Abstract
In this chapter, the combination of ultrasound and other physical enhancers, such as injections, electroporation, microneedles, and microdermabrasion, as well as the simultaneous use of low-frequency and high-frequency ultrasound, for enhanced transdermal delivery applications, is discussed. Although the field of sonophoresis is over 70 years old, there are surprisingly few reported studies aimed at combining ultrasound with other physical enhancers, except for iontophoresis. Further, many of the studies have been conducted in a proof-of-concept manner, with emphasis on the feasibility of the underlying idea, but with limited mechanistic discussion. In other words, the underlying fundamental interactions between ultrasound and other physical enhancers are not well understood, which provides an interesting area of potential future research.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Dual frequency
- Electroporation
- Microdermabrasion
- Microneedles
- Phonophoresis
- Physical enhancer
- Sonophoresis
- Ultrasound
1 Introduction
The use of ultrasound to improve transdermal delivery of therapeutics dates back to the middle of the last century, and despite its long history relative to other transdermal delivery methods, it did not receive considerable attention until recent advances in the fundamental understanding of the technology were made during the last two decades (Polat et al. 2010, 2011a). An important contemporary milestone in the field was the switch from therapeutic or high-frequency ultrasound (HFU) (>0.7 MHz) to low-frequency ultrasound (<100 kHz) when treating skin (Mitragotri et al. 1995). Since this rejuvenation of the technology, the use of ultrasound for delivering drugs to, or through, the skin, also known as sonophoresis, has garnered considerable attention in both academic and clinical settings (Polat et al. 2010, 2011a; Schoellhammer et al. 2014). The novelty of sonophoresis as a physical penetration enhancer, and especially with low-frequency sonophoresis, is that the mechanism of action is indirect. Specifically, the wealth of research in this area has shown that the main mechanism of transdermal enhancement with low-frequency sonophoresis is the ability of ultrasound to create cavitation bubbles and the subsequent action of these gaseous bubbles on the skin (Polat et al. 2011a, 2012). This can allow for generally milder treatments, because the aqueous coupling solution and dissolved gas primarily interact with the skin while still allowing for tunable treatment parameters by controlling the applied ultrasound frequency, intensity, pulse, and duration of the exposure. In contrast, most other technologies either directly act on the skin itself (i.e., laser ablation or microneedles) or act on the solute being delivered (i.e., iontophoresis of charged species). Due to these attributes, sonophoresis allows for some unique opportunities to exploit its enhancement mechanisms in combination with other enhancers to create synergies. To date, the most common of these combination therapies utilizing ultrasound have been with chemical enhancers, specifically surfactants, and/or iontophoresis, which are reviewed in Chapters. 25 and 29 of Volume 4, respectively. In this chapter, the combination of sonophoresis with other physical enhancers will be discussed. Specifically, the focus of this chapter will be the combination of ultrasound with injections (Sect. 23.2), electroporation (Sect. 23.3), microneedles (Sect. 23.4), microdermabrasion (Sect. 23.5), and other frequencies of ultrasound (Sect. 23.6) for transdermal applications.
2 Combination of Ultrasound and Injections
Despite using ultrasound primarily for physical therapy applications during its early years of use in medicine, it is interesting to note that multiple studies, dating to the 1950s, document the combined use of steroid injections with therapeutic (~1 MHz) ultrasound (Newman et al. 1958; Coodley 1960). Although these applications may not fit a strict definition of transdermal delivery as one may envision today, they are significant because they demonstrate that the unique attributes of ultrasound were attempted to be combined with more common drug delivery methods of the time. In fact, the mechanism of cavitation is even mentioned in a publication of this period (Mune and Thorseth 1963), indicating that there was some understanding of the mechanisms of ultrasound in medicine at that time.
