Abstract
The restoration of endodontically treated teeth must be considered as integral part of the endodontic treatment, since it plays a major role in the long-term success of the procedure, as well as in tooth longevity. In order to maximize the chances of success, the specificities of endodontically treated molars need to be carefully considered, as well as the recent advances in adhesion, digital technologies, and biomaterials. This chapter will critically discuss important aspects such as reinforcement, restoration retention, the need for a ferrule and/or for posts, and the importance of cuspal coverage. Best-practice recommendations will be made, with particular focus on tissue preservation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Cuspal coverage
- Composite
- Tooth fracture
- Post and core
- Chewing forces
- Ferrule
- Overlay
- Endocrown
- Tissue preservation
- Adhesion
van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. 2010;26:929–39.
This prospective study on molars with long-term follow-up investigated the durability of ceramic restorations that were luted with different bonding systems. More restorations failed in root canal-treated molars compared to vital counterparts (21 and 39 %, respectively). Other relevant factors for failure included the bonding agent used, gender, and parafunctional habits. The technique investigated showed advantages like less destruction of healthy tissue, and avoiding of endodontic treatment and/or deep cervical placement of restoration margins to obtain retention.
7.1 Introduction
Root canal treatment should not be considered finished until the tooth in question is restored in a timely and adequate fashion. It is clear from the literature that any delay between endodontic treatment and tooth restoration should be as brief as possible, since significantly reduced change of survival after endodontic treatment was reported for teeth restored with temporary restorations, compared to those receiving a permanent restoration [1]. Regarding the way endodontically treated molars should be restored, we lack a clear response to several important questions, which will be listed in the next section of this chapter.
Best clinical practice should refer to the highest level of evidence, that is, randomized controlled clinical studies. This is exemplified in the conclusion of authors dealing with the restoration of endodontically treated teeth. For example, Al-Omiri and others state [2]: “Most guidelines were based mainly on ex vivo studies and to a lesser extent on limited in vivo studies. The lack of long-term controlled randomized clinical studies was the main hindrance to reaching a conclusive and undisputable opinion regarding endodontic posts in terms of tooth fracture and biomechanical behaviour.” While Peroz and others find [3]: “These guidelines are based mainly on in vitro studies with an evidence level of IIa or IIb, as there is a lack of randomized clinical studies available.”
Even from clinical studies, it is difficult to extract clear clinical guidelines. For example, in a recently published practice-based study, it is stated that the influence of tooth type on the survival of endodontically treated teeth is not well established in the literature [4]. The authors found that restorations placed on premolars and anterior teeth were more successful compared with restorations in molars, but this is not universally accepted [5, 6].
In fact, lack of consideration of some factors prevents clear evidence-based guidelines for the restoration of endodontically treated teeth. To give a specific example, in a meta-analysis (high level of evidence) evaluating the prognostic factors for tooth survival after endodontic treatment, the placement of crowns or cast restorations was reported to improve tooth survival compared to direct restorations [7]. Nevertheless, some important parameters were not taken into account in the analysis in that study, notably the tooth type, the amount and distribution of residual tooth structure, or the type of final restoration.
Confounding variables further compromise these results. For example, it has been argued that teeth with preoperative periapical lesions are less likely to receive a crown compared to those without lesion and anterior teeth are more likely to be restored with a filling and sooner than posterior teeth [8]. This indicates a treatment selection bias and highlights that considering restorations of endodontically treated teeth must be specific to the type of tooth and the amount and distribution of remaining tissue.
The present chapter will focus on the literature dealing specifically with the restoration of molars after endodontic treatment. With the limitations pointed out above, the following aims at providing best-practice considerations in the restoration of endodontically treated molars, with particular focus on the most recent scientific data and technological innovations and relate that to clinical questions.
7.2 Questions That Arise in Daily Practice
Providing a fluid-tight seal and long-term stability of the root canal treatment is only one of many factors that the restorative dentist needs to fulfill. In general dental practice, patient expectations are more related to the restoration of masticatory function, the aesthetics, the longevity of the restoration, or to more practical factors such as chair-side time or the cost of the restorative procedure [9]. Hence, several questions come to mind when considering how an endodontically treated molar should be restored. The subsequent paragraphs will provide some clinical questions with briefly remarked answers that will be revisited later in the chapter.
-
Should all endodontically treated teeth be restored with a cast crown?
While cuspal coverage is typically recommended, this may not be necessary in many instances, since such a decision should depend on the amount of remaining coronal tissue. In teeth with little tissue loss, for example, limited to the access cavity, a direct restoration is a valid option. It is less expensive for the patient, conserves tooth structure, and is faster, and efficient, since the patient leaves the practice with a permanent restoration in a single appointment.
-
Where is the limit, deciding between a direct and indirect restoration for endodontically treated molars?
Historically, in teeth with substantial tissue loss, which is frequently the case when a root canal treatment is required, the use of metal posts was often necessary. This was to provide retention for nonadhesive materials such as silver amalgams (Fig. 7.1a) or other precious metal core materials to support cast crown (Fig. 7.1b, c).
Selection of clinical cases of molar endodontics with (a) a right mandibular first molar (46 FDI, #30 Universal) with inadequate root canal treatment, periapical lesions on both roots and a large amalgam restoration retained by two metal posts; (b) a long-span bridge restoration including three molars, with metal posts in multiple root canals; (c) tooth 36 (#19) with cast post and core in precious alloy before crown placement. Note the very thin remaining dentin layer toward the furcation of both roots indicated by arrows; (d) three-unit bridge placed 3 years ago with metal post and resin core in tooth 37 (#18). Note vertical root fracture indicated by the red arrow; (e) example of bridge restoration anchored by root canal posts, but with massive destruction of tooth structure due to recurrent caries; (f) left: inadequate root canal treatment with periapical radiolucent areas and resin composite restoration with two large metallic screw posts; center: same case after removal of the posts, endodontic retreatment; immediately after crown placement and 4-year follow-up showing periapical healing; (g) endodontically treated upper molar with large coronal tissue loss restored with bonded overlay composite restoration after preliminary margin relocation (Courtesy of Dr. T. Hollaert); (h) left: tooth 25 (#13) with vertical root fracture, 26 (#14) and 27 (#15) with mesial decay; right: same case after extraction of 25 (#13) and 27 (#15); crown preparation of 26 (#14) resulting in loss of tooth structure and pulpal inflammation requiring root canal treatment; the remaining composite material will have to be replaced; (i) left: tooth 26 (#14) with apical radiolucency on MB root, with a carrier-based fill in a pulp-floor perforation; right: tooth after endodontic retreatment, removal of the carrier, repair of the perforation, and lesion healing at the 1 year follow-up. The initial large composite restoration was maintained, and the access cavity filled by a direct composite
-
Are posts required for the restoration of endodontically treated molars? Which posts, for example, which type, shape, size, or diameter?
The placement of certain posts usually requires additional dentin removal, and may therefore result in a weakening of the tooth (Fig. 7.1c). The stiffness of metal posts materials could also generate inappropriate stresses on the thin remaining dentin walls, which may result in root fracture (Fig. 7.1d).
-
Do posts reinforce or weaken endodontically treated molars?
It must be kept in mind that retention of a restoration (survival) does not necessarily mean clinical success. In some instances, even if the retention provided by the post is sufficient to maintain the restoration in place, the loss of marginal seal should already be considered as a failure, and restoration repair or replacement should be performed. This is illustrated by a very extreme situation in Fig. 7.1e, but more moderate cases of this very situation are not uncommon. While reinforcement of thin, fragile root walls with a bonded fiber post is possible, posts often weaken teeth due to nonphysiological forces exerted and further loss of dentin to prepare the post space. This leads to a more general transition in modern dentistry, now giving more importance to the tooth survival than to the restoration survival, the former being certainly more important from a patient perspective.
-
Can an endodontically treated molar with extensive tissue loss be restored solely by a bonded restoration? Are posts required for root canal-treated molars?
Dental material technologies have evolved tremendously over the last decades. In particular, resin-based composites, which can be micromechanically and chemically bonded to the dental tissues, have become more and more reliable. By tradition, some dentists keep using metal posts to retain bonded composite restorations (Fig. 7.1f), while they accordingly should be replaced by fiber-reinforced resin-based posts, or possibly by no posts at all, either in case of a composite core covered by a full crown, or more recent adhesive strategies such as the so-called endocrowns or overlays in general (Fig. 7.1g).
-
Is adhesive technology sufficient to reinforce the tooth?
The preparation of a full crown frequently results in additional removal of sound tooth structure (Fig. 7.1h). Fiber posts rely on luting resin that fills discrepancies, so that additional widening of the space becomes unnecessary. This is supported by the fact that a ferrule should be obtained on endodontically treated teeth. If a 2 mm ferrule can be obtained, a post is not needed to retain the buildup.
-
Is a ferrule a must in endodontically treated molars or is tissue preservation more important? Is partial restoration a valid alternative to full crown? Should the cusps be covered?
A ferrule is generally admitted to be a must to prevent dislodging forces that will lead to coronal leakage. Cusps should be covered if structure loss is the size of an MOD preparation, or larger, and in undermined coronal walls. It should be considered in cases with loss of marginal ridges.
-
After endodontic (re-)treatment through an existing restoration, should the latter be replaced or repaired?
Very often, endodontic treatment is performed through an existing restoration, either a crown or a filling (Fig. 7.1i), which in some instances are still serviceable. Here preservation of the previous restoration and the direct restoration of the occlusal cavity may suffice.
-
Can endodontically treated molars be part of a multiunit restoration?
Despite the development of implant technology, endodontically treated teeth are still valid abutments in large-span restoration. This chapter focuses on single-tooth restoration for endodontically treated molars; detailed considerations for complex treatment plans likely require multispecialty discussion and are beyond the scope of this book.
-
Finally, how should a tooth with poor endodontic prognosis be restored?
Despite the high success rate of endodontic procedures, some teeth are compromised due to problems such as broken instruments, perforation, or stripping, which may result in a poorer prognosis of the endodontic treatment. A direct restoration for teeth with a poor prognosis may be an appropriate solution.
This list of question is not exhaustive, and the answers not comprehensive, but they illustrate part of the decision-making process of the dentist restoring a molar after root canal procedure, which offers specific challenges (Box 7.1). This chapter will provide considerations to help practitioners answer these questions, and make the best possible clinical decision.
