Abstract
Preclinical studies demonstrated that stem cell administration ameliorates the functional loss observed after ischemia, making stem cell transplantation an attractive approach to restore brain function after stroke in humans. Intra-arterial delivery of stem cells may offer advantages over intravenous or direct implant, such as the presence of a larger amount of stem cells in the ischemic and peri-ischemic area and the bypassing of a possible filter and retention in the peripheral organs. A shortcoming of this technique is the fact that it is an invasive procedure carrying a small, but non-negligible, risk of complications (e.g., brain ischemia). The necessity of the patency of the extra and intracranial circulation and the use of contrast are other limitations. We summarize five pilot trials using intra-arterial delivery of stem cell in patients with ischemic stroke. The limited data available comparing intra-arterial and intravenous stem cell routes in humans suggests a slightly greater relative uptake of 99-Technecium-marked cells in the cerebral hemisphere ipsilateral to the ischemia in the intra-arterial group. However, it is not known whether these results translate into clinical benefit. Larger trials are necessary to establish the efficacy of this approach.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ischemic Stroke
- Middle Cerebral Artery
- Middle Cerebral Artery Infarction
- Complete Middle Cerebral Artery
- Stem Cell Administration
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
In recent years, several studies have investigated the potential neuroprotective and restorative role of stem cells from different sources in animal models of brain ischemia (Mendez-Otero et al. 2007; Bliss et al. 2010; Hess and Hill 2011). Although the mechanisms of action are still unclear, most of these studies demonstrated that stem cell administration ameliorates the functional loss observed after ischemia, making stem cell transplantation an attractive approach to restore brain function after stroke in humans.
To date, only a few clinical studies evaluated stem cell transplantation in stroke patients. In most of these, stem cells were administered by intravenous (IV) route (Bang et al. 2005; Lee et al. 2010; Honmou et al. 2011; Savitz et al. 2011) or stereotactic surgery (Kondziolka et al. 2000; 2005; Savitz et al. 2005; Suarez-Monteagudo et al. 2009), and stem cells from different sources were used in different times after the stroke which makes comparisons among them difficult.
The aim of this chapter is to review the pilot trials of stem cells administered via intra-arterial (IA) route in patients with ischemic stroke and to discuss the advantages and shortcomings of this approach.
2 Advantages of the Intra-arterial Route
There are scarce data from preclinical and pilot trials in humans to support one route of administration over the others, for example, IA administration over IV route or direct implant (stereotactic surgery) in ischemic stroke. Moreover, the extrapolation of data acquired from the experience with other therapeutic modalities (e.g., thrombolysis) is complex and cannot directly be translated to cell therapies.
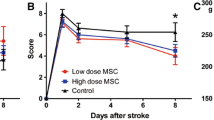
Over the past 10 years, the safety and exequibility of IA cell delivery has been investigated in patients with cardiac and peripheral vascular disease, and in most of them no significant adverse events attributed to the cell infusion were reported (Misra et al. 2012). The most important theoretical advantage of the IA route is the larger amount of stem cells in the ischemic and peri-ischemic area after direct injection in the affected artery rather than in the peripheral vein. Studies of thrombolytic therapy for ischemic stroke suggest that IA thrombolysis may be more effective than IV to recanalize large vessels, due to the higher amount of the thrombolytic drug in direct contact with the thrombus when the IA route is used (Mattle et al. 2008). However, when it refers to the delivery and homing of stem cells, the issue is disputable. In animal models, while Kamiya et al. (2008) reported that IA delivery led to a greater brain homing and functional progress in comparison to IV infusion in a model of transient ischemia, Vasconcelos-dos-Santos and collaborators (2012) found that both the IA and IV injections promoted comparable functional improvement with low and similar brain homing in a model of permanent ischemia. Moreover, different groups suggested that the effect of cell therapy in stroke may not be directly related to the presence of cells in the brain, since it was possible to observe functional recovery without the presence of cells in the cerebral parenchyma (Borlongan et al. 2004) or with very few cells present, as shown in studies using different types of cells after IA or IV administration (Bacigaluppi et al. 2009; Brenneman et al. 2010; Gao et al. 2001). To explain these results, it was suggested that the injected cells independent of the route could produce and release trophic factors such as brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), and vascular endothelial growth factor (VEGF). These factors could cross the blood–brain barrier and promote the beneficial effects observed in these animals (Borlongan et al. 2004).
