Abstract
Cell transplantation therapy for cerebral infarction has emerged as a promising treatment to reduce brain damage and enhance functional recovery. We previously reported that intra-arterial delivery of bone marrow mesenchymal stem cells (MSCs) enables superselective cell administration to the infarct area and results in significant functional recovery after ischemic stroke in a rat model. However, to reduce the risk of embolism caused by the transplanted cells, an optimal cell number should be determined. At 24 h after middle cerebral artery occlusion and reperfusion, we administered human MSCs (low dose: 1 × 104 cells; high dose: 1 × 106 cells) and then assessed functional recovery, inflammatory responses, cell distribution, and mortality. Rats treated with high- or low-dose MSCs showed behavioral recovery. At day 8 post-stroke, microglial activation was suppressed significantly, and interleukin (IL)-1β and IL-12p70 were reduced in both groups. Although high-dose MSCs were more widely distributed in the cortex and striatum of rats, the degree of intravascular cell aggregation and mortality was significantly higher in the high-dose group. In conclusion, selective intra-arterial transplantation of low-dose MSCs has anti-inflammatory effects and reduces the adverse effects of embolic complication, resulting in sufficient functional recovery of the affected brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual age-standardized mortality rate of ischemic stroke is steadily decreasing with the advancement of treatment strategies including endovascular treatment and intravenous administration of tissue plasminogen activator. Nevertheless, its morbidity is still a serious issue and the resultant symptoms can have a negative effect on quality of life. Recently, stem cell transplantation for stroke treatment has shown promising results in small and large animal models (Bliss et al. 2007; Chen et al. 2001; Eckert et al. 2013; Lindvall and Kokaia 2011; Misra et al. 2012; Stem Cell Therapies as an Emerging Paradigm in Stroke 2009). Many clinical trials are ongoing to establish this strategy in a clinical setting (Rosado-de-Castro et al. 2013). However, there are many variables that can affect the efficacy of cell transplantation, including donor cells (cell type, safety, and auto vs. allogeneic), recipients (patient age, stroke subtype, and location), treatment strategy (acute, sub-acute, or chronic, delivery route, and cell dose), and validation (functional assessment and imaging) (Abe et al. 2012).
Intra-arterial administration of stem cells is a feasible route for stem cell delivery to the stroke-affected brain with the advantage of superselective delivery without loss through filtering organs (Amar et al. 2003; Guzman et al. 2008a; Ishizaka et al. 2013). Animal studies have demonstrated higher rates of cell engraftment via intra-arterial delivery and a higher concentration of cells in the target ischemic lesion (Guzman et al. 2008b) and improved functional recovery than when compared to intravenous cell infusion (Kamiya et al. 2008; Yavagal et al. 2014). However, the major issue of intra-arterial delivery is embolic stroke due to aggregation of the cells in the blood vessels (Chua et al. 2011). These results suggest that low-dose, intra-arterial cell administration could prevent embolic complications and might induce functional recovery, that have not been clarified.
In this study, we determined whether low-dose mesenchymal stem cell (MSC) administration has a therapeutic effect, in terms of post-stroke functional recovery and the host environment, and investigated embolic complications in comparison with high-dose cell transplantation.
Methods
Middle Cerebral Artery Occlusion and Reperfusion Model
All animal procedures were approved by the Administrative Panel on Laboratory Animal Care of Nagasaki University. Male Sprague–Dawley rats (250–300 g) were anesthetized with 5 % isoflurane and maintained under anesthesia by 2 % isoflurane in 70 % N2O and 30 % O2 using a vaporizer during all surgical procedures. Transient middle cerebral artery occlusion (MCAO) was performed for 75 min with a 4.0 nylon monofilament suture (Encarnacion et al. 2011). The rectal temperature was maintained at 37 °C throughout the surgical procedure. Rats showing a modified neurological severity score (mNSS) from 5 to 8 points at 24 h post-stroke were included in this study.
Cell Culture and Transplantation
MSCs were obtained by iliac crest aspiration from a 19-year-old healthy female volunteer (cells registered in Lonza, Japan; Product Code: PT-2501). The cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA) supplemented with 10 % fetal bovine serum, 3 ng/ml basic fibroblast growth factor, and 2 % penicillin/streptomycin.
