Abstract
The objective of this chapter is to provide different treatment considerations to guide the clinician in the practice of evidence-based dentistry when performing treatment plans for endodontically treated teeth. As some of the existing literature is not clinically relevant, one must understand the limitations of published studies as they apply to clinical dentistry.
There are known clinical complications one could anticipate when attempting to restore a severely weakened vital or non-vital tooth with minimal residual sound tooth structure, incomplete ferrule, and fewer than two proximal contacts. The decision to endodontically treat a tooth should be based on its expected function within the entire dentition and whether or not it could predictably utilize its function for a long time. When the integrity of the enamel and dentin is compromised, one should consider coronal coverage, whether the tooth is vital or non-vital. Other chapters will discuss the different post and core materials and alternatives.
Ultimately, it is our responsibility to inform the patient of the risks/benefits and effort involved in attempting to maintain and restore a tooth.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
3.1 Introduction
The oral cavity… one of the most hostile environments there is. Yet, teeth have found shelter in it. The human tooth presents in various forms and shapes with a unique history of restorations and/or trauma. Stem cell-based biological tooth repair and regeneration is not part of the restorative dentist’s armamentarium just yet. However, as clinicians, we are often confronted with situations where we feel that we have to take upon the role of the “herodontist.” It is not uncommon for a patient to present with a dentition ornamented with different types of restoration materials: gold foil, silicate, amalgam, composite resin, and ceramics, just to name a few. Sometimes, a medley of these materials is present on the same tooth. Whether upon a routine examination or when evaluating an emergency patient with a trauma or a with a periapical lesion, practitioners must agree, in syntony with the patient, on the fate of problematic teeth. Before deciding on the outcome of a tooth with a periapical lesion or one that is extensively restored or severely damaged due to a carious lesions or trauma, the clinician must first assess the clinical status of the dentition as a whole, then that of the tooth, and have a clear understanding of the patient’s signs, symptoms, and chief complaint. Guided by the patient’s needs and preferences, and combining his or her experience with scientific evidence, the clinician must then practice the art of evidence-based dentistry. A methodological approach to every clinical situation can facilitate the thought process that takes place during treatment planning of the tooth, whether it is endodontically treated or not.
This chapter will discuss the treatment planning considerations that the clinician must walk through as he or she is faced with a moderate to severely damaged tooth with or without lesion of endodontic origin. After the establishment of a pulpal diagnosis, the evaluation of the remaining sound tooth structure and its relation to the periodontium, a decision is made on the restorability of the tooth. If it is restorable and the patient wishes to keep the tooth, one must consider the function the tooth will serve within the entire dentition and the stress it will be subjected to. In order to achieve full function and a predictable outcome, will the tooth require root canal therapy or a retreatment? Will the tooth necessitate a full coverage restoration with or without a post and core? Is there a ferrule effect or does the tooth need crown lengthening and/or orthodontic extrusion? This chapter will also be discussing the impact and outcome of such modalities. Finally, we will review different options if it is the patient’s final decision to extract the tooth.
3.2 Diagnosis
3.2.1 Assessing the Pulpal Status
An accurate diagnosis must be made to provide the appropriate treatment. After collecting the necessary information on the patient’s background through a meticulous medical and dental history, the clinician must pay careful attention to the signs and symptoms that are present in order to determine pulpal status. Even with an array of clinical tests, it is difficult to make a precise diagnosis as the pulp gradually evolves from one pulpal status to another. It is beyond the scope of this chapter to go in detail about endodontic diagnosis. Practically, we can say that root canal therapy is indicated when the pulpal status is irreversible pulpitis or pulpal necrosis. Nevertheless, when there is not enough sound tooth structure to serve as a foundation for a planned prosthetic procedure, it is sometimes indicated to perform an elective root canal treatment in situations of reversible pulpitis with deep carious lesion or normal pulp (Carrotte 2004).
3.2.2 Endo/Perio Lesions
Oftentimes, there is a close connection between the periodontal tissues and the pulpal tissues, whether through the apical opening or through lateral canals. Pulpal disease could cause periradicular lesions that take the same appearance as lesions of periodontal disease, at least radiographically. Accurate analysis of the combined information regarding the status of the pulp, the periradicular lesion, and the presence/absence of infraction or vertical root fractures will help the clinician to obtain the proper diagnosis and determine whether the problem is of an endodontic origin, a periodontal origin, or a real combination of both.
