Abstract
The use of antibiotic-loaded bone cement (ALBC) is an accepted method for prevention and treatment of infected joint arthroplasties. The prophylactic use of ALBC must be distinguished from its therapeutic use. The prophylactic use of low-dose ALBC in primary cemented total knee arthroplasty is recommended particularly in patients with high-risk profiles in order to reduce the incidence of periprosthetic joint infections and in the setting of aseptic revision knee arthroplasties. The routine use of high-dose ALBC in revision total joint arthroplasty is well accepted as static or articulating spacers in first-stage revision procedures. These spacers provide local delivery of antibiotics while offering stabilization of soft tissues, facilitating the future re-implantation procedure and improving clinical outcomes. Although limited clinical evidence exists on the use of ALBC at the time of definitive component re-implantation after septic revision, the rationale for its use is strong.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Total knee arthroplasty (TKA) is one of the most successful surgical procedures. A condylar design with good cementing technique has been considered the gold standard in TKA, due to the outstanding long-term results of cemented TKA in all age groups. Without stratifying for age, multiple published articles consistently cite a greater than 95% survivorship rate at 20 years (Scuderi et al. 1989; Ranawat et al. 1994; Font-Rodriguez et al. 1997; Milligan et al. 2019; Vessely et al. 2006). The practice of using polymethylmethacrylate (PMMA) in fixation of total joint arthroplasties has been present since its introduction by Sir John Charnley in the 1960s. The utility of PMMA in fixation of components and load distribution is not refuted. Addition of antibiotics to PMMA has been performed for the last 30 years in an effort to reduce the likelihood of infections, as well as part of the treatment of periprosthetic joint infections (PJIs).
Buchholz and Engelbrecht (1970) incorporated antibiotics in PMMA bone cements to reduce the infection rates in orthopedic surgery, assuming that the antibiotic will gradually be released to give higher local concentrations than can be achieved by systemic therapy.
The concept of using bone cement as a depot for antibiotics is attractive, particularly in high-risk patients or complex reconstructions (◘ Fig. 59.1) as it allows for delivery of antibiotics directly to the site of potential infection.
a–d Complex primary TKA in a high-risk patient for PJI. A 67-year-old female patient with severe right knee OA a, severe varus deformity b, ligament instability c, and significant bone loss. She also has a long-standing history of rheumatoid arthritis in immunosuppressive therapy (leflunomide and prednisone) and is considered in the high-risk category for PJI/SSI. She underwent a complex primary constrained cemented TKA using bone autograft augmentation. ALBC was used at a prophylactic dose (1.2 g of tobramycin and 1 g of vancomycin mixed per batch of cement). At 3-year follow-up, her right TKA was functioning well, and there was no evidence of PJI d
The elution profile of antibiotic-loaded bone cement (ALBC) has been evaluated: the elution kinetics of vancomycin, tobramycin, gentamicin, moxifloxacin, and clindamycin are better than cefazolin, daptomycin, meropenem, ertapenem, cefotaxime, ampicillin, amoxicillin-clavulanate, and cefepime (Gálvez-López et al. 2014; Anagnostakos et al. 2009; Chang et al. 2013).
Thus, the two most common antibiotics mixed with bone cement are vancomycin and aminoglycosides such as tobramycin and gentamicin. Recent annual arthroplasty registries have shown that 96.3% of cemented TKAs and 93.7% of total hip arthroplasties (THAs) used ALBC (Australian National Joint Replacement Registry 2018). Plain cement has a slightly higher rate of revision than ALBC when used in TKA (Australian National Joint Replacement Registry 2018). However, the role of ALBC in the prevention of infection still remains a controversial topic (Jiranek et al. 2006; Hendriks et al. 2004; Blomgren and Lindgren 1981).