Box 7.1. Specific Properties and Findings Regarding Endodontically Treated Molars
-
They differ from other tooth types, since they endure most of the vertical masticatory forces (100–300 N), and are protected from lateral forces by anterior teeth through anterolateral guidance.
-
Root canal therapy itself does not seem to weaken dental structures; increased susceptibility to fracture appears to be due in majority to coronal and pericervical hard tissue removal, not to local changes of dentin characteristics.
-
Three major technological developments are challenging the way endodontically treated molars have so far been restored:
-
Adhesive dentistry and the development of increasingly more reliable dental adhesives
-
The rise of digital technology, enabling the rapid and reliable design and manufacture of restoration in practice
-
The development of “Bio-”materials, with characteristics closer to the replaced tissues
-
7.3 Molar Restoration in an Era of Adhesive Dentistry, Digital Technology, and Biomaterials
Molar teeth endure the majority of the vertical masticatory forces, while most of the time, they are protected from lateral forces by anterior teeth through anterolateral guidance [10]. Occlusal loads sustained by molars during normal function range roughly between 100 and 300 N, while they do not exceed 50 N for premolars, and are lower yet for anteriors [11]. Higher values for maximum voluntary bite force have also been reported (500–800 N) [12], and can potentially reach even higher levels in case of parafunctions [10]. The variability is due to factors such as the type of food [13], age [12], or gender [14].
This underlines that restorative concepts should be specific to each tooth type, since each is submitted to very different challenges. Molar teeth are mostly submitted to axial forces of high intensity. Since root canal treatment weakens teeth due to loss of structure, there is a particular need to adequately protect endodontically treated molars against tooth fracture. In this regard, it is to some extent surprising that most reviews and guidelines dealing with restoration after endodontic treatment propose general concepts of restoration for all teeth, and not specific to each tooth type [15].
Tooth weakening following endodontic treatment seems to have little [10] or nothing to do [16] with local changes of dentin characteristics following endodontic treatment (e.g., loss of moisture, use of chelators, irrigants, or medicaments). The major cause for increased susceptibility to fracture of endodontically treated teeth appears to be the loss of hard tissue [10]. Endodontically treated teeth indeed very often undergo additional dentin removal in the process of the restoration, for example:
-
Creating post space
-
Preparation for full crowns
-
Occlusal reduction of thin dentin walls
In this regard, it is quite sobering that a major cause of further tissue damage is iatrogenic, especially given the efforts that are currently invested in developing strategies to regenerate dental tissues in order to strengthen tooth structure.
In light of this paradox, it is important to weigh the necessity or rationale of additional tissue sacrifice. The ultimate goal of dentistry is to retain a healthy complement of teeth for a lifetime; therefore, appropriate strategies should be “conservative” in order to control, rather than eliminate a condition, with existing tissues preserved as much as possible [17]. Indeed, it appears that habits, heritage, and/or traditions sometimes lead to a “conservative” dentistry in the sense of holding to traditional attitudes and values and cautious about change or innovation. In this regard, it is significant to consider certain advances and evolutions made over the past few decades that are of prime importance when considering the best way to restore endodontically treated molars: adhesive dentistry, digital technology, and biomimetics.
Adhesive dentistry started in 1955 with Buonocore, and bonding materials and strategies have since considerably evolved. Dental adhesives are now more and more reliable and predictable [18]. Specifically regarding restoration of endodontically treated molars, composite restorations enable us to do more and more without mechanical, nonadhesive, retention features such as cavity taper, grooves, or posts. Retention elements necessary in the era of silver amalgam are no longer needed, and this allows for more tissue preservation.
Another major breakthrough that is very likely to greatly affect tooth restoration is the advent of digital technology, specifically the CAD/CAM technology. Clearly, digital technology is changing dentistry and it is likely that the use of computers will replace manual tasks with the hope to get results faster and with fewer errors [19]. For endodontically treated teeth, with a likely further spread of CAD/CAM devices, clinicians may have the option of placing a permanent indirect restoration immediately after completion of endodontic treatment. As mentioned above, this approach is highly desirable in terms of endodontic success, as it limits or avoids temporary restoration failure.
Finally, another interesting evolution is the advent of “bio”-materials. Far more than just a buzzword, the addition of these three letters in front of the word “material” has a clear meaning, in that materials should not only be considered for their intrinsic qualities, but in the context of their integration in a living organism. Biomaterials are expected to behave and perform in a similar fashion as the tissue they replace. Therefore, their characteristics should be as close as possible to the tissues replaced. This should be kept in mind by clinicians when choosing the best strategy and most adapted material for tooth restoration. The current trend is to use materials whose mechanical properties are as close as possible to the dental tissues they replace [20], this is sometimes implied by the expression “biomimetics.”
For example, an important property to consider is the elastic modulus, which is the tendency of a material to be reversibly deformed when a force is applied to it. A significant difference of elastic modulus between the replacement material and the tissue replaced might result in inappropriate interfacial stress generation. The elastic modulus was determined to be about 19 GPa for dentin and 80–94 GPa for enamel [21]. In comparison, it is much higher in metals and other dental materials, for example, about 110 GPa for titanium, 200 GPa for stainless steel, 200 GPa for zirconium, and 300 GPa for aluminum oxide. This major difference in modulus suggests that metal posts in roots should be used with caution. In contrast, the elastic modulus of fiber posts ranges between 10 and 25 GPa, which is much closer to that of dentin [22].
The elastic moduli of currently available materials for coronal restoration are as follows: 10–15 GPa for hybrid resin-based composites [23], 10–17 GPa for glass ionomer [24], about 20 GPa for amalgam [25], 71 GPa for feldspathic porcelain, and 224 GPa for zirconia [26]. Interestingly, it has been shown that an increase in elastic modulus of the restoration from 5 to 20 GPa actually results in a 30 % reduction of stress at the tooth-restoration interface under occlusal load [27]. Hence, it seems to make sense that the deformation under load of the restorative materials should be as close as possible to that of the tooth, which according to the above values points to resin-based composites for dentin, and feldspathic porcelain for enamel. As illustrated, many clinical situations show that a lack of respect of these biomimetic concepts can result in a failure. Nevertheless, it is also possible to find other clinical cases where these concepts of integration are not respected, but where the restoration can still be considered a clinical success. In fact, clinical experience seems to illustrate that in dentistry, a treatment might be successful despite what we do, not because of what we do. Therefore, and given the lack of clear clinical evidence, risks pointed out by in vitro data need to be carefully appraised when restoring root canal-treated molar teeth.
7.4 Objectives of the Restoration of Endodontically Treated Teeth
Generally, goals of the restoration of teeth after endodontic treatments can be summarized in three main objectives: to restore tooth functions, to prevent infection or reinfection of the root canal space by providing a fluid-tight seal and to protect the remaining tooth structure against further tissue damage (Box 7.2).
Box 7.2. Objectives for the Restoration of Endodontically Treated Molars
-
To restore function
-
Mastication
-
Occlusal stability
-
Contact points with neighboring teeth to ensure protection of the marginal periodontal tissues
-
Aesthetics (to a lower extent in the posterior sector)
-
-
To prevent the infection or reinfection of the root canal space by providing a fluid-tight seal
-
An adequate tooth restoration increases the chances of healing when combined with an adequate root canal treatment and obturation
-
-
To protect the remaining tooth structure against further tissue damage, in particular tooth fracture
-
Increase of tooth longevity
-
Although these general objectives are not specific to molars, the latter appear to be the most commonly extracted teeth among endodontically treated teeth (81 %) compared to premolars (16 %) and incisors/canines (3 %) [28]. Here, particular attention should be paid to the reasons for extraction, which were mainly nonrestorable caries (>60 %), far ahead of persistent endodontic failure, nonrestorable root or cusp fracture, and iatrogenic perforation, which were in that study cited in about 9–12 % each.
The major tooth functions that need to be restored include mastication, occlusal stability, and protection of the marginal periodontal tissues by providing appropriate contact points with neighboring teeth. At the same time an esthetic result must be achieved, while this is typically less critical in the posterior than in the anterior dentition. The restoration of these functions is not specific to endodontically treated teeth, but common to all damaged teeth and will not be the focus of this chapter.
The second objective, to prevent infection or reinfection of the root canal space, is of prime importance regarding the long-term success of endodontic treatment, as will be discussed in the next section.
Finally, the third objective, to protect the residual tooth structure against further tissue damage (carious or noncarious causes), is particularly relevant to endodontically treated teeth. In cases of structural loss after caries removal or preparation, endodontically treated teeth require protection against fracture. This third objective is particularly important and critical in molars, since they receive most of the masticatory forces, as will be described further. Hence, this chapter will propose considerations to prevent this major cause for endodontic treatment failure.
7.5 Fluid-Tight Seal of the Root Canal System
After completion of endodontic treatment, the priority is to establish an adequate coronal seal to prevent any infection or reinfection of the root canal space. This important aspect is not specific to molars but common to all types of teeth. Is the quality of coronal restoration of equal importance as the quality of the root canal filling regarding the outcome of endodontic treatment? This question has been the subject of debate in the endodontic literature (Fig. 7.2). The discussion arose from a report that cases with good coronal restoration, regardless of the quality of endodontic treatment (conditions 3 and 4 in Fig. 7.2) were associated with a significantly higher success rate based on the absence of periapical lesion in a radiograph than the opposite situation (80 %, conditions 2 and 4 in Fig. 7.2) [29]. The same authors find, comparing the worst- and best-case scenarios (situations 1 and 4 in Fig. 7.1, respectively), success rates of about 20 % and 90 %, respectively.
Schematic diagram of possible clinical situations when restoring a root canal-treated molar (center). Clinical outcomes shown in cases 1–4 depend on the quality of both endodontics and restorative work, with better outcomes when both parts are done to quality criteria (red/green). See text for more details
Gillen and others [30] conducted a systematic literature review and meta-analysis of all papers published on this topic since the original work by Ray and Trope [29]. Based on new statistical analyses based on data from nine papers, they concluded that a better treatment outcome can be expected when performing both high-quality root canal treatment and restoration (situation 4 in Fig. 7.2) compared to either insufficient filling or root canal treatment (situations 2 and 3 in Fig. 7.2), where no significant difference in the odds of healing was observed [30].
In a best-practice approach, since it is clear that the highest treatment quality in both aspects results in the best chances of success, the joint and coordinated efforts of both endodontists and restorative dentists are necessary to achieve the best possible outcome. Importantly, these elements point out to endodontic specialists that a quality restoration is important for success of the endodontic treatment he/she performed. As mentioned above, a major reduction of survival after endodontic treatment is anticipated for teeth restored with temporary restorations compared to the teeth receiving a permanent restoration [1].
