Abstract
A review of relevant publications revealed that the criteria for defining refractory constipation were ill-defined. Common treatment for constipation includes osmotic, stimulant, and enterokinetic agents. Prucalopride is a new enterokinetic agent that has been shown in clinical trials to produce significant improvements in bowel functions, gastrointestinal symptoms, and quality of life. Patients who fail pharmacological treatment should be referred to specialized centers for physiological laboratory evaluation like transit studies, balloon expulsion, anorectal manometry, and defecography. Potential pathophysiology of refractory constipation include physiological disturbances like pelvic floor dyssynergia and slow transit constipation. Physical defects such as rectocoele and internal prolapse are uncommon. Psychological disturbances have been linked to persistent GI symptoms. Non-pharmacological treatments to consider include biofeedback and behavioral therapy. More studies are needed before surgery can be recommended. There is the possibility that a wider acceptance of the use of laxatives may substantially reduce the number of patients with refractory constipation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Before embarking on the work-up and management of refractory constipation, the clinician must ask, what is refractory constipation? Situations where patients may be considered to have refractory constipation are when patients are subjected to clinical trials of new pharmacological agents or referred for total colectomy. A review of relevant publications revealed that the criteria for defining refractory constipation were ill-defined. The majority of studies reported duration of constipation, and simply that laxatives had been unsuccessful. No information was available to determine the type of laxatives, dosing, and duration of treatments. In a recent review by the Asian Neurogastroenterology & Motility Association, a pharmacological non-responder was defined as failure to respond to bisacodyl at 10 mg every night for at least 4 weeks, with consideration given to a total treatment period of up to 12 weeks if access to specialized centers is limited, or prucalopride at 2 mg daily for up to 12 weeks, and combining a stimulant or prokinetic agent with an osmotic agent may also be considered [1]. This is based on recent high-quality clinical trials which demonstrated improvement in quality-of-life scores in patients on daily treatment with either of these agents for 4 weeks (bisacodyl or picosulfate) to 12 weeks (prucalopride) [2–6]. Contrary to popular belief, patients who had received active treatment with bisacodyl were able to reduce their dosage with time [6].
Prucalopride is a new enterokinetic agent that has been shown in clinical trials to produce significant improvements in bowel functions, gastrointestinal symptoms, and quality of life, with improvements maintained on continued use for up to 24 months [2–4, 7]. Based on secondary endpoint analysis of data derived from the pivotal studies, it appears that prucalopride may be particularly effective at improving bloating [8].
Other treatments that may be explored in the future are lubiprostone and linaclotide, which belong to a new class of pharmacological agents known as colonic secretagogues. Table 7.1 serves as a guide to the feasibility of maximizing pharmacological agents before labeling a patient as having refractory constipation. The information on dosing ranges and treatment durations is based on those used in clinical trials of these agents. However, it is unclear if such an extended treatment can produce durable improvement.
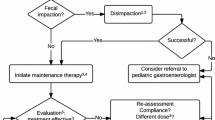
Patients who fail pharmacological treatment should be referred to specialized centers for physiological laboratory evaluation (see Fig. 7.1).
Potential Pathophysiology of Refractory Constipation
Physiological Factors
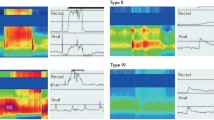
The two main physiological disturbances associated with refractory constipation are pelvic floor dyssynergia (PFD) and slow transit constipation (STC). Pelvic floor dyssynergia (alternative terms are anismus or obstructed defecation disorder) refers to paradoxical contraction or inadequate relaxation of the pelvic floor muscles during attempted defecation; this is believed to be an acquired behavioral disorder of defecation. Slow transit constipation is also referred to by its old name of colonic inertia, and refers to the inability of the colon to modify stool to an acceptable consistency and move the stool from the cecum to the rectosigmoid area. An alternative definition is prolonged colonic transit time that cannot be normalized even by the consumption of large amounts of dietary fiber. There is a wide variability of methodology used to measure colonic transit times, and the reproducibility of these tests is not high, and especially so for slow transit times [9]. Studies of patients referred to tertiary centers in Korea and Thailand (for presumed refractory constipation), reported PFD in 30–35 %, STC in 13–20 %, and PFD combined with STC 11–27 %, but a substantial proportion had normal transit constipation (13–47 %) [10, 11]. Similar to studies from the west, these Asian studies suggest that symptoms alone cannot distinguish the different constipation subtypes.