2 Evidence
Previous evidence has shown that ALBC together with systemic antibiotic prophylaxis was effective in reducing PJI in TKA compared with plain cement and systemic antibiotic prophylaxis (Chiu et al. 2002; Eveillard et al. 2003; Randelli et al. 2010); however, more recent evidence suggests that this question is still debatable. Two recent prospective studies showed that ALBC did not reduce the rate of deep infection following primary TKA compared with plain cement (Wilairatana et al. 2017; Wang et al. 2015). More recently, a systematic review on the use of ALBC in total joint arthroplasty evaluated six articles encompassing 6318 arthroplasties. Among the study population, 3217 of these arthroplasties received ALBC and 3101 arthroplasties using plain cement served as the control. Only two studies showed a significant effect of ALBC in preventing deep infection in primary TKA. Contradictory results were reported in the remaining four prospective and randomized clinical trial studies that showed no statistical difference between the two groups in terms of the incidence of deep or superficial SSIs (Schiavone Panni et al. 2016). In another meta-analysis, Kleppel et al. reported 4092 patients following TKA (3903 primary TKAs and 189 revision TKAs). At an average follow-up time of 47.2 months for primary TKA, the use of ALBC demonstrates a nonsignificant reduction in PJI/SSI; however, there was a significant reduction in revision TKA infection rates in the ALBC group (Kleppel et al. 2017). Additionally, a recent analysis of 731,214 joints from the National Joint Registry (NJR) of England and Wales after adjusting for other variables demonstrated that the use of ALBC had a significantly lower risk of revision for any cause (HR 0.85, 95% CI 0.77–0.93; p < 0.001), as well as reduction of revisions for infection (HR 0.84, 95% CI 0.67–1.01; p = 0.06) (Jameson et al. 2019).
The 2018 Second International Consensus Meeting (ICM) on Musculoskeletal Infection, based on moderate evidence and with super majority-strong consensus, recommended:
Antibiotic-impregnated cement may be used during primary TJA to reduce the risk of surgical site infections/periprosthetic joint infections. The benefits of antibiotic-impregnated cement vs. its cost and other potential adverse effects may be most justified in patients at high risk of infection (Parvizi 2019).
3 Indications for Antibiotic-Loaded Bone Cement
The prophylactic use of ALBC for the primary fixation of implants (◘ Fig. 59.1) must be clearly distinguished from its therapeutic use in the staged revision setting.
Considerable variation exists in the use of ALBC in primary TKA; however, given the available evidence we feel that selective use in high-risk patients is warranted.
In contrast, the routine use of ALBC in revision total joint arthroplasty is well accepted, with good supporting evidence in both aseptic and first-stage revision procedures utilizing articulating (◘ Fig. 59.2) or static spacers (◘ Fig. 59.3).
a–c Two-stage revision for chronic PJI with articulating spacer. A 60-year-old male patient with a history of posttraumatic left knee OA who underwent left TKA after smoking cessation optimization a. The postoperative course was complicated with an acute PJI secondary to CoNS failing DAIR and 6 weeks of specific antibiotic therapy, subsequently he presented with infection recurrence, this time with Candida albicans and underwent two-stage revision surgery b with articulating spacer (high-dose antibiotics: 3 g of vancomycin, 3.6 g of tobramycin, 200 mg of amphotericin B per batch of cement, No.3 batch × 40 g of cement in total). The patient received 6 weeks of IV vancomycin and ertapenem, and oral fluconazole (12 weeks). He underwent left TKA re-implantation c using metaphyseal cones, short cemented stems, and ALBC was used at prophylactic dose. He received long-term oral suppressive antibiotic therapy (trimethoprim-sulfamethoxazole and fluconazole) for 6 months postoperatively. At 1-year follow-up after re-implantation, there is no clinical evidence of infection recurrence
a–c Two-stage revision for chronic PJI with static ALBC spacer. A 73-year-old male patient with a history of index left TKA and two aseptic revisions for aseptic loosening, and 1 year after the last revision, he was diagnosed with coagulase-negative Staphylococcus chronic PJI a and underwent two-stage revision surgery with static ALBC spacer b due to the massive bone loss and instability (high-dose antibiotics: 3 g of vancomycin and 3.6 g of tobramycin, per 40 g batch of cement, No.3 batch × 40 g of cement in total). He completed 6 weeks of IV vancomycin. He underwent left TKA re-implantation c using a distal femoral replacement and metaphyseal cones, cemented stems, and ALBC was used at a prophylactic dose (1.2 g of tobramycin, 1 g of vancomycin mixed per batch of cement). He received long-term oral suppressive antibiotic therapy (doxycycline) for 6 months postoperatively. At 1.5-year follow-up after re-implantation, there is no clinical evidence of infection recurrence
Although limited clinical evidence exists on the use of ALBC at the time of definitive component re-implantation after septic revision, the rationale for its use is strong.
Prophylactic and Therapeutic Use of ALBC
-
Prophylactic—low-dose antibiotic (<1.2 g of antibiotic per 40 g pack of cement):
-
Primary TKA in high-risk groups for PJI*.