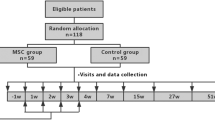
Cells were delivered thorough a catheter inserted from the stump of the distal external carotid artery to the internal carotid artery via bifurcation. The cell suspension was injected slowly (100 μl/min) along with the antegrade blood flow from the common carotid artery. As previous papers used 1 × 106 MSCs for intra-arterial administration (Ishizaka et al. 2013; Mitkari et al. 2014; Walczak et al. 2008; Yavagal et al. 2014), we randomly divided the animals into three groups; low-dose MSC group: 1 × 104 cells/300 μl, high-dose MSC group: 1 × 106 cells/300 μl, and control: 300 μl phosphate buffered saline. Cyclosporine A (10 mg/kg) was injected intraperitoneally every day until euthanasia.
Neurobehavioral Tests
Neurological recovery was assessed by the cylinder test and mNSS at day 0, 1, 2, 5, and 8 post-stroke. The cylinder test is used to measure forelimb use during vertical exploration (Horie et al. 2008). Rats were placed in a Plexiglas cylinder, and the number of times each rat reached and touched the cylinder in a weight-bearing fashion with the left, right, or both forelimbs was counted. Approximately 20 of these limb-use movements were counted per trial. The behavior score was calculated using the equation: (affected limb use + both limb use)/(unaffected limb use + both limb use), giving a ratio of affected to unaffected limb use. The mNSS consisted of motor (muscle status and abnormal movement), sensory (visual, tactile, and proprioceptive), reflex, and balance tests (Chen et al. 2001).
Histological and Immunohistochemical Analyses
All quantifications and analyses were performed in a double-blinded manner. Animals were anesthetized and perfused transcardially with 4 % paraformaldehyde at 8 days after MCAO. Brains were removed and prepared as 5-μm paraffin-embedded sections and 20-μm frozen coronal sections. Antigen retrieval was performed by incubation in target retrieval solution (pH 6.0; Dako, Carpinteria, CA) for 2 h at room temperature. For immunohistochemical staining, the 20-μm sections were incubated with primary antibodies (rabbit anti-Iba-1, 1:250, Wako Chemicals, Osaka, Japan; mouse anti-ED1, 1:100, ab31630, Abcam) at 4 °C overnight and then with secondary antibodies (biotinylated donkey anti-rabbit IgY, 1:500; Gallus, USA). The sections were then applied to an avidin–biotin-peroxidase complex kit (ChemMate ENVISION kit/HRP; Dako, Japan). Labeled proteins were visualized with 3,30-diaminobenzidine. The number of Iba-1-positive and ED-1-positive cells was counted using WinROOF software (Mitani, Tokyo, Japan). Peri-infarct, a region of drastic reorganization and rewiring of surviving circuits, was used as the region of analysis (Murphy and Corbett 2009).
To evaluate the MSC distribution, sections were incubated with mouse anti-human vimentin (1:50; Millipore, Tokyo, Japan) at 4 °C overnight and then with secondary antibodies (TOPRO-3, 1:500; Molecular Probes, Tokyo, Japan, or Alexa Fluor 488 donkey anti-mouse IgG, 1:1,000; Molecular Probes) for 2 h at room temperature. The sections were analyzed using a confocal laser microscope (LSM5 Pascal Ver 3.2; Zeiss). The mouse anti-human vimentin antibody stains cells of human mesenchymal origin.
To evaluate cell aggregation, we used PKH26 (Sigma, Japan), a red fluorescent cell linker. MSCs were harvested and stained with PKH26 before cell transplantation as described previously (Messina et al. 1992). Two days after transplantation, the rats were anesthetized and perfused to analyze the MSC distribution in the peri-infarct cortex and striatum. To label endothelial cells, the sections were also incubated with mouse anti-RECA-1 (1:500, Abcam, Tokyo, Japan) at 4 °C overnight and then with secondary antibodies (TOPRO-3, 1:500, or Alexa Fluor 488 donkey anti-mouse IgG, 1:1,000) for 2 h at room temperature.
