Abstract
Living systems are exposed to electromagnetic sources, including microwaves, from different sources such as sun, wireless communication technology, household microwave oven, etc. Microwaves are nonionizing but can affect biological systems through their thermal and non-thermal effects. These effects are presented at all levels of organism from subcellular structures to tissues, organs, and biological membranes, including the skin barrier that is the subject of the present chapter. The skin provides a natural barrier against permeation of chemicals, and, therefore, many drugs cannot be delivered transdermally in therapeutic amounts. To overcome this problem, many enhancement strategies have been employed. These enhancement methods are classified as physical methods and chemical penetration enhancers. This chapter introduces the use of microwaves as a novel physical percutaneous penetration enhancement method. It has been shown that microwaves are able to increase permeation of drugs through the skin in an intensity and time-dependent manner. These effects are due to both thermal and non-thermal effects of microwaves on the skin barrier. Skin permeation studies and mechanistic investigation of interaction of microwaves with skin material by Fourier transform infrared spectroscopy (FTIR) show that microwaves might induce their effects through disruption of intercellular lipids of the stratum corneum.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Microwave
- Electromagnetic radiation
- Skin
- Permeation enhancer
- Transdermal delivery
- Biological barrier
- Thermal
- Non-thermal
1 Introduction
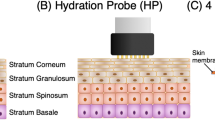
The skin provides a natural barrier against environmental hazards, including permeation of chemicals, and, therefore, many drugs cannot permeate the skin in therapeutic amounts. To overcome this problem, many strategies have been developed over the years including application of the so-called penetration enhancement methods. These enhancement methods are classified as physical methods and chemical penetration enhancers (Williams and Barry 2004; Lu and Flynn 2009). The skin barrier mainly resides in its superficial thin layer, the stratum corneum (SC). The intercellular lamellar structure of the SC is considered as the main pathway for permeation of both hydrophilic and lipophilic drugs (Moghimi et al. 1999) and also a target for most enhancement methods. Besides acting on the stratum corneum and intact viable epidermis, enhancement methods are expected to affect permeation of drugs through skin appendages as well, as was shown by Moghimi et al. (2013) for increased permeation of depilatory agents through hair shaft by chemical penetration enhancers.
The development of new enhancement methods is not closed yet and new methods are being introduced from time to time. This chapter introduces microwaves as a potential physical percutaneous penetration enhancement method. In this chapter, physics of microwaves, their biological effects, their effects on biological barriers, and finally enhancement effects of microwaves on different biological barriers, especially on the skin in order to increase percutaneous absorption of drugs, will be discussed.
2 Microwaves
2.1 Microwaves’ Physics and Applications
Microwaves are part of electromagnetic spectrum with frequencies ranging from 300 MHz to 300 GHz and wavelengths of 1 m to 1 mm (Fig. 10.1). These waves are at higher frequency end of radio waves (30 kHz–300 GHz) (Moulder 1998; Ku et al. 2002; Sorrentino and Bianchi. 2010; Mousa 2011). Therefore, radiofrequencies used for mobile communication (450–2200 MHz) are part of microwave range too (Mousa 2011). However, it is worth to note that there is no specific phenomenon identifying a precise frequency, and similarly, radiofrequency does not correspond to a precise frequency range. But, radiofrequency indicates all frequencies used in radio technology (Sorrentino and Bianchi. 2010; Mousa 2011). Therefore, microwaves are sometimes introduced as a separate band from radiofrequency in the literature.
Humans have always been exposed to natural electromagnetic radiations from different sources such as sun and outer space and even earth (e.g., microwave emission from rocks during compression). Today, living systems are more than ever exposed to this electromagnetic field due to rapid technological progress (Marjanović et al. 2012). Originally, microwaves were mainly used for communication, as they are being used nowadays in wireless communication technology such as mobile phone and television. In 1950s, the use of microwave energy to heat materials was discovered, and since then, microwaves are being used for their ability to heat materials as well. The most common application of microwave heating is the domestic microwave oven (Stuerga and Loupy 2006). However, to avoid interference with telecommunication and cellular phone frequencies, heating devices must use industrial, scientific, and medicinal frequencies (ISM), e.g., 915 and 2450 MHz; domestic ovens and laboratory systems usually work at 2450 MHz (Bradshaw et al. 1998). Microwaves have also been studied for their therapeutic applications in areas such as cardiology, surgery, ophthalmology, cancer therapy, and imaging (Lin 2006; Xie et al. 2006; Kurumi et al. 2007; Lammers et al. 2011; Toutouzas et al. 2012; Celik et al. 2013).
Microwaves provide some benefits over conventional heating methods. As microwave energy is absorbed by certain material, this technique allows selective treatment of material during heating process (e.g., in drying of pharmaceuticals) and prevents heating of other ingredients and containers. Uniformity of warming and higher temperature control in microwave heating prevent overheating of material and also decrease solute migration during drying of pharmaceutical solids (Aulton 2007). Other benefits of microwaves are rapid heating, penetration into the core of material irrespective of thermal conductivities, and higher thermal efficiency (Ku et al. 2002; Aulton 2007). In medical treatments such as microwave ablation, that is, tumor destruction by heating with microwave frequencies, microwaves offer many advantages over other thermoablative technologies, including higher intratumoral temperatures, larger tumor ablation volumes, and faster ablation times. Besides, microwave ablation does not require the placement of grounding pads (Simon et al. 2005).
However, numerous reports have shown that this nonionizing electromagnetic radiation can act as a potential health hazard for living systems, as discussed later. These effects are presented at all levels of organism from subcellular structures to organs and biological membranes, including the skin barrier that is the subject of the present chapter.
2.2 Interaction of Microwaves and Matter
Microwaves are reflected by metallic objects, absorbed by some dielectric materials, and transmitted without significant absorption through some other materials. Water, carbon, and foods with high water content are good microwave absorbers, whereas ceramics and most thermoplastic materials absorb microwaves only slightly (Taylor and Meek 2005; Stuerga and Loupy 2006).
