Abstract
The biomechanical studies showed that the anatomic single-bundle (SB) reconstruction was significantly better concerning the knee stability under a 90-N anterior force and a 5-Nm internal torque than the conventional SB reconstruction in a range between 0 and 30°. However, there were no significant differences between the two reconstructions not only in the other ranges of knee flexion under these loading conditions but also in all the ranges under the simulated pivot shift test. On the other hand, the anatomic double-bundle (DB) reconstruction was significantly better concerning the knee stability under a 90-N anterior force and a 5-Nm internal torque than the conventional SB reconstruction not only in a range between 0 and 30° but also in the range between 35 and 70°. In addition, the anatomic DB reconstruction was significantly better under the simulated pivot shift test than the conventional SB reconstruction in a range between 0 and 30°. These results showed that although both the anatomic SB and DB reconstructions were significantly better than conventional SB reconstruction, the effect of the anatomic SB reconstruction on the knee stability is not completely identical to the effect of the anatomic DB reconstruction. Preliminary in vivo data suggest that anatomic DB reconstruction can restore normal knee kinematics, but further studies including research on anatomic SB reconstruction are required before definitive conclusions can be reached.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anterior cruciate ligament
- Anteromedial bundle
- Anatomic reconstruction
- Double bundle
- Posterolateral bundle
- Single bundle
1 Introduction
Single-bundle (SB) reconstruction of the anterior cruciate ligament (ACL) is the standard surgical option to treat ACL-deficient knees. However, recent biomechanical studies have reported that conventionally performed SB ACL reconstruction cannot restore normal anterior translation or rotatory laxity [1, 2]. Kinematic studies have also shown that the SB reconstruction cannot completely restore the patient’s rotatory stability during walking or more strenuous activities [3, 4]. The normal ACL consists of anteromedial (AM) and posterolateral (PL) bundles, which have different functions [5–8]. To improve such biomechanical disadvantages of SB reconstruction, Yasuda et al. [9, 10] reported the first practical arthroscopic procedure to anatomically reconstruct both the AM and PL bundles of the ACL in 2004. Several biomechanical studies have reported significantly better knee stability than after conventional SB reconstruction [11–13]. On the other hand, recently, an idea of anatomic SB ACL reconstruction, in which the femoral tunnel is created at the center of the AM and PL bundle attachments on the femur, has attracted notice in the clinical field [14, 15]. Thus, a following question has been arisen. Is the effect of the anatomic SB reconstruction on the knee stability completely identical to the effect of the anatomic DB reconstruction? The first aim of this chapter is to answer this question. To answer to the question, the authors compared the degrees of superiority of the anatomic SB and DB reconstructions to the conventional SB reconstruction, using the previously reported database of the knee laxity after various ACL reconstruction procedures [16].
The second aim of this chapter is to answer the following question: Can the clinically available transtibial procedure for anatomic DB reconstruction really obtain significantly better knee stability in comparison with the conventional SB reconstruction procedure? This question must be asked because the previous biomechanical studies, which reported that the former procedure can obtain significantly better knee stability than the latter procedure [11–13], widely exposed the knee joint and directly identify the anatomic attachments. Clinically, however, the authors have used an arthroscopic transtibial procedure for femoral tunnel creation. Therefore, there is a possibility that the femoral tunnel positions in the clinical are not identical to the ideal tunnel locations created in the previous biomechanical studies. To answer the following question, the authors performed the arthroscopic transtibial procedure of anatomic DB reconstruction, which had been performed in the authors’ clinical practice, in cadaver specimens, and compared the results with those of the conventional SB reconstruction procedure [11].
2 Is the Effect of the Anatomic SB ACL Reconstruction Completely Identical to the Effect of the Anatomic DB ACL Reconstruction?