Anatomical Factors
Physical defects such as rectocoele (herniation of the rectal wall with retention of stool in the hernia after defecation) and internal prolapse are uncommon, reported in less than 1 %, even in tertiary centers [12]. At least one study has reported that biofeedback can help more than half of these patients to overcome their constipation without the need for surgical repair [13].
Psychological Factors
An important aspect that is frequently overlooked is the psychological one. Numerous studies had shown the association of abuse history, in particular sexual and childhood abuse, with functional gastrointestinal diseases. Depression is not uncommon, especially in the elderly. In young women with severe constipation, the possibility of an eating disorder should be considered [14]. The possibility of a past history of sexual and physical abuse should be kept in mind [15]. In a referral-based clinic, Drossman et al. reported that of 206 women with functional gastrointestinal disorders, 44 % reported a history of sexual abuse or physical abuse in childhood or later in life. However, only 17 % had informed their doctors about the abuse. As these women may be psychologically predisposed to submit themselves to surgery, it is especially important for the physician to ask specifically for a history of abuse before contemplating a referral to a surgeon [15–17]. There is a strong possibility that psychological factors are a major reason for refractory constipation. Psychological disturbances have been linked to persistent GI symptoms and frequent health-seeking behavior as well as failure to respond to tertiary-level treatment [18, 19].
Non-pharmacological Treatments
Biofeedback and Behavioral Therapy
Biofeedback is a training technique which aims to teach patients to relax, instead of contracting, their pelvic floor muscles during straining at stool. There are several variations of the method; some involve the use of visual or auditory signals, from surface or electromyographic electrodes or anal probes, to inform patients whether they are performing the appropriate muscular action. In its most basic form, patients may also be trained to evacuate rectal contents by using a balloon, or even oatmeal porridge in the shape of a stool, introduced into the rectum to simulate defecation [20, 21]. Currently, biofeedback therapy is applied primarily to patients with PFD. Overall, biofeedback is a safe treatment which may produce durable improvement beyond the active treatment period. Randomized control trials in refractory chronic constipation patients with PFD have reported 70–80 % success rates for up to 1 year [22–24]. Improvement was reported for constipation symptoms and overall symptoms, as well as dyssynergic pattern of defecation. However, the impact on quality of life or psychological state has not been fully assessed. As many as two-thirds of patients referred for biofeedback could have diagnosable psychiatric disorders, and those patients with a higher degree of quality-of-life impairment due to psychological distress are less likely to respond to biofeedback treatment [25].
Surgery
The scientific rationale for surgical treatments has not been clearly articulated. When contemplating a surgical referral, the following reservations should be considered. Initially promising results with small numbers of highly selected patients may not be replicated when extended to larger series with longer term follow-up. Surgical treatments have not been evaluated to the same rigorous degree that modern pharmacological agents are subjected to. Non-destructive treatment approaches may become available or prove to be more effective. An example is that in the 1970s and 1980s an operation known as anorectal myectomy was advocated for adult patients with outlet obstruction. However, longer term follow-up revealed that in the majority of patients, the improvement was not sustained, and there was a high incidence of incontinence [26, 27]. In its place, biofeedback is now offered to patients with outlet obstruction. Similarly, for sub-total colectomy with ileo-rectal anastomosis, which is advocated for colonic inertia, initial series comprising 6–30 patients followed up for up to 6 years reported satisfactory results in 60–100 %, but when one of these studies was extended for another 3 years and expanded to include 44 patients, the proportion of patients who were able to maintain normal bowel function fell to 50 %, while 71 % continued to experience abdominal pain, 39 % required further surgery, and almost a quarter required psychiatric treatment for severe psychological disturbances [28–31]. A number of studies have also in the past demonstrated that when bisacodyl was instilled into the colon of patients classified as colonic inertia, as many as 60–90 % achieved high amplitude propagated contractions [32–34]. This suggests that if high enough levels of the stimulant agent could be delivered, some of these colons could have been salvaged.
The possibility of a Munchausen phenomenon should be seriously considered in patients willing to subject themselves to an ablative procedure like colectomy. Patients with a history of sexual abuse had a ten-fold increased risk of surgery prior to their colectomy, and had a high probability of seeking medical care for abdominal complaints after their colectomy [35–38].
A number of recent studies found that the majority of patients with severe STC had evidence of small bowel motor abnormalities and are at risk of intestinal obstruction post-colectomy [39–43]. Our position is that any patient with functional constipation who is being considered for surgical intervention must undergo a formal psychiatric evaluation and an evaluation of GI motility with, at the minimum, measurement of small intestinal transit time.