Electromagnetic waves are composed of discrete units of energy called quanta or photons. The energy of these photons (E), that is, a direct function of the frequency of wave (f), can be found from Planck’s equation (Eq. 10.1):
where c is the speed of light in vacuum, h is Planck’s constant, and λ is the wavelength.
The interaction of electromagnetic waves and mater based on their energy radiated can be classified into nonionizing and ionizing. In this classification, microwaves are considered as nonionizing radiation (Vorst et al. 2006), as discussed below.
There are a variety of charges associated with mater: inner or core electrons tightly bound to the nuclei, valence electrons, free or conduction electrons, bound ions in crystals, and free ions in electrolytes. The electromagnetic field can induce oscillation of one or more types of mentioned charges at a frequency close to the natural frequency of the system. It is well known, e.g., that γ-ray or X-ray photons have energies suitable for excitation of inner or core electrons and induce ionization of atoms. The energy of photons by UV radiation is sufficient to induce transition of valence electrons of atoms. Electromagnetic fields in the infrared range induce atomic vibration in molecules only, while microwave band leads to rotation of polar molecules (Stuerga and Loupy 2006; Vorst et al. 2006). The same interactions are expected when human body is exposed to electromagnetic fields.
2.3 Thermal and Non-thermal Effects of Microwaves
Nonionizing radiations, including microwaves, can produce thermal and non-thermal effects, distinguished by the relative size of wavelength versus medium. Heating is the major effect of absorption of electromagnetic energy at frequencies of 10 Hz–300 GHz that induces the motion of charged particles and rotation of molecules, which covers the whole range of microwave radiation (300 MHz–300 GHz) (Challis 2005). If the temperature increase is more than 1 °C, the effect is considered a thermal effect. In such cases, radiation energy and, particularly, specific absorption rate (SAR) are high enough to heat the material (including tissues). The thermal effects are related to the heat generated by the absorption of microwave energy by substances with suitable electronic structure (such as small polar molecules and water), characterized by permanent or induced polarization (Foster and Glaser 2007). In these cases, the electrons try to resonate according to the radiation frequency, and the resulting molecular frictions produce heat in the system (Aulton 2007).
Some radiations, including microwaves and low-level radiofrequency radiation, can cause non-thermal effects, i.e., no obvious increase in temperature (less than 1 °C), where the intensity is not high enough to change the temperature significantly. As discussed later, microwaves show different effects on biological systems due to their non-thermal effects, such as alteration of conformation of macromolecules (like proteins and enzymes), which is said to be due to direct energy transfer from the electromagnetic field to vibration modes of these molecules (Taylor 1981; Porcelli et al. 1997; Laurence et al. 2000). However, contradictory to thermal effects and their hazards that are well documented, non-thermal effects are not well understood and their mechanisms are not fully explored. Non-thermal effects can occur even at power exposure conditions within the recommended safety standard (ICNIRP 1996; Nageswari 2003).
3 Biological Effects of Microwaves and Safety Criteria
Microwaves affect biological systems mainly through deposition of energy in the form of heat (Foster and Glaser 2007). In addition to thermal effects, a non-thermal mechanism does also exist. Non-thermal effects are very important because most common exposure is at low levels of radiofrequency radiation, which induce non-thermal effects (Repacholi 1998). Both effects will be discussed here.
3.1 Thermal Effects of Microwaves on Biological Systems
There are many investigations revealing that increased temperature higher than 1–2 °C results in several biological effects. Effects that have been reported to be due to microwave thermal effects are cataract formation and corneal lesion, change in gonadal function, damage to hematopoietic and immune systems, suppression of behavioral responses, and many other damages. Different mechanisms are behind these effects including damage to enzymes, proteins, lipids, membrane disruption, and protein aggregation (Daily et al. 1950, 1952; Stewart-DeHaan et al. 1983; Nageswari 2003; CSIRO 2013). Different investigations have shown that increased temperature can also affect barrier properties of biological membranes, which will be discussed in details later.
The rate at which the electromagnetic energy is absorbed by a tissue in the human body, and therefore the possibility and intensity of radiation thermal injuries, is quantified by specific absorption rate (SAR). SAR is the amount of energy absorbed per unit mass of the tissue and depends on intensity of the electromagnetic field, properties of the tissue, and distance from the electromagnetic source. SAR is expressed in watt per kilogram (W kg−1). Sensitivities of various tissues are different, and usually they are greater than 4 W kg−1 (ICNIRP 1998). Most tissues need to reach a particular temperature before thermal injuries can occur (called critical temperature). For example, critical lenticular temperature for cataract is reported to be 41 °C, below which the effect does not occur (Lipman et al. 1988). Other factors, e.g., blood supply of the organ, can also affect the intensity of the damage; lower blood supply (e.g., in eyes) makes the tissues more thermally vulnerable (Hyland 2000). Therefore, to provide a large margin of safety, the standards for SAR and intensity are set at 0.4 W kg−1 and 50 W m−2 for occupational exposure and 0.08 W kg−1 and 10 W m−2 for public exposure (ANSI/IEEE 1992; ICNIRP 1998).
3.2 Non-thermal Effects of Microwaves on Biological Systems
Non-thermal biological effects of microwaves are those that are not related to increased temperature in the system and can occur even at power exposure conditions within the recommended safety standard (ICNIRP 1996), with no obvious increase in body temperature (less than 1 °C). Human body can compensate for the extra energy and keep the temperature down during low-intensity radiation (Nageswari 2003).
Many biological effects are attributed to non-thermal effects of microwaves. Some of well-known interferences are depression of phagocytes (Mayers and Habeshaw 1973), alteration of blood–brain barrier permeability (Persson et al. 1997; Stam 2010), alteration of cell viability (Ballardin et al. 2011), deoxyribonucleic acid (DNA) damage (Lai and Singh 1996; Diem et al. 2005), changes of the activity of K+ channels (Geletyuk et al. 1995), alterations of membrane structure and function (Persson et al. 1992; Phelan et al. 1992, 1994), changes in permeability of liposomes (Saalman et al. 1991; Ramundo-Orlando et al. 1994; Mady and Allam 2011), altered enzyme activity (Byus et al. 1984; Allis and Sinha-Robinson 1987; Vojisavljevic 2011), protein structural modification (Porcelli et al. 1997; Chinnadayyala et al. 2012), and enhancement effect on skin penetration (Moghimi et al. 2010; Wong and Khaizan 2013). However, in spite of all of these reports and evidences, the existence of non-thermal biological effects still looks controversial and requires further investigation (Marjanović et al. 2012).