In addition, it has been postulated that the trapping of the cells in the lung after IV injection (“the lung barrier”) could represent a disadvantage of the IV over IA therapy since the number of cells reaching the brain would be decreased in this case. IA administration bypasses the filter of the peripheral organs including the lungs and directs most of the injected cells into the ischemic tissue. The increase in cell trapping in the lungs after IV injections was actually demonstrated in studies in animal models, which showed a greater uptake in the lungs when this route was compared with IA (Schrepfer et al. 2007). However, it is important to note that different cell types might behave differently in respect to the lungs. For example, a study in normal rats using different cell types found that bone marrow mononuclear cells (BMMCs) passage was 30-fold greater when compared to mesenchymal stem cells (MSCs) and the differences in cell trapping were attributed to the smaller size of the BMMCs when compared to the MSCs and to differences in the adhesion capabilities of both cell types (Fischer et al. 2009). On the other hand, while pulmonary activity may be seen as a negative factor because cells reach the arterial circulation in smaller proportions, it should be noted that studies in an animal model of myocardial infarction have shown that MSC trapped in the lung secreted tumor necrosis factor-inducible gene 6 protein (TSG6), which decreased myocardial damage and increased myocardial function (Lee et al. 2009). It remains to be investigated whether this passage through the lungs as well as other organs such as the spleen could be instructive to the injected cells or not and whether this passage could result in changes in the functional capabilities of the injected cells.
3 Limitations
The major disadvantage of the IA administration is the fact that it is an invasive procedure with a small, but non-negligible, risk of complications. A retrospective study reviewing cerebral angiographies in nearly 20,000 patients indicated that the risk of complications due to the procedure is approximately 2 % and that the risk of a new stroke is approximately 0.14 % (Kaufmann et al. 2007). In addition to the intrinsic risks of a cerebral angiography, it is possible that the injection of cells may increase the risk of ischemia due to the occlusion of microvessels or capillaries. A preclinical study using MSCs found that despite the benefits of IA delivery of stem cells to the ischemic brain, there was a clear risk of vascular occlusion and also an increase in mortality compared to non-transplanted animals (Walczak et al. 2008). In fact, in one pilot trial of IA administration of BMMCs in acute stroke that included seven patients, the only complication was an embolic stroke in one patient during the angiographic procedure but before the administration of the cells (de Freitas et al. 2006). The patient did not receive the BMMCs and presented neurological deterioration. The fact that no other patient in the pilot clinical trials presented new ischemic lesions on diffusion-weighted (DWI) magnetic resonance imaging (MRI) after injection of the cells argues that the complication is linked to the procedure, not to the cells per se. Another shortcoming is the requirement of the patency of the intracranial and extracranial circulation (e.g., significant stenosis or occlusion was an exclusion criterion of all the pilot studies). In our view, the occlusion of an intracranial artery but with reasonable collateral supply should not be considered a definitive contraindication to IA administration, since in these cases even with more proximal injections, cells would still be able to reach the damaged area through collateral circulation. Finally, another disadvantage of the IA route is the contact of the cells with the contrast used in the arteriography since results from our group have shown that the viability of the cells decreases in the presence of the contrast (unpublished results).
4 Pilot Clinical Trials
At the time of writing this chapter, only five trials of stem cell administration for ischemic stroke using IA delivery were reported in the literature (de Freitas et al. 2006; Battistella et al. 2011; Friedrich et al. 2012; Moniche et al. 2012; Banerjee et al. 2012), two of them in abstract form (de Freitas et al. 2006; Banerjee et al. 2012) (Table 13.1).
