Abstract
Fat necrosis is a benign inflammatory condition of the adipose tissue that can commonly affect the hypodermis. The usage of imaging in fat necrosis may support the clinical diagnosis especially when lumps or bumps are found on clinical examination or the differential diagnosis with a malignant entity should be performed. This chapter discusses the application of common imaging modalities, its general principles, indications, advantages, and disadvantages.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Gadolinium Contrast Medium
- Posterior Acoustic Enhancement
- Focal Asymmetry
- Hypoechoic Halo
- Nuclear Imaging Modality
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Fat necrosis is a benign non-suppurative inflammatory entity of the adipose tissue that results from the aseptic saponification of lipids by enzymes. The reported causes include trauma, radiotherapy, anticoagulation, inflammatory diseases, surgery, percutaneous interventions, and perinatal asphyxia, hypoxemia, or hypothermia [1]. Imaging has been growingly used for studying fat necrosis due to the often variable history and clinical findings that can simulate other conditions which includes the differential diagnosis of palpable lumps and bumps when this entity affects the hypodermis. Additionally, patients may not spontaneously refer an inciting event such as trauma. Reports on imaging of fat necrosis started with the usage of X-rays, such as mammography, and have expanded to other imaging modalities such as ultrasound, MRI (magnetic resonance imaging), and most recently PET-CT (positron emission tomography-computed tomography). Besides the support to the clinical diagnosis, the usage of these imaging techniques may provide an anatomic perspective for evaluating the extent and characteristics of the structural changes in the tissues, as well as a support for assessing the differential diagnosis.
The aim of this chapter is to focus on the imaging characteristics of hypodermal fat necrosis with different imaging modalities and discuss some general principles, indications, advantages, and disadvantages for each method.
2 Imaging Methods
2.1 X-Rays Mammography
X-rays are the most simple and accessible form of imaging study and involve the usage of low dose radiation for diagnostic purposes. Usually, this modality is not intended for particular study of fat necrosis; however, there are radiological signs suggestive of this condition that are frequently and incidentally found in the hypodermis, commonly during mammography screenings. The most frequent mammographic characteristic of fat necrosis is the presence of round- or oval-shaped hypodense structures, frequently showing a hyperdense calcified rim, also called “egg-shell”- or “rim-like”-type calcification that corresponds to calcified lipid cysts (Fig. 4.1). This sign is almost pathognomonic of fat necrosis; therefore, the patients presenting this feature may not need additional imaging studies and should continue with the recommended screening program according to their age and history. Less frequent forms of presentation of fat necrosis on mammography include focal asymmetries that may imply parenchymal edema. However, microcalcifications or spiculated dense masses can also be detected, the latter being related to a major presence of fibrosis or scarring [2, 3]. Since these occasionally seen mammographic signs may mimic a breast malignancy, more imaging studies are usually needed in these particular cases.