The exact mechanism of interaction of microwaves at non-thermal levels with biological systems is not fully understood yet. In contrast to thermal microwave effects in which SAR or power density is the main factors, many other parameters are important for non-thermal effects (Belyaev et al. 2000, 2005). A resonance-like or frequency-dependent interaction that has been suggested by Fröhlich (1988) might be used to explain microwave non-thermal effects. Accordingly, the living system might respond to this radiation due to similarity of its oscillation with biological endogenous rhythms and therefore causes oscillations of a section of membrane, proteins, or DNA. Another suggested mechanism is triggering of the heat shock or activation of cellular stress response by altering the conformation of proteins by a mechanism other than heating (Daniells et al. 1998; Laurence et al. 2000). Generation of reactive oxygen species (ROS) is another suggested mechanism. ROS have some beneficial effects in cell signaling and cell proliferation. However, when its production exceeds antioxidant defense mechanism, ROS can lead to cellular damage (Marjanović et al. 2012).
3.3 Effect of Microwave on Biological Membranes
There are strong evidences showing that microwaves may alter structural and functional properties of biological membranes at subcellular level to epithelia, from lipid bilayers to proteins and ionic channels and pumps at different cells and organs (e.g., see Brovkovich et al. 1991; Geletyuk et al. 1995; Moghimi et al. 2010; Yu and Yao 2010; Wong and Khaizan 2013). Actually, cell membranes are considered to be one of the major targets for microwave radiation as these structures are theoretically considered to be sensible to coherent excitations above 109 Hz (Fröhlich 1988). In this section studies about the effects of this nonionizing radiation on cells (as example for simple cellular membranes) and blood–brain barrier (as example for membranes with tight junctions) will be discussed. The effects on skin barrier will be provided in details in the next section.
The effects of microwave radiation on different properties related to cells and microorganisms including, but not limited to, viability (Atmaca et al. 1996), structural changes (Kim et al. 2008), decontamination (Shamis et al. 2008), and permeability (the subject of present work) have been investigated over the years, among which, a few studies related to barrier properties will be discussed here.
Fang et al. (2011) studied the effect of low-dose microwave radiation (2.45 GHz, 1.5 W g−1) on Aspergillus parasiticus to find that microwave and conventional heating treatment both caused increased cell membrane permeability, verified by increase in Ca+2, protein, and DNA leakage. However, the mechanisms of action of conventional heating and microwaves were found to be different, as discussed below. Conventional heating increased electrolyte leakage through loss of enzyme activity within the cell membrane, while microwave irradiation induced influx of Ca+2 through increased membrane fluidity that opened Ca+2 channels. In agreement to this investigation, Shamis et al. (2011) studied the effect of microwave on E. coli at a frequency of 18 GHz and showed that upon microwave treatment, E. coli cells exhibited a cell morphology different from that of cells treated with conventional heating procedure. Moreover, confocal laser scanning microscopy revealed that fluorescein isothiocyanate conjugated dextran was taken up by the microwave-treated cells, suggesting that pores had formed within the cell membrane.
Webber et al. (1980) showed in vitro ultrastructural changes in mouse neuroblastoma cells under exposure to microwave pulses at 2.7 GHz and also conventional heating method. They showed that cells remained viable and maintained normal architecture without any membrane damage at low level of microwave radiation, while very drastic damages occurred when cells were exposed to an increased level of the radiation. It was shown that at 3.9 KV cm−1 microwave for 60 s, the membrane was broken and the cell became leaky due to large number of breaks in the cell membrane. As similar changes were not seen by heat alone, it was suggested that these microwave effects may be non-thermal in nature (Webber et al. 1980).
As an example for a more complex barrier, the effects of microwaves on the blood–brain barrier (BBB) are discussed here. The mammalian brain is protected by the hydrophobic blood–brain barrier, which prevents harmful substances from reaching the brain tissue. This barrier consists of vascular endothelial cells of the capillaries with tight junctions between these cells (Nittby et al. 2009). It has been shown that microwave frequencies (2.5–3.2 GHz) that increase brain temperature to values above 40 °C can increase BBB permeability. However, microwave irradiation fails to open the BBB when brain temperature is kept below 40 °C. These data suggest that hyperthermia is an effective mechanism for opening the BBB (Sutton and Carroll 1979; Moriyama et al. 1991). In this direction, neuronal albumin uptake in the brain was shown to be dose dependently related to brain temperature, once temperature increased up to 1 °C or more (Kiyatkin and Sharma 2009). The permeability enhancement effect is said to be dependent on the degree of temperature rise, electromagnetic field SAR (energy absorbed per unit mass), duration of exposure, and the rate of heat distribution and dissipation in the body (Stam 2010).
Besides the above-mentioned thermal effects, several findings have also been reported on the non-thermal effects of microwaves on permeability of the blood–brain barrier. Increased leakage of fluorescein after 30 min of pulsed and continuous wave exposure (Frey et al. 1975) and passage of mannitol, inulin and dextran at very low energy levels have been reported (Oscar and Hawkins 1977). Töre and coworkers also showed albumin extravasation in rats exposed for 2 h–900 MHz at SAR values of 0.12, 0.5, and 2 W kg−1, which are expected to show non-thermal effects (Töre et al. 2001, 2002).