The pulp can be tested to determine its status. However, even necrotic pulps may have pain receptors that can be stimulated and lead to a false-positive response (Dummer et al. 1980). Sometimes, when using vitality tests, the presence of adjacent metal-based restorations might lead to a false diagnosis (Stock 1995). In most cases, if the testing indicates a pulp disease, a conventional root canal treatment can help in the healing of the periradicular lesions. It is uncommon for periodontal disease to be limited to a single tooth, and, generally, pockets are wider when of periodontal origin.
Other origins for periradicular lesions are developmental malformations, failing root canal treatments, and poor coronal restorations that provide a pathway for bacterial contamination (Ray and Trope 1985; Saunders and Saunders 1990, 1994). Root perforations as a result of extensive caries lesions, or resorption, or iatrogenic reasons during instrumentation of canal can also be responsible for a combined endodontic-periodontal problem (Seltzer et al. 1970).
3.2.3 Resorption
The dental pulp is an integral part of the rest of the body, and when there is disruption/rupture of the neurovascular supply in an otherwise normal pulp, ingress of bacteria could occur and pulpal necrosis could result (Andreasen and Kahler 2015), that is, of course, besides the potential injury to the periodontium and surrounding bone. Compromise of the neurovascular supply and trauma to the periodontal ligament may lead to resorptive processes that could sometimes be stopped provided the appropriate treatment is performed (Fig. 3.1). By completing a root canal therapy (Heithersay 1999) or performing a decoronation (Malmgren et al. 2006), the clinician could salvage a tooth prior to the resorption process breaking down a significant amount of tooth structure. The clinician must keep in mind that resorption could be trauma induced or idiopathic (Rivera and Walton 1994) and could also be in conjunction with a root fracture. It is important to assess the type of resorption as some do require root canal treatment and some do not. An evaluation by the endodontist might be of order.
(a) A patient presented to the clinic complaining of an unusual “bump on her gum”. Intraoral examination revealed localized swelling on the labial mucosa, buccal of left maxillary central incisor. Probing around the tooth was within normal limits and the patient was asymptomatic. Percussion was inconclusive on all anterior teeth. The patient could recall a history of dental trauma a year prior to the examination. This periapical radiograph of the left maxillary central incisor shows a periapical radiolucency with what seems to be a communicating internal-external inflammatory resorption. The tooth tested non-vital to pulpal testing. (b) Endodontic treatment was initiated and an attempt to induce calcification by using calcium hydroxide alone was made. (c) Root canal therapy was completed and adjunct surgical procedure was performed to apply ProRoot MTA (Dentsply Tulsa Dental Specialties) on the buccal aspect of the root, where the resorption communicated with the periodontal ligament space. A fiber post was bonded into the root canal and a provisional crown was fabricated
3.2.4 Periodontal Considerations
There are many factors to be evaluated when assessing the periodontal condition. The age of the patient, the initial bone loss, the probing depths, the clinical attachment loss, the mobility, the root form, the furcation involvement, and whether or not the patient is a smoker are to be considered when determining the prognosis of a tooth. In a retrospective study of 102 patients (816 molars) undergoing regular periodontal therapy, Miller et al. assigned scores to all teeth on the basis of periodontal prognostic factors. They determined that of all the factors evaluated, smoking had the most negative impact (246 % greater chance of losing their teeth), far exceeding the impact of pocket depth, mobility, or furcation involvement. The authors also mentioned that 78.3 % of the molars treated were never extracted and survived for an average of 24.2 years, which indicates that under preventive maintenance therapy, periodontal health can be maintained (Miller et al. 2014). One limitation of the study resides in the fact that the severity of the furcation involvement was not assessed; only its presence or absence was considered. However, it is understood by dental health professionals that the more severe the furcation involvement, the more difficult it is for the patient to maintain proper dental hygiene. The same could be said about pocket depths in excess of 3 mm. Surgical periodontal therapy could be indicated to reduce the pocket depth and increase the likelihood of dental hygiene to be effective.
Another prospective study on 100 treated periodontal patients under maintenance care (2509 teeth) was carried over a period of 16 years in an attempt to determine the effectiveness of commonly taught clinical parameters utilized in the assignment of prognosis to accurately predict tooth survival. The study concluded that initial probing depth, initial furcation involvement, initial mobility, initial crown-to-root ratio and parafunctional habit with no biteguard were all associated with tooth loss (McGuire and Nunn 1996). Teeth that were used as abutment for fixed partial dentures (FPDs) were lost at a lower rate than those who served the same function for removable partial dentures (RPDs). Interestingly, the authors suggested that the reasons that FPDs may have greater survival rate might be related to the initial choice of the tooth as an abutment, as only very healthy teeth would be used for a fixed abutment.
