophageal reflux disease (GERD) is a common problem in Gastroenterology practice. 24-h pH-metry was considered as the gold standard for diagnosis of GERD in the past. However, 24-h pH-metry does not pickup reflux of neutral or alkaline content from the stomach. Therefore, it has a lower sensitivity to diagnose GERD and hence, this has been replaced largely by 24-h impedance pH-monitoring. It has more sensitivity for detection of all reflux episodes and confirms their nature (liquid, gas, mixed), extent, composition, and clearance.
Intraluminal impedance is based on the measurement of electrical impedance between closely arranged electrodes during a bolus passage, using a probe. Cylindrical shaped metal electrodes are mounted on a thin plastic catheter. Each neighboring pair of electrodes (impedance segment) is connected to an impedance voltage transducer, which measures the resistance between the two neighboring electrodes. Impedance refers to electrical resistance and is represented by Z. The impedance is inversely proportional to the electrical conductivity of the luminal contents and the cross-sectional area between the two electrodes [1, 2]. In the absence of swallow or reflux within the esophagus, the impedance is identified by the electrical conductivity of the inner wall and it is relatively stable, and is known as baseline impedance value [3]. Since air has a low conductivity, gaseous reflux during belching results in an increase in impedance value; in contrast, swallowed or refluxed liquid would result in a drop in impedance due to higher electrical conductivity of liquids. Bolus movement recorded by impedance monitoring are either retrograde and ante-grade (Fig. 9.1). Retrograde bolus movements denote reflux, whereas ante-grade bolus movement is due to swallow [4]. The pH sensor during impedance monitoring classifies reflux episodes as acid (<4) and non acid (>4) [5].
Impedance of Various Boluses
Conductivity of empty esophageal lumen is relatively stable (baseline impedance value 2000–4000 Ω).
Liquid reflux
retrograde drop in Z by 50 % of the baseline value, as the ionic content of the liquid bolus increases electrical conductivity.
Gaseous reflux
retrograde rise in Z by ~5000 Ω, as gas is a poor conductor of electricity.
Mixed bolus
is recognized by change in impedance both on upward and downward direction from baseline indicating presence of air as well as liquid in the bolus.
pH Monitoring
pH monitoring is performed commonly using two pH sensors made up of either glass or antimony electrodes, the proximal sensor placed 5 cm above manometrically located upper border of lower esophageal sphincter (LES) zone and the distal sensor (15 cm below the proximal sensor) placed in the stomach to assess the degree of gastric HCl secretion. Two types of reflux on 24-h pH monitoring include [4]:
-
Acidic reflux: Reduction in pH <4
-
Non-acidic reflux: pH ≥ 4
Reflux Detection by 24-h Combined Impedance pH-Monitoring
Since the current technology permits evaluation of gastroesophageal reflux events by a combination of both impedance and pH monitoring techniques, which is superior to the conventional technology, 24-h pH-impedance monitoring has replaced pH-metry alone for diagnosis of GERD. Reflux events (liquid or gaseous) are detected by impedance monitoring while the acidity of the refluxate is determined by simultaneous pH monitoring [6].
Indications
Indications for 24-h impedance pH-monitoring include (a) confirmation of the diagnosis of GERD, particularly in patients with atypical symptoms; (b) before-surgical or endoscopic anti-reflux treatment; (c) assessment of response to treatment, including nocturnal acid breakthrough in patients on proton pump inhibitor (PPI) and (d) assessment of efficacy of surgical and endoscopic therapy. In such clinical situations, impedance testing is able to assess non-acid reflux as well [7–10].
Equipment
The equipment consists of a pH-impedance catheter, data logger (Fig. 9.2) with flash card, and computer with software,. Catheters are long, flexible tubes made of polyurethane in a variety of diameters and lengths. The catheters have multiple impedance sensor pairs along their length and one or two pH sensors made of either glass or antimony (Figs. 9.3 and 9.4) [11]. The standard pH-impedance catheter has six to eight pairs of impedance sensors that collect data 3, 5, 7, 9, 15, and 17 cm proximal to the LES [5].
Technique
Steps to be taken prior to and during the monitoring are discussed here.
Patient Preparation
24 h pH-impedance monitoring is done after an overnight fast. All drugs that could affect esophageal motility must be discontinued at least 72 h before the study. Often, the study is done while the patient is off anti-secretory agents including PPI. However, to assess response to anti-secretory treatment or nocturnal acid breakthrough, the study has to be done while the patient is on therapy [12]. The procedure must be adequately explained to the patient.