4 Enhancement Effects of Microwaves Toward Skin Permeation
To affect skin permeation, microwaves should penetrate the skin barrier. There is no full investigation available in terms of penetration depth of microwaves into human body and tissues. Radiofrequencies (including microwaves) may be absorbed, reflected, or pass through the tissues. The penetration depth depends on different factors including radiation frequency and energy absorption by tissue components. As microwaves absorption in the body is mainly by water, tissues with lower water content have significantly less absorption and, therefore, allow deeper microwaves penetration (reviewed by Kitchen 2001). The penetration depth depends on the radiation frequency as well and increases with decreased frequency (Kitchen 2001). The penetration depth of microwaves into human body is reported to be less than 1 mm for frequencies above 25 GHz (Stewart et al. 2006). Tamyis et al. (2013) showed that the penetration depth of microwaves in human volunteers’ skin is less than 0.8 mm for frequencies of higher than 30 GHz and reaches to about 1 mm when the frequency is decreased to 20 GHz. Microwaves can reach to deeper parts of the skin and body at lower frequencies (Adair 2003; Khounsary 2013). As far as the skin barrier is concerned, investigations have shown that 2.45 GHz microwaves affect transdermal permeation of drugs, a good indication that microwaves can penetrate and affect the skin barrier (Moghimi et al. 2010; Wong and Khaizan 2013). Besides, Wong and Khaizan (2013) showed that 2.45 GHz microwaves affect Raman and FTIR spectra of dermis, an indication that microwaves are able to affect skin layers beyond the epidermis.
So far, the investigations on the effects of microwaves on the skin have been limited mainly to areas other than permeation studies, such as heat shock protein changes in the skin as a result of mobile signals (Sanchez et al. 2007), protein expression in the human skin (Karinen et al. 2008), enhanced healing process of septic and aseptic wounds in rabbits (Korpan et al. 1994), and the treatment of the skin lesions caused by Leishmania major (Eskandari et al. 2012). However, surprisingly, there are only a small number of studies reported on the effects of microwaves on the skin permeation of drugs, as discussed later.
It is well known to the experts of the area of transdermal drug delivery that increased temperature can increase percutaneous absorption of most drugs. On the other hand, it has been shown that microwaves produce both thermal and non-thermal effects in the skin (Adair 2003; Stewart et al. 2006) and that they can increase human skin surface temperature (Walters et al. 2000). At very high frequencies (higher than 10 GHz), there is significant heating of the skin from even 10 mW cm−2, as all of the energy is absorbed in a small region. These effects can be considered as indirect indications for the ability of microwaves to increase the percutaneous absorption of drug, through their thermal effects.
The first investigation on the effects of microwaves on percutaneous absorption of drugs was performed by our group (Moghimi et al. 2010). This investigation employed nitrofurazone as the model penetrant and microwaves at 2.45 GHz and 3–120 W. The investigation revealed that microwaves increase permeation of nitrofurazone through their non-thermal effects in a time-dependent and power-dependent manner (Moghimi et al. 2010). Recently Wong and Khaizan (2013) investigated the microwave-induced transdermal drug permeation enhancement and showed that under exposure of microwaves at 2.45 GHz, skin permeation of sulphanilamide increases in a time-dependent manner. Using these two studies and some other related investigations, we try in the following sections to elucidate the properties and mechanism of microwave-induced enhancement toward skin permeation of drugs.
4.1 Effects of Microwaves’ Intensity and Exposure Time on Skin Barrier Performance
Table 10.1 provides the effects of different intensities of microwaves (3–120 W) for two different exposure times on the permeation of nitrofurazone through rat skin at 30 °C. The results indicate that microwaves are able to improve percutaneous absorption of nitrofurazone in a power-dependent manner, in a way that by increasing the power from 3 W to 120 W, the enhancement ratio increases from 1.1 to 2.7 (Moghimi et al. 2010). These experiments were performed at constant temperature and show that microwaves can increase percutaneous absorption of drugs through its non-thermal effects. These data are in agreement with Nakai et al. (2002), who reported that microwaves increase diffusion coefficient of CO2 through cellulose acetate membrane and that the enhancement effects increase with the microwave intensity increase for quantities of 100, 300, and 500 W. Wong and Khaizan (2013) also showed that treatment of the skin by microwave at 2450 MHz increased permeation of sulphanilamide and that the enhancement effect was increased significantly when the exposure time was increased from 2.5 min to 5 min. In addition, they showed that by increasing the duration of exposure to values of higher than 5 min at the same frequency, the skin color was changed from whitish to brownish that revealed heat–burn effects of microwave. The same burning effect was reported by the same group for lower exposure times (<5 min) when skin samples were exposed to lower frequency of 915 MHz (Wong and Khaizan 2013).
Moghimi et al. (2010) used two protocols of 90 and 45-min exposure times with resting intervals of 45 and 90 min, respectively, at different intensities of 15–120 W, and showed that equal microwave energies (or power intensity × exposure time) provide equal enhancement ratios for permeation of nitrofurazone through rat skin, irrespective of the delivery protocol (Table 10.2). This shows that the amount of delivered energy seems to be a key factor for the skin permeation enhancement effect of microwaves. Such a behavior allows alteration of the enhancement ratio and, therefore, drug input rate, through either adjustment of the exposure time or tuning the intensity of the microwaves. Besides, both above-mentioned protocols were of pulsatile type, i.e., employed resting time intervals. Therefore, these data show that, e.g., two separate 45-min exposures with 90-min resting interval equal one 90-min continuous exposure in terms of absorption enhancement ability. This might show that the enhancing effect of microwaves is cumulative, at least for the conditions used in this investigation (Moghimi et al. 2010). In this direction, it has been reported that damage induced by electromagnetic radiation is cumulative (Hardell and Sage 2008). Such a property should be considered in design and application of microwave devices to guarantee optimized drug delivery and also guarantee safety of the patient.
4.2 Stratum Corneum Lipid Disruption by Microwaves
Wong and Khaizan (2013) showed reduction of hydrogen bonding in microwave-treated rat skin by Fourier transform infrared spectroscopy (FTIR) and concluded that microwaves interact with keratin and/or polar moieties of lipid materials in the stratum corneum. Moreover, analysis of Raman spectra of the epidermal membrane by the same group showed that the polar lipids convert from ordered to disordered state. This alkyl chain-packing fluidization was attributed to increased permeation of sulphanilamide through microwave-treated abdominal rat skin (Wong and Khaizan 2013).