In 2006, our group reported in the International Stroke Conference the results of a small pilot trial designed to evaluate the safety and feasibility of IA transplantation of autologous BMMCs in patients with acute middle cerebral artery (MCA) ischemia (de Freitas et al. 2006). Inclusion criteria were age between 18 and 80, a score between 4 and 20 in the National Institutes of Health Stroke Scale (NIHSS), and administration of the cells within 7 days of stroke onset. Seven patients (two women) with a mean age of 49 years (range from 38 to 58) and mean NIHSS of 9.5 were included in the trial. Bone marrow cells were aspirated (50 ml) from the posterior iliac crest under local anesthesia, and BMMCs were isolated by density gradient on Ficoll-Paque Plus, resuspended in saline with 5 % human serum albumin and immediately injected (30 × 106 cells in 10 ml) in the MCA under continuous transcranial Doppler and electroencephalographic monitoring. The infusion was done at the rate of approximately 1 ml/min. Patients underwent anticoagulation with intravenous heparin to obtain an activated clotting time of two to three times baseline. Differently from cardiac studies that performed intracoronary administration of the cells, a balloon catheter was not used to occlude the target MCA and increase cell delivery because of the risk of arterial dissection. One patient exhibited neurological deterioration (recurrent embolization) during arteriography, did not receive the cells, and was excluded from further analysis. The six patients treated exhibited an uneventful subsequent clinical course, with no new lesions appearing in sequential DWI MRI exams (D7, D60, and D120) and no sign of embolization or epileptic activity. Mean NIHSS scores varied from 9.5 (entry) to 4.5 (D60) and 3 (D120). The corresponding modified Rankin Scale (mRS) and Barthel Index (BI) scores were 3.5, 2, and 2 and 52.5, 92.5, and 52.5, respectively.
To evaluate the feasibility of monitoring the cells implanted into the brain, in one of the patients, approximately 1 % of the 3.0 × 107 BMMCs delivered into the left MCA were labeled with 150 MBq (4 mCi) Technetium-99 m (Tc-99 m) by incubation with hexamethylpropylene amine oxime (HMPAO) (Correa et al. 2007). Tomographic views of the brain, obtained 8 h after BMMC-labeled cell delivery, revealed intense accumulation of the cells in the ipsilateral hemisphere. A whole-body scan was done and showed left brain, liver, and spleen uptake. The results suggested that brain SPECT imaging with labeled cells could be a viable noninvasive method for studying the fate of transplanted cells in vivo.
To address the feasibility of the IA administration of BMMCs after the first few days of ischemic stroke (nonacute stroke phase), Battistella et al. (2011) design a pilot trial with similar characteristics and inclusion criteria of the previous study but including patients up to 90 days after the stroke onset (NCT00473057). Another difference from the previous trial was that in all patients approximately 10 % of the BMMCs were labeled with Tc-99 m and scintigraphies were carried out 2 and 24 h after the procedure to analyze cellular homing and biodistribution. Six male patients, with a mean age of 69 years (range from 24 to 65 years), received between 1.25 × 108 and 5 × 108 BMMCs via IA administration from 59 to 82 (mean 69) days after MCA infarcts, with a mean NIHSS of 9 (range from 4 to 13) at the time of cell infusion. No signs of worsening in the neurological condition were observed immediately after the procedure or during the follow-up period. At the 180-day follow-up evaluation, all patients had improved their scores in comparison with the values before transplantation. For example, the NIHSS scores improved (range from −1 to −8 points) during follow-up in all patients. Two patients suffered generalized seizures after the end of follow-up (around 200 days after the BMMC infusion); one was successfully treated with phenytoin, and the other was treated with a combination of oxcarbazepine and lamotrigine. Whole-body scans obtained 2 h after transplantation of labeled BMMCs showed uptake in the brains of all patients, which ranged from 0.6 to 5.1 % when compared to the activity in the whole body. Quantification of cell uptake in SPECT images indicated preferential uptake on the side of the lesion in all patients. Nevertheless, these differences were widely variable, ranging from 58 to 98 % of total brain uptake. The remaining cell uptake was distributed mainly to the liver, lungs, spleen, and kidneys in all patients. Due to the short half-life of Technetium, uptake could only be visualized in the brains of two patients 24 h after injection, while in all patients uptake was seen in the liver, lungs, spleen, kidneys, and bladder (Barbosa da Fonseca et al. 2009; 2010).