Entering Patients Details into the System
Since 24-h pH impedance monitoring is an ambulatory procedure, the recorded data are collected in a flash card, which is a component of the data logger. Hence, the flash card is inserted into the computer with the pH impedance monitoring software and is fed with the patient’s details, such as name, hospital number, age, and gender. There are three event keys which are selected for symptoms (such as event key 1 for heartburn, key 2 for regurgitation, and key 3 for chest pain). Subsequently, the flash card is re-inserted into the data logger and then the procedure is initiated.
Electrode Calibration
Electrodes must be calibrated before each study, as failure to do so may lead to gross inaccuracy. Calibration is performed with both an acidic and neutral buffer of known pH (usually pH 4 and 7) [11, 12]. Usually, the probe is dipped in pH 4 solution first, then in pH 7 for calibration after washing in between with distilled water.
Positioning of the Catheter
The catheter is positioned into the esophagus through transnasal route. Initially, both the pH electrodes (proximal and distal) are placed deep inside the stomach and then the catheter is pulled gradually to position the proximal port 5 cm above the manometrically determined upper margin of LES zone. Since the change in the pH from stomach to esophagus (acid drift) can be seen in real time, this parameter also helps in placement of the pH sensor. The proximal pH electrode needs to be placed 5-cm above the upper border of LES, determined on manometry. The distal pH electrode is kept in the stomach to record gastric acidity [12]. The proximal end of the catheter emerging from the patient’s nose is affixed to the face with tape during the study period (Fig. 9.5).
24-h Monitoring
The data logger is hung from the patient’s shoulder throughout the 24-h study period. A diary is given to the patient with instructions to record the time of meal, symptoms, and body posture. The patient is also instructed to press the pre-defined event markers in the data logger for all such events such as a meal, lying down, getting up, and symptoms. The patient is instructed to continue usual daily activities and diet, including those activities known to precipitate symptoms, as changes in typical routines may affect data interpretation. The patient is asked to avoid acidic drinks during the study period. Once the study is completed, the catheter is removed. Subsequently, the flash card is inserted into the computer with software and the signal files are downloaded and analyzed.
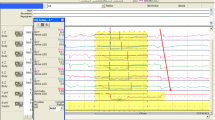
During the analysis, the signal is visually scanned for adequacy of recording including events marks, gastric pH, and presence of reflux (Fig. 9.6). All reflux events are analyzed during the total recording period, in upright and supine phases. From the impedance-pH recordings, the parameters of acid and bolus exposure are analyzed using the software (Tables 9.1 and 9.2) [4]. The standard cut-off values of percentage time of 24-h recording period, esophageal pH below 4, and of bolus exposure are used to diagnose abnormal gastroesophageal reflux, as shown in Tables 9.1 and 9.2. Based on whether the abnormal reflux occurred during supine or upright period during 24-h recording, patients are further diagnosed as having supine, upright, or combined refluxers.
Definition of Esophageal Reflux Parameters
Acid exposure (%)
Defined as the total time during which the lower esophageal pH was below four divided by the duration of monitoring.
Bolus exposure (%)
Defined as being analogous to acid exposure by adding the duration of all reflux defined by impedance, and dividing this value by duration of monitoring.
Symptom index (SI)
Defined as the number of symptoms associated with reflux divided by the total number of symptoms. A value of SI ≥50 % is abnormal and is considered to diagnose GERD (i.e., at least half of symptoms are associated with reflux).
Normal Values of Reflux Parameters
Normal values for impedance-pH monitoring off acid-suppression therapy have been determined from studies on healthy volunteers [13–15]. Based on the 95th percentile as the upper limit of normal, the proposed normal value of total distal reflux is ≤ 73, percentage time distal esophageal pH ≤4.2 (pH parameter), and percentage bolus exposure ≤ 1.1 (impedance parameter) (Table 9.1).
Published data on normal values for impedance-pH monitoring while on acid-suppression therapy are lacking. Such studies are important for interpreting esophageal impedance pH monitoring studies while on acid-suppressive treatment, as persistent symptoms of gastroesophageal reflux while on acid-suppression therapy is not uncommon. A study by Vela et al. reported that PPI therapy reduced the number of acid reflux episodes with a proportional increase in non-acid reflux, the net result of which was an unchanged total number of reflux episodes on or off therapy as observed during post-prandial studies [16]. The normal range of reflux episodes “on therapy” (<73) has been determined by extrapolating the data from healthy volunteers “off therapy” [13] and by assuming that PPI primarily changes the pH of the refluxate without affecting the total number of reflux episodes [16]. This presumption, however, may not be entirely correct.
Interpretation
During assessment of pH- impedance tracings, the impedance channels are used to detect the occurrence of reflux, and pH changes help to classify the reflux episodes as acid (pH < 4) or non-acid (pH > 4) [9]. Data analysis is performed on the liquid and mixed reflux episodes during the upright, supine, and total phases of measurement. Parameters recorded during pH-impedance monitoring include: (a) total reflux (liquid and gaseous) percent time and those in upright and recumbent postures; (b) acidic and non-acidic reflux in upright, recumbent, and both postures; (c) duration of esophageal pH < 4 in upright, recumbent, and both the postures; (d) acid exposure percent time in upright, recumbent, and both the postures; (e) mean acid clearance time; and (f) symptom correlation to reflux (acidic and non-acidic) [11].
