Abstract
Dystonic head tremor (DHT) is characterized by head tremor associated with cervical dystonia (CD). Deep brain stimulation (DBS) can be considered when local treatment with botulinum toxin or oral medication has failed. However, there is lack of data regarding the optimal target structure for surgery in DHT.
DBS of the ventrolateral (VL) thalamus is an established treatment option for medically refractory tremor. Tremor suppression is described as being most effective when stimulating at the inferior thalamic base and within the posterior subthalamic area (PSA). Moreover, there is surgical evidence from the pre-DBS era that both lesions and high-frequency stimulation of the PSA improve CD. Based on these observations, we performed DBS in three patients with DHT, placing the proximal contacts of the electrodes into the inferior base of VL thalamic nuclei and the distal contacts into the adjacent PSA. Chronic stimulation improved not only head tremor but also CD. These findings suggest that DBS at the base of VL thalamus and the adjacent PSA should undergo further investigation as a potential target for patients with DHT.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
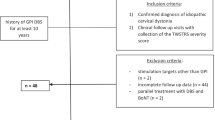
Dystonic head tremor (DHT) describes head tremor in patients with primary cervical dystonia (CD) [3, 4, 25]. DHT is found in 68 % of CD patients [22], and is less responsive to oral pharmacotherapy than hand tremor [6]. Local injections of botulinum toxin often improve not only CD but also tremor, but in some cases deep brain stimulation (DBS) might be considered. It is suggested that treatment of dystonic tremor matches the treatment of dystonia [6, 24], i.e., pallidal stimulation, although results in patients with DHT are conflicting and limited to case reports. We [18] and others [28] have reported on successful stimulation of the globus pallidus, pars interna (GPi) in single patients with DHT. In contrast, DHT was refractory to GPi stimulation in two other cases [16, 19].
We report on three patients with medically refractory DHT who underwent stereotactic implantation of quadropolar DBS electrodes. We aimed to place the upper contacts of the DBS lead at the base of the ventrolateral (VL) thalamus, and the lower contacts within the adjacent posterior subthalamic area (PSA). Our decision was driven by reports on excellent tremor suppression of different etiology by DBS at the VL thalamic base and within the PSA [8, 10], and relief of cervical dystonia by lesioning [17, 20, 21] and early explorative DBS [20] within the PSA.
Case histories, stereotactic localization of the most effective contacts, and clinical outcome are described, and results are discussed.
Patients and Methods
Patients
CD was rated according to the Toronto Western Spasmodic Torticollis Rating Scale, Part I — Torticollis Severity Scale (TWSTRS (I), maximal 35 points). Head tremor was evaluated on the basis of the Fahn–Tolosa–Marin Tremor Rating scale, Part A, subitem 4: head tremor at rest (lying down), posture (when sitting or standing) and action (when turning); severity rating: 0 = none, 1 = slight; barely perceivable, 2 = moderate, may be intermittent, 3 = marked, 4 = severe (TRS (A) head, maximal 12 points). Clinical data of individual patients are summarized in Table 1.
Surgical Procedure
All patients described here underwent stereotactic bilateral implantation of DBS electrodes into the inferior base of VL thalamus and adjacent PSA. Operative interventions were performed in local anaesthesia as described previously [7, 18]. The surgical target was defined 6–7 mm posterior and 12.5–13.5 mm lateral to the midcommissural point. Surgery included simultaneous microrecordings from 2 to 3 microelectrodes (MicroGuide, Alpha–Omega, Nazareth, Israel) in steps of 250–500 μm using a Ben’s gun approach to map kinetic and tremor-related cells and the inferior border of the thalamus. Macrostimulation via the uninsulated distal end of the guide tube was performed intraoperatively to identify the trajectory resulting in most effective tremor suppression which was associated with the least adverse effects. We intended to position at least two contacts of the quadropolar 3389 electrodes (Medtronic Inc. Minneapolis, MN, USA) within the PSA. At the end of the operative procedure, both DBS electrodes were test-stimulated to assess side-effects. Tremor had subsided in most cases due to a microlesioning effect and could not be assessed further. Stimulator implantation (model Kinetra or PC, Medtronic Inc.) was performed in general anaesthesia on the same day or on the day following electrode implantation.
We employed intraoperative computerized tomography scanning (CT, Siemens Somatom with sliding-gantry system, Erlangen, Germany) to determine the position of the implanted electrodes. Stereotactic CT images (1 mm slice thickness; window center 80 HU, ‘width’ 95–100 HU; matrix 512 × 512 pixel; FOV 280 mm) covering the distal >30 mm of the implanted electrodes were obtained while the stereotactic frame (Zamorano-Dujovny; Stryker-Leibinger, Freiburg, Germany) was left in place. The postoperative CT scans were co-registered with preoperative CT and magnetic resonance images (MRI).