Along the same lines, in vitro data have pointed out that temporary materials (neither Cavit, conventional glass ionomer, or a combination of both) were unable to prevent bacterial leakage over a 2-month period, whereas a bonded-resin-based material was able to do so [31]. This problem becomes particularly striking, considering that nowadays the endodontic and restorative phases are more often in the hands of two different practitioners and treatment decisions are influenced by insurance coverage also. Hence, the joint and coordinated efforts of both endodontists and restorative dentists are necessary to achieve the best possible outcome for the patient.
Even when under the control of one general dentist, endodontic and restorative procedures are usually performed in two separate appointments. Therefore, one needs to consider approaches that can ensure immediate, reliable, and definitive sealing of the root canal system, very likely through an adhesive procedure. One possible approach is the one proposed by Magne’s group, called immediate dentin sealing (IDS). This procedure may consist of immediate placement of a bonding system at the surface of freshly cut dentin and was demonstrated to improve bond strength of indirect restorations as compared with delayed bonding procedure at the next appointment, when placing the restoration [32]. Hence, in the context of restoring endodontically treated teeth, IDS has a dual advantage: providing an immediate seal, and improving bond strength for the restoration to come (see Box 7.3). The additional placement of a thin layer of flowable resin-based composite at the entrance of the root canals and on the pulp chamber floor can also be recommended. It must finally be kept in mind that IDS requires the final restoration to be placed within the next 2 weeks after bonding placement. After longer periods, a reduction of the cohesion between bonding and resin-based composite was indeed observed [33], possibly due to the decay of free radicals within the adhesive layer, which reach undetectable levels in less than 1 month after light-curing [34]. An additional procedure including the placement of a silane agent is then required, as well as a fresh layer of bonding agent [35].
Box 7.3. Sealing the Endodontic Space
-
The combination of both good endodontic treatment and good coronal restoration results in significantly better endodontic treatment outcome
-
The placement of an adhesive resin-based composite layer at the entrance of root canals and over the whole surface of pulp-chamber and cavity immediately after completion of endodontic treatment represents the best way to prevent reinfection of the root canal system. This initial layer will serve as substrate for the subsequent adhesive restoration.
-
Immediate dentin sealing (IDS) is indicated first to reduce the risk of contamination of the root canal system associated with temporary restorations, and second, to increase bond strength of the future coronal restoration.
-
Ideally, the endodontist could/should take care of the placement of this initial layer. The subsequent placement of the permanent restoration as soon as possible requires agreement between both the endodontist and restorative dentist, both on best-practice restorative procedure and sequence.
As mentioned earlier, one of the objectives of the restoration of endodontically treated teeth is to protect the remaining tooth structure against further tissue damage, in particular tooth fracture. The major cause for increased susceptibility to fracture of endodontically treated teeth is the loss of hard tissue; it is important to weigh the impact of caries removal, preparation for coronal restorations, access cavities, or root canal preparation on tooth stiffness. This issue was evaluated in premolars in the classic work by Reeh and others [36], and the residual tooth stiffness relative to an unaltered tooth (100 %) was sequentially: 95 % after access cavity only, 80 % after occlusal cavity preparation, 54 % after two-surface cavity preparation, 37 % after MOD cavity preparation, 33 % after access cavity preparation, 34 % after root canal instrumentation, and only 32 % after root canal obturation.
In molars, the average residual tooth stiffness was reported to range between 81 and 95 % after an MO cavity preparation, and between 60 and 61 % after an MOD cavity preparation, depending on the cusp considered [37]. This is lower than what was observed for premolars, although it is problematic to directly compare the values of two separate studies. Nevertheless, it may be concluded that the reduction in tooth stiffness results mainly from cumulative tissue loss at the coronal level. To address this tooth weakening, three important clinical concepts need to be considered: the ferrule effect, the placement of post(s), and cuspal coverage.
7.6 The Ferrule Effect in Molars
The dental ferrule refers to a circumferential band of dentin of at least 1–2 mm of dentin coronal to the margin of the preparation for a full crown (Fig. 7.3). It has been suggested that the presence of a ferrule may reinforce endodontically treated teeth, the “ferrule effect,” especially in teeth restored with cast post and core [38]. It was also observed that an adequate ferrule lowers the impact of the other factors (post and core system, luting agents, or crown material) on the survival of endodontically restored teeth [39].
From left to right, an endocrown (no ferrule), a post and core (either fiber post and resin composite core or metal cast post and core) covered by a full crown (no ferrule), and a crown covering a post and core with apical extension of preparation margin, providing a 2 mm ferrule. The red arrow symbolizes the risks the apical extension may represent, here regarding the furcation, but in general regarding the respect of the biological width space
Most research was done with single-rooted teeth and comparatively little data are available on molars. In the two major literature reviews that focus on the importance of the ferrule effect, one did not mention a single work devoted to molars [38] and the other reported the critical need for more clinical trials that investigate an effect on molars [39]. Only one clinical study focused specifically on endodontically treated, restored molars, and concluded that the amount of tooth structure available for ferrule (evaluated retrospectively from bitewing radiographs) may not be a significant prognostic parameter [40]. However, two other clinical studies included molars [41, 42] and both reported improved survival for teeth with ferrule (93 % at 3 years [41] and 98 % at 5 years [42]) compared to teeth without ferrule (74 % [41], 93 % [42]). Notably, in these two studies molars represented less than half of the teeth and a minority of the failures [42].
Therefore, while from a mechanical standpoint a ferrule is logical and recommended whenever possible, it is somewhat speculative to generalize and recommend ferrules for all molars based on these data alone. Moreover, it should be kept in mind that occlusal loads on molars are mostly axial, whereas the ferrule effect has mostly been demonstrated to be effective in protecting single-rooted teeth against lateral and oblique forces.
Interestingly, in an in vitro study comparing the importance of ferrule in endodontically treated molars restored with full metal crowns, it was reported that the presence of a 2 mm ferrule was a determinant factor on the fracture resistance and fracture mode. However, the forces required to induce fracture were well above the physiological forces, or even parafunctional levels, either in the ferrule group (2035–2934 N) or in the no-ferrule group (1528–1879 N) [43]. As stated before, results based on one type of teeth should no longer be generalized to all endodontically treated teeth without any distinction, as it is often the case in the literature.
Hence, given the lack of solid evidence in favor of the need of ferrule in molars, it is questionable whether it should be achieved at the expense of the remaining tooth structure (Fig. 7.3) and it is questionable to make the decision to extract a molar based solely on the lack of ferrule. Interestingly, when dentists are made aware of the additional tissue loss (3–45 %) associated with complete versus partial coverage restoration in molars, over 50 % of the clinicians altered their initial choice of restoration design from full to partial coverage [44]. Besides, the preparation of a ferrule at any cost in case of little remaining coronal tissue might be associated with additional problems. Notably, the subgingival margin placement can lead to a reduction of the biologic width space (distance between crown margin and alveolar crest) below the required 2–3 mm and to difficulties with the margin impression, excess luting cement removal, and cleaning of the area by the patient. The alternatives, crown lengthening or orthodontic extrusion, represent additional costs and delay for the patient; details of these procedures are beyond the scope of this text. Given the significant progress made in adhesive dentistry, preservation of coronal tissue should be contemplated instead of ferrule preparation in molars, and alternative approaches such as so-called endocrowns should be considered, as will be described further.
Admittedly, endodontic treatment in molars is typically rendered when a major portion of enamel and dentin has been already lost due to caries. Moreover, there are molars that may have a guarded prognosis (see also Chaps. 2 and 8) but still require a restoration (Fig. 7.4). Obviously, there is a range of clinical scenarios in the restoration of molar endodontics, and a variety of possible solutions will be discussed below.
(a) Teeth 15 and 16 (#4, 3) with periapical lesions, 16 (#3) with a perforation of pulp chamber floor (arrows). Both teeth received root canal (re-) treatment, and the perforation of tooth 16 (#3) as well as the vestibular canals were obturated. Direct composite restoration on tooth 16 (#3) and composite endocrown placed on tooth 15 (#4). Teeth are clinically asymptomatic at 8 months, and there are no signs of pathosis either in the periapical or in the furcal regions. (b) Tooth 26 (#14) presenting with a large periapical lesion with overextended fill and inadequate coronal obturation. The apical size of the MB root canal was very large and an apical plug was placed, followed by the placement of a direct composite restoration. At the 1-year follow-up, the tooth is asymptomatic and there is evidence of bone fill; the patient decided to keep the composite restoration
7.7 Post Placement in Endodontically Treated Molars
The question whether post placement is indicated in the restoration of endodontically treated teeth is quite difficult to answer with a clear yes or no based on the available literature. There are numerous factors involved, such as the post material or diameter, the quality of the bonding interface between post and dentin, the core material, the crown material, the amount of residual tooth structure, and others. This makes studies difficult to compare, and probably accounts for the contradicting results found in the literature. Importantly, tooth type is a major factor to consider, and most of the studies evaluating post placement were done on single-rooted teeth. The results obtained for incisors or premolars are not directly transferable to molars, and each tooth type has specific characteristics, notably the major differences in occlusal load intensity and directions [45]. Hence, only studies involving molars will be considered here. As regards the type of post, fiber-reinforced composite posts present characteristics that support their use instead of metal posts, since as already mentioned their elastic modulus is much closer to dental tissues, while at the same time displaying a fracture strength of 600–1100 MPa [22, 46], in other words, lower than metal posts (around 1400 MPa) but still much higher than dentin (200 MPa) [46]. It has also been suggested that the consequences of root fracture are more severe with metal posts than with fiber-reinforced composite posts [47]. In addition, the latter can be bonded to both root canal surface and resin-based restorative materials, which is not the case of their metallic counterparts. Hence, even if metal posts have been used for years in the clinics, the present chapter will only address the interest of using or not fiber posts in molar restoration.
7.8 Bonding in the Root Canal: The Worst-Case Scenario
Even in the event that a post is required (which as will be discussed below, does not seem to be clearly the case in molars), several aspects make its bonding procedure difficult.