2.1 Methods
Eight fresh-frozen cadaveric knees were used in this study [16]. Each knee was mounted onto the specially designed apparatus, which was reported in the previous literature in detail [17]. The intact knee was moved by hand from full extension to 110° of flexion and then back to extension for three cycles. Then, the below-described measurement of the knee laxity was repeated in the normal knee and the ACL-reconstructed knees. Each of the following loads was applied to the tibia: (1) 90-N tibial anterior drawer force, (2) 5-Nm tibial internal rotation torque, (3) 5-Nm tibial external rotation torque, and (4) a combined load to simulate the pivot shift test: 50-N iliotibial tract tension, 5-Nm valgus moment, and 1-Nm tibial internal rotation torque, according to our previous works [18, 19]. The iliotibial tract was loaded by linking it with a nylon cable to a pneumatic cylinder. In each loading condition, three cycles of knee flexion-extension between 0 and 110° were repeated manually. The kinematics of the tibiofemoral joint was measured dynamically with a Polaris stereo optical system (Northern Digital Inc., Waterloo, Canada) with Traxtal active optical trackers (Traxtal Technologies Inc., Toronto, Canada) mounted on the tibia and femur.
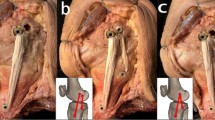
The conventional SB reconstruction procedure was performed using the same technique as the above-described study (Fig. 9.1a) [10]. In anatomic SB reconstruction, the tibial tunnel was placed at the center of the normal ACL attachment between the medial and lateral tibial eminences, and the femoral tunnel was placed at the center between the AM and PL bundle attachments (Fig. 9.1b). The anatomic DB reconstruction was performed with the previously reported procedure with a specially designed device (Fig. 9.1c) [20, 21]. After one reconstruction was made in a cadaver knee, the knee laxity was measured. Then, after the graft was removed and the vacant tunnel was filled with polyester resin paste, the next reconstruction was performed and the knee laxity was measured. Thus, the knee laxity data after each ACL reconstruction were obtained, independent from the order of measurement. The following analyses were made using this database. The authors divided the whole range of knee flexion into three ranges, a range between 0 and 30°, a range between 35 and 70°, and a range between 75 and 110°, and comparisons were made in each range. Rather than present normal laxity data, this article displays the changes from normal, which has greater clarity regarding residual laxities after the reconstructions.
(a, b, c): The conventional single-bundle procedure A, the single femoral tunnel was placed at the center of the anatomic attachment of the anteromedial bundle of the ACL; B, the tibial tunnel was placed at the center of the anatomic attachment of the ACL; C, the intra-articular autogenous tendon graft was composed of 4 strands of tendons
(d, e, f): The anatomic single-bundle procedure A, the femoral tunnel was placed at the center of the anatomic attachment of the ACL; B, the tibial tunnel was placed at the center of the anatomic attachment of the ACL; C, the autogenous tendon portion of the graft was composed of 4 strands of tendon
(g. h, i): The anatomic double-bundle procedure A, two femoral tunnels were created at the centers of the anatomic attachments of the anteromedial and posterolateral bundles; B, two tibial tunnels were created at the centers of the anatomic attachments of the anteromedial and posterolateral bundles; C, the two tendon grafts placed in the tunnels (From Ref. [16]. Reprinted by permission of SAGE Publications. 2011 American Orthopaedic Society for Sports Medicine)
2.2 Results
Under a 90-N anterior force (Fig. 9.2), the ANOVA demonstrates that the anatomic SB reconstruction was significantly better than the conventional SB reconstruction (p = 0.0211) only in the range between 0 and 30° and that there were no significant differences in the other ranges of knee flexion (Table 9.1). On the other hand, the anatomic DB reconstruction was significantly better than the conventional SB reconstruction both in the range between 0 and 30° (p = 0.0027) and in the range between 35 and 70° (p = 0.0041). Under a 5-Nm internal torque (Fig. 9.3), the ANOVA demonstrates that the anatomic SB reconstruction was significantly better than the conventional SB reconstruction (p = 0.0344) only in the range between 0 and 30° (Table 9.1). On the other hand, the anatomic DB reconstruction was significantly better than the conventional SB reconstruction both in the range between 0 and 30° (p = .0268) and in the range between 35 and 70° (p = 0.0479). Under the simulated pivot shift test (Fig. 9.4), the ANOVA demonstrates that there was no significant difference between the anatomic and conventional SB reconstructions at each range of knee flexion (Table 9.1). On the other hand, the anatomic DB reconstruction was significantly better than the conventional SB reconstruction only in the range between 0 and 30° (p = 0.0259).