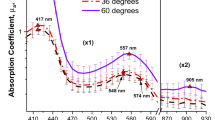
Moghimi et al. (2010) came to the same conclusion through another approach as discussed below. It has been shown that the enhancement effect of some penetration enhancers is temperature dependent, indicating that the mechanism of action of the enhancer and effects of thermal energy on the barrier might be the same, as was shown for the effects of cineole toward permeation of 5-fluorouracil through stratum corneum model lipid membranes (Moghimi et al. 1997). This phenomenon was investigated for the effects of microwaves on percutaneous absorption of drugs as well. To perform this investigation, considering the main transition temperature (T m) of the skin that is around 35–37 °C, the effects of 2.45 GHz microwaves on the permeation of nitrofurazone were investigated by Moghimi et al. (2010) at four different temperatures of 25 and 30 °C (below T m), 37 °C (at T m), and 42 °C (above T m). Results (Fig. 10.2 and Table 10.3) showed that while both microwave and temperature increase the permeability coefficient of the penetrant through rat skin, microwave enhancement ratios, calculated as the microwave-treated/untreated permeability coefficients at any given temperature, show a parabolic relationship with temperature, i.e., an increase in the enhancement ratio up to 30 °C and decrease at higher temperatures (Moghimi et al. 2010).
Effects of temperature on enhancement ratios of microwaves (2.45 GHz, 60 W) toward permeation of nitrofurazone through rat skin, indicating a parabolic relationship between enhancement ratio and temperature (Raw data from Moghimi et al. 2010). Enhancement ratios are calculated as microwave-treated/untreated permeability coefficient for any given temperature
Moghimi and coworkers performed the above-mentioned experiment at a controlled constant temperature for each temperature point to avoid thermal effects of microwaves. Therefore, the observed parabolic relationship between microwave enhancement effects and temperature (Fig. 10.2 and Table 10.3) might show that non-thermal effects of microwaves and heat obey a same mechanism or share the same sites of action for their permeation enhancement action. As a result, when the barrier properties of the skin are reduced by temperature, less room is left for microwave effects. Such a parabolic relationship between enhancement ability of chemical penetration enhancers and temperature has also been reported for permeation of 5-fluorouracil through a lamellar lipid structure model of human stratum corneum intercellular domain (Moghimi et al. 1997). On the other hand, it has been shown that heating the human skin in the range of 25–80 °C affects only the lipids, while proteins are affected at temperatures above 100 °C (Al-Saidan et al. 1998). Therefore, the enhancement effects of temperature toward permeation of nitrofurazone through rat skin might be attributed to the lipid domain of the skin barrier, and, considering the above-mentioned parabolic relationship and related discussions, it was concluded that microwaves’ non-thermal effects arise mainly from disruption of lamellar lipid structures of the stratum corneum (Moghimi et al. 2010). In agreement to this conclusion, Wong and Khaizan have recently reported that while application of microwaves at 2450 MHz for 5 min was able to fluidize the lipid structure of rat epidermis, the increase in temperature at the same condition was negligible (about 1 °C, from 30 to 31 °C), indicating that microwave non-thermal effects are able to fluidize stratum corneum lipid structure (Wong and Khaizan 2013).
Our group has also investigated the effects of coadministration of oleic acid (a lipid fluidizer) and microwaves (at 2.45 GHz and 60 W) on the permeation of nitrofurazone through rat skin (Alinaghi 2006). Results showed that while the enhancement ratios of oleic acid alone and microwaves alone were 2.7 and 2.2, respectively, the enhancement ratio of the combination was around 2.9 (Fig. 10.3). These data indicate that microwaves had not been able to show a significant enhancement effect in the presence of oleic acid (Alinaghi 2006). Oleic acid is well known for its fluidizing effect on stratum corneum lipids (Williams and Barry 2004), and again these data suggest that microwaves impose their effect mainly through fluidization of the stratum corneum lipids (Alinaghi 2006). The slight increase in enhancement by microwaves in oleic acid-treated samples (from 2.7 to 2.9) might be due to further fluidization of lipids by microwaves (Alinaghi 2006). Another possibility is increased permeation of oleic acid by microwaves as was reported by Wong and Khaizan (2013) who showed that treatment of rat skin by microwaves (2.45 GHz for 5 min) increases oleic acid uptake by epidermal membrane and that permeation of sulfanilamide under combination of oleic acid and microwaves is more than those of microwaves alone or oleic acid alone. Wong and Khaizan (2013) also found that the effects of oleic acid on epidermal membrane spectra, as studied by Raman and FTIR spectroscopy methods, are similar to that of microwave treatment (2.45 GHZ for 5 min).
Enhancement effects of microwaves (MW) and oleic acid (OA) toward permeation of nitrofurazone through rat skin. Microwaves were used at 2.45 GHz and 60 W at constant temperature (Raw data from Alinaghi 2006)
As discussed above, microwaves are able to affect the lipid bilayer structures of biological membranes. Liposomes are good models for mechanistic studies on biological lipid bilayers, including the effects of microwaves. Gaber and coworkers (2005) studied the effect of 900 MHz microwave irradiation at 12 W kg−1 SAR on the bilayer permeability of liposomes (made from egg phosphatidylcholine) using light-scattering techniques. FTIR and nuclear magnetic resonance (NMR) studies as well as optical anisotropy measurements were employed to reveal structural alterations in exposed vesicles. Results showed conformational changes and disordering in the hydrocarbon acyl chain of liposomal lipids. Also a significant increase in leakage of liposomes above their transition temperature upon exposure to microwaves was observed. They revealed that this could be attributed to a transient pore formation in the liposomes lipid bilayers (Gaber et al. 2005).
Beneduci et al. (2012) studied the effect of microwaves at 53–58 GHz on dimyristoylphosphatidylcholine multilamellar liposomes using 2H-NMR and showed that microwaves induced a reduction of water ordering at the membrane interface. Besides, they found that microwaves shifted the ripple-to-fluid transition temperature of the bilayers from 25 °C to 27 °C. This microwave-induced upward shift of the transition temperature was attributed to the non-thermal effects of microwave on the lamellar lipid bilayers (Beneduci et al. 2012).
It is obvious from the above-mentioned arguments that the intercellular lamellar lipid structure of the stratum corneum is an important target for both thermal and non-thermal effects of microwaves.