-
Revision TKA (aseptic revision and re-implantation).
-
-
Therapeutic—high-dose antibiotic (>3 g of antibiotic per 40 g pack of cement):
-
First stage of a two-stage revision procedure in the antibiotic spacer.
-
Per 40 g pack of cement: 3 g of vancomycin and 3.6 g of tobramycin; if fungal infection is present or suspected, 150–200 mg of amphotericin B is added.
-
*Host risk factors for SSI/PJI in TJA: chronic kidney disease, diabetes mellitus, malnutrition, immunosuppression, rheumatoid arthritis, HIV/AIDS, peripheral vascular disease, obesity, smoking, clotting disorders, chronic obstructive pulmonary disease, untreated hepatitis C, MRSA colonization, chronic anticoagulation, previous joint surgery, previous joint infection, transplant, osteonecrosis, posttraumatic osteoarthritis, bariatric surgery (Parvizi 2019).
Although there is no consensus about the definition of high-dose ALBC, it is generally accepted that a dose higher than 2 g of antibiotic per 40 g of cement represents a high-dose ALBC (Hanssen and Spangehl 2004).
4 Industrially Manufactured Versus “Homemade” Preparations of ALBC
Commercially available ALBCs offer different options of viscosity (low, medium, and high viscosity) and antibiotics for the surgeon. The most common brands are included in ◘ Table 59.1; however, several concerns remain about having readily available ALBCs. Typically, aminoglycosides are included in the commercially ALBC, providing coverage against Gram-negative bacteria including Pseudomonas, Proteus, Escherichia coli, Klebsiella pneumoniae, Enterobacteriaceae, Serratia, and the Gram-positive Staphylococcus. However, tobramycin has the added benefit of superior activity against Pseudomonas. Additionally, vancomycin potentially has a higher antimicrobial activity when compared with gentamicin for methicillin-resistant Staphylococcus aureus (MRSA) while remaining heat-stable with adequate elution (Tunney et al. 1998; Kuechle et al. 1991; Adams et al. 1992). Studies have raised concerns regarding the following:
-
Increasing microbial resistance
-
Insufficient dose of antibiotic
-
Additional unnecessary cost
-
Reduced mechanical properties of the commercial preparations (Frew et al. 2017)
We must also consider the cost associated with the use of the ALBC. In the United States, the average cost of 1 pack (40 g) of industrially manufactured ALBC is somewhere between $215 and $325, compared to homemade preparations using pain cement that could be around $100. In a recent systematic review about cost implications of ALBC, King et al. conclude that hospital systems performing 1000 TKAs per year could save between $155,000 and $310,000 per year by switching to plain-cement homemade preparations (King et al. 2018). Industrially manufactured ALBC may be preferred due to the ease of access and time saving. However, biomechanical and elution testing has demonstrated that 1 g of vancomycin in homemade ALBC can reduce cost without compromising the mechanical strength or elution of the drug (Lee et al. 2016). Furthermore, a recent study comparing the elution properties of commercially available ALBC with homemade preparations using high-performance liquid chromatography mass spectrometry observed the highest peak concentrations of antibiotics from the homemade cements containing vancomycin added in the operating theater. The overall elution of antibiotics was fivefold (vancomycin) and twofold (gentamicin) greater from the homemade mix compared with commercially mixed cement (Frew et al. 2017).
Considering the excellent elution properties and lower costs associated with the preparation of homemade ALBC in the operating theater by hand, it seems there is no significant advantage of using expensive commercially available ALBC.
4.1 Relevant Tips/Tricks of “Homemade” ALBC Articulating Spacers: Authors’ Preferred Technique
Implants/Materials Needed
-
Cruciate-retaining (CR) or posterior stabilized (PS) femoral component
-
All-polyethylene CR or PS tibial component
-
Bone Cement × 40 g pack (usually 3–4 batches are needed):
-
3 g of vancomycin powder per batch
-
3.6 g of tobramycin powder per batch
-
150 mg of amphotericin B powder per batch (if concerns for fungal infection)
-
Methylene blue 1 mL per batch
-
Mineral oil
-
Two cement guns to make dowels
-
Disposable cement spatula
-
Hand-mixed
-
4.2 Technical Tips for Mixing ALBC (◘ Fig. 59.4)
High volumes of antibiotic powder make mixing difficult if the antibiotic and cement powders are mixed together before introducing the liquid monomer.