2.2 Ultrasound
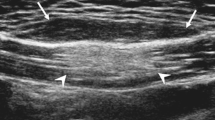
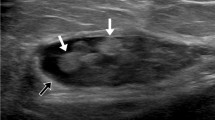
Also called sonography, this widely available imaging method is based on the properties of sound waves and has been increasingly used for studying fat necrosis in soft tissues due to the high definition images of the superficial layers provided by the current machines. Besides its non-radiating nature and proved safety characteristics, there are several advantages of ultrasound such as its real time, 2D and 3D multiaxial and dynamic performance, as well as its reasonable balance between resolution and penetration that allow us to obtain a wide range of anatomical information that can reach from the skin layers to the bony margin. Also, ultrasound can show the vascularity of the tissues through its color or power Doppler capabilities which includes the detection of the type of vessel (arterial or venous) and the velocity of blood flow (cm/s) [4, 5]. This may avoid the adverse reactions due to the use of contrast media that have been widely reported with other imaging modalities such as CT or MRI. The current limitations of ultrasound are lesions that measure <0.1 mm, with only epidermal location, and the detection of pigments such as melanin [6]. These last two limitations are not relevant for the study of fat necrosis. In fact, the hypodermis seems to be a perfect target for ultrasound use, due to its anatomically superficial location in soft tissue that makes it easily accessible with most of the linear probes that work with frequencies ≥7.5 MHz. Nevertheless, probes working with higher frequencies (≥12 MHz) are most commonly recommended for studying the hypodermis due to their higher definition at this tissue depth. On ultrasound, the most common sign of fat necrosis is the presence of well-defined round or oval-shaped anechoic pseudocystic structures, frequently with posterior acoustic enhancement, and sometimes surrounded by a hyperechoic calcified rim. These pseudocystic structures correspond to the oily cysts produced by the liquefaction of the fatty tissue. Internal echoes and a fluid–fluid level may sometimes be recognized in these pseudocysts, usually in cases with history of trauma where the serohematic material combines with the liquefied material of the fatty lobules. Also, increased echogenicity of the hypodermis and isoechoic pseudonodules, surrounded by an anechoic or hypoechoic halo, may be detected. These latter ultrasound features indicate the degree of hypodermal inflammation. Less frequent sonographic signs are anechoic masses with a posterior acoustic shadowing artifact due to gross calcification and well- or ill-defined hypoechoic solid pseudo-masses due to prominent fibrosis and scarring. All these characteristics may appear as single or combined features in the affected region (Figs. 4.2 and 4.3). Hypo- or hypervascularity in the hypodermis may be detected according to the level of inflammation present in the tissue, hypervascularity being the most commonly found in inflamed stages [1, 3, 7]. In cases presenting subcutaneous fat necrosis of the newborn, ultrasound has been reported to successfully support the diagnosis [8–10]. Thus, the main indications for ultrasound in fat necrosis are to support the early diagnosis and rule out solid tumors that may be hard to differentiate on a clinical basis only.
2.3 Magnetic Resonance Imaging
This is an imaging method based on the response of the body’s hydrogen ions in a magnetic field. This technique has been widely used in the study of soft tissues, mainly in the musculoskeletal field, due to its high definition anatomical images. The main disadvantages of this method are its high cost and the potential adverse reactions to gadolinium, the usual contrast medium used in these examinations. Additionally, MRI has limited ability to show small calcifications, a common finding in fat necrosis which may be seen in this imaging technique as areas of signal void or may simply go undetected. On MRI, a wide spectrum of findings has been reported in fat necrosis and some of the findings may even mimic a malignant tumor such as a breast cancer. The most typical finding on MRI is a round or oval nodule or mass with hypointense T1-weighted signal on fat-saturated images that correspond to a lipid pseudocyst. Also, fat necrosis can show as well- or ill-defined isointense or hypointense areas or pseudonodules on T1-weighted images probably due to its inflammatory and hemorrhagic characteristics. In case with strong fibrosis, architectural distortion, with or without spiculated margins, and variable degrees of intensity (low, intermediate, or high signal) on T1-weighted images are reported. Fat suppression sequences may help to differentiate fat necrosis from malignant tumors. On T2-weighted sequences, isointense, hypointense, and hyperintense appearances have been described. Pseudonodular, globular, and laminated appearances have been additionally reported (Fig. 4.4). After the injection of gadolinium contrast medium, fat necrosis can show variable appearances that can range from no enhancement to irregular or peripheral enhancement and from thin to thick rims of enhancement [1–3, 7, 11, 12]. The most frequent indications for MRI regarding fat necrosis are to complete the imaging study in cases with mammographic abnormalities, especially the ones where a malignancy must be ruled out, and to assess the differential diagnosis in cases presenting palpable large lumps or extensive trauma.