5 Conclusion and Future Horizons
It is clear that microwaves are able to increase percutaneous absorption of drugs through their both thermal and non-thermal effects. The effectiveness and enhancing capacity of this enhancement method depend on exposure time, applied power, and the used frequency. It is also clear that microwaves impose their enhancement effects, at least in part, through fluidization of the intercellular lipids of the stratum corneum. Microwaves can be considered as a potential physical enhancement method for transdermal drug delivery. Besides, as microwave generators are electronic devices, they have the potential to be used for programmed/bioresponsive drug delivery. This technique is expected to open new horizons in the field of transdermal drug delivery, alone or as a combination with other enhancement methods such as chemical penetration enhancers.
However, application of microwaves as a percutaneous absorption enhancement method is still in its infancy. Further investigations are required for full analysis and mechanistic investigation of the effects of microwaves on the skin barrier, including their effects on lipids, proteins, and skin appendages. Also as microwaves work at molecular levels, the effects of physicochemical properties of the penetrants also deserve a full investigation. Finally, as microwaves can damage tissues in certain intensities and frequencies, this enhancement method should be investigated for optimized conditions to prevent unnecessary damages to the skin or other body organs.
References
Adair RK (2003) Biophysical limits on athermal effects of RF and microwave radiation. Bioelectromagnetics 24:39–48
Alinaghi A (2006) Studying the effects of microwave on drug diffusion. PharmD Thesis. School of Pharmacy, Shahid Beheshti University of Medical Sciences. Tehran. p. 110.
Allis JW, Sinha-Robinson BL (1987) Temperature-specific inhibition of human red cell Na+/K+ ATPase by 2450-MHz microwave radiation. Bioelectromagnetics 8(2):203–212
Al-Saidan SM, Barry BW, Williams AC (1998) Differential scanning calorimetry of human and animal stratum corneum membranes. Int J Pharm 168:117–122
ANSI/IEEE [American National Standards Institute/Institute of Electrical and Electronics Engineers] (1992) C95.1 Safety levels with respect to human exposure to radio frequency electromagnetic fields, 3 kHz to 300 GHz. The Institute of Electrical and Electronics Engineers, New York
Atmaca S, Akdag Z, Dasdag S et al (1996) Effect of microwaves on survival of some bacterial strains. Acta Microbiol Immunol Hung 43(4):371–378
Aulton E (2007) Drying. In: Aulton E (ed) Aulton’s pharmaceutics. Churchill Livingstone, Edinburgh, pp 425–440
Ballardin M, Tusa I, Fontana N et al (2011) Non-thermal effects of 2.45 GHz microwaves on spindle assembly, mitotic cells and viability of Chinese hamster V-79 cells. Mutat Res 716(1–2):1–9
Belyaev IY, Shcheglov VS, Alipov ED et al (2000) Non-thermal effects of extremely high frequency microwaves on chromatin conformation in cells in vitro: dependence on physical, physiological and genetic factors. IEEE Trans Microwave Theory Tech 48:2172–2179
Belyaev IY, Hillert L, Protopopova M et al (2005) 915 MHz microwaves and 50 Hz magnetic field affect chromatin conformation and 53BP1 foci in human lymphocytes from hypersensitive and healthy persons. Bioelectromagnetics 26(3):173–184
Beneduci A, Filippelli L, Cosentino K et al (2012) Microwave induced shift of the main phase transition in phosphatidylcholine membranes. Bioelectrochemistry 84:18–24
Bradshaw SM, Wyk EJS, Swardt JBD (1998) Microwave heating principles and the application to the regeneration of granular activated carbon. J S Afr Inst Min Metall 4:201–212
Brovkovich VM, Kurilo NB, Barishpol’ts VL (1991) Action of millimeter-range electromagnetic radiation on the Ca pump of sarcoplasmic reticulum. Radiobiologiia 31(2):268–271
Byus CV, Lundak RL, Fletche RM et al (1984) Alteration in protein kinase activity following exposure of cultured human lymphocytes to modulated microwave fields. Bioelectromagnetics 5(3):341–351
Celik U, Alagoz N, Yildirim Y et al (2013) New method of microwave thermokeratoplasty to correct myopia in 33 eyes: one-year results. J Cataract Refract Surg 39(2):225–233
Challis LJ (2005) Mechanisms for interaction between RF fields and biological tissue. Bioelectromagnetics 7:S98–S106
Chinnadayyala SSM, Santhosh M, Goswami P (2012) Microwave based reversible unfolding and refolding of alcohol oxidase protein probed by fluorescence and circular dichroism spectroscopy. Chem Mater Sci 3(4):317–323
CSIRO (2013) Biological effects and safety of electromagnetic radiation. http://electricwords.emfacts.com/csiro. Accessed 9 Mar 2013
Daily LKG, Wakim JF, Herrick E et al (1950) The effects of microwave diathermy on the eye. Am J Ophthalmol 33:1241–1254
Daily LKG, Wakim JF, Herrick EM (1952) The effects of microwave diathermy on the eye of the rabbit. Am J Ophthalmol 35:1001–1017
Daniells C, Duce I, Thomas D et al (1998) Transgenic nematodes as biomonitors of microwave-induced stress. Mutat Res 399:55–64
Diem E, Schwarz C, Adlkofer F et al (2005) Non-thermal DNA breakage by mobile-phone radiation (1800 MHz) in human fibroblasts and in transformed GFSH-R17 rat granulosa cells in vitro. Mutat Res 583(2):178–183
Eskandari SE, Azimzadeh A, Bahar M et al (2012) Efficacy of microwave and infrared radiation in the treatment of the skin lesions caused by leishmania major in an animal model. Irn J Publ Health 41(8):80–83