The first of these studies was reported by Newman et al., who investigated the effect of ultrasound on hydrocortisone injection for the treatment of bursitis of the shoulder (Newman et al. 1958). Ultrasound was applied at 1 MHz and 0.8–3.0 W/cm2, for a duration of 5–10 min, either daily or every 3 days, for a total of 12 treatments. A total of 225 patients were involved in the study, with the authors demonstrating that hydrocortisone injection, in combination with ultrasound treatment, provided equivalent or improved pain scores when compared to the control group. A similar study by Coodley, involving treatment of bursitis or posttraumatic lesions of different joints in the body, showed that the combination of hydrocortisone injection with ultrasound generally provided more rapid recovery for patients (Coodley 1960). Forty-seven patients, with ailments of the shoulder, elbow, knee, ankle, or wrist, were treated with injection followed by ultrasonic therapy (1 MHz, 1–2 W/cm2, 5–6 min treatment duration). In all, only four of the 47 patients observed little or no aid from the combined therapy, with many patients experiencing more rapid recovery and clearing of symptoms that were resistant to other forms of therapy.
3 Combination of Ultrasound and Electroporation
Although not as common as iontophoresis, the combination of sonophoresis with electroporation has been investigated with respect to the delivery of certain model charged species and a moderate molecular weight immunosuppressant drug (see Table 23.1) (Kost et al. 1996; Liu et al. 2006, 2010). Electroporation is the process of increasing skin permeability by applying a high-voltage, pulsed electric field across the skin and has been shown to act by the mechanism of electrophoresis, electroosmosis, and enhanced diffusion through the formation of transient, aqueous channels in the skin (Prausnitz et al. 1993; Denet et al. 2004). The first published investigation into the simultaneous combination of high-frequency ultrasound (HFU) and electroporation was conducted by Kost et al. (1996). In this study, the transport of two model permeants, calcein and sulforhodamine, were investigated in response to 10–150 V electric pulses (1 millisecond every min) in combination with 1 and 3 MHz HFU at an intensity of 1.4 W/cm2. Although no increase in skin permeability to either model permeant was observed with HFU alone, the combination of 1 MHz HFU and electroporation increased the flux of calcein by a factor of 2 and that of sulforhodamine by a factor of 3, compared to the enhancements observed by electroporation alone. Further, the lag time to steady-state diffusion across the skin was decreased by 40 %, relative to the case of electroporation alone, from 15 to 9 min. However, when 3 MHz ultrasound was applied in place of 1 MHz ultrasound, very little synergism with electroporation was observed. This led the authors to conclude that the mechanism of synergism between HFU and electroporation was cavitation-induced disordering of the skin’s lipid bilayers and convection across the skin, as cavitational effects are inversely proportional to ultrasound frequency. Furthermore, the authors concluded that convection-induced enhancement was dependent on the properties of the permeant considered. For example, the electric field played a larger role in the flux enhancement of the more highly charged calcein (total charge of −4) than in the transport of sulforhodamine (total charge of −1) across the skin, due to the role of electrophoresis (Kost et al. 1996).
In another series of studies, Liu et al. investigated the effect of chemical enhancers, ultrasound, and electroporation treatment, either individually or in-series, on the transdermal uptake and delivery of the uncharged immunosuppressant Cyclosporine A (molecular weight of ~1200 g/mol) (Liu et al. 2006, 2010). Note that the treatment modality in this case is significantly different than in the study conducted by Kost et al. (Kost et al. 1996), because the electroporation, ultrasound, and chemical enhancer treatments were all decoupled and occurred in series, rather than with simultaneous application. In both publications by Liu et al., if applied, chemical enhancers (azone, sodium cholate, sodium thiosulfate, menthol, N-Methyl pyrrolidine, dimethyl sulfoxide, and sodium dodecyl sulfate at varying concentrations in ethanol or water), were utilized first to treat skin samples for an incubation time of 2 h. The chemical enhancer solution was then replaced with a 0.5 % Cyclosporine A in 60 % saline/40 % ethanol solution to be used as the coupling medium for