The difference in anterior translation from the intact knee (which is the zero-datum axis) under 90-N anterior load for the intact and ACL-reconstructed knee (mean +/− standard deviation). Values above the datum axis represent greater laxity compared with the intact behavior, and vice versa. R, reconstruction
The difference from the intact knee in tibial internal rotation under 5-Nm internal rotation torque for the ACL-reconstructed knee (mean +/− standard deviation). R, reconstruction (From Ref. [16]. Reprinted by permission of SAGE Publications. 2011 American Orthopaedic Society for Sports Medicine)
The difference in the tibial anterior translation from the intact knee during the pivot shift for the ACL-reconstructed knee (mean +/− standard deviation). ACL anterior cruciate ligament, R reconstruction (From Ref. [16]. Reprinted by permission of SAGE Publications. 2011 American Orthopaedic Society for Sports Medicine)
2.3 Discussion
The first study question was whether the effect of the anatomic SB reconstruction on the knee stability is completely identical to the effect of the anatomic DB reconstruction. The present analyses showed that the anatomic SB reconstruction was significantly better concerning the knee stability under a 90-N anterior force and a 5-Nm internal torque than the conventional SB reconstruction in a range between 0 and 30°. However, it is noted that there were no significant differences between the two reconstructions not only in the other ranges of knee flexion under these loading conditions but also in all the ranges under the simulated pivot shift test. On the other hand, the anatomic DB reconstruction was significantly better concerning the knee stability under a 90-N anterior force and a 5-Nm internal torque than the conventional SB reconstruction not only in a range between 0 and 30° but also in the range between 35 and 70°. In addition, the anatomic DB reconstruction was significantly better under the simulated pivot shift test than the conventional SB reconstruction in a range between 0 and 30°. These results showed that although both the anatomic SB and DB reconstructions were significantly better than conventional SB reconstruction, the effect of the anatomic SB reconstruction on the knee stability is not completely identical to the effect of the anatomic DB reconstruction. Namely, a significant effect of anatomic DB reconstruction on the knee laxity can be found in a wider range of knee flexion under each loading condition in comparison with the anatomic SB reconstruction. From the clinical viewpoint, the authors can say that the anatomic DB reconstruction is biomechanically superior to the anatomic SB reconstruction.
The biomechanical reason of the difference between the effects of the two anatomic reconstructions is speculated. Yamamoto et al. [22] reported that the effect of “laterally placed” SB reconstruction, in which the femoral tunnel was created at the center of the PL bundle attachment on the femur, on the knee stability was not significant in a range of knee flexion, but significant only in a range near full extension. In the anatomic SB reconstruction, the femoral tunnel was created at the center between the AM and PL bundle attachments. The distance between the two femoral tunnels created in these two reconstructions was only several millimeters. Therefore, the bundle created in anatomic SB reconstruction is considered to become slack in a range of knee flexion, although the degree of the slackness may be less than the bundle created in the “laterally placed” SB reconstruction. The complex function of the ACL results from integration of the AM and PL bundle functions. Therefore, it is considered that there is a limit in reconstructing the ACL with one bundle. Thus, this study showed that, biomechanically, the anatomic DB procedure can reconstruct the ACL function closer to the normal one than the anatomic SB procedure, at least, immediately after surgery. In the anatomic DB reconstruction, anterior tibial translations were slightly over constrained immediately after surgery. However, after ACL reconstruction, stress relaxation occurs immediately after surgery even after rigorous preconditioning [23]. This should be taken into account, independent of the type of fixation device [24, 25]. Preliminary in vivo data [9, 10, 29–31] suggest that anatomic DB reconstruction can restore normal knee kinematics, but further studies including research on anatomic SB reconstruction are required before definitive conclusions can be reached.