First, it is not trivial to clean the root canal dentin and prepare it for bonding. Following endodontic treatment, obturation, and post space preparation, large areas of the root canal walls were indeed shown to be covered with smear layer, debris, and materials (sealer or gutta-percha) [48], which interfere with the post bonding efficiency. Since NaOCl was also demonstrated to decrease the bond strength [49], there may be an interest of neutralizing this effect by use of antioxidant such as sodium ascorbate [50, 51]. In Lai’s work, control of abundant rinse with water prior to bonding is lacking, while in Vongphan’s paper, there is no significant difference between control and when abundant water rinse is performed after NaOCl. Hence, it is still unclear whether or not this additional step is really beneficial.
Second, the ease of bonding procedure (etching, rinsing, primer application, drying, bonding application), resin-material injection, and photopolymerization is not as straightforward in the root canal space as in the coronal portion, which can result in lower bonding quality, more voids, or suboptimal resin polymerization [52].
Third, another major limitation of the bonding procedure in the root canal is related to the well-known polymerization shrinkage of resin-based composite, and the resulting stresses generated on the surrounding tooth structure. If the shrinkage stress exceeds the bond strength of the adhesive system to dentin, gaps form along the interface [52]. The magnitude of shrinkage stress is related to a parameter called “C-factor,” which refers to the ratio of the bonded surfaces to the unbonded ones [53]; the higher the C-factor, the greater is the shrinkage stress [54]. Significant bond strength reduction is already observed when increasing C-factor from 1 to 3 [55], and the C-factor values in root canals are expected to be much higher, since theoretically every dentin wall can be considered to have an opposing wall, and therefore very few surfaces are unbonded [52]. It is interesting to notice that the addition of a post as compared to filling the root canal with only resin results not only in a massive increase of C-factor, but also to a significant reduction of microtensile bond strength to root canal dentin (7.3–9.6 MPa with a post compared to 20.4–39.8 MPa without a post) while variations of resin volume by modifications of root canal width did not seem to affect bond strength [56].
Finally, higher bond strength values have been reported in coronal compared to apical dentin [57]. This questions the interest of preparing long post spaces, as compared to using only the coronal portion of the root canals, such as in the endocrown strategy, which will be described further.
All these limitations explain why bonding posts in the root canal is probably the worst-case scenario, with a particularly important risk of debonding and gap formation between post and root canal dentin, and low dentin bond strength. Additionally, there is concern of the stability of this little predictable bond with time, especially after repeated thermal, chemical, and mechanical stresses [58]. Indeed, Bouillaguet et al. [57] state that “clinical failure is not seen when sufficient coronal dentin is available because the restoration does not rely heavily on the bonding of the post to the root dentin.” This then logically questions the rationale of using posts to increase the restoration retention and/or reinforce the teeth.
7.8.1 Do Posts Reinforce Endodontically Treated Molars?
Based on in vitro studies, it is generally considered that the use of posts does not increase the fracture resistance of endodontically treated teeth [3], but these data are mostly based on metal post restorations, which do not bond to the dentin structure. Hence, it is worth revisiting this question with fiber-reinforced composite posts, and specifically regarding molar restoration.
Unlike for metal posts, in vitro data seem to highlight a possible strengthening effect of fiber posts on endodontically treated teeth. Again, a large majority of works addressing the use of posts to reinforce teeth included singe-rooted teeth. Let us consider those specifically focused on molars. In an in vitro work quoted earlier regarding the role of ferrule, a significantly higher fracture resistance was observed for teeth with posts (around 2900 N with ferrule, around 2000 N without ferrule and no significant difference between glass fiber and cast posts) than without posts (around 2000 N with ferrule, around 1500 N without ferrule).
Cast posts were associated with the highest rate of nonrestorable failures (80–100 %), whereas nonrestorable failures were reported in only 10–30 % of teeth with fiber posts or without posts (25° load direction) [43]. In another in vitro study, it was concluded that fiber post placement does not increase fracture resistance of endodontically treated mandibular molars with one or two remaining cavity walls in case of indirect composite overlay placement (fracture resistance around 1000 N for restored teeth after fatigue compared to 2992 N for intact teeth) [59]. However, they also observed that fiber post insertion could lead to more restorable fractures in case of extra axial loads (65 % nonrestorable fractures without post and 30 % with post) (45° load direction). Similar observations were again made when comparing different onlay materials (gold, composite, and ceramics) on MOD cavities with buccal and lingual cusp coverage, that is, fracture resistance ranging from about 1600 N (for ceramic and composite inlays) to 2900 N (for gold inlays), again well above physiological and parafunctional forces in all cases [60]. The effect of fiber post placement was not significant for composite or ceramic onlays, but well for gold onlays (about 2300 N without post and about 2900 N with post). Another study investigated direct composite restorations of root canal-treated molars with or without fiber posts, and reported fracture resistance ranging from 700 to 1600 N, depending on the number of remaining cavity walls [61]. They concluded that fracture resistance is not affected by the presence of fiber posts, but depends mostly on the number of residual walls, with a significant reduction of fracture resistance observed with less than two remaining walls. A higher proportion of nonrestorable failure was observed for restorations with fiber posts (0–50 %) than without (40–70 %). Another study by the same group investigated fracture resistance of root canal-treated molars restored with zirconia crowns, with different degrees of coronal tissue loss. They reported a significant improvement in fracture resistance with fiber posts (average ranging from about 1200 to 1450 N, with 20–33.3 % of nonrestorable fractures) compared to without posts (average ranging from about 1150 to 1250 N, with 6.7–20 % of nonrestorable fractures) [62].
In summary, based on in vitro studies, there is no consensus on the effect of fiber posts on endodontically treated molars, since some of them support a reinforcement and others do not. The common finding of all these in vitro data points is that failure occurs above normal intraoral forces, or even parafunctional forces which have a range from 700 to 1000 N in the posterior mandible. Hence, it is questionable whether or not the differences observed well above physiological forces, as well as the conclusions regarding restorability after failure, are in any way related to the clinical reality. All the conditions might very well be equivalent under physiological forces.
Considering clinical data, a meta-analysis on the subject concluded that the use of post retention had no significant influence on tooth survival after endodontic treatment, and a substantial heterogeneity among the included studies was deplored [7]. By contrast, a prospective study on tooth survival by the same group reported that teeth with cast post-and-core restorations were 2.6 times more likely to be extracted [1]. Since almost 90 % of the extracted teeth with cast post and core were premolars and molars, they concluded that the use of such retention systems should better be avoided in posterior teeth, and replaced by alternative treatment options [1]. They also reported that despite the large number of teeth included (1,617 teeth), the statistical power was not sufficient to test the interaction between factors, notably tooth type or post and core material, due to the small number of failures. The lack of consideration of tooth type in the majority of the clinical studies on endodontically treated teeth survival is a major limitation to determine whether or not the placement of posts participate in the reinforcement of endodontically treated molars specifically. As pointed out earlier [3], more clinical studies taking into account tooth type are required to determine whether or not a post should be used.
Among the few studies including molars, two reported no influence of post placement on restoration survival, one comparing at 5 years between cast post and core, direct post and composite core restoration and post-free all-composite core restorations [42], and the other direct composite resin-core-crown reconstructions with or without prefabricated metal posts [63]. However, the use of metal posts with composites is not an appropriate association, as mentioned earlier, and molars represented only 20–25 % of the teeth in both studies.
Several other studies investigating fiber posts included molars, but all were lacking appropriate controls, that is, molars with comparable tissue loss and without fiber post were not included. For example, Mancebo et al. evaluated the survival of root-treated teeth restored with fiber post and composite core covered by a crown, but molars represented only 18 % of the teeth included, only 3/14 failures, and most importantly no control without posts were investigated [41]. Another retrospective study evaluated the long-term performance of three types of fiber posts after a service period of 7–11 years. Almost 1,000 posts were in the study, with a total of 79 failures, 39 for endodontic reasons and 40 actual restoration failures. It was concluded that fiber posts “may be used routinely for restoring endodontically treated teeth” [64]. The evidence provided is again insufficient to determine if fiber posts should be used, since again no control without posts were considered, and only about 20 % of the teeth were molars, which represented only 13 of the 40 restoration failures, all due either to post debonding or to crown dislodgement.
In fact, to clearly determine whether fiber posts participate in endodontically treated molar reinforcement, a randomized clinical study would need to evaluate restoration with and without posts, for a given tooth type, and for similar levels of tissue destruction. To our knowledge such study does not exist for molars. This is further underlined in a prospective study evaluating the risk factors for failure of glass-fiber-reinforced composite post restorations, which concluded that tooth and restoration type as well as remaining cavity walls were significant predictors of endodontically teeth restoration failure [6]. In their work, a two to three times higher failure rate was observed in restorations placed in incisors or canines compared to those placed in premolars or molars. Though, as mentioned by the authors themselves, some limitations such as small sample size and small number of failures led to small statistical power. Once more, no control without posts was considered, and no specific focus was put on molars. The authors explain the higher failure rate in anterior teeth by the fact that fatigue fractures are caused by tension stress and not by compression, and the anterior region is therefore considered to be an area of higher risk, compared to molar areas, which bear less nonaxial forces. However, their results are in contradiction with the meta-analysis by Ng et al. [7] and the practice-based research by Skupien et al. [4], which report increased survival of nonmolar endodontically treated teeth, irrespective of the presence or absence of a post.
Bitter et al. considered the level of tissue loss and compared restorations with or without fiber posts (mean observation period of 32.4 months, 90 patients, 120 teeth). They concluded that fiber post placement is useful to reduce restoration failures of endodontically treated teeth with no remaining coronal wall, whereas no significant effect was shown in teeth with one or more remaining coronal walls [65]. Unfortunately, tooth type was again not considered, and the low number of failures of molars restored without posts (3/37) and with posts (0/25), which again is insufficient to conclude regarding the advantages of using posts in molars. The result of a recent practice-based study (almost 800 teeth, mean observation time 4.5 years, 50 % were molars, 700 without posts, 100 with post, post type not specified) concluded that the use of posts had no significant effect on either tooth survival or restoration success [4], though again the influence of post specifically on molar teeth could not be evaluated. The authors bring up the fact that the longevity of teeth and restorations do not only depend on the restorative considerations but also on factors related to the practitioner and the patient [66]. This is a very important aspect, since, as mentioned by Skupien et al., the dentist’s decision making may for example result in teeth with a more important coronal breakdown receiving a post [4].