both electroporation and ultrasound treatment. Then, if applied, the skin was treated with 110 V electric pulses every 20 s (300 ms pulse length) for 10–20 min. Finally, if applied, ultrasound treatment was conducted, at a frequency of 20 kHz, an intensity of 0.8 W/cm2, a 50 % pulse length (1 s ON: 1 s OFF), a transducer to skin distance of 0.5 cm, and a total treatment time of 30 min (Liu et al. 2006, 2010). Based on the mode of treatment of each enhancer in these studies, which effectively decoupled their ability to interact with one another, one would not expect to observe a large extent of synergism, which was the case. Only modest enhancements over controls were reported when ultrasound and electroporation were combined, with slightly higher delivery when a trimodal treatment, including an azone pretreatment, was utilized. These mild “synergistic” interactions were attributed to partial disorganization of the stratum corneum lipids, making them more susceptible to the other modes of treatment (Liu et al. 2006, 2010). Subsequent histological examination of the skin under these different treatment regimens showed no evidence of structural damage. Subsequent studies have further investigated the use of in-series treatment utilizing electroporation (1 ms, 300 V pulses) followed by 20 kHz ultrasound at 6.1 W/cm2 for 2 min for the delivery of 4.4 kDa dextran labeled with fluorescein isothiocyanate (Petchsangsai et al. 2014). A synergistic increase in the measured flux was achieved compared to the flux achieved with either method alone (Petchsangsai et al. 2014). Other studies have noted only minimal enhancement as a result of the combination of electroporation with ultrasound utilizing an in-series treatment regimen, suggesting that the method is highly regimen dependent (Zorec et al. 2015).
4 Combination of Ultrasound and Microneedles
Similar to the work involving sonophoresis and injection combination therapies outlined in Sect. 23.2, recent work by Yoon et al. investigated the combination of an in-series treatment involving microneedle application to the skin coupled with ultrasound therapy (Yoon et al. 2009, 2010). Specifically, the study evaluated the efficacy of ultrasound-assisted glycerol delivery through the skin pretreated with microneedles, for skin optical clearing applications. As the inherent structure of the skin causes significant scattering and low transmission of light, skin optical clearing can be important in the applications of skin diagnosis and therapy. In this study, solid microneedles with a diameter of 70 μm and a length of 500 μm were first utilized to treat ex vivo porcine skin. Subsequently, a 70 % glycerol solution was applied to the treated skin area utilizing 1 MHz ultrasound, at an intensity of 2 W, for up to 60 min. Comparison of the reduced scattering coefficients of treated skin showed that the combination of ultrasound and microneedles resulted in the relative contrast of the skin increasing by over twofold compared to samples treated only with microneedles (Yoon et al. 2009, 2010). Other studies have investigated the combination of microneedles with ultrasound for the delivery of therapeutically relevant small molecules, such as lidocaine, carbohydrates, and model proteins (Han and Das 2013; Petchsangsai et al. 2014; Nayak et al. 2016). Han et al. investigated the use of microneedle application followed by 20 kHz ultrasound for the delivery of bovine serum albumin (Han and Das 2013). Solid microneedles with lengths between 1.2 and 1.5 mm were used followed by sonication with 20 kHz ultrasound at an intensity of 15 W for 10 min. Han et al. found that this method enhanced the permeability of bovine serum albumin approximately tenfold over passive diffusion, and approximately 2.5-fold over the use of either microneedles or ultrasound alone (Han and Das 2013). The delivery of lidocaine was also enhanced using this combination strategy over the use of either microneedles or ultrasound alone (Nayak et al. 2016). Specifically, the delivery of lidocaine from hydrogel formulations was enhanced almost fivefold 30 min after treatment (Nayak et al. 2016). Petchsangsai et al. have also reported synergistic effects of combining microneedle, electroporation, and sonophoresis treatment regimens to deliver 4.4 kDa fluorescein isothiocyanate-dextran. Their findings showed that trimodal application (of all three physical enhancers) provided greater skin permeation of the model compound compared to any dual modality treatment, with no appreciable skin damage observed under any treatment regimen (Petchsangsai et al. 2014).