Fang Y, Hu J, Xiong S et al (2011) Effect of low dose microwave radiation on Aspergillus parasiticus. Food Control 22:1078–1084
Foster KR, Glaser R (2007) Thermal mechanisms of interaction of radiofrequency energy with biological systems with relevance to exposure guidelines. Health Phys 92(6):609–620
Frey AH, Feld SR, Frey B (1975) Neural function and behavior: defining the relationship. Ann NY Acad Sci 247:433–439
Fröhlich H (1988) Biological coherence and response to external stimuli. Springer, Berlin
Gaber MH, Halim NAE, Khalil WA (2005) Effect of microwave radiation on the biophysical properties of liposomes. Bioelectromagnetics 26(3):194–200
Geletyuk VI, Kazachenko VN, Chemeris NK et al (1995) Dual effects of microwaves on single Ca2+−activated K+ channels in cultured kidney cells. FEBS Lett 359(1):85–88
Hardell L, Sage C (2008) Biological effects from electromagnetic field exposure and public exposure standards. Biomed Pharmacother 62(2):104–109
Hyland GJ (2000) Physics and biology of mobile telephony. Lancet 356(25):1833–1836
ICNIRP (1996) Guideline on UV radiation exposure limits. Health Phys 71(6):978
ICNIRP (1998) Guideline for limiting exposure to time-varying electric, magnetic and electromagnetic fields (up to 300 GHz). Health Phys 74(4):494–522
Karinen A, Heinävaara S, Nylund R et al (2008) Mobile phone radiation might alter protein expression in human skin. BMC Genomics 9:77
Khounsary A (2013) Microwave health effects. Argonne National Laboratory, US Department of Energy. http://www.newton.dep.anl.gov. Accessed 24 June 2013
Kim SY, Jo EK, Kim HJ et al (2008) The effects of high-power microwaves on the ultrastructure of Bacillus subtilis. Lett Appl Microbiol 47:35–40
Kitchen R (2001) Radiofrequency and microwave radiation safety handbook. Newnes, Oxford, pp 59–60
Kiyatkin EA, Sharma HS (2009) Permeability of the blood–brain barrier depends on brain temperature. Neuroscience 161:929–939
Korpan NN, Resch KL, Kokoschinegg P (1994) Continuous microwave enhances the healing process of septic and aseptic wounds in rabbits. J Surg Res 57:667–671
Kurumi Y, Tani T, Naka S et al (2007) MR-guided microwave ablation for malignancies. Int J Clin Oncol 12(2):85–93
Ku HS, Siu F, Siores E et al (2002) Application of fixed and variable frequency microwave (VFM) facilities in polymeric materials processing and joining. 2nd World Engineering Congress, 22–25, Kuching, Malaysia. From University of Queensland (Australia) Website at: http://eprints.usq.edu.au/2438/. Accessed 14 June 2013
Lai H, Singh NP (1996) Single and double-strand DNA breaks after acute exposure to radiofrequency radiation. Int J Radiat Biol 69:13–521
Lammers RJM, Witjes JA, Inman BA et al (2011) The role of a combined regimen with intravesical chemotherapy and hyperthermia in the management of non-muscle-invasive bladder cancer: a systematic review. Eur Urol 60(1):81–93
Laurence JA, French PW, Lindner RA et al (2000) Biological effects of electromagnetic fields-mechanisms for the effects of pulsed microwave radiation on protein conformation. J Theor Biol 206:291–298
Lin JC (2006) Microwave surgery inside the heart. IEEE Microw Mag 7(3):32–36
Lipman RM, Tripathi BJ, Tripathi RC (1988) Cataracts induced by microwave and ionizing radiation. Surv Ophthalmol 33(3):200–210
Lu GW, Flynn GL (2009) Cutaneous and transdermal delivery-processes and systems of delivery. In: Florence A, Siepmann J (eds) Modern pharmaceutics, Vol. 2. Informa Healthcare, New York, pp 43–101
Mady MM, Allam MA (2011) The influence of low power microwave on the properties of DPPC vesicles. Phys Med 28:48–53
Marjanović AM, Pavičić I, Trošić I (2012) Biological indicators in response to radiofrequency/microwave exposure. Arh Hig Rada Toksikol 63(3):407–416
Mayers CP, Habeshaw JA (1973) Depression of phagocytosis: anon-thermal effect of microwave radiation as a potential hazard to health. Int J Radiat Biol 24(5):449–461
Moghimi HR, Williams AC, Barry BW (1997) A lamellar matrix model for stratum corneum intercellular lipids. V. Effects of terpene penetration enhancers on the structure and thermal behavior of the matrix. Int J Pharm 146:41–54
Moghimi HR, Barry BW, Williams AC (1999) Stratum corneum and barrier performance; a model lamellar structural approach. In: Bronaugh RL, Maibach HI (eds) Percutaneous absorption, 3rd edn. Dekker, New York, pp 515–553
Moghimi HR, Alinaghi A, Erfan M (2010) Investigating the potential of non-thermal microwave as a novel skin penetration enhancement method. Int J Pharm 401(1–2):47–50
Moghimi HR, Jamali B, Farahmand S et al (2013) Effect of essential oils, hydrating agents, and ethanol on hair removal efficiency of thioglycolates. J Cosmet Dermatol 12:41–48
Moriyama E, Salcman M, Broadwell RD (1991) Blood–brain barrier alteration after microwave-induced hyperthermia is purely a thermal effect: I. Temperature and power measurements. Surg Neurol 35(3):177–182
Moulder JE (1998) Power-frequency fields and cancer. Crit Rev Biomed Eng 26(1–2):1–116
Mousa A (2011) Electromagnetic radiation measurements and safety issues of some cellular base stations in Nablus. J Eng Sci Technol Rev 4:35–42
Nageswari NS (2003). Biological effects of microwaves and mobile telephony. Proceedings of the International Conference on Non-ionizing Radiation at UNITEN (ICNIR 2003) Electromagnetic Fields and Our Health. 20–22 Oct 2003.