3 Can the Clinically Available Transtibial Anatomic DB Procedure Really Obtain Significantly Better Knee Stability in Comparison With Conventional SB Reconstruction Procedure?
3.1 Methods
A different biomechanical study was performed to compare the anatomical DB reconstruction performed with the arthroscopic transtibial procedure, which has been clinically used, with the conventional SB reconstruction procedure using eight fresh-frozen cadaveric knees [11]. These two procedures were reported in the previous clinical study [10]. The same measurement system and loading conditions as the above-described study [16] were used in this experiment. The test regimen was repeated with the knee in three further states: (1) after arthroscopic transection of the ACL, (2) after arthroscopically assisted anatomic DB ACL reconstruction, and (3) after arthroscopically assisted SB ACL reconstruction. The bone tunnels were filled with polyester resin paste.
3.2 Results
Under a 90-N anterior force, the anterior translation versus flexion curves for SB and DB reconstruction were significantly less than in the ACL-deficient knee (p < 0.0235) (Fig. 9.5). Tibial anterior translation with the DB reconstruction was a mean of 3.5 mm less than with the SB reconstruction at 20° of knee flexion, and post hoc testing found that this difference was significant at all flexion angles from 0 to 75° (p <0.0119). Under 5-Nm internal torque (Fig. 9.6), the tibial rotation with the DB reconstruction was a mean of 2.5° less than that with the SB reconstruction near knee extension. Post hoc testing showed that this was significantly less from 0 to 45° of knee flexion (p <0.0347). Significant differences were not found between the ACL-deficient knee and the SB reconstruction. Under the simulated pivot shift test (Fig. 9.7), the anterior translation versus flexion curves were significantly different among the ACL-deficient knee and the SB and DB reconstructions (p < 0.0001). The anterior translation with the DB reconstruction was significantly less than with the SB reconstruction (p = 0.0006); the post hoc tests found significant differences (p < 0.0387) at 20 and 25° of knee flexion, where the mean difference in the anterior shift was 2 mm. Thus, this study showed that anterior laxity under anterior tibial load, rotational laxity under internal tibial torque, and anterior laxity under pivot shift loading were significantly less after the anatomic DB reconstruction performed with the arthroscopic transtibial procedure, which has been clinically used, than after the conventional SB reconstruction.
The difference in anterior translation from the intact knee (which is the zero-datum axis) under 90-N anterior load for the intact, ACL-deficient, and ACL-reconstructed knee (mean +/− standard deviation). ACL anterior cruciate ligament, R reconstruction (From Ref. [11]. Reprinted by permission of SAGE Publications. 2010 American Orthopaedic Society for Sports Medicine)
The difference from the intact knee in tibial internal rotation under 5-Nm internal rotation torque for the ACL-deficient and ACL-reconstructed knee (mean +/− standard deviation). ACL anterior cruciate ligament, R reconstruction (From Ref. [11]. Reprinted by permission of SAGE Publications. 2010 American Orthopaedic Society for Sports Medicine)
The difference in the tibial anterior translation from the intact knee during the pivot shift for the ACL-deficient and ACL-reconstructed knee (mean +/− standard deviation). ACL anterior cruciate ligament, R reconstruction (From Ref. [11]. Reprinted by permission of SAGE Publications. 2010 American Orthopaedic Society for Sports Medicine)
3.3 Discussion
The second study question was whether the clinically available transtibial procedure for anatomic DB reconstruction can really obtain significantly better knee stability in comparison with the conventional SB reconstruction procedure. The anterior translation laxity in response to a 90-N anterior drawer force was significantly less after the anatomic DB reconstruction than after the SB reconstruction from 0 to 75° of knee flexion. Previous biomechanical studies have shown that the PL bundle of the intact ACL carries one-half to two-thirds of the total force in the ACL near full extension of the knee, when the knee is subjected to an anterior tibial load [8, 26, 27]. As the conventional SB reconstruction reproduces only the AM bundle, loss of the function of the natural PL bundle is considered to result in the insufficient function in the conventional SB reconstruction in the range between 0 and 75° of knee flexion. On the other hand, Yamamoto et al. [22] and Yasuda et al. [28] reported that the reconstructed PL bundle cannot restrain anterior tibial translation at flexion angles of the knee. This fact explains the similarity concerning the knee laxity between the two reconstructions: namely, only the reconstructed AM bundle stabilizes the knee near flexion position in response to anterior tibial load.