Clinical Utility
In contrast to pH-metry alone, impedance-pH metry can detect non-acid and gas reflux in addition to acidic reflux [5, 7, 17]. Therefore, it may be used to diagnose reflux even while the patient is on treatment with acid-lowering drugs [18, 19]. In this condition, impedance testing is intended to assess whether non-acid reflux is the cause of ongoing symptoms. In the pH-impedance technique, proximal extent of reflux can be assessed, the type of refluxate be determined (gas, mixed, or liquid), and a calculated SI may help to evaluate whether the ongoing symptoms correlate with reflux events [20].
A number of studies have evaluated the utility of impedance testing in GERD patients both on and off PPI therapy. Moreover, in patients with repeated belching, impedance monitoring may help to determine whether the belching is gastric or supra-gastric in nature, and whether there is associated GERD.
A study of 60 patients on PPI treatment reported higher SI with 24-h impedance-pH monitoring compared with pH testing alone (77.1 % vs 66.7 %, p < 0.05). Another study of 150 patients with non-erosive reflux disease undergoing 24-h impedance-pH monitoring (off PPI therapy) found that 87 patients (58 %) had a normal esophageal acid exposure. However, 15 % of them had a positive SI for acid, 12 % for non-acid, and 5 % for both. Two studies aimed to evaluate genesis of symptom development following reflux reported that a higher proximal extent, greater reduction in pH, prolonged acid clearance time, and mixed reflux (air and liquid) were more likely to be associated with symptoms. These studies suggest that 24-h impedance-pH monitoring (off PPI therapy) in patients with typical symptoms is more sensitive than pH testing alone [21–24].
In a study of 168 patients with persistent GERD symptoms despite twice-daily PPI therapy, 86 % were found symptomatic during the 24-h impedance-pH monitoring test; however, more than half of the symptomatic patients had a negative SI (e.g., symptoms did not correlate with a reflux event). Of the 69 patients with a positive SI, acid reflux was the cause of symptom in 11 % and non-acid reflux in 37 %, which was only detectable by impedance. In another multicentric study of 150 patients, a positive SI was found in association with non-acid reflux in 32 %. Thus, these studies suggest that 30–40 % of patients with persistent symptoms on PPI therapy have non-acid reflux as a cause, and this can currently only be identified with impedance testing.
24-h impedance-pH monitoring is useful to investigate patients with atypical symptoms (cough, hoarseness) of GERD [25–31]. In a study of 22 patients with unexplained chronic cough who underwent impedance-pH monitoring, 30.6 % of coughing episodes were associated with reflux. Another study of 100 patients with unexplained chronic cough underwent impedance-pH monitoring. They found that chronic cough was temporally associated with a reflux event in almost 50 % of patients. These studies suggest that 24-h impedance-pH monitoring may diagnose GERD as a cause of chronic cough in some patients that would be missed with only pH testing.
Advantages of impedance-pH metry, therefore, may be summarized as:
-
Nature (liquid, gaseous or mixed), movement, and extent of reflux in the esophageal lumen can be detected
-
Efficacy of the PPI therapy can be checked
-
This technique has a higher yield in identifying patients with cough due to reflux compared to pH monitoring alone
-
Analysis of the relationship between symptoms and all types of reflux events, both acid and non-acid
However, the disadvantages include:
-
pH-impedance technique cannot estimate the volume of the refluxate
-
Costly and time-consuming procedure
-
Interpretation of non-acid reflux episodes has a high inter-observer variability
-
Automatic analysis considers only a drop of impedance of ≥ 50 % as a reflux episode; however, a drop of 49 % also can contribute to a reflux episode
-
The recordings are complex and filled with artifacts; a thorough (and time-consuming) review of the recordings, episode by episode, is still required
Conclusion
Though all patients with GERD may not need physiological testing for confirmation of abnormal gastroesophageal reflux, these tests are essential in a subset of patients. Catheter-based 24-h impedance pH monitoring scores over conventional 24-pH metry. In expert hand, 24-h pH impedance monitoring is easy to perform and analyze. These physiological tests are also useful to assess response to pharmacological and non-pharmacological treatment for GERD, when indicated.
References
Nguyen HN, Domingues GR, Lammert F. Technological insights: combined impedance manometry for esophageal motility testing-current results and further implications. World J Gastroenterol. 2006;12:6266–73.