A clinical trial with the largest number of patients was recently published. Friedrich et al. (2012) administered the BMMCs IA in 20 patients with more severe MCA infarctions and at an earlier time point than the previous trials (mean time from stroke onset to treatment 6 ± 1.8 days). The mean age was 63 years (range from 30 to 78), 14 were males, and the right hemisphere was the affected side in 12 patients. The mean baseline NIHSS score was 17 ± 5.6 (median 15.5, range from 9 to 28). The mean cell count in the infused solution was 22.08 × 107 cells (range from 5.1 to 107–60 × 107). None of the patients met the primary end point focused on safety: clinically significant procedural complications (defined as a decline of ≥4 points in the NIHSS score or death), symptomatic intracranial hemorrhage, new ischemic lesions on computed tomography (CT) and/or DWI MRI at day 7 post procedure, clinical seizures and/or epileptic discharges on serial electroencephalogram (EEG) at any time during the hospitalization, and development of intracranial neoplasia in the long-term follow-up. Eight patients (40 %) showed a good clinical outcome, defined previously as a mRS ≤ 2 at 90 days.
Also recently, the results of another trial were published (Moniche et al. 2012). This trial enrolled 10 patients with severe (NIHSS ≥8) MCA infarction to receive BMMCs transplantation (NCT00761982). The first 10 consecutive patients included were considered the active group, and 10 patients were included in the control group. Although no bone marrow aspiration or sham injection was performed in the control group, neurologists who evaluated the patients at 1, 3, and 6 months were unaware of the treatment allocation. Mean NIHSS was comparable between the two groups (15.6 in BMMC group versus 15.0 in the control group, p = 0.82), and transplantation was done at 6.4 (±1.3) days after stroke onset. There were no serious adverse events during the BMMC transplantation procedure. During follow-up, two BMMC-treated patients had an isolated partial seizure at 3 months. There were no seizures in the control group. Neurological disability at 6 months was not significantly different in the two groups, but there was a trend toward a better outcome when higher numbers of CD34+ cells were injected.
Banerjee et al. (2012) reported in the European Stroke Conference the partial results of their study (NCT00535197). The aim of the investigators is to enroll 10 patients with complete MCA infarctions, isolate and harvest CD34+ by immunoselection, and inject them into the MCA within 7 days of the event. Up to the presentation, five patients had been enrolled with no serious treatment-related adverse events, and all presented improvement in their clinical scores and reduction in lesion volume up to 6 months follow-up.
5 Comparison Between Intravenous and Intra-arterial Administration in Humans
The small number of patients and diverse characteristics (e.g., inclusion criteria, type and number of cells injected, time of administration) prevent direct comparison of IA and IV stem cell studies. Recently, Rosado-de-Castro et al. (2012) compared safety end points and biodistribution of cells in patients with subacute ischemic stroke treated in the same hospital, using the same cell type and similar inclusion criteria but different routes. After bone marrow harvesting, approximately 2 × 107 BMMNCs were labeled with 99mTc and delivered via IA or IV together with the unlabeled cells. Scintigraphies were carried out at 2 h and 24 h after cell transplantation. Seven patients were included in the IA group (six of these were already described above in the study of Battistella et al. 2011) and five in the IV group, between 19 and 89 days after stroke. Cell homing in the brain compared to the whole body was low and similar between both routes at 2 h and 24 h. However, when the homing in the ischemic hemisphere was compared with the uptake in the contralateral hemisphere, there was a slightly greater relative uptake of 99mTc-BMMNCs at 2 h in the IA group (68.1 ± 14.6 in the IA group versus 53.4 ± 3.8 in the IV group, p = 0.023). The quantification of whole-body images indicated that the IA route led to greater uptake in the liver and spleen and lower uptake in the lungs at 2 h when compared to the IV route. All patients had neurological improvement, with a decrease in the NIHSS ranging from 1 to 10 points during the follow-up period. Two patients of the IA group and 5 patients of the IV group had seizures that were controlled with antiepileptic medication.