In contrast to the previously described studies, Chen et al. developed a system involving hollow microneedle arrays through which ultrasound could be transmitted for direct delivery of drugs into the viable epidermis (Chen et al. 2010). The authors manufactured 80 μm in diameter by 100 μm in length hollow microneedles, with a ceramic membrane applied directly to the back of the microneedle array emitting ultrasound at 20 kHz and intensities between 0.1 and 1 W/cm2. The authors demonstrated that the delivery of both small (calcein, MW ~ 623 g/mol) and large (bovine serum albumin, MW ~ 66,430 g/mol) molecules was significantly improved with the sonophoretically enhanced microneedle arrays (SEMAs), relative to each modality individually or to native skin. In fact, the SEMAs increased the flux of both small and large model permeants by approximately an order of magnitude relative to native skin. The authors explained their findings by proposing that cavitation generated in the hollow microneedles, as a result of the applied ultrasound, would cause bulk flow of material through the microneedles, thereby depositing their contents directly into the skin in proximity to the dermal vasculature. Further, heat generated by dissipation of the applied acoustic waves could cause enhanced diffusivity of the drug compounds, as well as increased absorptivity of the surrounding tissue (Chen et al. 2010). Therefore, this novel, fabricated device may be an exciting new advancement in the field of combined transdermal therapies.
5 Combination of Ultrasound and Microdermabrasion
A unique 2008 clinical study by Dudelzak et al. investigated the use of microdermabrasion skin treatments, followed by high-frequency sonophoresis, through a complex containing hyaluronic acid, retinol, and peptide, in the treatment of photo-aged skin (Dudelzak et al. 2008). Microdermabrasion is a process that involves mechanical exfoliation of the skin, which is commonly used for the treatment of photodamage and acne scarring, among other skin conditions. Specifically, inert abrasive crystals, such as aluminum oxide, are propelled at the skin surface and subsequently discarded along with any material removed from the skin. For this study, the authors hypothesized that skin dryness, texture, hue, tone, and the presence of rhytids could be improved by combining the benefits commonly seen from microdermabrasion, followed by the delivery of a topical complex by sonophoresis (Dudelzak et al. 2008).
Patients enrolled in the study were administered once-weekly treatments for a total of 8 weeks, which involved microdermabrasion and subsequent ultrasound-assisted delivery of the photorejuvenating complex (Dudelzak et al. 2008). Ultrasound treatments were administered at a frequency of 3 MHz, an intensity of 1.4 W/cm2, and a duration of 5 min. In between these treatments, patients manually applied the topical complex and sunscreen twice daily. Patients were evaluated both at baseline and at 3 months following the final treatment, by both patient/investigator scoring and histological examination. Histological results showed evidence of increased vasculature, type I and III collagen deposition, and increased collagen fiber diameter, all indicators of injury repair and dermal remodeling by the applied treatment. Investigator and patient scores also demonstrated improvements in all the categories evaluated, suggesting that combined microdermabrasion and ultrasonic delivery of skin rejuvenating products may be an effective way of treating patients with photodamaged skin (Dudelzak et al. 2008).
6 Combination of Multiple Ultrasound Frequencies
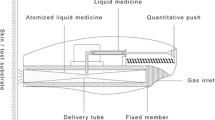
Although the chapter, to this point, has discussed studies involving combinations of sonophoresis with other physical enhancers, a new exciting approach to exploiting the fundamental physical mechanisms of sonophoresis has recently been proposed, through the simultaneous application of low-frequency and high-frequency ultrasound on skin (Schoellhammer et al. 2012). It is well known that the diameter of cavitation bubbles produced by ultrasound is inversely proportional to the applied ultrasound frequency (Polat et al. 2011b, 2012). Therefore, it follows that higher ultrasound frequencies typically produce a larger population of smaller diameter bubbles, while lower frequencies produce a smaller population of larger diameter bubbles. The work of Schoellhammer et al. found that by streaming a large number of bubbles, produced by high-frequency ultrasound (1–3 MHz), across the surface of skin, and subsequently collapsing those bubbles at the skin surface by simultaneously applying low-frequency ultrasound, a much larger and more uniform area of the skin could be permeabilized (Schoellhammer et al. 2012). The setup for the experiments is shown in Fig. 23.1.