Multiple authors have reported that periodontal reasons are the most common cause for extraction of endodontically treated teeth with 59.4 % and 42.6 % of all extracted teeth (Fonzar et al. 2009). In esthetically challenging situations, with the presence of apical periodontitis, or when retreatment is needed, extraction of the tooth followed by implant placement has been recommended (Setzer and Kim 2014). However, as discussed above, if proper periodontal treatment is rendered, even on teeth with moderate vertical bone loss or furcation involvement, the prognosis could be good (Setzer and Kim 2014).
Any tooth is just as strong as its weakest link. If its foundation is compromised, its entire outcome also is. Besides a dental emergency, periodontal health has to be achieved and maintained before any treatment is to be initiated. As we will discuss later, when it comes to mechanical forces, a tooth is subjected to stresses that come from all directions. The weaker the support it has from its periodontium, the more likely the horizontal stresses on the entire system are to increase and the more strain the restoration and the periodontium have to absorb. Distribution of stress being a cornerstone concept in prosthodontics, the clinician must consider, when dealing with a less than ideal, yet healthy, periodontium to lighten the occlusion in eccentric movements. For example, when restoring a canine with a compromised, yet acceptable, crown-to-root ratio, the clinician should consider a group function rather than a canine guidance.
3.3 Tooth Restorability
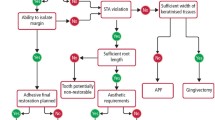
For a comprehensive treatment plan to be formulated and before using the treatment planning flowchart in Fig. 3.2, a complete evaluation of the mouth along with that of the particular tooth in question is necessary. The clinician must evaluate the overall periodontal support, the occlusal scheme, and the presence or absence of parafunction. With regard to the occlusal plane in a comprehensive treatment plan, a tooth that has extruded and is not in harmony with the occlusal plane might not allow enough vertical space for an antagonist. For this tooth to be restored, the plan might involve the possibilities of orthodontic intrusion or crown lengthening with or without root canal therapy (see Fig. 3.3). Also, when it comes to the tooth in question, one must evaluate the quality of the root canal treatment. The latter is still a major cause of failure, as reviewed in Chap. 1.
This photograph shows the right mandibular second molar (mirror image) that has supra-erupted into the opposing edentulous space. Several years after its extraction, this patient is considering replacing his maxillary missing right maxillary first molar. An interdisciplinary approach, possibly involving orthodontic movement and/or crown lengthening and/or endodontic therapy, has to be considered to bring this tooth into the normal occlusal plane
A tooth serving as an abutment for an FPD or an RPD is subject to different stresses than if it were to support a single restoration. Lastly, if the possibility of crown lengthening is considered, the clinician must keep in mind some considerations for the crown-to-root ratio, the taper of the root, and the location of any furcation.
3.3.1 Evaluation of the Remaining Tooth Structure
Some clinical conditions (e.g., a vertical root fracture or an infraction that extends far apically into the periodontium) could justify the extraction of the affected tooth, particularly if the patient is not keen on the clinician performing an explorative surgery to determine its restorability. Other, less dramatic scenarios require the removal of carious dentin and/or defective restorations in order to properly assess the overall condition of the tooth (Fig. 3.4). It is following this step that we would determine if the margin placement of the intended prosthesis is violating biologic principles (see the concept of biological width in Chap. 1, Fig. 1.2) and if the remaining sound tooth structure is sufficient in order to provide a strong support that will confer the restoration longevity and function. It is also at this stage that we assess the crown-to-root ratio and the occlusal forces the tooth is subject to in the dentition and determine the necessity of crown lengthening (Fig. 3.2).
Several of these teeth would be deemed unrestorable even without removing the carious dentin and defective restorations. If crown lengthening is performed to obtain adequate ferrule on sound tooth structure, with or without endodontic therapy, the crown-to-root ratio becomes compromised. Considering the taper of the roots, the tooth preparation for any type of complete-coverage crown might result in very thin residual dentin walls
3.3.2 Ferrule
Following excavation of carious dentin and removal of defective restorations, it is essential that sound tooth structure remains circumferentially to produce a cervical ferrule. Please refer to Chap. 1 for more detailed explanation about the ferrule concept.
If the condition of the tooth is such that even adjunct surgical and/or orthodontic procedures cannot provide a 2 mm-high ferrule, without compromising significantly the prognosis of the tooth, extraction might be the solution (Fig. 3.4). When extensive tooth structure is lost after carious dentin or a faulty restoration are removed, or following trauma or endodontic access, but that the ferrule is at least 2 mm high and 1 mm thick, the clinician must consider the fabrication of a foundation prior to tooth preparation for complete-coverage restoration. In some cases, the tooth breakdown is so extensive that it could be in proximity to the pulp. These scenarios might necessitate an elective root canal treatment and the buildup of a core. The latter will increase the retention and resistance form of the future restoration.