In summary, it appears that clinical data are insufficient to justify the use of posts to reinforce endodontically treated molars. As stated by Al-Omiri and others, the guidelines are mainly based on in vitro studies and only limited in vivo material [2]. More long-term randomized controlled clinical trials taking into account tooth type and the loss of coronal structure are clearly required to reach an irrefutable conclusion regarding the use of posts to prevent fracture of endodontically treated molars [2].
7.8.2 Do Posts Increase Restoration Retention?
Posts are generally suggested to increase retention in case of large hard tissue loss, usually with less than two remaining cavity walls [3]. Several restorative strategies are in fact possible, as summarized in Fig. 7.5.
Schematic of the various restorative options when restoring endodontically treated molars with large tissue loss. (1) No post placement, core buildup without root canal anchorage, and full crown. (2) No post placement, core buildup with root canal anchorage, and full crown. (3) Placement of one or several post(s) in the root canals and core buildup, or placement of a cast post and core, and full crown. (4) Endocrown
To our knowledge, there is no clear consensus on which of these strategies provides the best restoration retention. A first issue is the variability of materials used for each of these strategies. Considering Fig. 7.5, it is clear that depending on the materials selected for the crown, the core, and the post, different behaviors and performances can be expected. Specifically, in situations 1–3, the properties of the core composite material, which will account for an important part of the flexural behavior of the coronal part of the tooth, may vary significantly (e.g., flexural strength from 57 to 125 MPa, and elastic modulus from about 3 to 13 GPa) [67]. Often, flowable dual-cured or self-cured materials are used by practitioners both for post bonding and for a fast one-step core buildup.
The mechanical properties of these materials are often inferior to those of highly filled light-cured composites. In addition, the multiplication of interfaces (Fig. 7.5, situation 3: dentin-post, dentin-core, core-crown, etc.) might increase the probability of flaws, and partial restoration debonding. On the contrary, the endocrown (Fig. 7.5, situation 4) allows the use of a single high-performance material (indirect composite or ceramics) and a single interface (crown-dentin). This variability of materials and interfaces between the different restorative options might account for the fact that the most frequently reported reasons for clinical failures of fiber post restorations were post debonding and post fractures, in some cases with core fracture [65]. This is probably linked to the difficulty to predictably bond in the root canal, as it was earlier alluded to. Since the loss of restoration retention was associated in most cases with the presence of little remaining coronal tissue, the authors concluded that the mechanical failures were due to the lack of coronal tooth structure [65]. These observations clearly question the added value of fiber posts, since the lack of tooth structure is precisely when the use of posts is recommended. Unfortunately, no control without post was included and it is therefore unclear whether posts are really appropriate to improve restoration retention. Finally, as previously mentioned regarding the risk of fracture, there are major issues accounting for the absence of consensus regarding the use of fiber posts, mainly the lack of consideration of tooth type and level of tissue loss in the majority of the clinical studies, as well as the limited number of failures in some studies.
Hence, even if it cannot be completely excluded that fiber posts may participate to increase restoration retention in molars, the evidence is very weak. It seems that endodontically treated molars rarely, if ever, require a post for restoration retention [58]. First, molars provide more coronal tooth structure, hence a larger bonding area as compared to anterior teeth and in general a large pulp chamber. Second, as already mentioned, they are mostly submitted to vertical forces [58, 68], while fiber posts may resist mainly against lateral forces. Third, the use of adhesive strategies has become more and more reliable (see Fig. 7.6); the necessity of using posts is therefore questioned by current in vitro data and clinical results using adhesive restorative strategies.
7.9 A New Treatment Option: The Endocrown
The absence of requirement of post placement in molars is further highlighted by recent promising results reported for a new type of adhesive restoration called the “endocrown.” Endocrowns are in fact large adhesive inlay-onlay restorations used to restore endodontically treated teeth with large tissue loss. They can either extend to the pulp chamber when present (Fig. 7.7), or in case of very shallow or inexistent pulp chamber, they may also be bonded on an almost flat surface after obliteration of the root canal entrances (Fig. 7.6).
According to in vitro data, endocrown restorations in molar teeth are quite promising compared to conventional crowns associated with fiber posts. Finite element analyses in a molar model revealed lower levels of stress (compressive, tensile, and shear) in teeth restored with ceramic endocrowns than in those restored with either fiber or cast post and a conventional full crown [69], the highest stresses occurring in teeth restored with fiber posts. In any case, contact stresses around the restorations were not higher than 1.6 MPa, which is much lower than the bonding strength reported between the bonding system and tooth tissues (around 30 MPa). Hence, according to the authors, ceramic endocrowns in molars have a low risk of fracture or debonding under physiological loads [69]. They further underline the interest of such adhesive restorations in molars by stressing first their minimally invasive preparation of tooth structures and lower risk of root damage, and second, the more favorable ratio between crown height and width in molars, which leads to smaller forces exerted on restorations compared to incisors for example, with a much larger restoration-tooth interface. Of course, any flaw within the material can increase the risk of restoration fracture, and any procedural mistake during the bonding procedure can favor debonding. Moreover, the reduction of bond strength with time under load and temperature changes, which is material specific, needs to be kept in mind [70]. In fracture strength experiments, ceramic endocrowns were shown to be more resistant to compressive forces than teeth restored with fiber posts, composite core, and conventional full crowns. In both cases, failure occurred by fracture of the tooth in most cases [71]. Again, fracture strength values were higher than physiological forces and the compression load was applied with a 45° load direction, which may not correspond to most situations in the molar region, where most forces are probably axial.
These promising in vitro results are confirmed by clinical studies. One study investigated CAD/CAM ceramic crowns placed in posterior teeth ranked in three different groups with various stump height (bondable and retentive surface) with one group of 70 molars that had only a pulp chamber retention cavity [72]. Among the molars, no significant difference in survival was observed between the three groups, with a survival of up to 94 % after a mean service life of 55 ± 15 months. As mentioned by the authors, comparable survival rates have been previously documented for conventional metal-ceramic or all-ceramic crowns. Of the 70 molar endocrowns, nine were lost due to adhesive failure, two because of vertical root fractures (similar same as conventional crowns), two for other reasons. In that study the major cause for failure was debonding, which is a restorable failure. Interestingly, while molars in the classic and reduced groups presented some fracture of ceramics (five molars), no ceramic fracture could be observed in the endocrown group [72]. This is in accordance with in vitro data, reporting superior fracture resistance of monolithic ceramic restorations compared to their porcelain-veneered counterparts [73].
In another clinical study including mostly molars (142 molars, 40 premolars), it was reported that large ceramic bonded restorations placed in endodontically treated teeth showed a similar failure rate compared to those placed in vital teeth (5-year failure rate of about 10 % for endodontically treated teeth and about 7 % for vital teeth) [74]. A 15-year prospective study by the same group included different groups depending on the degree of tooth preparation, among which 14 premolars and 14 molars were endodontically treated, without retention or post and core treatments (64 premolars and 188 molars total) [75]. Contrary to the short-term study, it was reported that ceramic restorations failed significantly more on nonvital teeth (39 %) than on vital teeth (21 %) after a mean observation period of about 13 years. Interestingly, the main reasons for failure were restoration loss and ceramic fracture (without differentiation between vital or nonvital teeth), which were easy repairable; only three root fractures were reported.
Another clinical study evaluated the survival of 53 endodontically treated and morphologically compromised molars restored with monolithic CAD/CAM ceramic endocrowns, and reported a success rate of 94 % after 4 years [76]. Failures were due to debonding (one tooth, restorable failure), restorable fracture (one tooth), secondary caries (one tooth, restorable failure), and one extraction due to persistent pain. Finally, another study investigating the survival of indirect composite onlays in posterior endodontically treated teeth (158 molars and 31 premolars) reported about 97 % restoration survival over a period of 24–52 months [77], which is in the same range at the survival reported for all-ceramic and metal-ceramic crowns at 5 years (up to 96 %) in a systematic review [78]. These data seem to indicate that overlay restorations are a reasonable option to restore endodontically treated molars.
Beyond the promising survival rates, this restoration strategy presents other advantages; importantly it does not require significant tissue removal for the placement of the restoration. It must be kept in mind that in molar endodontics, each restorative procedure significantly increased the amount of lost hard tissue volume [79]. Endocrowns are clearly a more conservative approach, which reduces the risk of procedural accidents such as root perforations or loss of the apical canal seal [58]. Moreover, post space preparation may increase the chances of root fracture [68]. Finally, deep cervical placement of restoration margins is not needed, which enables maximum conservation of enamel. This is crucial to obtain a predictable and efficient bond.
In conclusion, there is a lack of clear evidence regarding the need to use posts to restore endodontically treated molars. Even if there is not sufficient evidence to say that fiber posts should be avoided, evidence is accumulating to show that the loss of tooth structure is a factor favoring tooth fracture. Hence, if in view of the pros and cons presented above for the use of a fiber post, clinicians are still convinced that a post is necessary to restore endodontically treated molars, they should by all means avoid any further tissue loss; removal of root canal filling material should be sufficient and NO additional space for the post should be created using drills. However, given their promising results and specific advantages of the endocrown option, it is our opinion that these adhesive procedures appear as a preferable choice.
7.10 Placement of Full Crowns After Molar Endodontics: Clinical Data and Study Biases
According to several studies, the presence of full or partial, direct or indirect restoration does not seem to affect the success of endodontic treatments [4, 8, 80]. However, there is a general assumption that survival of endodontically treated teeth is improved when systematically providing a full crown after the endodontic treatment. In a systematic literature review, it was reported that tooth survival for root canal-treated teeth restored with a crown or with a direct restoration decrease to about 81 ± 12 % and 63 ± 15 %, respectively, at 10 years [81]. However, that study made no distinction regarding the amount of tissue loss or the type of tooth. Moreover, the authors actually considered mainly survival of the restoration, not of the tooth, since failure was considered as: fracture of the tooth, fracture of the restoration, post fracture, post decementation, dislodgment of the restoration, marginal leakage of the restoration, and tooth loss, and several of these failure events are restorable.