Illustration of an experimental setup in which a large population of bubbles are generated with the high-frequency ultrasound horn, parallel to the skin surface (a), followed by application of the low-frequency ultrasound, perpendicular to the skin surface (b), and subsequent collapse of the bubbles in the vicinity of the skin (c) causing perturbation to the skin surface (Reprinted, with permission, from Elsevier) (Schoellhammer et al. 2012)
In these experiments, high-frequency ultrasound at 1 and 3 MHz was investigated, in combination with low-frequency ultrasound at 20, 40, and 60 kHz (Schoellhammer et al. 2012). The intensity of the applied ultrasound was 1.5 W/cm2 and 8 W/cm2 for the high and low frequencies, respectively. In addition to the frequency combinations, the effects of duty cycle (pulsed 1 s ON: 1 s OFF, or continuous) and a chemical enhancer in the coupling solution, sodium lauryl sulfate (SLS), were also investigated. Initial experiments were carried out utilizing a physical dosimeter and aluminum foil pitting, to assess the size and quantity of cavitation bubbles produced by the different treatments. These experiments showed that the number of pits and the total pitted area of samples treated with all frequency combinations, utilizing a phosphate-buffered saline (PBS)-coupling solution, increase dramatically relative to controls in which only low-frequency ultrasound is utilized. When SLS was added to the coupling solution, the results were not as straightforward, however. Specifically, the combination of 20 kHz ultrasound and either 1 or 3 MHz ultrasound was statistically insensitive to the presence of SLS in the coupling solution. However, both 40 kHz and 60 kHz ultrasound, combined with either 1 or 3 MHz ultrasound, caused total pitted area values to drop nearly to the level of control samples treated only with the lower frequency (single-frequency treatment) when SLS was present. The authors explained that this observation was a result of SLS adsorption to the cavitation bubbles inhibiting bubble growth and coalescence, due to electrostatic effects, and a decrease in the surface energy of the bubbles, due to a decrease in the surface tension of the bubbles. Because the 40 kHz and 60 kHz frequencies generate bubbles that are smaller than those generated by the 20 kHz frequency, gas nuclei are not able to grow above the threshold size for cavitation bubbles to form and, therefore, dissolve back into solution due to the Laplace pressure. Further, the authors explained that bubbles that do collapse at the skin surface may be less energetic, due to a decrease in surface tension due to surfactant adsorption, resulting in either smaller pits or in pits that cannot be observed on the aluminum foil. These mechanisms, however, were argued to be less important at 20 kHz, which is supported by the data, because the bubbles would be generally larger at 20 kHz and less sensitive to the Laplace pressure. As a result, these bubbles have sufficient energy to create observable pits on the aluminum foil. Duty cycle was found to have no statistically significant effect in these experiments (Schoellhammer et al. 2012).
The optimal condition observed in the aluminum foil pitting experiments was then utilized to carry out in vitro experiments with porcine skin (Schoellhammer et al. 2012). Specifically, for these experiments, the combination of 20 kHz ultrasound and 1 MHz ultrasound utilizing a 1 % SLS in PBS solution was investigated relative to controls. The results were consistent with the previous pitting experiments, where skin samples treated for 6 min using the dual-frequency approach yielded observable skin perturbation on 27 % of the skin surface, while less than 5 % was observable in samples treated with 20 kHz alone. The transdermal delivery of model low molecular weight (glucose) and high molecular weight (inulin) hydrophilic compounds was also investigated through dual-frequency and single-frequency treated samples. The simultaneous application of 20 kHz and 1 MHz was found to decrease the lag time to delivery of both glucose and inulin through the skin samples. Further, the quantity of glucose delivered using the dual-frequency treatment was enhanced by a factor of 2.7–13.6 times, and the quantity of inulin delivered was enhanced by a factor of 2.0–3.8 times, relative to that delivered with 20 kHz ultrasound alone, in 2–6 min of total treatment time (1–3 min of ultrasound exposure at 50 % duty cycle) (Schoellhammer et al. 2012). The authors concluded that the combination of dual ultrasound frequencies could be optimized to enhance skin permeability more uniformly across the skin surface, which could decrease the necessary treatment area to achieve therapeutic levels of delivery.