ALBC Preparation—work on the back table. The cement powder and the liquid monomer are mixed together first until a fluid and homogeneous mixture is obtained. Then, 1 mL/batch of methylene blue is added, and antibiotics (powder) are added finally. The mixture is gently mixed with a spatula. The cement syringe nozzle tubes are generously covered with mineral oil inside in order to prevent adherence of the cement. Tibial augments can also be made and are useful in the case of a gap mismatch
It is rather recommended to first mix together the PMMA monomer and powder to form the liquid cement, followed by adding 1 mL/batch of methylene blue to obtain a homogeneously blue and fluid cement. Subsequently, the antibiotic powder is slowly added.
Vancomycin powder and some generic brands of tobramycin are crystalline in nature, which can make mixing difficult. It is preferable to leave many of the large crystals intact when preparing ALBC for use as beads or spacers because this makes a more porous mixture, which facilitates a higher volume of antibiotic elution.
In contrast, when mixing crystalline antibiotics into cement to be used for prosthesis fixation, the crystals should be pulverized with a mortar and pestle before being added to the liquid cement because the crystalline defects significantly weaken the cement.
Step 1: Prepare Intramedullary Dowels and Augments of ALBC
Medullary dowels were popularized by Dr. Arlen Hanssen (Hanssen and Spangehl 2004) from Mayo Clinic, Rochester, MN, and have the advantages to provide a local-delivery antibiotic system in the medullary canal and facilitate its removal during re-implantation. To optimize time, this can be performed prior to incision at the back table working area using one batch 40 g of cement, and 2 dowels of cement (10–15 cm long) are prepared by introducing high-dose ALBC into the cement gun nozzle tube, providing an excellent size and shape for a spacer to be inserted into the medullary canal (◘ Fig. 59.5). The cement gun nozzle has been previously spread in the interior surface with sterile mineral oil to facilitate the extraction.
a–d Bone preparation and trialing. After a thorough synovectomy, the proximal tibia and distal femur are refreshed a. Flexion b and extension c gaps are assessed, which helps anticipate any flexion/extension mismatch and, therefore, the use of previously made ALBC augments. Then multiple liner options (d) are put in place in order to obtain a balanced knee
It is important to create a small bulb at the end of the dowel to prevent migration into the femoral or tibial canal.
In roughly 1/3 of infected knee replacements without stems, there is extension of the infectious process into the medullary femoral or tibial canals (Hanssen and Spangehl 2004), and antibiotic beads in the medullary canals can be extremely difficult to remove at re-implantation. Also, 5-mm augments for the tibial and femur (distal and posterior) augments could be made using trial components, previously spread with mineral oil (◘ Fig. 59.4).
Step 2: Refreshing the Cuts, Femur and Tibia Preparation (◘ Fig. 59.5)
After the infected implants are removed, a thorough synovectomy is performed. The tibia is prepared perpendicular to its mechanical axis. The intramedullary canal is reamed (usually up to 12–13 cm) and a minimal refreshing proximal cut is performed. Then, we proceed with the femoral preparation. The femoral component should be sized to fit the remaining distal femur in the sagittal plane. An intramedullary guide is placed. The distal femur cut is refreshed using a cutting guide with the proper rotation. The remaining cuts of the femur are refreshed (by either free-hand or using the 4-in-1 cutting block). This helps with the debridement of the remaining bone cement as well. A box for a PS implant is prepared if this is needed. Subsequently, assessment of the extension and flexion gaps is performed with the use of a laminar spreader in both extension and flexion, obtaining the respective gap measurement with a ruler (◘ Fig. 59.5b, c). If a gap mismatch is anticipated (as usually happens), some ALBC femoral and/or tibial augments could be made according to the previous assessment or at the beginning with the residual ALBC during the preparation of the medullary dowels. A trial is then placed. Multiple liner options are trialed to achieve appropriate stability in flexion/extension (◘ Fig. 59.5d).
The trial implants are removed, and irrigation is performed. We use a total of 0.35% povidone-iodine solution for 3 minutes followed by pulse lavage, then disinfection with 1 L of 0.05% chlorhexidine gluconate (IrriSept) for another 3 minutes, and finally high-pressure pulse lavage irrigation with 6 L of sterile saline. We change the drapes for clean drapes. The tourniquet is released, and hemostasis is obtained. We change gloves and then proceed with cementation of the implants.