Results
All patients had inconspicuous family history for tremor and dystonia. Tremor was in part relieved by alcohol in cases 1 and 3. Preoperatively, treatment with oral medication and electromyography (EMG)-guided local botulinum toxin injections up to occurrence of side-effects was largely ineffective. MRI was inconspicuous in all patients.
Following bilateral electrode implantation into the base of VL thalamus and adjacent PSA, chronic stimulation improved tremor and cervical dystonia in all cases. Coordinates of clinically effective electrode contacts and programming parameters are provided in Table 2. The following section contains the detailed case presentations.
Case 1
This 39-year-old male patient presented with a 26-year history of initial arm tremor followed by head twisting and trembling. On examination, he had DHT (CD with torti- and laterocollis to the left) with a positive geste antagonistique associated with an irregular, kinetic head tremor (mainly ‘yes–yes’ direction) and a position-specific severe jerky component when leaning the head backwards. Furthermore, he had mild dysarthria and a slight and not disabling action tremor of both hands (TWSTRS (I) 8 points, TRS (A) head 6 points; Table 1). Surface EMG of right sternocleidomastoid and upper trapezius muscles showed a mixture of regular and irregular bursts with a duration of 100 ms or longer. Epsilon sarcoglycan gene mutation was negative. Postoperatively dysarthria and CD were unchanged. Microlesioning resulted in a complete cessation of the tremulous head motion, which lasted up to 16 days. Consequently, the head tremor progressively re-appeared. Monopolar stimulation performed bilaterally with the second most distal contacts (i.e., contacts 1- and 9- cathodal vs case + anode) improved symptoms markedly (TWSTRS (I) 1 points, TRS (A) head 2 points), but induced a slight increase of dysarthria and imbalance. Therefore, 3 months postoperatively the active contacts were changed bilaterally to the second most proximal contacts (contacts 2- and 10-; Table 2). Stimulation in the left hemisphere was continued in the PSA; however, stimulation on the right side was at the base of the thalamus (Table 2). This resulted in lasting improvement of DHT without side-effects for more than 20 months. Whereas tremor immediately improved after the initiation of stimulation, CD improved progressively over a time period of 3–5 months.
Case 2
This 66-year-old female patient presented with a 10-year history of head trembling and involuntary turning of the head to the right. On examination, she had mild and intermittent right torticollis and a slight lateral shift to the left associated with an irregular and position specific 4–5 Hz DHT (predominantly ‘yes–yes’ direction). Both abnormal head posture and DHT were improved by touching the chin with one finger. Holding the arms straight forward, a slight dystonic finger posture on the left was present (TWSTRS (I) 7 points, TRS (A) head 5 points).
In contrast to the other patients, postoperatively no relevant microlesioning effect could be observed. Permanent monopolar stimulation of contacts ‘2’ and ‘9’ was performed at the thalamic base on both sides (Table 2). Stimulation through the more distal contacts also resulted in efficient tremor suppression, but induced disturbing dysarthria. Tremor improved within a few days after initiation of stimulation, CD within the first 3 months. Best results were seen with stimulation at the VL thalamic base on both sides (Table 2). Clinical improvement was stable, and was rated after18 months (TWSTRS (I) 2 points, TRS head (A) 2 points; Table 1).
Case 3
This 54-year-old male patient presented with head tremor started 16 years ago, followed by involuntary head turning 2–3 years later. Slight bilateral postural hand tremor appeared 2 years prior to surgery. On examination, he had mild torticollis to the left (30°) and mild laterocollis to the right (15°) and moderate to severe slightly irregular and position specific DHT of high frequency (6–8 Hz) but low amplitude (exclusively ‘no–no’ direction). Geste antagonistique was positive for both abnormal head posture and DHT. Additionally, a postural arm tremor of rather high frequency and low amplitude without intention tremor was present (TWSTRS (I) 10 points, TRS head (A) 8 points). Permanent monopolar stimulation of the second most distal contacts ‘1’ and ‘9’, located in the PSA, proved to be most effective and without adverse effects (Table 2). CD and DHT showed stable improvement as documented 13 months postoperatively (TWSTRS (I) 4 points, TRS (A) head 3; Table 2).
Discussion
Classification of head tremor associated with CD is not unambiguous [3, 25]. The patients reported here all presented with both CD and associated head tremor, and their condition was classified as dystonic head tremor [3, 4, 25]. Diagnosis of DHT is supported by reduction of head tremor amplitude during a geste antagonistique maneuver [5, 12] and presence of a neck position-specific tremor component or a jerky, irregular tremor [3, 13] with rhythmic expression of rapid dystonic movements. As observed in two of our patients, tremor relief through alcohol can not only be seen in essential tremor but also in DHT [12].