In a more recent study, Schoellhammer et al. investigated the mechanism of enhancement and the tolerability of treatment utilizing 20 kHz and 1 MHz ultrasound both in vitro and in vivo (Schoellhammer et al. 2015). Specifically, the authors investigated the flux of 4 kDa dextran across the skin treated with either 20 kHz and 1 MHz ultrasound or 20 kHz ultrasound alone and found a 2.5-fold and sixfold increase in flux at treatment times of 6 and 8 min, respectively. Interestingly, this increase in flux at both treatment times was larger than the increase in the area of the skin that was permeabilized as a result of ultrasound treatment, suggesting that treatment with 20 kHz and 1 MHz ultrasound results in a larger area of the skin being made permeable, with a higher permeability achieved than that using 20 kHz ultrasound alone. Schoellhammer et al. confirmed this result through the estimation of pore sizes in the skin as a result of the treatment utilizing hindered transport theory (Polat et al. 2011b). Indeed resulting pore sizes in the skin treated with 20 kHz and 1 MHz ultrasound were an order of magnitude larger than those generated as a result of treatment with 20 kHz ultrasound alone (Schoellhammer et al. 2015). Dual-frequency ultrasound was also shown by histology to result in a comparable level of tissue perturbation as that achieved with 20 kHz ultrasound alone both in vitro and in vivo, suggesting that this method should be just as tolerable as the use of 20 kHz alone, which is FDA-approved (Schoellhammer et al. 2015).
Conclusions
In this chapter, we have discussed the combination of ultrasound and other physical enhancers, such as injections, electroporation, microneedles, and microdermabrasion, as well as the simultaneous use of low-frequency and high-frequency ultrasound, for enhanced transdermal delivery applications. As discussed, despite a long research history in the area of sonophoresis, few reported studies have focused on the combination of ultrasound and other physical enhancers, except for iontophoresis. Further, many of these studies have been carried out in a proof-of-concept manner, with emphasis on testing the feasibility of the underlying idea, but with little discussion on clinical or practical relevance, as well as with regard to understanding the mechanisms underlying the observed increased enhancements. In other words, the fundamental mechanisms of interaction between ultrasound and other physical enhancers are not that well understood, which provides an interesting area of potential future research.
References
Chen B, Wei J, Iliescu C (2010) Sonophoretic enhanced microneedles array (SEMA)—Improving the efficiency of transdermal drug delivery. Sensors Actuators B Chem 145(1):54–60
Coodley E (1960) Bursitis and post-traumatic lesions: management with combined use of ultrasound and intra-articular hydrocortisone. Am Pract Dig Treat 11:181
Denet AR, Vanbever R, Préat V (2004) Skin electroporation for transdermal and topical delivery. Adv Drug Deliv Rev 56(5):659–674
Dudelzak J, Hussain M, Phelps RG, Gottlieb GJ, Goldberg DJ (2008) Evaluation of histologic and electron microscopic changes after novel treatment using combined microdermabrasion and ultrasound-induced phonophoresis of human skin. J Cosmet Laser Ther 10(4):187–192
Han T, Das DB (2013) Permeability enhancement for transdermal delivery of large molecule using low-frequency sonophoresis combined with microneedles. J Pharm Sci 102(10):3614–3622
Kost J, Pliquett U, Mitragotri S, Yamamoto A, Langer R, Weaver J (1996) Synergistic effect of electric field and ultrasound on transdermal transport. Pharm Res 13(4):633–638
Liu H, Li S, Pan W, Wang Y, Han F, Yao H (2006) Investigation into the potential of low-frequency ultrasound facilitated topical delivery of Cyclosporine A. Int J Pharm 326(1–2):32–38