6 Conclusions
IA delivery of stem cells is a promising therapy for patients with cerebral infarcts. Pilot studies in stroke patients suggest that it is safe. Whether homing of stem cells in the affected brain region is larger with IA than with IV therapy is debatable. Limited data from a human study suggest a slightly greater homing of cells in the hemisphere ipsilateral to the ischemia when the cells are delivered IA. However, whether this result translates into greater clinical benefits is unclear since there are data indicating that functional recovery may occur even in the absence of stem cells in the brain. Moreover, the passage of the cells in peripheral organs may confer them protective properties. Larger, randomized phase III studies are necessary to establish the efficacy of this approach and the best delivery route.
References
Bacigaluppi M, Pluchino S, Peruzzotti-Jametti L, Kilic E, Kilic U, Salani G, Brambilla E, West MJ, Comi G, Martino G, Hermann DM (2009) Delayed post-ischaemic neuroprotection following systemic neural stem cell transplantation involves multiple mechanisms. Brain 132:2239–2251
Banerjee S, Bentley P, Hamady M, Davis J, Shlebak A, Gordon M, Habib N, Chataway J (2012) Phase I trial of autologous CD34+ haematopoietic stem cells in acute ischemic stroke. Cerebrovasc Dis 33:58, abstract
Bang OY, Lee JS, Lee PH, Lee G (2005) Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol 57:874–882
Barbosa da Fonseca LM, Battistella V, de Freitas GR, Gutfilen B, Dos Santos Goldenberg RC, Maiolino A, Wajnberg E, Rosado de Castro PH, Mendez-Otero R, Andre C (2009) Early tissue distribution of bone marrow mononuclear cells after intra-arterial delivery in a patient with chronic stroke. Circulation 120:539–541
Barbosa da Fonseca LM, Gutfilen B, Rosado de Castro PH, Battistella V, Goldenberg RC, Kasai-Brunswick T, Chagas CL, Wajnberg E, Maiolino A, Salles Xavier S, Andre C, Mendez-Otero R, de Freitas GR (2010) Migration and homing of bone-marrow mononuclear cells in chronic ischemic stroke after intra-arterial injection. Exp Neurol 221:122–128
Battistella V, de Freitas GR, da Fonseca LM, Mercante D, Gutfilen B, Goldenberg RC, Dias JV, Kasai-Brunswick TH, Wajnberg E, Rosado-de-Castro PH, Alves-Leon SV, Mendez-Otero R, Andre C (2011) Safety of autologous bone marrow mononuclear cell transplantation in patients with nonacute ischemic stroke. Regen Med 6:45–52
Bliss TM, Andres RH, Steinberg GK (2010) Optimizing the success of cell transplantation therapy for stroke. Neurobiol Dis 37:275–283
Borlongan CV, Hadman M, Sanberg CD, Sanberg PR (2004) Central nervous system entry of peripherally injected umbilical cord blood cells is not required for neuroprotection in stroke. Stroke 35:2385–2389
Brenneman M, Sharma S, Harting M, Strong R, Cox CS Jr, Aronowski J, Grotta JC, Savitz SI (2010) Autologous bone marrow mononuclear cells enhance recovery after acute ischemic stroke in young and middle-aged rats. J Cereb Blood Flow Metab 30:140–149