Luminex Assay
MILLIPLEX MAP kits (Millipore, Bedford, MA, USA) were used for microsphere-based multiplex immunoassays to measure the concentrations of various proteins. The following rat-specific cytokines and chemokines were measured in rat brain tissue: interleukin (IL)-4, IL-1β, IL-6, IL-10, IL-12p70, interferon gamma, IL-17, MCP-1, tumor necrosis factor-α, epidermal growth factor, and vascular endothelial growth factor. The system was set to analyze 100 μl of sample per well according to the manufacturer’s protocol. At 5 days after MCAO, the rats were anesthetized and euthanized. Rat brains were removed and small pieces were cut from cerebral cortex while excluding the infarct core. Then, the brains were homogenized in phosphate buffered saline as a 10 % solution, and cytokine/chemokine levels were measured.
Statistical Analysis
Data are presented as the mean ± SEM. Data were tested for normality and equal standard deviations in GraphPad InStat (Ver 3.10; GraphPad Software, USA) to determine the appropriate statistical test (parametric vs. nonparametric). The figure legends describe the statistical tests. Unless stated otherwise, all tests were two-tailed. Differences were considered statistically significant at P < 0.05.
Results
MSC Transplantation Leads to Behavioral Recovery at Both Low and High Doses
Behavioral scores were markedly lower at day 1 post-stroke in all groups. However, the animals treated with MSCs showed significant recovery in the cylinder test at day 5 (control: 0.26 ± 0.1; low-dose MSCs: 0.71 ± 0.1; high-dose MSCs: 0.54 ± 0.1, Fig. 1a) and the mNSS at day 8 (control: 6.2 5 ± 0.9; low-dose MSCs: 4.0 ± 0.8, high-dose MSCs: 4.5 ± 0.6, Fig. 1b). The animals with low-dose MSCs showed better neurological recovery, but there was no significant difference between low- and high-dose MSCs. Body weight increases were also evident in the animals treated with MSCs regardless of low or high doses (Fig. 1c).
Time course of behavioral changes evaluated by the cylinder test (a), mNSS (b), and body weight (c) showed recovery in mesenchymal stem cell (MSC)-treated animals with no difference between low and high doses [n = 8; one-way analysis of variance (ANOVA), Tukey–Kramer multiple comparison test, *P < 0.05 low-dose MSCs vs. control, # P < 0.05 high-dose MSCs vs. control]
MSC Transplantation has an Anti-inflammatory Effect at Both Low and High Doses
At 7 days post-transplantation (8 days post-stroke), many Iba 1-positive microglia (19,457.6 ± 3,388.2 cells/mm2) and ED1-positive activated microglia (14,036.0 ± 1,663.8 cells/mm2) had infiltrated into both the peri-infarct cortex and striatum (Fig. 2). However, the animals that received MSCs showed fewer Iba 1-positive cells (low-dose MSCs: 10,655.3 ± 1,985.3 cells/mm2; high-dose MSCs: 11,426.5 ± 1,763.7 cells/mm2) and ED1-positive cells (low-dose MSCs: 9,797.7 ± 969.8 cells/mm2; high-dose MSCs: 8,517.1 ± 1,327.2 cells/mm2) in the peri-infarct cortex and striatum. Luminex assays showed significant reductions of IL-1β (control: 327.1 ± 21.6 pg/ml; low-dose MSCs: 211.0 ± 21.4 pg/ml; high-dose MSCs: 237.8 ± 34.6 pg/ml) and IL-12p70 (control: 53.3 ± 8.9 pg/ml; low-dose MSCs: 30.3 ± 6.4 pg/ml; high-dose MSCs: 32.3 ± 1.2 pg/ml) in animals treated with MSCs (Fig. 3).