Step 3: Femoral and Tibial Implant Preparation and Cementation (◘ Fig. 59.6)
The tip of the all-polyethylene tibial component is removed with an oscillating saw in order to accommodate for the tibial dowel. Both medullary ALBC dowels are placed into the respective medullary canal, followed by gentle cementation of the bony surfaces of the femur and the tibia. While the cement is curing, small holes should be made for future cement interdigitations (this can be achieved with a freer). The all-polyethylene tibial implant and femoral components are precoated with cement (if ALBC augments are used, they must be included at this point) and impacted gently until fully seated, starting with the tibia and then applying the femoral component in deep knee flexion. Once the femur is seated, the knee is compressed in extension until the cement is dry. Any gaps between the femoral component and host bone can be filled with cement (◘ Fig. 59.6).
4.3 Antibiotic Elution from “Homemade” High-Dose ALBC Spacers
Antibiotics used in “homemade” cement spacers must be water-soluble, thermostable, and available in powder form. Therefore, not all antibiotics can be mixed into bone cement.
During polymerization, the exothermic reaction produces heat, ranging from 70 to 120 °C in vitro (Monzón et al. 2019), which warrants the use of heat-stable antibiotics.
Thus, the most commonly used antibiotics are gentamicin, tobramycin, vancomycin, and cefazolin. Elution of antibiotics from high-dose ALBC spacers depends on the concentration of antibiotics used, the brand of cement from which the mixing is made, the mixing methods, and porosity .
Lee et al. (2016) added 4 g of vancomycin (from three different manufacturers) into four different types of surgical-grade bone cements. Their elution study showed a constant burst release during the first hour, and then a plateau was reached at 72 hours. The authors also showed that regardless of the vancomycin manufacturer, Palacos cement resulted in the highest cumulative elution.
Mixing two antibiotics has been shown to increase elution.
Paz et al. (2015) investigated the effect of adding cefazolin to vancomycin in high-dose ALBC. Their results showed that elution was significantly increased when cefazolin was added. Moreover, Hanssen et al. (2004) showed that mixing high-dose antibiotics creates considerable cement porosity facilitating elution for at least 4 weeks.
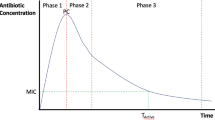
Interestingly, Martinez-Moreno et al. (2014) investigated the elution properties of 11 different antibiotics used in high-dose ALBC spherical beads for 30 days. Throughout the course of the investigation, the authors showed a triphasic pattern of elution with a progressive increase in the first 24 hours, then a rapid decrease, and a final phase of low and steady decline. Among the tested antibiotics, three were shown to be poor candidates (ampicillin, amoxicillin clavulanate, and cefepime) with undetectable concentrations at day 4.
Miller et al. (2012) compared three different mixing methods:
-
Hand-stirred with bowl and spatula
-
Bowl-mixed using a mechanical mixing bowl
-
Dough-phase mixing with vancomycin left in chunks (1–5 mm)
Their elution analysis showed that dough-phase mixing leads to greater release. Several studies have investigated antibiotic levels at longer time points. Hsieh et al. (2006) mixed 4 g of vancomycin and 4 g of aztreonam with 40 g of cement. Their results showed that at a mean of 107 days after surgery, the concentration of antibiotics in the joint fluid was well above the minimal inhibitory concentration (MIC). Masri et al. (1998) blended high-dose tobramycin (between 1.2 and 4.8 g) and vancomycin (1–2 g) to 40 g of bone cement and implanted a knee Prostalac in 15 patients. The re-implantation was performed at a mean of 118 days. At that time, the authors showed that the use of at least 3.6 g of tobramycin and 1 g of vancomycin per cement batch was necessary to maintain intra-articular concentrations above the MIC.
4.4 Potential Complications of High-Dose ALBC Spacers
Considering the potential adverse effects of ALBC, it is important to distinguish between its prophylactic use (low-dose) and its high-dose use during the first stage of a two-stage revision procedure.
For routine use of low-dose ALBC, Hansen et al. (2014) have shown no notable increase in bacteria resistance or changes in infecting pathogen profile. Otherwise, to date, no medical systemic complications have been reported with the use of low-dose ALBC (Gandhi et al. 2018).