Liu H, Wang Y, Xu L, Li S-M (2010) Investigation into the potential of electroporation facilitated topical delivery of cyclosporin A. PDA J Pharm Sci Technol 64(3):191–199
Mitragotri S, Blankschtein D, Langer R (1995) Ultrasound-mediated transdermal protein delivery. Science 269:850–853
Mune O, Thorseth K (1963) Ultrasonic treatment of subcutaneous infiltrations after injections. Acta Orthop 33(1–4):347–349
Nayak A, Babla H, Han T, Das DB (2016) Lidocaine carboxymethylcellulose with gelatine co-polymer hydrogel delivery by combined microneedle and ultrasound. Drug Deliv 23(2):668–679
Newman MK, Kill M, Frampton G (1958) Effects of ultrasound alone and combined with hydrocortisone injections by needle or hypospray. Am J Phys Med Rehab 37(4):206–209
Petchsangsai M, Rojanarata T, Opanasopit P, Ngawhirunpat T (2014) The combination of microneedles with electroporation and sonophoresis to enhance hydrophilic macromolecule skin penetration. Biol Pharm Bull 37(8):1373–1382
Polat BE, Blankschtein D, Langer R (2010) Low-frequency sonophoresis: application to the transdermal delivery of macromolecules and hydrophilic drugs. Expert Opin Drug Deliv 7(12):1415–1432
Polat BE, Hart D, Langer R, Blankschtein D (2011a) Ultrasound-mediated transdermal drug delivery: mechanisms, scope, and emerging trends. J Control Release 152(3):330–348
Polat BE, Figueroa PL, Blankschtein D, Langer R (2011b) Transport pathways and enhancement mechanisms within localized and non-localized transport regions in skin treated with low-frequency sonophoresis and sodium lauryl sulfate. J Pharm Sci 100(2):512–529
Polat BE, Deen WM, Langer R, Blankschtein D (2012) A physical mechanism to explain the delivery of chemical penetration enhancers into skin during transdermal sonophoresis — Insight into the observed synergism. J Control Release 158(2):250–260
Prausnitz MR, Bose VG, Langer R, Weaver JC (1993) Electroporation of mammalian skin: a mechanism to enhance transdermal drug delivery. Proc Natl Acad Sci U S A 90(22):10504–10508
Schoellhammer CM, Polat BE, Mendenhall J, Maa R, Jones B, Hart DP, Langer R, Blankschtein D (2012) Rapid skin permeabilization by the simultaneous application of dual-frequency, high-intensity ultrasound. J Control Release 163(2):154–160
Schoellhammer CM, Blankschtein D, Langer R (2014) Skin permeabilization for transdermal drug delivery: recent advances and future prospects. Expert Opin Drug Deliv 11(3):393–407
Schoellhammer CM, Srinivasan S, Barman R, Mo SH, Polat BE, Langer R, Blankschtein D (2015) Applicability and safety of dual-frequency ultrasonic treatment for the transdermal delivery of drugs. J Control Release 202(28):93–100
Yoon J, Park D, Son T, Seo J, Jung B (2009) Enhancement of transdermal delivery of glycerol by micro-needling method combined with sonophoresis. Photonics in dermatology and plastic surgery. SPIE, San Jose, pp 24–29
Yoon J, Park D, Son T, Seo J, Nelson JS, Jung B (2010) A physical method to enhance transdermal delivery of a tissue optical clearing agent: Combination of microneedling and sonophoresis. Lasers Surg Med 42(5):412–417
Zorec B, Jelenc J, Miklavčič D, Pavšelj N (2015) Ultrasound and electric pulses for transdermal drug delivery enhancement: ex vivo assessment of methods with in vivo oriented experimental protocols. Int J Pharm 490(1–2):65–73
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Polat, B.E., Schoellhammer, C.M., Langer, R., Blankschtein, D. (2017). Combined Use of Ultrasound and Other Physical Methods of Skin Penetration Enhancement. In: Dragicevic, N., I. Maibach, H. (eds) Percutaneous Penetration Enhancers Physical Methods in Penetration Enhancement. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53273-7_23
Download citation
DOI: https://doi.org/10.1007/978-3-662-53273-7_23
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53271-3
Online ISBN: 978-3-662-53273-7
eBook Packages: MedicineMedicine (R0)