The assumption that a crown is systematically required after root canal treatment is supported either by prospective studies without randomization [1] or by retrospective studies. For example, in a large epidemiological study including almost 800,000 molars [82], it was reported that among the 3 % of extracted teeth at 8 years, the number of teeth without crown (large amalgam or composite restoration, or no restoration at all) was more than sixfold higher compared to teeth with crowns. However, such comparison was not provided among the 97 % of retained teeth. The lack of randomization between full indirect restorations and partial direct restorations in the available studies represents a major bias [8], since the amount of remaining tissue and/or the tooth prognosis play a major and subjective part in the decision making. This is clearly illustrated by a recent Cochrane review, concluding that “there is insufficient evidence to support or refute the effectiveness of conventional fillings over crowns for the restoration of root filled teeth. Until more evidence becomes available clinicians should continue to base decisions on how to restore root filled teeth on their own clinical experience, while taking into consideration the individual circumstances and preferences of their patients” [83]. Hence, personal guidelines or preferences followed by the practitioners for the restoration of endodontically treated teeth will affect the outcomes one way or the other. For example, on the one hand, a practice-based study reported that the survival of endodontically restored teeth restored with resin composite was superior to crowns [4]. Interestingly, the authors specify that endodontically treated teeth were restored routinely with a direct composite and that the placement of crowns was limited to severely damaged teeth, the latter being therefore more at risk of fracture.
On the other hand, other studies used the exact opposite reasoning; for example, teeth with poor prognosis may be considered not worth the investment of a crown [5]. This is supported by the observation that teeth presenting a periapical lesion before the restoration were significantly less likely to receive a crown (64 %) than teeth without a lesion (76 %) [8]. Therefore, teeth with a better long-term prognosis may be more likely to receive a crown, which introduces an important risk of bias in the conclusions drawn from observational studies and can lead to an overestimation of the effect of crown restoration on tooth longevity. Moreover, it has been suggested that patients who can afford crown placement might have a higher socioeconomic status and dental awareness, both potentially affecting tooth longevity [5]. In addition, cuspal coverage is provided in all cases for full crown restorations, whereas it is not a routine procedure when performing a more conservative direct restoration.
High-quality randomized controlled clinical trials are needed, which have to consider tooth type and remaining coronal tissue, to evaluate the importance of partial direct, indirect or full-crown restoration (Box 7.4).
Box 7.4. Tooth Reinforcement and Restoration Retention
-
There is insufficient evidence to support the necessity to systematically establish a ferrule in ET molars.
-
Fibers posts do not seem to reinforce endodontically treated molars. In vitro works, report that failure with or without posts occurs well above normal intraoral forces, or even parafuntional forces. In clinical studies, the data are insufficient to justify the use of posts to reinforce endodontically treated molars.
-
Endodontically treated molars rarely, if ever, require a post for restoration retention since molars provide a large bonding area and are mostly submitted to vertical forces (whereas fiber posts help resist against lateral forces).
-
If practitioners still want to place fiber posts, they should not remove additional tissue to prepare the post space and avoid any procedural errors, such as root perforation.
-
Adhesive strategies such as “endocrown” or overlays are considered increasingly as a reliable option, based on the accumulating evidence of in vitro and clinical works. They represent an efficient and more conservative approach, although more clinical studies are needed to fully confirm this trend.
7.11 The Relevance of Cuspal Coverage
One current strategy suggested to make endodontically teeth less susceptible to fracture is to provide cuspal coverage. This is supported by some studies that suggest improved longevity of fully crowned teeth, but one has to consider the mentioned study biases. As concluded by Ng et al. [1], the systematic provision of full crown coverage is probably a large exaggeration of the true need, since it requires further removal of tooth tissue from an already weakened tooth. These authors recommend that the restoration preparation should try to preserve as much remaining tooth tissue as possible, and partial cuspal coverage by overlays appears therefore as the restoration of choice for many endodontically treated molars.
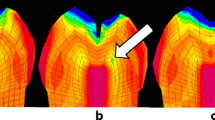
Regarding in vitro data, the interest of covering the cusps these teeth has first been described by Linn and others [37], who reported that cusp coverage with gold or amalgam overlays protects teeth with MO and MOD cavities against fracture. A finite element analysis reported that the reduction of buccal and lingual cusps and their coverage by an overlay results in a fourfold reduction of stresses generated in the dentin as compared with an inlay restoration without cuspal reduction [84]. Another in vitro study compared fracture resistance of root canal-treated molars with MO cavities, restored with either direct or indirect composite restoration with cuspal coverage [85]. They reported no significant difference, once again with values well above physiological forces (around 1400 N). Interestingly, values in the same range were reported when using direct composite to restore cavities with two or more remaining walls, but without cuspal coverage (from 1200 to 1600 N) [61]. However, the resistance values dropped significantly for teeth with one or no remaining wall (700–800 N), though still above physiological values.
The importance of remaining tooth structure is also highlighted in a clinical study, investigating the success of direct restoration without cusp coverage (n = 220 teeth, 195 composite, 14 amalgam, 11 IRM), as a function of three types of remaining tooth structures [86]:
-
Type I: maximum remaining tooth structure, approximately Class I cavity, the remaining walls being more than 2 mm thick
-
Type II: moderate remaining tooth structure, approximately a Class II cavity, two walls minimum being more than 2 mm thick.
-
Type III: minimum remaining tooth structure, less than two walls being more than 2 mm thick.
The restoration success rates for Type I, II and III decreased from more than 94 % at 1 year to about 78 % (Type I), 45 % (Type II), and 18 % (Type III) at 5 years. This led to the conclusion that endodontically treated molars with little coronal tissue loss (Type I) can be successfully restored for a prolonged period with dental composite, and without cusp coverage. On the contrary, for teeth with larger tissue loss (Type II and III) the short-term success is quite high but it drops significantly with time. Importantly, in that study, success was defined as tooth needing a new restoration, a repair procedure, or an extraction (failures due to endodontic and periodontal reasons were excluded). Hence, restorable and non-restorable failures were not discriminated in the calculations. Finally, it is mentioned that over the observation period of up to 10 years, only 6 % of the teeth had to be extracted out of the 46 % total failures, which indicates that most failures were restorable.
Hence, the question whether or not all cusps should systematically be covered by the material remains unclear from the literature (see Box 7.5). Nevertheless, it seems reasonable to cover selectively any wall that appears too weak to withstand the high occlusal forces of the posterior area, especially in case of parafunctional forces (Fig. 7.8). It is also probably excessive to cover strong cusps (2 mm thickness or more being a reasonable estimate), given the paramount importance of coronal tissue preservation for fracture resistance. As to define what is a “strong” cusp, it is quite difficult to provide an absolute thickness threshold, but it is reasonable to state that 2 mm represent a strict minimum.
Box 7.5. Cuspal Coverage
-
Full crown is not systematically required after root canal treatment of ET molars. Even if this is supported by most of the available literature, this is probably an overtreatment, given the numerous biases in the clinical studies. Many factors such as tooth type, extent and distribution of tissue loss, or else type and material of final restoration need to be considered to decide for the appropriate restorative strategy.
-
Cuspal coverage of ET molars seems reasonable for any cavity wall that appears too weak to withstand the high occlusal forces of the posterior area, especially in case of parafunctional forces.
7.12 Direct or Indirect Restoration: Selection of Material and Clinical Procedures
Two major aspects to consider when considering a direct or an indirect restoration strategy are the restitution of tooth anatomy and the biomimetic properties of the material.
Regarding the first aspect, it is clear that the larger the restoration, the more difficult it is to recreate good proximal contact points, occlusal anatomy, and optimal contact with opposing teeth. Hence, it is common clinical sense that large restorations, that is, when one cusp or more are to be restored, will be more easily and more predictably prepared indirectly. This is also supported by clinical studies, reporting that the longevity of direct restorations decreases when the number of restored surfaces increases [87, 88].
Biomimetic properties of a restorative material (Fig. 7.8) relate to how well the material mimics the properties of the replaced dental tissue, mainly esthetically and mechanically; two material classes are applicable here: resin-based composites and ceramics. Between and within these two material classes, a wide range of biomechanical characteristics can be described. It is not the purpose of the present chapter to review every material available, but to provide the reader with general important principles.
According to the objectives presented above for the restoration of root canal-treated molars, the material chosen should both restore function and prevent any further damage to the tooth. In this regard, one important aspect is then to avoid the generation of stresses within the remaining tooth structure. Finite element analyses have shown that increasing the elastic modulus of the restoration material from 5 to 20 GPa leads to a significant reduction in stresses in the neighboring dental tissues [27], whereas a further increase above 20 GPa results in a stress increase [84].
Only highly filled composites reach the lower bounds of this range, and these materials also happen to possess the highest flexural strength and microhardness [23]. Accordingly, such high-performance composites should be favored for direct restorations, while materials with low mechanical properties such as the recent bulk-fill composites should be avoided [89]. Finally, given the major importance of irradiation protocols on the final composite properties [90], it is recommended that composites are placed in 2 mm increments, each one being light-cured during 20 s at a light irradiance of about 1000 mW/cm2 [91].
For adhesive indirect restorations, recommended in case of large tissue loss, CAD/CAM blocks appear to be the best current available option. Among materials available in that category, there is currently no clinical evidence that ceramics perform better than composites for onlay restorations [92]. Hence, the choice must currently be made based on the available in vitro data.
Purely at the material level, lithium disilicate blocks were so far considered as the best combination of high flexural strength and resistance to fatigue degradation, while resin composite blocks outperformed glass-rich ceramics [93]. However, none of the available materials perfectly mimics the properties of the replaced tissues. For example, the elastic modulus of lithium disilicate (around 70 GPa) [94] is indeed much higher than dentin, and in fact in the range of the values of enamel. As described for direct composites, the elastic modulus of composite blocks with dispersed fillers approaches the lower values reported for dentin [94, 95]. Another recently introduced composite block technology is based on a polymer-infiltrated ceramic network [94, 95]. The latter represents an interesting new avenue for indirect restorations, since it presents intermediate properties between dentin and enamel [95].
To sum up, in absence of a clear advantage of one material over the other, it appears that both lithium disilicate and high-performance composite represent appropriate options for the restoration of molars. Glass-rich ceramics and low-performance artisanal indirect composites should now clearly be avoided [93, 95].
Despite the clinical procedures and materials recommended above based on the amount of remaining dental tissues and material specificities (summarized in Fig. 7.8), the restorative dentist may have to opt for a direct composite restoration even in a case that an indirect restoration was indicated. The main reason is when the tooth is compromised, either due to the guarded prognosis of the endodontic treatment (Figs. 7.1i and 7.4a, b), or to other issues such as periodontal problems. In such cases, a direct restoration with high-performance composite materials is a valid temporary alternative, while endodontic success is evaluated. As mentioned before, large direct composite restoration in root canal-treated molars have good short-term prognosis (<2 years), even with little remaining coronal tissue [86]. Hence, such a restorative approach can be performed to temporize, and leave some time to evaluate healing. Then a more durable strategy can be performed, such as full crown, or overlay, except if the patient cannot afford the cost of an indirect restoration, in which case the direct composite may become a permanent option (Fig. 7.8).