Potential complications are associated with the use of high-dose ALBC. Thus, there are several case reports of nephrotoxicity (acute renal injury/failure) associated with the addition of aminoglycosides or other antibiotics in ALBC knee spacers (Geller et al. 2017; Menge et al. 2012; Aeng et al. 2015; James and Larson 2015; van Raaij et al. 2002; Curtis et al. 2005; Patrick et al. 2006; Roman and Slama 2015; Salim et al. 2018; Song et al. 2010; Berliner et al. 2018).
Monitoring the renal function is recommended during and in the case of ongoing renal dysfunction; removal of the spacer as soon as possible should be considered.
Song et al. (2010) reported a case of a 69-year-old woman who developed pain, fever, generalized skin rash, and abnormal laboratory findings around 2 weeks after the placement of a spacer with high-dose piperacillin/tazobactam. Aeng et al. (2015) investigated a series of patients treated with an ALBC spacer with a high dose of tobramycin (3.6 g) and a moderate dose of vancomycin (1.5 g). The authors showed an incidence of acute kidney injury (AKI) of 20%. Interestingly, they also found two risk factors associated with AKI: intraoperative blood transfusion and postoperative treatment with NSAIDs.
Williams et al. (2014) described a case of a patient developing a painful blistering rash during the week following a TKA cemented with ALBC containing 2 g of vancomycin. However, the patient had a history of Stevens–Johnson syndrome to IV vancomycin 6 years prior. Such a history of life-threatening allergy reaction would represent the only contraindication to the addition of a specific antibiotic. Otherwise, there is no published contraindication to the use of high-dose ALBC.
Take-Home Messages
-
ALBC in TKA could be used as a method of prophylaxis as compared with the treatment of an established PJI.
-
Prophylactic ALBC (low dose): use in high-risk group patients in the setting of primary or revisions, therapeutic use (high dose): during the first-stage revision TKA for spacers (articulating or static).
-
Homemade ALBC is cost-effective, providing excellent elution and mechanical properties with lower costs compared to commercial preparations.
-
Antibiotic powder is preferred over liquid to improve elution and mechanical properties.
-
The authors recommended the following sequence of mixing:
-
1.
Mix liquid monomer and powder to create a liquid cement.
-
2.
Add 1 cc of methylene blue/batch of cement for visualization purposes.
-
3.
Add antibiotic powder.
-
1.
References
Adams K, Couch L, Cierny G, Calhoun J, Mader JT (1992) In vitro and in vivo evaluation of antibiotic diffusion from antibiotic-impregnated polymethylmethacrylate beads. Clin Orthop Relat Res 278:244–252
Aeng ESY, Shalansky KF, Lau TTY, Zalunardo N, Li G, Bowie WR, Duncan CP (2015) Acute kidney injury with tobramycin-impregnated bone cement spacers in prosthetic joint infections. Ann Pharmacother 49(11):1207–1213
Anagnostakos K, Wilmes P, Schmitt E, Kelm J (2009) Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop 80(2):193–197
Australian National Joint Replacement Registry, Annual Report 2018. https://aoanjrr.sahmri.com/annual-reports-2018
Berliner ZP, Mo AZ, Porter DA, Grossman JM, Hepinstall MS, Cooper HJ, Scuderi GR (2018) In-hospital acute kidney injury after TKA revision with placement of an antibiotic cement spacer. J Arthroplast 33(7S):S209–S212
Blomgren G, Lindgren U (1981) Late hematogenous infection in total joint replacement: studies of gentamicin and bone cement in the rabbit. Clin Orthop Relat Res 155:244–248
Buchholz HW, Engelbrecht H. Uber die Depotwirkung einiger Antibiotica bei Vermischung mit dem Kunstharz Palacos [Depot effects of various antibiotics mixed with Palacos resins]. Chirurg. 1970 Nov;41(11):511–5. German. PMID: 5487941.