Fass J, Silny J, Braun J, Heindrichs U, Dreuw B, Schumpelick V, et al. Measuring esophageal motility with a new intraluminal impedance device. First clinical results in reflux patients. Scand J Gastroenterol. 1994;29:693–702.
Dolder M, Tutuian R. Laboratory based investigations for diagnosing gastroesophageal reflux disease. Best Pract Res Clin Gastroenterol. 2010;24:787–98.
Cho YK. How to interpret esophageal impedance pH monitoring. J Neurogastroenterol Motil. 2010;16:327–30.
Tutuian R, Castell DO. Review article: complete gastro-oesophageal reflux monitoring – combined pH and impedance. Aliment Pharmacol Ther. 2006;24 Suppl 2:27–37.
Sifrim D, Fornari F. Esophageal impedance-pH monitoring. Dig Liver Dis. 2008;40:161–6.
Bredenoord AJ. Impedance-pH monitoring: new standard for measuring gastro-oesophageal reflux. Neurogastroenterol Motil. 2008;20:434–9.
Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:647–55.
Villa N, Vela MF. Impedance-pH testing. Gastroenterol Clin North Am. 2013;42:17–26.
Sifrim D, Holloway R, Silny J, Xin Z, Tack J, Lerut A, et al. Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology. 2001;120:1588–98.
Ghoshal UC, Singh R, Misra A. Esophageal function tests in clinical practice: a review. Trop Gastroenterol. 2010;31:145–54.
Wang A, Pleskow DK, Banerjee S, Barth BA, Bhat YM, Desilets DJ, et al. Esophageal function testing. Gastrointest Endosc. 2012;76:231–43.
Shay S, Tutuian R, Sifrim D, Vela M, Wise J, Balaji N, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–43.
Zentilin P, Iiritano E, Dulbecco P, Bilardi C, Savarino E, De Conca S, et al. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig Liver Dis. 2006;38:226–32.
Zerbib F, des Varannes SB, Roman S, Pouderoux P, Artigue F, Chaput U, et al. Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian-French cohort of healthy subjects. Aliment Pharmacol Ther. 2005;22:1011–21.
Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001;120:1599–606.
Tutuian R, Castell DO. Reflux monitoring: role of combined multichannel intraluminal impedance and pH. Gastrointest Endosc Clin N Am. 2005;15:361–71.
Galmiche JP. Impedance-pH monitoring in proton pump inhibitor resistant patients: ready for clinical application? Gut. 2006;55:1379–81.
Hirano I, Richter JE. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. 2007;102:668–85.
Vela MF. Non-acid reflux: detection by multichannel intraluminal impedance and pH, clinical significance and management. Am J Gastroenterol. 2009;104:277–80.
Bredenoord AJ, Weusten BL, Timmer R, Conchillo JM, Smout AJ. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am J Gastroenterol. 2006;101:453–9.
Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni MC, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–93.
Bredenoord AJ, Weusten BL, Curvers WL, Timmer R, Smout AJ. Determinants of perception of heartburn and regurgitation. Gut. 2006;55:313–8.
Tutuian R, Vela MF, Hill EG, Mainie I, Agrawal A, Castell DO. Characteristics of symptomatic reflux episodes on Acid suppressive therapy. Am J Gastroenterol. 2008;103:1090–6.
Mainie I, Tutuian R, Shay S, Vela M, Zhang X, Sifrim D, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–402.
Tutuian R, Mainie I, Agrawal A, Adams D, Castell DO. Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest. 2006;130:386–91.
Bajbouj M, Becker V, Neuber M, Schmid RM, Meining A. Combined pH-metry/impedance monitoring increases the diagnostic yield in patients with atypical gastroesophageal reflux symptoms. Digestion. 2007;76:223–8.
Blondeau K, Tack J. Pro: impedance testing is useful in the management of GERD. Am J Gastroenterol. 2009;104:2664–6.
Zerbib F, Roman S, Ropert A, des Varannes SB, Pouderoux P, Chaput U, et al. Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am J Gastroenterol. 2006;101:1956–63.
Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–54.
Blondeau K, Dupont LJ, Mertens V, Tack J, Sifrim D. Improved diagnosis of gastro-oesophageal reflux in patients with unexplained chronic cough. Aliment Pharmacol Ther. 2007;25:723–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer India
About this chapter
Cite this chapter
Ghoshal, U.C., Singh, R. (2016). Catheter-Based 24-h pH-Metry and Impedance: Technique, Interpretation, and Clinical Application. In: Ghoshal, U. (eds) Evaluation of Gastrointestinal Motility and its Disorders. Springer, New Delhi. https://doi.org/10.1007/978-81-322-0822-8_9
Download citation
DOI: https://doi.org/10.1007/978-81-322-0822-8_9
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-0821-1
Online ISBN: 978-81-322-0822-8
eBook Packages: MedicineMedicine (R0)