Nakai Y, Tsujita Y, Yoshimizu H (2002) Control of gas permeability for cellulose acetate membrane by microwave irradiation. Desalination 145(1):375–377
Nittby H, Brun A, Eberhardt J et al (2009) Increased blood–brain barrier permeability in mammalian brain 7 days after exposure to the radiation from a GSM-900 mobile phone. Pathophysiology 16:103–112
Oscar KJ, Hawkins TD (1977) Microwave alteration of the blood–brain barrier system of rats. Brain Res 126:281–293
Persson BRR, Salford LG, Brun A et al (1992) Increased permeability of the blood–brain barrier induced by magnetic and electromagnetic fields. Annal N Y Acad Sci 649:356–358
Persson BRR, Salford LG, Brun A et al (1997) Blood–brain barrier permeability in rats exposed to electromagnetic fields used in wireless communication. Wirel Netw 3:455–461
Phelan AM, Lange DG, Kues HA et al (1992) Modification of membrane fluidity in melanin-containing cells by low-level microwave radiation. Bioelectromagnetics 13:131–146
Phelan AM, Neubauer CF, Timm R et al (1994) Athermal alterations in the structure of the canalicular membrane and ATPase activity induced by thermal levels of microwave radiation. Radiat Res 137(1):52–58
Porcelli M, Cacciapuoti G, Fusco S et al (1997) Non-thermal effects of microwaves on proteins: thermophilic enzymes as model system. FEBS Lett 402:102–106
Ramundo-Orlando A, Mossa G, d’Inzeo G (1994) Effect of microwave radiation on the permeability of carbonic anhydrate loaded with unilamellar liposome. Bioelectromagnetics 15:303–313
Repacholi MH (1998) Low-level exposure to radiofrequency electromagnetic fields: health effects and research needs. Bioelectromagnetics 19:1–19
Saalman E, Norden B, Arvidsson L et al (1991) Effect of 2.45 GHz microwave radiation on permeability of unilamellar liposomes to 56-carboxyfluorescein. Evidence of non-thermal leakage. Biochim Biophys Acta 1064:124–130
Sanchez S, Haro E, Ruffie G et al (2007) In vitro study of the stress response of human skin cells to GSM-1800 mobile phone signals compared to UVB radiation and heat shock. Radiat Res 167:572–580
Shamis Y, Taube A, Shramkov Y et al (2008) Development of a microwave treatment technique for bacterial decontamination of raw meat. Int J Food Eng 4:1–15
Shamis Y, Taube A, Mitik-Dineva N et al (2011) Specific electromagnetic effects of microwave radiation on Escherichia coli. Appl Environ Microbiol 77(9):3017–3022
Simon JC, Dupuy DE, Mayo-Smith WW (2005) Microwave ablation: principles and applications. Radiographics 25:S69–S83
Stam R (2010) Electromagnetic fields and the blood–brain barrier. Brain Res Rev 65:80–97
Sorrentino R, Bianchi G (2010) Microwave and RF engineering. Wiley, New York, pp 1–8
Stewart-DeHaan PJ, Creighton MO, Larsen LE et al (1983) In vitro studies of microwave-induced cataract, separation of field and heating effects. Exp Eye Res 36:75–90
Stewart DA, Gowrishankar TR, Weaver JC (2006) Skin heating and injury by prolonged millimeter-wave exposure: theory based on a skin model coupled to a whole body model and local biochemical release from cells at supra physiologic temperatures. IEEE Trans Plasma Sci 34(4):1480–1493
Stuerga D, Loupy A (eds) (2006) Microwaves in organic synthesis, 2nd edn. WILEY-VCH Verlag, Weinheim
Sutton CH, Carroll FB (1979) Effects of microwave-induced hyperthermia on the blood–brain barrier of the rat. Radio Sci 14(65):329–334
Tamyis NM, Ghodgaonkar DK, Taib MN and Wui WT (2013) Dielectric properties of human skin in vivo in the frequency range 20–38 GHz for 42 healthy volunteers. URSI: Union Radio-Scientific Internationale. http://www.ursi.org/proceedings/ProcGA05/pdf/KP.45(0850). Accessed 24 June 2013
Taylor LS (1981) The mechanism of athermal microwave biological effects. Bioelectromagnetics 2:259–267
Taylor LA, Meek TT (2005) Microwave sintering of lunar soil: properties, theory, and practice. J Aerospace 18(3):188–196.
Töre F, Dulou PE, Haro E et al. (2001) Two-hour exposure to 2-W/kg, 900-MHz GSM microwaves induces plasma protein extravasation in rat brain and dura matter. Proceedings of the 5th International congress of the EBEA, Helsinki; 2001. pp 43–45
Töre F, Dulou PE, Haro E et al (2002) Effect of 2 h GSM-900 microwave exposures at 2.0, 0.5 and 0.12 W/kg on plasma protein extravasation in rat brain and dura matter. Proceedings of the 24th Annual Meeting of the Bioelectromagnetics Society (BEMS), 2002; 61–62
Toutouzas K, Grassos C, Drakopoulou M et al (2012) First in vivo application of microwave radiometry in human carotids. J Am Coll Cardiol 59(18):1645–1653
Vojisavljevic V (2011) Low intensity microwave radiation as modulator of the l-lactate dehydrogenase activity. Med Biol Eng Comput 49(7):793–799
Vorst VA, Rosen A, Koysuk Y (2006) RF/Microwave interaction with biological tissue. Wiley, Hoboken
Walters TJ, Blick DW, Johnson LR (2000) Heating and pain sensation produced in human skin by millimeter waves: comparison to a simple thermal model. Health Phys 78(3):259–267
Webber MM, Barnes FS, Seltzer LA et al (1980) Short microwave pulses cause ultrastructural membrane damage in neuroblastoma cell. J Ultrastruct Res 71:321–330
Williams AC, Barry BW (2004) Penetration enhancers. Adv Drug Deliv Rev 56:603–618
Wong TW, Khaizan AN (2013) Physicochemical modulation of skin barrier by microwave for transdermal drug delivery. Pharm Res 30(1):90–103
Xie Y, Guo B, Xu L et al (2006) Multistatic adaptive microwave imaging for early breast cancer detection. IEEE Trans Biomed Eng 53(8):1647–1657
Yu Y, Yao K (2010) Non-thermal cellular effects of low power microwave radiation on the lens and lens epithelial cells. J Int Med Res 38(3):729–736
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Moghimi, H.R., Alinaghi, A. (2017). Microwaves as a Skin Permeation Enhancement Method. In: Dragicevic, N., I. Maibach, H. (eds) Percutaneous Penetration Enhancers Physical Methods in Penetration Enhancement. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53273-7_10
Download citation
DOI: https://doi.org/10.1007/978-3-662-53273-7_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53271-3
Online ISBN: 978-3-662-53273-7
eBook Packages: MedicineMedicine (R0)