For tibial internal rotation torque, the anatomic DB reconstruction restored the tibial rotation of the ACL to the level of the intact knee, whereas the conventional SB reconstruction did not. Yasuda et al. [28] measured the AM and PL graft tensions intraoperatively and found that tension of the PL graft was increased significantly by internal rotation at 15 and 30° of knee flexion. On the other hand, a graft placed in the conventional SB reconstruction was more vertical than the two bundles placed in the anatomic DB reconstruction, so it could not effectively the knee near extension in response to 5-Nm internal rotation torque.
In the pivot shift loading, the conventional SB reconstruction allowed a “mini-pivot” to persist. In previous biomechanical and clinical studies [18, 19], it was reported that SB ACL reconstruction frequently leaves a residual mini-pivot. Woo et al. [1] reported that the SB reconstruction using the hamstring tendon graft or the bone-patella tendon-bone graft cannot completely restore the normal anterior laxity and that it is not effective for rotatory instability. In addition, kinematic studies [3, 4] demonstrated that SB reconstruction with the bone-patella tendon-bone or hamstring tendon graft did not have a significant effect on the rotatory instability during walking or more active activities. This study supported the evidence that the rotatory instability may persist after conventional SB reconstruction. Recent clinical studies [29–31] have reported that 32–49 % of the patients had a positive pivot shift, grade 1 or 2, at a few years after SB ACL reconstruction. These studies implied that clinical results for the pivot shift test after common SB reconstruction procedures may be worse than the previously expected result.
4 Clinical Relevance of These Studies
These biomechanical results cannot directly refer to selection of ACL reconstruction procedure in the clinical field, because the selection is decided from various clinical viewpoints, including not only biomechanical superiority but also surgeon’s skill, frequency of postoperative graft failure, cost of the surgery, and so on. However, one of the final goals of ACL reconstruction is the complete restoration of normal knee stability in all patients. The authors believe that the biomechanical superiority in knee stability may affect the long-term clinical results concerning postoperative meniscus damage and/or osteoarthritic changes, resulting in possible superiority in future subjective and functional evaluations. To pursue the complete restoration of normal knee stability in the long-term clinical results, it is essential to select the procedure in which the biomechanical function of the reconstructed ACL is the closest to that of the normal ACL at the time of surgery. Therefore, the authors believe that the anatomic DB reconstruction is the most effective procedure to pursue the final goal of ACL reconstruction. However, surgeons should have sufficient skill to successfully perform the anatomic double-bundle reconstruction.