Correa PL, Mesquita CT, Felix RM, Azevedo JC, Barbirato GB, Falcão CH, Gonzalez C, Mendonça ML, Manfrim A, de Freitas G, Oliveira CC, Silva D, Avila D, Borojevic R, Alves S, Oliveira AC Jr, Dohmann HF (2007) Assessment of intra-arterial injected autologous bone marrow mononuclear cell distribution by radioactive labeling in acute ischemic stroke. Clin Nucl Med 32:839–841
de Freitas GR, Mendonca ML, Bezerra DC, Silva SA, Falcão CH, Gonzales C, Moreira RC, Haddad AF, Tuche FA, Santos DP, Andre C, Mesquita CT, Oliveira AC Jr, Elia V, Dohmann HJ, Borojevic R, Mendez-Otero R, Dohmann HF (2006) Safety and feasibility of intra-arterial autologous bone marrow mononuclear cell transplantation in acute ischemic stroke. Stroke 37:624–625, abstract
Fischer UM, Harting MT, Jimenez F, Monzon-Posadas WO, Xue H, Savitz SI, Laine GA, Cox CS Jr (2009) Pulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev 18:683–692
Friedrich MA, Martins MP, Araujo MD, Klamt C, Vedolin L, Garicochea B, Raupp EF, Ammar JS, Machado DC, Costa JC, Nogueira RG, Rosado-de-Castro PH, Mendez-Otero R, de Freitas GR (2012) Intra-arterial infusion of autologous bone-marrow mononuclear cells in patients with moderate to severe middle-cerebral-artery acute ischemic stroke. Cell Transplant 21:S13–S21
Gao J, Dennis JE, Muzic RF, Lundberg M, Caplan AI (2001) The dynamic in vivo distribution of bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs 169:12–20
Hess DC, Hill WD (2011) Cell therapy for ischaemic stroke. Cell Prolif 44:1–8
Honmou O, Houkin K, Matsunaga T, Niitsu Y, Ishiai S, Onodera R, Waxman SG, Kocsis JD (2011) Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 134:1790–1807
Kamiya N, Ueda M, Igarashi H, Nishiyama Y, Suda S, Inaba T, Katayama Y (2008) Intra-arterial transplantation of bone marrow mononuclear cells immediately after reperfusion decreases brain injury after focal ischemia in rats. Life Sci 83:433–437
Kaufmann TJ, Huston J III, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF (2007) Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology 243:812–819
Kondziolka D, Wechsler L, Goldstein S, Meltzer C, Thulborn KR, Gebel J, Jannetta P, DeCesare S, Elder EM, McGrogan M, Reitman MA, Bynum L (2000) Transplantation of cultured human neuronal cells for patients with stroke. Neurology 55:565–569
Kondziolka D, Steinberg GK, Wechsler L, Meltzer CC, Elder E, Gebel J, Decesare S, Jovin T, Zafonte R, Lebowitz J, Flickinger JC, Tong D, Marks MP, Jamieson C, Luu D, Bell-Stephens T, Teraoka J (2005) Neurotransplantation for patients with subcortical motor stroke: a phase 2 randomized trial. J Neurosurg 103:38–45
Lee RH, Pulin AA, Seo MJ, Kota DJ, Ylostalo J, Larson BL, Semprun-Prieto L, Delafontaine P, Prockop DJ (2009) Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5:54–63
Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY (2010) A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 28:1099–1106
Mattle HP, Arnold M, Georgiadis D, Baumann C, Nedeltchev K, Benninger D, Remonda L, von Büdingen C, Diana A, Pangalu A, Schroth G, Baumgartner RW (2008) Comparison of intraarterial and intravenous thrombolysis for ischemic stroke with hyperdense middle cerebral artery sign. Stroke 39:379–383