Selection of the DBS target in DHT is mainly driven by individual characteristics of the dystonic tremor rather than based on clear-cut clinical disease classification. Furthermore, there is lack of clinical studies comparing the efficacy of potential targets for DHT, i.e., VL thalamus, PSA and GPi. We decided to place the electrodes with the lower contacts within the PSA and the upper contacts at the base of VL thalamus as delineated by intraoperative microelectrode recordings. In all our three DHT patients, bilateral DBS did not only improve tremor but also CD. Stereotactic localization demonstrated an even distribution of clinically effective electrode contacts between VL thalamus and PSA (Table 2). The stereotactic coordinates of the electrodes implanted are presented in Table 2.
Two recent case series documented successful thalamic DBS in two [27] and three [19] patients with severe dystonic tremor, two of them with DHT [19]. In addition, stimulation of structures within the PSA have been reported to improve various dystonic tremor syndromes [1, 14, 23], including one case with symptomatic DHT after perinatal anoxia [14]. In one case, bilateral DBS of the subthalamic nucleus has been reported to completely suppress tremor and nearly resolve CD in a patient with DHT and action tremor of the hands [2]. However, the localization of the active electrode contacts was not reported.
The PSA is an anisotropic region in which different systems intersect. Whereas cerebellothalamic projections within the PSA may represent the relevant substrate for the surgical relief of tremor, modulation of pallidofugal fibres within the PSA may bring out the beneficial effects on dystonic symptoms. Pallidofugal fibres of the ansa lenticularis and the lenticular fasciculus (Forel’s field H2) join in Forel’s field H before entering the thalamus in Forel’s field H1 [15, 26]. Within the PSA, the zona incerta (ZI) conveys afferents from the interstitial nucleus of Cajal. It has been known for a long time that stimulation of this nucleus as well as stimulation within the ZI may induce head rotation in animals [9, 11]. Moreover the ZI receives afferents from GPi and substantia nigra, pars reticulata and sends efferents to the ventroanterior and VL thalamic nuclei (overview in [23]).
Taken together, the intricate anatomical relationships at the thalamic base with its high density of different fiber systems and interconnected nuclei put any operative intervention in the thalamic base/PSA border zone in the position of “bottle-neck surgery”. Along with this, we found the most effective and therefore active electrodes for tremor and dystonia relief to be located in the VL thalamic base (n = 3) as well as in the adjacent PSA (n = 3). So the “bottle-neck” approach may help to explain the efficacy of the PSA as surgical target in a variety of disease entities, such as different tremors, Parkinson’s disease and dystonia.
General conclusions from this case series are limited due to the small sample size. Hitherto, reports on DBS in patients with DHT have been rare. Patients reported here expressed relatively more tremor than dystonia. Therefore effects of DBS in the VL thalamic base/PSA in DHT patients with more severe dystonic symptoms remain to be evaluated. A prospective and controlled study with separate investigations of all contacts on tremor and dystonia in a blinded fashion is desirable.
References
Blomstedt P, Sandvik U, Tisch S (2010) Deep brain stimulation in the posterior subthalamic area in the treatment of essential tremor. Mov Disord 25(10):1350–1356
Chou KL, Hurtig HI, Jaggi JL, Baltuch GH (2005) Bilateral subthalamic nucleus deep brain stimulation in a patient with cervical dystonia and essential tremor. Mov Disord 20(3):377–380
Deuschl G (2003) Dystonic tremor. Rev Neurol (Paris) 159(10 Pt 1):900–905
Deuschl G, Bain P, Brin M (1998) Consensus statement of the Movement Disorder Society on Tremor. Ad Hoc Scientific Committee. Mov Disord 13(Suppl 3):2–23
Deuschl G, Heinen F, Kleedorfer B, Wagner M, Lucking CH, Poewe W (1992) Clinical and polymyographic investigation of spasmodic torticollis. J Neurol 239(1):9–15
Gironell A, Kulisevsky J (2009) Diagnosis and management of essential tremor and dystonic tremor. Ther Adv Neurol Disord 2(4):215–222