References
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon: a cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am 84:907–914
Lee MC, Seong SC, Lee S et al (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23:771–778
Georgoulis AD, Ristanis S, Chouliaras V, Moraiti C, Stergiou N (2007) Tibial rotation is not restored after ACL reconstruction with a hamstring graft. Clin Orthop Relat Res 454:89–94
Tashman S, Kolowich P, Collon D, Anderson K, Anderst W (2007) Dynamic function of the ACL-reconstructed knee during running. Clin Orthop Relat Res 454:66–73
Bach JM, Hull ML, Patterson HA (1997) Direct measurement of strain in the posterolateral bundle of the anterior cruciate ligament. J Biomech 30:281–283
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22:85–89
Kurosawa H, Yamakoshi K, Yasuda K, Sasaki T (1991) Simultaneous measurement of changes in length of the cruciate ligaments during knee motion. Clin Orthop Relat Res 256:233–240
Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH (1997) In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res 15:285–293
Yasuda K, Kondo E, Ichiyama H et al (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Kondo E, Merican AM, Yasuda K, Amis AA (2010) Biomechanical comparisons of knee stability after anterior cruciate ligament reconstruction between two clinically available trans-tibial procedures: anatomic double bundle versus single bunde. Am J Sports Med 38:1349–1358
Mae T, Shino K, Miyama T et al (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy 17:708–716
Markolf KL, Park S, Jackson SR, McAllister DR (2008) Simulated pivot-shift testing with single and double bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am 90:1681–1689
Ho JY, Gardiner A, Shah V, Steiner ME (2009) Equal kinematics between central anatomic single bundle and double bundle anterior cruciate ligament reconstructions. Arthroscopy 25:464–472
Lee JK, Lee S, Seong SC, Lee MC (2014) Anatomic SB ACL reconstruction is possible with use of the modified transtibial technique: a comparison with the anteromedial transportal technique. J Bone Joint Surg Am 96:664–672
Kondo E, Merican AM, Yasuda K, Amis AA (2011) Biomechanical comparison of anatomic double-bundle, anatomic single-bundle and non-anatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39:279–288
Cuomo P, Rama KR, Bull AMJ, Amis AA (2007) The effects of different tensioning strategies on knee laxity and graft tension after double 171 bundle anterior cruciate ligament reconstruction. Am J Sports Med 35:2083–2090
Bull AMJ, Andersen HN, Basso O, Targett J, Amis AA (1999) Incidence and mechanism of the pivot shift: an in vitro study. Clin Orthop Relat Res 363:219–231
Lie DT, Bull AM, Amis AA (2007) Persistence of the mini pivot shift after anatomically placed anterior cruciate ligament reconstruction. Clin Orthop Relat Res 457:203–209
Bellier G, Christel P, Colombet P, Djian P, Franceschi JP, Sbihi A (2004) Double-stranded hamstring graft for anterior cruciate ligament reconstruction. Arthroscopy 20:890–894
Christel P, Franceschi JP, Sbihi A, Colombet P, Djian P, Bellier G (2005) Anatomic anterior cruciate ligament reconstruction: the French experience. Oper Tech Orthop 15:103–110
Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE (2004) Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med 32:1825–1832
Arnold MP, Lie DTT, Verdonschot N, de Graaf R, Amis AA, van Kampen A (2005) The remains of anterior cruciate ligament graft tension after cyclic knee motion. Am J Sports Med 33:536–542
Numazaki H, Tohyama H, Nakano H, Kikuchi S, Yasuda K (2002) The effect of initial graft tension in anterior cruciate ligament reconstruction on the mechanical behaviors of the femur-graft-tibia complex during cyclic loading. Am J Sports Med 30:800–805
Yamanaka M, Yasuda K, Tohyama H, Nakano H, Wada T (1999) The effect of cyclic displacement upon the biomechanical characteristics of anterior cruciate ligament reconstructions. Am J Sports Med 27:772–777
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Yasuda K, Ichiyama H, Kondo E, Miyatake S, Inoue M, Tanabe Y (2008) An in vivo biomechanical study on the tension-versus-knee flexion angle curves of two grafts in anatomic double-bundle anterior cruciate ligament reconstruction: effects of initial tension and internal tibial rotation. Arthroscopy 24:276–284
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single- and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res 454:108–113
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 36:1675–1687
Muneta T, Koga H, Mochizuki T et al (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Kondo, E., Yasuda, K. (2016). Biomechanics of Single- and Double-Bundle ACL Reconstruction. In: Ochi, M., Shino, K., Yasuda, K., Kurosaka, M. (eds) ACL Injury and Its Treatment. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55858-3_9
Download citation
DOI: https://doi.org/10.1007/978-4-431-55858-3_9
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55856-9
Online ISBN: 978-4-431-55858-3
eBook Packages: MedicineMedicine (R0)