Mendez-Otero R, de Freitas GR, Andre C, de Mendonca ML, Friedrich M, Oliveira-Filho J (2007) Potential roles of bone marrow stem cells in stroke therapy. Regen Med 2:417–423
Misra V, Lal A, El Khoury R, Chen PR, Savitz SI (2012) Intra-arterial delivery of cell therapies for stroke. Stem Cells Dev 21:1007–1015
Moniche F, Gonzalez A, Gonzalez-Marcos JR, Carmona M, Pinero P, Espigado I, Garcia-Solis D, Cayuela A, Montaner J, Boada C, Rosell A, Jimenez MD, Mayol A, Gil-Peralta A (2012) Intra-arterial bone marrow mononuclear cells in ischemic stroke: a pilot clinical trial. Stroke 43:2242–2244
Rosado-de-Castro PH, Schmidt F, Battistella V, Souza S, Gutfilen B, Goldenberg R, Kasai-Brunswick T, Vairo L, Silva R, Wajnberg E, Brasil P, Gasparetto R, Maiolino A, Alves-Leon S, Andre C, Mendez-Otero R, de Freitas GR, Barbosa da Fonseca L (2012) Safety and biodistribution of bone marrow mononuclear cells after intra-arterial or intravenous transplantation in subacute stroke patients (Submitted)
Savitz SI, Dinsmore J, Wu J, Henderson GV, Stieg P, Caplan LR (2005) Neurotransplantation of fetal porcine cells in patients with basal ganglia infarcts: a preliminary safety and feasibility study. Cerebrovasc Dis 20:101–107
Savitz SI, Misra V, Kasam M, Juneja H, Cox CS Jr, Alderman S, Aisiku I, Kar S, Gee A, Grotta JC (2011) Intravenous autologous bone marrow mononuclear cells for ischemic stroke. Ann Neurol 70:59–69
Schrepfer S, Deuse T, Reichenspurner H, Fischbein MP, Robbins RC, Pelletier MP (2007) Stem cell transplantation: the lung barrier. Transplant Proc 39:573–576
Suarez-Monteagudo C, Hernandez-Ramirez P, Alvarez-Gonzalez L, Garcia-Maeso I, de la Cuetara-Bernal K, Castillo-Diaz L, Bringas-Vega ML, Martinez-Aching G, Morales-Chacon LM, Baez-Martin MM, Sanchez-Catasus C, Carballo-Barreda M, Rodriguez-Rojas R, Gomez-Fernandez L, Alberti-Amador E, Macias-Abraham C, Balea ED, Rosales LC, Del Valle PL, Ferrer BB, Gonzalez RM, Bergado JA (2009) Autologous bone marrow stem cell neurotransplantation in stroke patients. An open study. Restor Neurol Neurosci 27:151–161
Vasconcelos-dos-Santos A, Rosado-de-Castro PH, Lopes de Souza SA, da Costa Silva J, Ramos AB, Rodriguez de Freitas G, Barbosa da Fonseca LM, Gutfilen B, Mendez-Otero R (2012) Intravenous and intra-arterial administration of bone marrow mononuclear cells after focal cerebral ischemia: is there a difference in biodistribution and efficacy? Stem Cell Res 9:1–8
Walczak P, Zhang J, Gilad AA, Kedziorek DA, Ruiz-Cabello J, Young RG, Pittenger MF, van Zijl PC, Huang J, Bulte JW (2008) Dual-modality monitoring of targeted intra-arterial delivery of mesenchymal stem cells after transient ischemia. Stroke 39:1569–1574
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this chapter
Cite this chapter
de Freitas, G.R., Mendez-Otero, R. (2013). Intra-arterial Cell Therapy in Stroke Patients. In: Jolkkonen, J., Walczak, P. (eds) Cell-Based Therapies in Stroke. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1175-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1175-8_13
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1174-1
Online ISBN: 978-3-7091-1175-8
eBook Packages: MedicineMedicine (R0)