Regarding the bonding strategy for the adhesive restorative strategies recommended above, one-step adhesives or cements should be considered with caution, since they seem to be related to significantly lower in vitro and clinical performances [96] (Box 7.6). Accordingly, it is recommended to use the most efficient adhesive technologies, that is, either the three-step Etch & Rinse (e.g., Optibond FL, Kerr, Orange, CA, USA) or the mild self-etch products (e.g., Clearfil SE Bond, Kuraray US, New York, NY, USA), the latter possessing the additional advantage of creating a chemical bond to hard tissues when containing molecules such as 10-MDP (10-methacryloxydecyl dihydrogen phosphate), and being potentially less technique-sensitive [97]. In case of indirect restorative procedure, the application of a separate bonding system prior to the resin composite cement is also required, since it leads to increased bond strength [98].
Box 7.6. Bonding Procedure Recommendations
-
Prior to bonding, thoroughly clean the tooth substrate, for example, by air abrasion
-
Use the best available adhesive technologies, that is, a three-step Etch & Rinse (e.g., Optibond FL, Kerr) or a mild self-etch product (e.g., Clearfil SE Bond, Kuraray)
-
In case of indirect restoration, appropriately condition the overlay intrados: sandblasting for resin composites, sandblasting + etching with 5 % hydrofluoric acid for ceramics, followed by the application of a silane agent for both types of substrates
-
In case of restoration repair (which leads to increased restoration longevity), clean the surfaces with air abrasion, and optimize surface conditioning to the nature of the existing restoration; silanization is a must in any case
Specifically, for bonding to a dental substrate after an endodontic procedure, all adhesive substrates (enamel, coronal, and pulpal floor dentin) should be thoroughly cleaned, since any residue of endodontic sealer, sodium hypochlorite, or temporary filling agent is likely to interfere with bonding. For example, a negative effect of sodium hypochlorite on bonding was described for some bonding systems, an effect that could be reversed by use of antioxidants such as sodium ascorbate [50]. However, the negative effects of sealers and irrigants appear to be system-specific, and the restorative dentist is frequently not aware of all particular materials used by the endodontist. Hence, a nonspecific cleaning method prior to bonding, such as air abrasion, may be a more rational approach.
Following the cleaning of the dental surfaces and the application of the bonding system, the tooth will receive either a highly filled resin-based composite in case of a direct restoration, or a dual-cure resin composite cement followed by an onlay in case of an indirect restoration. The surface of the latter will need to be preliminary conditioned, that is, either sandblasted for resin composites, or sandblasted and/or etched with 5 % hydrofluoric acid for ceramics, followed by the application of a silane agent for both types of substrates.
7.13 Restoration Repair: A Rational Strategy
The points discussed above regarding an ideal restoration procedure concern all cases where the placement of a new restoration is considered. However, in many cases, the root canal system must be (re-) accessed, in presence of a satisfactory permanent restoration, for endodontic reasons (see Fig. 7.1i). In such cases, the practitioner must decide whether the existing restoration will be repaired, or replaced by a new restoration. Failing restorations or restorations presenting small defects are replaced by most clinicians [66], though this leads to an additional removal of sound tooth structure, and in general to a higher cost for the patient. Moreover, there is now cumulative evidence demonstrating that repair of restorations is not only a viable alternative to replacement, but one that leads to increased restoration longevity [66].
In fact, the mean survival period of existing crowns that had access cavity filled with a resin composite after root canal treatment was not different from new crowns, placed after root canal treatment [99] (Fig. 7.9). Such repair procedures must be conducted appropriately in order to restore the mechanical properties of the restoration as well as to provide optimal seal. Apart from the need to smoothen and clean the surfaces to repair (e.g., with a combination of bur and air abrasion), the nature and chemical specificities of the materials to be repaired must be carefully considered, and the products and strategies must be adapted to the substrate [35]. Composites need to be silanated prior to the application of a bonding system; ceramics need to be etched with 5 % hydrofluoric acid (with caution), then silanated prior to the application of a bonding system; metal surfaces require the application of a silica coating, then be silanated before the application of a bonding and a resin composite [53].
Example of a tooth with clinically satisfactory coronal restoration (full crown), but unsatisfactory root canal treatment. The retreatment was performed through the crown after access opening, and removal of the metal post. The access opening was then repaired by placement of a resin composite restoration
7.14 Restoration of endodontically treated molars as part of multi-unit restorations
The majority of this chapter was devoted to the restoration of isolated teeth, which represents the majority of the cases. Now the question that needs to be asked is how to restore after an endodontic treatment a tooth which will be part of a plural restoration (bridge, abutment, etc.). In fact, based on the available literature, the question that shall rather be asked is whether or not an endodontically treated molar be part of a plural restoration at all. The available data shows that the use of endodontically treated molar in plural restorations is subject to caution, reduced tooth survival being reported [4, 80]. This may be due to various causes, including higher occlusal stresses on the abutment teeth, different distribution of these stresses, with potentially an increased shear force component, or else the removal of a large amount of sound tissue to accommodate for the insertion axis. In light of these aspects, and given the good quality of modern implant strategies, it seems more reasonable to avoid the use of an ET molar as part of a plural restoration whenever possible. In spite of those considerations, if the use of a root-treated molar needs to be used as an abutment, the recommendations made above may need to be reconsidered. For example, a post insertion may in that case be more justified [3], as well as the creation of a ferrule.
In conclusion, for single-tooth restoration after molar root canal treatment, overall best practices suggest that clinicians consider the following during the restoration of root canal-treated molars:
-
Overall adequate amount of structure retained
-
Systematic need for ferrule and full crown contested
-
Partial indirect restoration considered
-
Cuspal coverage generally recommended
-
Bacteria-tight coronal seal maintained
-
Post placement avoided or critically evaluated
-
Appropriate restoration material selected and correctly placed
-
Biting pattern and functional forces considered
-
Repair considered whenever possible
References
Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44:610–25.
Al-Omiri MK, Mahmoud AA, Rayyan MR, Abu-Hammad O. Fracture resistance of teeth restored with post-retained restorations: an overview. J Endod. 2010;36:1439–49.
Peroz I, Blankenstein F, Lange KP, Naumann M. Restoring endodontically treated teeth with posts and cores – a review. Quintessence Int. 2005;36:737–46.
Skupien JA, Opdam N, Winnen R, Bronkhorst E, Kreulen C, Pereira-Cenci T, et al. A practice-based study on the survival of restored endodontically treated teeth. J Endod. 2013;39:1335–40.
Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002;87:256–63.
Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod. 2012;38:432–5.
Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43:171–89.
Chugal NM, Clive JM, Spangberg LS. Endodontic treatment outcome: effect of the permanent restoration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:576–82.
Azarpazhooh A, Dao T, Ungar WJ, Da Costa J, Figueiredo R, Krahn M, et al. Patients’ values related to treatment options for teeth with apical periodontitis. J Endod. 2016;42:365–70.
Dietschi D, Bouillaguet S, Sadan A. Restoration of the endodontically treated tooth. In: Hargreaves KM, Berman LH, editors. Cohen’s pathways of the pulp. 10th ed. St. Louis: Mosby Elsevier; 2011. p. 777–807.
Hidaka O, Iwasaki M, Saito M, Morimoto T. Influence of clenching intensity on bite force balance, occlusal contact area, and average bite pressure. J Dent Res. 1999;78:1336–44.
Varga S, Spalj S, Lapter Varga M, Anic Milosevic S, Mestrovic S, Slaj M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthod. 2011;33:427–33.
Kawata T, Yoda N, Kawaguchi T, Kuriyagawa T, Sasaki K. Behaviours of three-dimensional compressive and tensile forces exerted on a tooth during function. J Oral Rehabil. 2007;34:259–66.
Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van THMA, Witter DJ, Kalk W, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79:1519–24.
Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 2006;13:57–83.
Cheron RA, Marshall SJ, Goodis HE, Peters OA. Nanomechanical properties of endodontically treated teeth. J Endod. 2011;37:1562–5.
Giannobile WV, Lang NP. Are dental implants a panacea or should we better thrive to save teeth? J Dent Res. 2016;95:5–6.
Van Meerbeek B, Peumans M, Poitevin A, Mine A, Van Ende A, Neves A, et al. Relationship between bond-strength tests and clinical outcomes. Dent Mater. 2010;26:e100–21.
van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12.
Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature – part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38:733–43.
Xu HH, Smith DT, Jahanmir S, Romberg E, Kelly JR, Thompson VP, et al. Indentation damage and mechanical properties of human enamel and dentin. J Dent Res. 1998;77:472–80.
Zicari F, Coutinho E, Scotti R, Van Meerbeek B, Naert I. Mechanical properties and micro-morphology of fiber posts. Dent Mater. 2013;29:e45–52.
Leprince J, Palin WM, Mullier T, Devaux J, Vreven J, Leloup G. Investigating filler morphology and mechanical properties of new low-shrinkage resin composite types. J Oral Rehabil. 2010;37:364–76.
Magni E, Ferrari M, Hickel R, Ilie N. Evaluation of the mechanical properties of dental adhesives and glass-ionomer cements. Clin Oral Investig. 2010;14:79–87.
Bryant RW, Mahler DB. Modulus of elasticity in bending of composites and amalgams. J Prosthet Dent. 1986;56:243–8.
White SN, Miklus VG, McLaren EA, Lang LA, Caputo AA. Flexural strength of a layered zirconia and porcelain dental all-ceramic system. J Prosthet Dent. 2005;94:125–31.
Asmussen E, Peutzfeldt A. Class I and class II restorations of resin composite: an FE analysis of the influence of modulus of elasticity on stresses generated by occlusal loading. Dent Mater. 2008;24:600–5.
Zadik Y, Sandler V, Bechor R, Salehrabi R. Analysis of factors related to extraction of endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e31–5.
Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28:12–8.
Gillen BM, Looney SW, Gu LS, Loushine BA, Weller RN, Loushine RJ, et al. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod. 2011;37:895–902.
Rechenberg DK, Schriber M, Attin T. Bacterial leakage through temporary fillings in core buildup composite material – an in vitro study. J Adhes Dent. 2012;14:371–6.
Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94:511–9.