Infiltration of microglia (Iba-1-positive cells) and activated microglia (ED1-positive cells) was significantly suppressed after mesenchymal stem cell (MSC) transplantation in the peri-infarct cortex and striatum at 8 days post-stroke (a). Representative image showing that Iba-1-positive cells were drastically suppressed in the peri-infarct cortex of low- and high-dose MSC groups (b). Scale bar = 100 μm. N = 8; one-way ANOVA, Tukey–Kramer multiple comparison test, *P < 0.05 vs. control
Differences in MSC Distribution and Overall Mortality at Low and High Doses
MSCs were widely distributed throughout the cortex and striatum of the ipsilateral hemisphere at 24 h after transplantation of high-dose MSCs (cortex: 546.3 ± 55.9/mm2; striatum: 475.9 ± 79.9/mm2, Fig. 4), while few cells were observed in the low-dose MSC group (cortex: 314.8 ± 57.5/mm2, P = 0.008; striatum: 88.9 ± 37.3/mm2, P < 0.001, Fig. 4). Interestingly, more PKH-positive aggregated cells were detected in the RECA-positive endothelial lumen around the cortex and striatum in animals treated with high-dose MSCs (low-dose MSCs: 0.21 ± 0.1/mm2; high-dose MSCs: 0.003 ± 0.003/mm2, Fig. 5; P = 0.002). No PKH-positive cells were identified in the control group. Overall mortality was also high in the high-dose MSC group compared with that in the low-dose MSC group at 8 days post-stroke (Table 1).
Many human mesenchymal stem cells (MSCs) were distributed throughout the peri-infarct area in the high-dose MSC group at 24 h post-transplantation, whereas very few MSCs had reached the brain parenchyma in the low-dose MSC group (a). Quantification of the distributed cells showed a significantly larger number of cells in both the cortex and striatum of the high-dose MSC group (b, n = 6; **P < 0.01, ### P < 0.001, unpaired t test with two-tailed value; scale bar = 100 μm)
Many aggregated PKH-positive human mesenchymal stem cells (MSCs) were detected in the RECA-1-positive endothelial lumen of the high-dose MSC group at 24 h post-transplantation (a). Quantification of the aggregated cells showed a significantly larger number of aggregations in the high-dose MSC group (b, n = 6; **P < 0.01, unpaired t test with two-tailed value; scale bars = 100 and 50 μm in the magnified image
Discussion
In this study, accelerated functional recovery after stroke was observed in model animals treated with MSCs at not only a high dose (1 × 106 cells) but also a low dose (1 × 104 cells). Anti-inflammatory effects were also evident by decreases in microglia infiltration and cytokine induction, suggesting that enough cells had migrated into the brain to prevent secondary damage after stroke.
Recent animal studies have shown the efficacy of stem cell transplantation via the carotid arteries (Andres et al. 2011a; Byun et al. 2013; Gutierrez-Fernandez et al. 2011; Janowski et al. 2013; Chua et al. 2011; Kamiya et al. 2008; Li et al. 2001; Rosenblum et al. 2012; Walczak et al. 2008; Yang et al. 2013; Yavagal et al. 2014). Intra-arterial delivery of stem cells might be a novel therapeutic strategy that addresses the main issue with intravenous delivery, namely the dispersal of cells throughout the body, and fewer transplantable cells are needed for engraftment in the brain parenchyma (Guzman et al. 2008a; Liu et al. 2006). Therefore, intra-arterial cell transplantation has the potential to maximize the effect of a smaller number of cells in the selected vascular territory. This approach is particularly advantageous for autologous transplantation because time is needed to expand autologous cells for transplantation in a clinical setting. However, the major issue of intra-arterial delivery is embolic stroke due to aggregation of the cells in the blood vessels (Chua et al. 2011). It has been reported that intra-arterial transplantation has the risk of reducing cerebral blood flow, which is associated with microembolic stroke. However, intra-arterial cell delivery with maintained blood flow can be used to successfully deliver cells into the cerebral vasculature without causing ischemic changes, allowing transplanted cells to undergo targeted migration to the damaged brain (Chua et al. 2011). Another study demonstrated a clear risk of vascular occlusion and a large increase in mortality (67 % for intra-arterial transplantation compared with 7 % in nontransplanted animals) (Walczak et al. 2008). Therefore, the cell size, velocity of injection (Janowski et al. 2013), and cell dose are major determinants of the safety of intra-arterial cell transplantation. Some reports have investigated the superiority of intra-arterial delivery in comparison with intravenous delivery (Byun et al. 2013; Gutierrez-Fernandez et al. 2011; Pendharkar et al. 2010). However, few studies have investigated the dose-dependent efficacy and safety of intra-arterial delivery of stem cells (Yavagal et al. 2014). Intra-arterial transplantation enables selective cell administration to the affected territory, thus, a lower cell dose is required while preventing embolic strokes. Here, we found that a low dose of MSCs (1 × 104) provides functional recovery after stroke, but further assessment of the optimal cell dose is required to evaluate the efficacy and adverse effects.