Hamel W, Fietzek U, Morsnowski A, Schrader B, Herzog J, Weinert D, Pfister G, Muller D, Volkmann J, Deuschl G, Mehdorn HM (2003) Deep brain stimulation of the subthalamic nucleus in Parkinson’s disease: evaluation of active electrode contacts. J Neurol Neurosurg Psychiatry 74(8):1036–1046
Hamel W, Herzog J, Kopper F, Pinsker M, Weinert D, Muller D, Krack P, Deuschl G, Mehdorn HM (2007) Deep brain stimulation in the subthalamic area is more effective than nucleus ventralis intermedius stimulation for bilateral intention tremor. Acta Neurochir (Wien) 149(8):749–758
Hassler R (1954) Experimentelle und anatomische Befunde über die Drehbewegungen und ihre nervösen Apparate. Arch Psychiat Nervenkr 192:488–526
Hassler R (1965) Correlations between clinical and autoptic findings in stereotaxic operations of parkinsonism. Confin Neurol 26:282–290
Hyde JE, Toczek S (1962) Functional relation of interstitial nucleus to rotatory movements evoked from zona incerta stimulation. J Neurophysiol 25:455–466
Jankovic J, Leder S, Warner D, Schwartz K (1991) Cervical dystonia: clinical findings and associated movement disorders. Neurology 41(7):1088–1091
Jedynak CP, Bonnet AM, Agid Y (1991) Tremor and idiopathic dystonia. Mov Disord 6(3):230–236
Jeong SG, Lee MK, Lee WH, Ghang CG (2009) Deep brain stimulation of the subthalamic area for dystonic tremor. J Korean Neurosurg Soc 45(5):303–305
Jones EG (1985) The thalamus. Plenum Press, New York
Krause M, Fogel W, Kloss M, Rasche D, Volkmann J, Tronnier V (2004) Pallidal stimulation for dystonia. Neurosurgery 55(6):1361–1368
Moll CK, Hamel W, Ostertag CB, Muller D, Finsterbusch J, Engel AK, Munchau A (2008) Subthalamotomy in cervical dystonia: a case study of lesion location and clinical outcome. Mov Disord 23(12):1751–1756
Moll CK, Sharott A, Hamel W, Munchau A, Buhmann C, Hidding U, Zittel S, Westphal M, Muller D, Engel AK (2009) Waking up the brain: a case study of stimulation-induced wakeful unawareness during anaesthesia. Prog Brain Res 177:125–145
Morishita T, Foote KD, Haq IU, Zeilman P, Jacobson CE, Okun MS (2010) Should we consider Vim thalamic deep brain stimulation for select cases of severe refractory dystonic tremor. Stereotact Funct Neurosurg 88(2):98–104
Mundinger F (1977) New stereotactic treatment of spasmodic torticollis with a brain stimulation system (author’s transl). Med Klin 72(46):1982–1986
Mundinger F, Riechert T, Disselhoff J (1972) Long-term results of stereotactic treatment of spasmodic torticollis. Confin Neurol 34(2):41–50
Pal PK, Samii A, Schulzer M, Mak E, Tsui JK (2000) Head tremor in cervical dystonia. Can J Neurol Sci 27(2):137–142
Plaha P, Khan S, Gill SS (2008) Bilateral stimulation of the caudal zona incerta nucleus for tremor control. J Neurol Neurosurg Psychiatry 79(5):504–513
Raethjen J (2011) Current therapy for tremor. Aktuelle Neurol 38(6):315–319
Rivest J, Marsden CD (1990) Trunk and head tremor as isolated manifestations of dystonia. Mov Disord 5(1):60–65
von Monakow C (1895) Experimentelle und pathologisch-anatomische Untersuchungen über die Haubenregion, den Sehhügel und die Regio subthalamica, nebst Beiträgen zur Kenntnis früh erworbener Gross und Kleinhirndefecte. Arch Psychiatr Nervenkr 27:1–128, 386–478
Woehrle JC, Blahak C, Kekelia K, Capelle HH, Baezner H, Grips E, Weigel R, Krauss JK (2009) Chronic deep brain stimulation for segmental dystonia. Stereotact Funct Neurosurg 87(6):379–384
Yianni J, Nandi D, Hyam J, Elliott V, Bain P, Gregory R, Aziz T (2004) Failure of chronic pallidal stimulation in dystonic patients is a medical emergency. Neuromodulation 7(1):9–12
Financial Disclosure and Potential Conflict of Interest
The authors have occasionally received travel expenses and honoraria from Medtronic Inc. for speaking at meetings.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this paper
Cite this paper
Buhmann, C., Moll, C.K.E., Zittel, S., Münchau, A., Engel, A.K., Hamel, W. (2013). Deep Brain Stimulation of the Ventrolateral Thalamic Base and Posterior Subthalamic Area in Dystonic Head Tremor. In: Nikkhah, G., Pinsker, M. (eds) Stereotactic and Functional Neurosurgery. Acta Neurochirurgica Supplement, vol 117. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1482-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1482-7_11
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1481-0
Online ISBN: 978-3-7091-1482-7
eBook Packages: MedicineMedicine (R0)