(a, b). Fat necrosis on MRI (axial views). (a) T1-weighted sequence shows isointense pseudonodule with a hypointense rim located in the hypodermis of the right side of the lower back (arrow, fat necrosis area). In the vicinity, a hypointense oval-shaped hypodermal structure is detected that corresponds to a hematoma (hm). (b) T2-weighted image of the same case shows a change in the intensity of the hematoma (hm) with a fluid–fluid level (hyperintense/hypointense) and no change in the intensity of the pseudonodule (arrow, fat necrosis site) in comparison with the T1-weighted sequence (Courtesy of Drs. Raul Valenzuela and Herly Pulgar)
2.4 Computed Tomography and Positron Emission Tomography
Computed tomography (CT) implies the cross-sectional usage of X-rays and has a broad range of applications, mainly in the neurological, cardiac, and abdominal fields. Thus, CT has been extensively used for staging malignant conditions. However, there are few reports in literature on the usage of CT for studying hypodermal fat necrosis, mostly showing isolated case reports. Advantages of CT are its wide availability and relatively short time of examination due to the new multi-slice machines that can acquire and process the images very rapidly. Disadvantages of CT are its high cost, its radiating nature, and the need for intravenous contrast media. On CT, fat necrosis has been reported as a well-defined hypodense mass with rim enhancement or a globular mass with central fat density [11].
Positron emission tomography (PET) is a nuclear imaging modality that registers the gamma rays emitted by a positron emitting radionuclide, also called tracer. The most commonly used tracer is fluorodeoxyglucose (FDG), an analog of glucose. However, this is a radiating modality that also requires injection of an agent.
In recent years the combination of these two modalities (PET-CT) has gained adepts due to the mix of the anatomical and biological images that have been widely used in the staging of cancerous lesions [13]. However, PET-CT has certain notable shortcomings, including the inability to perform simultaneous data acquisition and the significant radiation dose to the patient [14]. PET-CT is now used in the staging of melanoma, showing high sensitivity especially in advanced stages [15, 16]. Nevertheless, there are several reports of false positives of PET-CT due to the glycolytic activity present in inflammation that can easily mimic a malignancy in this modality [17–19]. These inflammatory features are common in fat necrosis; therefore, this condition seems to be one of the most common pitfalls for PET-CT. These reports mention pseudonodular solid images with hypermetabolic activity and increased uptake of FDG (Fig. 4.5). Besides fat necrosis, other causes of false positives of PET-CT have been reported. Among them are acute and chronic inflammation or infection, physiologic lactation, benign breast masses, including silicone granuloma, fibroadenoma, and postsurgical or radiotherapy changes. Therefore, the usage of PET-CT is not recommended as a first imaging modality in fat necrosis. Moreover, the usage of this imaging modality may cause diagnostic dilemmas in oncologic imaging [20].
(a, b) Fat necrosis on 3D ultrasound and PET-CT. Patient with history of removed in situ melanoma in the left leg. (a) 3D ultrasound (gray scale, 5–8 s reconstruction, longitudinal view) shows two anechoic pseudocysts (*) surrounded a hyperechoic pseudonodular structure (o) consistent with fat necrosis. (b) PET-CT (coronal view) demonstrates a false-positive uptake of FDG in the hypodermis of the left thigh with two hypermetabolic pseudonodules (arrows). Abbreviations: d dermis, h hypodermis (PET-CT image courtesy of Dr. Vicky Roizen)
3 Conclusion
There are several imaging methods that can reveal the anatomical characteristics of hypodermal fat necrosis. The usage of imaging in this condition is intended for the assessment of the differential diagnosis of lumps and bumps in the soft tissues, also to try to rule out malignant tumors. The advantages and disadvantages of each technique as well as the availability of these modalities in the medical institutions should be considered, when selecting the appropriate imaging modality for each case.
References
Atasoy MM, Oren NC, Ilica AT, Güvenç I, Günal A, Mossa-Basha M. Sonography of fat necrosis of the breast: correlation with mammography and MR imaging. J Clin Ultrasound. 2013;41(7):415–23. doi:10.1002/jcu.22061.
Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192:815–25.
Tan PH, Lai LM, Carrington EV, et al. Fat necrosis of the breast – a review. Breast. 2006;15:313–8.
Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012;31:97–111.
Wortsman X. Ultrasound in dermatology: why, how, and when? Semin Ultrasound CT MR. 2013;34:177–95.
Wortsman X, Wortsman J. Clinical usefulness of variable-frequency ultrasound in localized lesions of the skin. J Am Acad Dermatol. 2010;62:247–56.
Walsh M, Jacobson JA, Kim SM, Lucas DR, Morag Y, Fessell DP. Sonography of fat necrosis involving the extremity and torso with magnetic resonance imaging and histologic correlation. J Ultrasound Med. 2008;27:1751–7.
Marszałek A, Maciejewska J, Bowszyc-Dmochowska M, Prokurat A. Subcutaneous fat necrosis of the newborn – a case report and review of literature. Pol J Pathol. 2010;61:240–4.
Vasireddy S, Long SD, Sacheti B, Mayforth RD. MRI and US findings of subcutaneous fat necrosis of the newborn. Pediatr Radiol. 2009;39:73–6.
Avayú E, Rodríguez C, Wortsman X, et al. Newborn fat necrosis: case-report. Rev Chil Pediatr. 2009;80:60–4.
Chan LP, Gee R, Keogh C, Munk PL. Imaging features of fat necrosis. AJR Am J Roentgenol. 2003;181:955–9.
Daly CP, Jaeger B, Sill DS. Variable appearances of fat necrosis on breast MRI. AJR Am J Roentgenol. 2008;191:1374–80.
Bockisch A, Beyer T, Antoch G, et al. Positron emission tomography/computed tomography – imaging protocols, artifacts, and pitfalls. Mol Imaging Biol. 2004;6:188–99.
Pichler BJ, Wehrl HF, Kolb A, Judenhofer MS. Positron emission tomography/magnetic resonance imaging: the next generation of multimodality imaging? Semin Nucl Med. 2008;38:199–208.
Schröer-Günther MA, Wolff RF, Westwood ME, et al. F-18-fluoro-2-deoxyglucose positron emission tomography (PET) and PET/computed tomography imaging in primary staging of patients with malignant melanoma: a systematic review. Syst Rev. 2012;1:62. doi:10.1186/2046-4053-1-62.
Hinz T, Voth H, Ahmadzadehfar H, et al. Role of high-resolution ultrasound and PET/CT imaging for preoperative characterization of sentinel lymph nodes in cutaneous melanoma. Ultrasound Med Biol. 2013;39:30–6.
Kashyap R, Lau E, George A, et al. High FDG activity in focal fat necrosis: a pitfall in interpretation of posttreatment PET/CT in patients with non-Hodgkin lymphoma. Eur J Nucl Med Mol Imaging. 2013;40(9):1330–6.
Akkas BE, Ucmak Vural G. Fat necrosis may mimic local recurrence of breast cancer in FDG PET/CT. Rev Esp Med Nucl Imagen Mol. 2013;32:105–6.
Lee SA, Chung HW, Cho KJ, et al. Encapsulated fat necrosis mimicking subcutaneous liposarcoma: radiologic findings on MR, PET-CT, and US imaging. Skeletal Radiol. 2013;42(10):1465–70.
Adejolu M, Huo L, Rohren E, Santiago L, Yang WT. False-positive lesions mimicking breast cancer on FDG PET and PET/CT. AJR Am J Roentgenol. 2012;198:W304–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Wien
About this chapter
Cite this chapter
Wortsman, X. (2015). Imaging of Hypodermal Fat Necrosis. In: Téot, L., Meaume, S., Akita, S., Ennis, W.J., del Marmol, V. (eds) Skin Necrosis. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1241-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1241-0_4
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1240-3
Online ISBN: 978-3-7091-1241-0
eBook Packages: MedicineMedicine (R0)