Yavagal et al. (2014) showed that administration of allogeneic intra-arterial MSCs at 24 h, but not 1 h, after cerebral ischemia has a therapeutic effect. Rosenblum et al. (2012) described that the hyperacute phase in post-ischemic brain tissue may be detrimental to administrated intra-arterial cells, and that waiting for the inflammatory response to diminish in the first days is advantageous. We previously reported that motor function improves earlier when MSCs are administrated at 24 h, and later at 4 days, but not at 7 days (Ishizaka et al. 2013). In this study, we transplanted the cells 24 h after stroke according to our previous report (Ishizaka et al. 2013).
Previously, we reported that intraparenchymal cell transplantation promotes endogenous repair processes, such as angiogenesis, blood–brain barrier integrity, dendritic plasticity, and axonal sprouting in the peri-infarct area after stroke (Andres et al. 2011b; Horie et al. 2011). In this study, after intra-arterial administration of both low and high doses of cells, we found significant suppression of microglial activation and reductions in interleukin (IL)-1β and IL-12p70 expression at 5 days post-stroke. A study of modulation by human MSCs in vitro and in vivo revealed that human MSCs decrease the expression of microglial activation markers ED1 and Iba1 (McGuckin et al. 2013). IL-1β is considered to be a neurotoxic mediator, because a loss of IL-1β functions has been reported to reduce the infarct size (Boutin et al. 2001). IL-12 is produced by infiltrating macrophages in the ischemic brain (Shichita et al. 2012). In our study, we found that the low-dose of MSCs (1 × 104) still exerted anti-inflammatory effects and reduced adverse effects of embolic complications, resulting in sufficient functional recovery of the affected brain.
Several limitations of this study should be addressed. First, we did not examine the dose dependency or optimal cell dose. The cell source, injection velocity, and other technical differences also affect the risk of embolic stroke after intra-arterial transplantation. A cerebral blood flow study or magnetic resonance imaging was not performed to confirm embolic strokes. Nevertheless, we believe this is the first study of low-dose MSCs to show efficacy for functional recovery after intra-arterial transplantation. These results should be translated to a clinical phase I/II study using low-dose cells for intra-arterial transplantation after stroke.
Conclusions
It may be possible to minimize the risk of embolic strokes affecting morbidity and mortality by reducing the number of MSCs administered via the intra-arterial route. Low-dose cell transplantation by intra-arterial delivery may be sufficient for anti-inflammatory effects and functional recovery after stroke. Assessment of the optimal cell dose is needed to establish such cell transplantation therapy as a clinical strategy, especially using autologous bone marrow stem cells at the very early stage of stroke.
Change history
30 January 2020
The original version of this article unfortunately contained an error in affiliation of Yuhtaka Fukuda.