Chang Y, Tai CL, Hsieh PH, Ueng SWN (2013) Gentamicin in bone cement: a potentially more effective prophylactic measure of infection in joint arthroplasty. Bone Joint Res 2(10):220–226
Chiu F-Y, Chen C-M, Lin C-FJ, Lo W-H (2002) Cefuroxime-impregnated cement in primary total knee arthroplasty: a prospective, randomized study of three hundred and forty knees. J Bone Joint Surg Br Vol 84(5):759–762
Curtis JM, Sternhagen V, Batts D (2005) Acute renal failure after placement of tobramycin-impregnated bone cement in an infected total knee arthroplasty. Pharmacotherapy 25(6):876–880
Eveillard M, Mertl P, Tramier B, Eb F (2003) Effectiveness of gentamicin-impregnated cement in the prevention of deep wound infection after primary total knee arthroplasty. Infect Control Hosp Epidemiol 24(10):778–780
Font-Rodriguez DE, Scuderi GR, Insall JN (1997) Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res 345:79–86
Frew NM, Cannon T, Nichol T, Smith TJ, Stockley I (2017) Comparison of the elution properties of commercially available gentamicin and bone cement containing vancomycin with ‘home-made’ preparations. Bone Joint J 99(B-1):73–77
Gálvez-López R, Peña-Monje A, Antelo-Lorenzo R, Guardia-Olmedo J, Moliz J, Hernández-Quero J, Parra-Ruiz J (2014) Elution kinetics, antimicrobial activity, and mechanical properties of 11 different antibiotic loaded acrylic bone cement. Diagn Microbiol Infect Dis 78(1):70–74
Gandhi R, Backstein D, Zywiel MG (2018) Antibiotic-laden bone cement in primary and revision hip and knee arthroplasty. J Am Acad Orthop Surg 26(20):727–734
Geller JA, Cunn G, Herschmiller T, Murtaugh T, Chen A (2017) Acute kidney injury after first-stage joint revision for infection: risk factors and the impact of antibiotic dosing. J Arthroplast 32(10):3120–3125
Hansen EN, Adeli B, Kenyon R, Parvizi J (2014) Routine use of antibiotic laden bone cement for primary total knee arthroplasty: impact on infecting microbial patterns and resistance profiles. J Arthroplast 29(6):1123–1127
Hanssen AD, Spangehl MJ (2004) Practical applications of antibiotic-loaded bone cement for treatment of infected joint replacements. Clin Orthop Relat Res 427:79–85
Hendriks JGE, van Horn JR, van der Mei HC, Busscher HJ (2004) Backgrounds of antibiotic-loaded bone cement and prosthesis-related infection. Biomaterials 25(3):545–556
Hsieh P-H, Chang Y-H, Chen S-H, Ueng SWN, Shih C-H (2006) High concentration and bioactivity of vancomycin and aztreonam eluted from simplex cement spacers in two-stage revision of infected hip implants: a study of 46 patients at an average follow-up of 107 days. J Orthop Res 24(8):1615–1621
James A, Larson T (2015) Acute renal failure after high-dose antibiotic bone cement: case report and review of the literature. Ren Fail 37(6):1061–1066
Jameson SS, Asaad A, Diament M, Kasim A, Bigirumurame T, Baker P, Mason J, Partington P, Reed M (2019) Antibiotic-loaded bone cement is associated with a lower risk of revision following primary cemented total knee arthroplasty: an analysis of 731,214 cases using National Joint Registry data. Bone Joint J 101(B-11):1331–134
Jiranek WA, Hanssen AD, Greenwald AS (2006) Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J Bone Joint Surg Br Vol 88(11):2487–2500
King JD, Hamilton DH, Jacobs CA, Duncan ST (2018) The hidden cost of commercial antibiotic-loaded bone cement: a systematic review of clinical results and cost implications following Total knee arthroplasty. J Arthroplast 33(12):3789–3792
Kleppel D, Stirton J, Liu J, Ebraheim NA (2017) Antibiotic bone cement's effect on infection rates in primary and revision total knee arthroplasties. World J Orthop 8(12):946–955
Kuechle DK, Landon GC, Musher DM, Noble PC (1991) Elution of vancomycin, daptomycin, and amikacin from acrylic bone cement. Clin Orthop Relat Res 264:302–308
Lee S-H, Tai C-L, Chen S-Y, Chang C-H, Chang Y-H, Hsieh P-H (2016) Elution and mechanical strength of vancomycin-loaded bone cement: in vitro study of the influence of brand combination. PLoS One 11(11):e0166545
Masri BA, Duncan CP, Beauchamp CP (1998) Long-term elution of antibiotics from bone-cement: an in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J Arthroplast 13(3):331–338