Conclusion
The management of refractory constipation remains a challenge, not least because criteria for refractoriness has not been clearly defined. On the one hand, there is much prejudice regarding the use of laxatives that is not evidence based, while on the other hand, there is much uncritical acceptance of the effectiveness of fiber treatment that is poorly substantiated. There is the possibility that a wider acceptance of the use of laxatives may substantially reduce the number of patients with refractory constipation. The main challenge appears to be to identify and recognize the role that psychological disturbances play in refractory constipation. More attention to psychologically directed treatments, including biofeedback, with greater accessibility to these treatments, may help to reduce the number of patients who are driven to the treatment of last resort, ablative surgery.
References
Gwee KA, Ghoshal UC, Gonlachanvit S, Chua AS, Myung SJ, Rajindrajith S, et al. Primary care management of chronic constipation in Asia: the ANMA chronic constipation tool. J Neurogastroenterol Motil. 2013;19:149–60.
Quigley EM, Vandeplassche L, Kerstens R, Ausma J. Clinical trial: the efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation--a 12-week, randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2009;29:315–28.
Camilleri M, Kerstens R, Rykx A, Vandeplassche L. A placebo-controlled trial of prucalopride for severe chronic constipation. N Engl J Med. 2008;358:2344–54.
Tack J, van Outryve M, Beyens G, Kerstens R, Vandeplassche L. Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Gut. 2009;58:357–65.
Ke M, Zou D, Yuan Y, et al. Prucalopride in the treatment of chronic constipation in patients from the Asia-Pacific region: a randomized, double-blind, placebo-controlled study. Neurogastroenterol Motil. 2012;24:999–e541.
Kamm MA, Mueller-Lissner S, Wald A, Richter E, Swallow R, Gessner U. Oral bisacodyl is effective and well-tolerated in patients with chronic constipation. Clin Gastroenterol Hepatol. 2011;9:577–83.
Camilleri M, Van Outryve MJ, Beyens G, Kerstens R, Robinson P, Vandeplassche L. Clinical trial: the efficacy of open-label prucalopride treatment in patients with chronic constipation – follow-up of patients from the pivotal studies. Aliment Pharmacol Ther. 2010;32:1113–23.
Kerstens R, Vandeplassche L, Dubois D, Wouters L. Response of chronic constipation symptoms to prucalopride treatment and relationship with patient satisfaction. Gut. 2011;60:A159.
Rao SS, Ozturk R, Laine L. Clinical utility of diagnostic tests for constipation in adults: a systematic review. Am J Gastroenterol. 2005;100:1605–15.
Gonlachanvit S, Patcharatrakul T. Causes of idiopathic constipation in Thai patients: associations between the causes and constipation symptoms as defined in the Rome II criteria. J Med Assoc Thai. 2004;87 Suppl 2:S22–8.
Kim DH, Myung SJ, Yang SK, et al. Clinical parameters for differentiating pelvic floor dyssynergia (PFD) in constipated patients. Korean J Gastroenterol Motil. 2002;8:167–76.
Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of constipation in a tertiary referral gastroenterology practice. Am J Gastroenterol. 1995;90:1471–5.
Lau CW, Heymen S, Alabaz O, Iroatulam AJ, Wexner SD. Prognostic significance of rectocele, intussusception, and abnormal perineal descent in biofeedback treatment for constipated patients with paradoxical puborectalis contraction. Dis Colon Rectum. 2000;43:478–82.
Boyd C, Abraham S, Kellow J. Psychological features are important predictors of functional gastrointestinal disorders in patients with eating disorders. Scand J Gastroenterol. 2005;40:929–35.
Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–33.
Arnold RP, Rogers D, Cook DA. Medical problems of adults who were sexually abused in childhood. BMJ. 1990;300:705–8.
Bachmann GA, Moeller TP, Benett J. Childhood sexual abuse and the consequences in adult women. Obstet Gynecol. 1988;71:631–42.
Koloski NA, Talley NJ, Boyce PM. Does psychological distress modulate functional gastrointestinal symptoms and health care seeking? A prospective, community Cohort study. Am J Gastroenterol. 2003;98:789–97.
Mason HJ, Serrano-Ikkos E, Kamm MA. Psychological state and quality of life in patients having behavioral treatment (biofeedback) for intractable constipation. Am J Gastroenterol. 2002;97:3154–9.
Bleijenberg G, Kuijpers HC. Treatment of the spastic pelvic floor syndrome with biofeedback. Dis Colon Rectum. 1987;30:108–11.
Lestar B, Penninckx F, Kerremans R. Biofeedback defaecation training for anismus. Int J Colorectal Dis. 1991;6:202–7.
Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–64.
Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007;50:428–41.
Rao SS, Seaton K, Miller M, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007;5:331–8.
Dykes S, Smilgin-Humphreys S, Bass C. Chronic idiopathic constipation: a psychological enquiry. Eur J Gastroenterol Hepatol. 2001;13:39–44.
Yoshioka K, Keighley MR. Randomized trial comparing anorectal myectomy and controlled anal dilatation for outlet obstruction. Br J Surg. 1987;74:1125–9.
Pinho M, Yoshioka K, Keighley MR. Long term results of anorectal myectomy for chronic constipation. Br J Surg. 1989;76:1163–4.
Schouten WR. Severe, longstanding constipation in adults. Indications for surgical treatment. Scand J Gastroenterol Suppl. 1991;188:60–8.
Kamm MA, Hawley PR, Lennard-Jones JE. Outcome of colectomy for severe idiopathic constipation. Gut. 1988;29:969–73.
Nyam DC, Pemberton JH, Ilstrup DM, Rath DM. Long-term results of surgery for chronic constipation. Dis Colon Rectum. 1997;40:273–9.
Ghosh S, Papachrysostomou M, Batool M, Eastwood MA. Long-term results of subtotal colectomy and evidence of noncolonic involvement in patients with idiopathic slow-transit constipation. Scand J Gastroenterol. 1996;31:1083–91.
Bassotti G, Chiarioni G, Germani U, Battaglia E, Vantini I, Morelli A. Endoluminal instillation of bisacodyl in patients with severe (slow transit type) constipation is useful to test residual colonic propulsive activity. Digestion. 1999;60:69–73.
Herve S, Savoye G, Behbahani A, Leroi AM, Denis P, Ducrotte P. Results of 24-h manometric recording of colonic motor activity with endoluminal instillation of bisacodyl in patients with severe chronic slow transit constipation. Neurogastroenterol Motil. 2004;16:397–402.
Kamm MA, van der Sijp JR, Lennard-Jones JE. Observations on the characteristics of stimulated defaecation in severe idiopathic constipation. Int J Colorectal Dis. 1992;7:197–201.
O’Brien S, Hyman N, Osler T, Rabinowitz T. Sexual abuse: a strong predictor of outcomes after colectomy for slow-transit constipation. Dis Colon Rectum. 2009;52:1844–7.
FitzHarris GP, Garcia-Aguilar J, Parker SC, Bullard KM, Madoff RD, Goldberg SM, et al. Quality of life after subtotal colectomy for slow-transit constipation: both quality and quantity count. Dis Colon Rectum. 2003;46:433–40.
El-Tawil AM. Persistence of abdominal symptoms after successful surgery for idiopathic slow transit constipation. South Med J. 2002;95:1042–6.
Zutshi M, Hull TL, Trzcinski R, Arvelakis A, Xu M. Surgery for slow transit constipation: are we helping patients? Int J Colorectal Dis. 2007;22:265–9.
Zarate N, Knowles CH, Yazaki E, Lunnis PJ, Scott SM. Clinical presentation and patterns of slow transit constipation do not predict coexistent upper gut dysmotility. Dig Dis Sci. 2009;54:122–31.
Seidl H, Gundling F, Pehl C, Pfeiffer A, Schepp W, Schmidt T. Small bowel motility in functional chronic constipation. Neurogastroenterol Motil. 2009;21:1278–e122.
Preston DM, Hawley PR, Lennard-Jones JE, Todd IP. Results of colectomy for severe idiopathic constipation in women (Arbuthnot Lane’s disease). Br J Surg. 1984;71:547–52.
Knowles CH, Scott M, Lunniss PJ. Outcome of colectomy for slow transit constipation. Ann Surg. 1999;230:627–38.
Glia A, Akerlund JE, Lindberg G. Outcome of colectomy for slow-transit constipation in relation to presence of small-bowel dysmotility. Dis Colon Rectum. 2004;47:96–102.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer India
About this chapter
Cite this chapter
Gwee, KA., Gong, X., Siah, K.T.H. (2016). Approach to Patients with Refractory Constipation. In: Ghoshal, U. (eds) Evaluation of Gastrointestinal Motility and its Disorders. Springer, New Delhi. https://doi.org/10.1007/978-81-322-0822-8_7
Download citation
DOI: https://doi.org/10.1007/978-81-322-0822-8_7
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-0821-1
Online ISBN: 978-81-322-0822-8
eBook Packages: MedicineMedicine (R0)