References
Abe K, Yamashita T, Takizawa S, Kuroda S, Kinouchi H, Kawahara N (2012) Stem cell therapy for cerebral ischemia: from basic science to clinical applications. J Cereb Blood Flow Metab 32:1317–1331
Amar AP, Zlokovic BV, Apuzzo MLJ (2003) Endovascular restorative neurosurgery: a novel concept for molecular and cellular therapy of the nervous system. Neurosurgery 52:402–413
Andres RH, Choi R, Pendharkar AV, Gaeta X, Wang N, Nathan JK, Chua JY, Lee SW, Palmer TD, Steinberg GK, Guzman R (2011a) The CCR2/CCL2 interaction mediates the transendothelial recruitment of intravascularly delivered neural stem cells to the ischemic brain. Stroke 42:2923–2931
Andres RH, Horie N, Slikker W, Keren-Gill H, Zhan K, Sun G, Manley NC, Pereira MP, Sheikh LA, McMillan EL, Schaar BT, Svendsen CN, Bliss TM, Steinberg GK (2011b) Human neural stem cells enhance structural plasticity and axonal transport in the ischaemic brain. Brain 134:1777–1789
Bliss T, Guzman R, Daadi M, Steinberg GK (2007) Cell transplantation therapy for stroke. Stroke 38:817–826
Boutin H, LeFeuvre RA, Horai R, Asano M, Iwakura Y, Rothwell NJ (2001) Role of IL-1alpha and IL-1beta in ischemic brain damage. J Neurosci 21:5528–5534
Byun JS, Kwak BK, Kim JK, Jung J, Ha BC, Park S (2013) Engraftment of human mesenchymal stem cells in a rat photothrombotic cerebral infarction model: comparison of intra-arterial and intravenous infusion using MRI and histological analysis. J Korean Neurosurg Soc 54:467–476
Chen J, Li Y, Wang L, Zhang Z, Lu D, Lu M, Chopp M (2001) Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke 32:1005–1011
Chua JY, Pendharkar AV, Wang N, Choi R, Andres RH, Gaeta X, Zhang J, Moseley ME, Guzman R (2011) Intra-arterial injection of neural stem cells using a microneedle technique does not cause microembolic strokes. J Cereb Blood Flow Metab 31:1263–1271
Eckert MA, Vu Q, Xie K, Yu J, Liao W, Cramer SC, Zhao W (2013) Evidence for high translational potential of mesenchymal stromal cell therapy to improve recovery from ischemic stroke. J Cereb Blood Flow Metab 33:1322–1334
Encarnacion A, Horie N, Keren-Gill H, Bliss TM, Steinberg GK, Shamloo M (2011) Long-term behavioral assessment of function in an experimental model for ischemic stroke. J Neurosci Methods 196:247–257
Gutierrez-Fernandez M, Rodriguez-Frutos B, Alvarez-Grech J, Vallejo-Cremades MT, Exposito-Alcaide M, Merino J, Roda JM, Diez-Tejedor E (2011) Functional recovery after hematic administration of allogenic mesenchymal stem cells in acute ischemic stroke in rats. Neuroscience 175:394–405
Guzman R, Choi R, Gera A, De Los Angeles A, Andres RH, Steinberg GK (2008a) Intravascular cell replacement therapy for stroke. Neurosurg Focus 24:E15
Guzman R, De Los Angeles A, Cheshier S, Choi R, Hoang S, Liauw J, Schaar B, Steinberg G (2008b) Intracarotid injection of fluorescence activated cell-sorted CD49d-positive neural stem cells improves targeted cell delivery and behavior after stroke in a mouse stroke model. Stroke 39:1300–1306
Horie N, Maag AL, Hamilton SA, Shichinohe H, Bliss TM, Steinberg GK (2008) Mouse model of focal cerebral ischemia using endothelin-1. J Neurosci Methods 173:286–290
Horie N, Pereira MP, Niizuma K, Sun G, Keren-Gill H, Encarnacion A, Shamloo M, Hamilton SA, Jiang K, Huhn S, Palmer TD, Bliss TM, Steinberg GK (2011) Transplanted stem cell-secreted vascular endothelial growth factor effects poststroke recovery, inflammation, and vascular repair. Stem Cells 29:274–285
Ishizaka S, Horie N, Satoh K, Fukuda Y, Nishida N, Nagata I (2013) Intra-arterial cell transplantation provides timing-dependent cell distribution and functional recovery after stroke. Stroke 44:720–726
Janowski M, Lyczek A, Engels C, Xu J, Lukomska B, Bulte JW, Walczak P (2013) Cell size and velocity of injection are major determinants of the safety of intracarotid stem cell transplantation. J Cereb Blood Flow Metab 33:921–927
Kamiya N, Ueda M, Igarashi H, Nishiyama Y, Suda S, Inaba T, Katayama Y (2008) Intra-arterial transplantation of bone marrow mononuclear cells immediately after reperfusion decreases brain injury after focal ischemia in rats. Life Sci 83:433–437