Menge TJ, Koethe JR, Jenkins CA, Wright PW, Shinar AA, Miller GG, Holt GE (2012) Acute kidney injury after placement of an antibiotic-impregnated cement spacer during revision total knee arthroplasty. J Arthroplasty 27(6):1221–1227.e1221–1222
Miller R, McLaren A, Leon C, McLemore R (2012) Mixing method affects elution and strength of high-dose ALBC: a pilot study. Clin Orthop Relat Res 470(10):2677–2683
Milligan DJ, O’Brien S, Doran E, Gallagher NE, Beverland DE (2019) Twenty-year survivorship of a cemented mobile bearing total knee arthroplasty. Knee 26(4):933–940
Monzón RA, Coury JG, Disse GD, Lum ZC (2019) Bone cement in total hip and knee arthroplasty. JBJS Rev 7(12):e6
Parvizi J, Gehrke T. Part IX: biofilm. In: Parvizi J, Gehrke T, eds. Proceedings of the second international consensus meeting on musculoskeletal infection: data trace. 2019:959–982
Patrick BN, Rivey MP, Allington DR (2006) Acute renal failure associated with vancomycin- and tobramycin-laden cement in total hip arthroplasty. Ann Pharmacother 40(11):2037–2042
Paz E, Sanz-Ruiz P, Abenojar J, Vaquero-Martín J, Forriol F, Del Real JC (2015) Evaluation of elution and mechanical properties of high-dose antibiotic-loaded bone cement: comparative “in vitro” study of the influence of vancomycin and cefazolin. J Arthroplast 30(8):1423–1429
Ranawat CS, Flynn WF, Deshmukh RG (1994) Impact of modern technique on long-term results of total condylar knee arthroplasty. Clin Orthop Relat Res 309:131–135
Randelli P, Evola FR, Cabitza P, Polli L, Denti M, Vaienti L (2010) Prophylactic use of antibiotic-loaded bone cement in primary total knee replacement. Knee Surg Sports Traumatol Arthrosc 18(2):181–186
Roman C, Slama TG (2015) Acute renal failure related to implanted antibiotic-impregnated cement joint spacer. Infect Dis Clin Pract 23(3):e15–e16
Salim SA, Everitt J, Schwartz A, Agarwal M, Castenada J, Fülöp T, Juncos LA (2018) Aminoglycoside impregnated cement spacer precipitating acute kidney injury requiring hemodialysis. Semin Dial 31(1):88–93
Schiavone Panni A, Corona K, Giulianelli M, Mazzitelli G, Del Regno C, Vasso M (2016) Antibiotic-loaded bone cement reduces risk of infections in primary total knee arthroplasty? A systematic review. Knee Surg Sports Traumatol Arthrosc 24(10):3168–3174
Scuderi GR, Insall JN, Windsor RE, Moran MC (1989) Survivorship of cemented knee replacements. J Bone Joint Surg Br Vol 71(5):798–803
Song EK, Seon JK, Jeong MS (2010) Delayed-type hypersensitivity reaction to piperacillin/tazobactam in a patient with an infected total knee replacement. J Bone Joint Surg Br Vol 92(11):1596–1599
Tunney MM, Ramage G, Patrick S, Nixon JR, Murphy PG, Gorman SP (1998) Antimicrobial susceptibility of bacteria isolated from orthopedic implants following revision hip surgery. Antimicrob Agents Chemother 42(11):3002–3005
van Raaij TM, Visser LE, Vulto AG, Verhaar JAN (2002) Acute renal failure after local gentamicin treatment in an infected total knee arthroplasty. J Arthroplast 17(7):948–950
Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ (2006) The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res 452:28–34
Wang H, Qiu G-X, Lin J, Jin J, Qian W-W, Weng X-S (2015) Antibiotic bone cement cannot reduce deep infection after primary total knee arthroplasty. Orthopedics 38(6):e462–e466
Wilairatana V, Sinlapavilawan P, Honsawek S, Limpaphayom N (2017) Alteration of inflammatory cytokine production in primary total knee arthroplasty using antibiotic-loaded bone cement. J Orthop Traumatol 18(1):51–57
Williams B, Hanson A, Sha B (2014) Diffuse desquamating rash following exposure to vancomycin-impregnated bone cement. Ann Pharmacother 48(8):1061–1065
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer-Verlag GmbH, DE, part of Springer Nature
About this chapter
Cite this chapter
Prieto, H.A., Gibon, E. (2022). Antibiotic-Loaded Bone Cement in Total Knee Arthroplasty. In: Hansen, E., Kühn, KD. (eds) Essentials of Cemented Knee Arthroplasty. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-63113-3_59
Download citation
DOI: https://doi.org/10.1007/978-3-662-63113-3_59
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-63112-6
Online ISBN: 978-3-662-63113-3
eBook Packages: MedicineMedicine (R0)