Dall’Oca S, Papacchini F, Goracci C, Cury AH, Suh BI, Tay FR, et al. Effect of oxygen inhibition on composite repair strength over time. J Biomed Mater Res B Appl Biomater. 2007;81:493–8.
Leprince J, Lamblin G, Truffier-Boutry D, Demoustier-Champagne S, Devaux J, Mestdagh M, et al. Kinetic study of free radicals trapped in dental resins stored in different environments. Acta Biomater. 2009;5:2518–24.
Hickel R, Brushaver K, Ilie N. Repair of restorations – criteria for decision making and clinical recommendations. Dent Mater. 2013;29:28–50.
Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512–6.
Linn J, Messer HH. Effect of restorative procedures on the strength of endodontically treated molars. J Endod. 1994;20:479–85.
Stankiewicz NR, Wilson PR. The ferrule effect: a literature review. Int Endod J. 2002;35:575–81.
Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: a literature review. J Endod. 2012;38:11–9.
Setzer FC, Boyer KR, Jeppson JR, Karabucak B, Kim S. Long-term prognosis of endodontically treated teeth: a retrospective analysis of preoperative factors in molars. J Endod. 2011;37:21–5.
Mancebo JC, Jimenez-Castellanos E, Canadas D. Effect of tooth type and ferrule on the survival of pulpless teeth restored with fiber posts: a 3-year clinical study. Am J Dent. 2010;23:351–6.
Creugers NH, Mentink AG, Fokkinga WA, Kreulen CM. 5-year follow-up of a prospective clinical study on various types of core restorations. Int J Prosthodont. 2005;18:34–9.
Santana FR, Castro CG, Simamoto-Junior PC, Soares PV, Quagliatto PS, Estrela C, et al. Influence of post system and remaining coronal tooth tissue on biomechanical behaviour of root filled molar teeth. Int Endod J. 2011;44:386–94.
Murphy F, McDonald A, Petrie A, Palmer G, Setchell D. Coronal tooth structure in root-treated teeth prepared for complete and partial coverage restorations. J Oral Rehabil. 2009;36:451–61.
Castro CG, Santana FR, Roscoe MG, Simamoto Jr PC, Santos-Filho PC, Soares CJ. Fracture resistance and mode of failure of various types of root filled teeth. Int Endod J. 2012;45:840–7.
Plotino G, Grande NM, Bedini R, Pameijer CH, Somma F. Flexural properties of endodontic posts and human root dentin. Dent Mater. 2007;23:1129–35.
Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36:609–17.
Serafino C, Gallina G, Cumbo E, Ferrari M. Surface debris of canal walls after post space preparation in endodontically treated teeth: a scanning electron microscopic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:381–7.
Ari H, Yasar E, Belli S. Effects of NaOCl on bond strengths of resin cements to root canal dentin. J Endod. 2003;29:248–51.
Lai SC, Mak YF, Cheung GS, Osorio R, Toledano M, Carvalho RM, et al. Reversal of compromised bonding to oxidized etched dentin. J Dent Res. 2001;80:1919–24.
Vongphan N, Senawongse P, Somsiri W, Harnirattisai C. Effects of sodium ascorbate on microtensile bond strength of total-etching adhesive system to NaOCl treated dentine. J Dent. 2005;33:689–95.
Schwartz RS. Adhesive dentistry and endodontics. Part 2: bonding in the root canal system-the promise and the problems: a review. J Endod. 2006;32:1125–34.
Schwartz RS, Fransman R. Adhesive dentistry and endodontics: materials, clinical strategies and procedures for restoration of access cavities: a review. J Endod. 2005;31:151–65.
Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21:17–24.
Yoshikawa T, Sano H, Burrow MF, Tagami J, Pashley DH. Effects of dentin depth and cavity configuration on bond strength. J Dent Res. 1999;78:898–905.
Aksornmuang J, Nakajima M, Senawongse P, Tagami J. Effects of C-factor and resin volume on the bonding to root canal with and without fibre post insertion. J Dent. 2011;39:422–9.
Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003;19:199–205.
Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30:289–301.
Scotti N, Coero Borga FA, Alovisi M, Rota R, Pasqualini D, Berutti E. Is fracture resistance of endodontically treated mandibular molars restored with indirect onlay composite restorations influenced by fibre post insertion? J Dent. 2012;40:814–20.
Salameh Z, Ounsi HF, Aboushelib MN, Al-Hamdan R, Sadig W, Ferrari M. Effect of different onlay systems on fracture resistance and failure pattern of endodontically treated mandibular molars restored with and without glass fiber posts. Am J Dent. 2010;23:81–6.
Salameh Z, Sorrentino R, Papacchini F, Ounsi HF, Tashkandi E, Goracci C, et al. Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fiber posts. J Endod. 2006;32:752–5.
Salameh Z, Ounsi HF, Aboushelib MN, Sadig W, Ferrari M. Fracture resistance and failure patterns of endodontically treated mandibular molars with and without glass fiber post in combination with a zirconia-ceramic crown. J Dent. 2008;36:513–9.
Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH. Composite resin core-crown reconstructions: an up to 17-year follow-up of a controlled clinical trial. Int J Prosthodont. 2008;21:109–15.
Ferrari M, Cagidiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, et al. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007;20:287–91.
Bitter K, Noetzel J, Stamm O, Vaudt J, Meyer-Lueckel H, Neumann K, et al. Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. J Endod. 2009;35:1477–82.
Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101.
Rüttermann S, Alberts I, Raab WH, Janda RR. Physical properties of self-, dual-, and light-cured direct core materials. Clin Oral Investig. 2011;15:597–603.
Bitter K, Kielbassa AM. Post-endodontic restorations with adhesively luted fiber-reinforced composite post systems: a review. Am J Dent. 2007;20:353–60.
Dejak B, Mlotkowski A. 3D-finite element analysis of molars restored with endocrowns and posts during masticatory simulation. Dent Mater. 2013;29:e309–17.
Peumans M, Hikita K, De Munck J, Van Landuyt K, Poitevin A, Lambrechts P, et al. Bond durability of composite luting agents to ceramic when exposed to long-term thermocycling. Oper Dent. 2007;32:372–9.
Biacchi GR, Basting RT. Comparison of fracture strength of endocrowns and glass fiber post-retained conventional crowns. Oper Dent. 2012;37:130–6.
Bindl A, Richter B, Mörmann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int J Prosthodont. 2005;18:219–24.
Zhang Y, Lee JJ, Srikanth R, Lawn BR. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater. 2013;29:1201–8.
van Dijken JW, Hasselrot L, Ormin A, Olofsson AL. Restorations with extensive dentin/enamel-bonded ceramic coverage. A 5-year follow-up. Eur J Oral Sci. 2001;109:222–9.
van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. 2010;26:929–39.
Ozyoney G, Yan Koglu F, Tagtekin D, Hayran O. The efficacy of glass-ceramic onlays in the restoration of morphologically compromised and endodontically treated molars. Int J Prosthodont. 2013;26:230–4.
Chrepa V, Konstantinidis I, Kotsakis GA, Mitsias ME. The survival of indirect composite resin onlays for the restoration of root filled teeth: a retrospective medium-term study. Int Endod J. 2014;47:967–73.
Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CHF. A systematic review of the survival and complication rates of all-ceramic and metal–ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res. 2007;18:73–85.
Ikram OH, Patel S, Sauro S, Mannocci F. Micro-computed tomography of tooth tissue volume changes following endodontic procedures and post space preparation. Int Endod J. 2009;42:1071–6.
Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44:583–609.
Stavropoulou AF, Koidis PT. A systematic review of single crowns on endodontically treated teeth. J Dent. 2007;35:761–7.
Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846–50.
Fedorowicz Z, Carter B, de Souza RF, Chaves CA, Nasser M, Sequeira-Byron P. Single crowns versus conventional fillings for the restoration of root filled teeth. Cochrane Database Syst Rev. 2012;5:CD009109.
Jiang W, Bo H, YongChun G, LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent. 2010;103:6–12.
Plotino G, Buono L, Grande NM, Lamorgese V, Somma F. Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J Prosthet Dent. 2008;99:225–32.
Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent. 2005;93:164–70.
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007;23:2–8.
Pallesen U, van Dijken JW, Halken J, Hallonsten AL, Hoigaard R. Longevity of posterior resin composite restorations in permanent teeth in Public Dental Health Service: a prospective 8 years follow up. J Dent. 2013;41:297–306.
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent. 2014;42:993–1000.
Leprince JG, Palin WM, Hadis MA, Devaux J, Leloup G. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent Mater. 2013;29:139–56.
Leprince J, Devaux J, Mullier T, Vreven J, Leloup G. Pulpal-temperature rise and polymerization efficiency of LED curing lights. Oper Dent. 2010;35:220–30.
Fron Chabouis H, Smail Faugeron V, Attal JP. Clinical efficacy of composite versus ceramic inlays and onlays: a systematic review. Dent Mater. 2013;29:1209–18.
Belli R, Geinzer E, Muschweck A, Petschelt A, Lohbauer U. Mechanical fatigue degradation of ceramics versus resin composites for dental restorations. Dent Mater. 2014;30:424–32.
Ruse ND, Sadoun MJ. Resin-composite blocks for dental CAD/CAM applications. J Dent Res. 2014;93:1232–4.
Mainjot AK, Dupont NM, Oudkerk JC, Dewael TY, Sadoun MJ. From artisanal to CAD-CAM blocks: state of the art of indirect composites. J Dent Res. 2016;95(5):487–95.
Poitevin A, De Munck J, Van Ende A, Suyama Y, Mine A, Peumans M, et al. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent Mater. 2013;29:221–30.
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28:215–35.
Ariyoshi M, Nikaido T, Foxton RM, Tagami J. Microtensile bond strengths of composite cores to pulpal floor dentin with resin coating. Dent Mater J. 2008;27:400–7.
Dammaschke T, Nykiel K, Sagheri D, Schafer E. Influence of coronal restorations on the fracture resistance of root canal-treated premolar and molar teeth: a retrospective study. Aust Endod J. 2013;39:48–56.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Leprince, J.G., Leloup, G., Hardy, C.M.F. (2017). Considerations for the Restoration of Endodontically Treated Molars. In: Peters, O. (eds) The Guidebook to Molar Endodontics. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-52901-0_7
Download citation
DOI: https://doi.org/10.1007/978-3-662-52901-0_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-52899-0
Online ISBN: 978-3-662-52901-0
eBook Packages: MedicineMedicine (R0)