Li Y, Chen J, Wang L, Lu M, Chopp M (2001) Treatment of stroke in rat with intracarotid administration of marrow stromal cells. Neurology 56:1666–1672
Lindvall O, Kokaia Z (2011) Stem cell research in stroke: how far from the clinic? Stroke 42:2369–2375
Liu H, Honmou O, Harada K, Nakamura K, Houkin K, Hamada H, Kocsis JD (2006) Neuroprotection by PlGF gene-modified human mesenchymal stem cells after cerebral ischaemia. Brain 129:2734–2745
McGuckin CP, Jurga M, Miller AM, Sarnowska A, Wiedner M, Boyle NT, Lynch MA, Jablonska A, Drela K, Lukomska B, Domanska-Janik K, Kenner L, Moriggl R, Degoul O, Perruisseau-Carrier C, Forraz N (2013) Ischemic brain injury: a consortium analysis of key factors involved in mesenchymal stem cell-mediated inflammatory reduction. Arch Biochem Biophys 534:88–97
Messina LM, Podrazik RM, Whitehill TA, Ekhterae D, Brothers TE, Wilson JM, Burkel WE, Stanley JC (1992) Adhesion and incorporation of lacZ-transduced endothelial cells into the intact capillary wall in the rat. Proc Natl Acad Sci USA 89:12018–12022
Misra V, Ritchie MM, Stone LL, Low WC, Janardhan V (2012) Stem cell therapy in ischemic stroke: role of IV and intra-arterial therapy. Neurology 79:S207–S212
Mitkari B, Nitzsche F, Kerkela E, Kuptsova K, Huttunen J, Nystedt J, Korhonen M, Jolkkonen J (2014) Human bone marrow mesenchymal stem/stromal cells produce efficient localization in the brain and enhanced angiogenesis after intra-arterial delivery in rats with cerebral ischemia, but this is not translated to behavioral recovery. Behav Brain Res 259:50–59
Murphy TH, Corbett D (2009) Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci 10:861–872
Pendharkar AV, Chua JY, Andres RH, Wang N, Gaeta X, Wang H, De A, Choi R, Chen S, Rutt BK, Gambhir SS, Guzman R (2010) Biodistribution of neural stem cells after intravascular therapy for hypoxic-ischemia. Stroke 41:2064–2070
Rosado-de-Castro PH, Pimentel-Coelho PM, da Fonseca LM, de Freitas GR, Mendez-Otero R (2013) The rise of cell therapy trials for stroke: review of published and registered studies. Stem Cells Dev 22:2095–2111
Rosenblum S, Wang N, Smith TN, Pendharkar AV, Chua JY, Birk H, Guzman R (2012) Timing of intra-arterial neural stem cell transplantation after hypoxia-ischemia influences cell engraftment, survival, and differentiation. Stroke 43:1624–1631
Shichita T, Ago T, Kamouchi M, Kitazono T, Yoshimura A, Ooboshi H (2012) Novel therapeutic strategies targeting innate immune responses and early inflammation after stroke. J Neurochem 123(Suppl 2):29–38
Stem Cell Therapies as an Emerging Paradigm in Stroke (STEPS) (2009) Bridging basic and clinical science for cellular and neurogenic factor therapy in treating stroke. Stroke 40:510–515
Walczak P, Zhang J, Gilad AA, Kedziorek DA, Ruiz-Cabello J, Young RG, Pittenger MF, van Zijl PC, Huang J, Bulte JW (2008) Dual-modality monitoring of targeted intraarterial delivery of mesenchymal stem cells after transient ischemia. Stroke 39:1569–1574
Yang B, Migliati E, Parsha K, Schaar K, Xi X, Aronowski J, Savitz SI (2013) Intra-arterial delivery is not superior to intravenous delivery of autologous bone marrow mononuclear cells in acute ischemic stroke. Stroke 44:3463–3472
Yavagal DR, Lin B, Raval AP, Garza PS, Dong C, Zhao W, Rangel EB, McNiece I, Rundek T, Sacco RL, Perez-Pinzon M, Hare JM (2014) Efficacy and dose-dependent safety of intra-arterial delivery of mesenchymal stem cells in a rodent stroke model. PLoS ONE 9:e93735
Acknowledgments
This work was supported in part by a Grant-in-Aid for Scientific Research to Y.F (No. 25462223).
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukuda, Y., Horie, N., Satoh, K. et al. Intra-Arterial Transplantation of Low-Dose Stem Cells Provides Functional Recovery Without Adverse Effects After Stroke. Cell Mol Neurobiol 35, 399–406 (2015). https://doi.org/10.1007/s10571-014-0135-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-014-0135-9