According to Hempton and Dominici (2010), most of the retention and resistance to dislodgment of the restoration occurs at the apical third of the preparation. Therefore, the positioning of the margin remains of crucial importance. The clinician must avoid placing the margin if it is to be seated partially or completely on the core buildup. This precaution must be taken in order to avoid the stresses from occlusion to be transmitted to the foundation restoration or, in the case of a post and core, to the internal aspect of the post and the root. That interface is usually filled with cement, and, under occlusal stress, the fatigue of the cement could lead to dislodgment of the post and core or to the fracture of the tooth. In an in vitro study, Pilo et al. (2008) suggested that having a minimum thickness and length of ferrule is very important to prevent fractures. They explained that, in case fractures occur, they do so in the tooth structure, not in core material. Also, the potential of the teeth to fracture is directly related to the amount of dentin removed.
3.3.3 Dentin and Enamel Integrity
Worthy of mention, careful attention must be taken when instrumenting the canal during endodontic therapy as well as when preparing a post space. Over-instrumentation will contribute to over-enlargement of the root canal and unnecessary dentin removal. It is well accepted that a minimum of 1 mm of dentinal thickness wall is necessary to prevent its fracture and properly support the core foundation, if any is planned (Ouzounian and Schilder 1991).
As it was discussed in the previous chapter, mechanical properties of endodontically treated teeth could confer the dentin of the tooth different mechanical properties. However, it has been suggested that the type of cavity preparation could play an even more significant impact on cuspal deflection (separation of the cusps). In one study, it has been determined that intact mandibular molars had a cuspal deflection of up to 1.0 μm. As for MO cavity preparations, the deflection was noted to less than 2 μm of movement. MOD preparations showed a movement of 3–5 μm. Endodontic access preparations were responsible for a movement of 7.0–8.0 μm for the MO group and 12.0–17.0 μm for the MOD group (Panitvisai and Messer 1995). It has been advocated that maintaining the continuity of enamel maintains the tooth rigidity; henceforth, consideration should be given to some sort of cuspal protection, particularly when there is an increase of twofold or threefold from the MO to the MOD group with endodontic access preparation.
It seems that the mechanical properties of the endodontically treated tooth’s dentin might not be as critical as the initial appearance of the tooth that lead to the endodontic treatment. The integrity of the enamel seems to play a more important role than whether or not it has been treated endodontically. In the next section, we will have a closer look at the literature when it comes to the impact of such results on the overall outcome of the tooth.
Let us go back to the treatment planning flowchart (Fig. 3.2). After determining the stress that will be applied to that tooth, we need to answer two questions: (1) Is there enough remaining sound tooth structure to retain a core? and (2) Is the remaining tooth structure strong enough to resist crown fracture at the neck of the tooth? If the answer to both these questions is “no,” then a cast dowel and core or a prefabricated post and core buildup are to be considered. If the answer to both questions is “yes,” then a (composite resin or amalgam) core restoration buildup should be considered (Figs. 3.2 and 3.5).
(a) After removal of the carious dentin and defective margins, the remaining tooth structure on the maxillary right second premolar is insufficient to retain a core and is not strong enough to resist crown fracture at the neck of the tooth. As for the maxillary right first molar, it has fewer than three walls left and would need a post to retain a core. On the other hand, the maxillary right second molar has sufficient walls left to retain a core and resist crown fracture at its neck. (b) A cast dowel and core was placed on the maxillary right second premolar, a prefabricated metal post was inserted into the palatal root of the maxillary right first molar, and an amalgam core was built. As for the maxillary right second molar, an amalgam core was used to rebuild the missing tooth structure
In a randomized clinical trial on 360 premolars followed up for 3 years, Cagidiaco et al. (2008) divided the teeth in six groups of 60 premolars based on the amount of the dentin left at the coronal level after endodontic treatment and before abutment buildup. They then randomly assigned them into subgroups with or without fiber posts. They determined that a (fiber) post might not be needed in four coronal walls situation but that as soon as we lost one wall, we started seeing failures in the groups with no post. In the post group, failures increased in the group with one coronal wall and the groups with no wall with or without a 2 mm ferrule. Two studies by Ferrari et al. (2007, 2012) also confirmed that the placement of a fiber post reduced significantly the failures on endodontically treated premolars. The preservation of one coronal wall significantly reduced the failure risk.
In situations of three or four coronal walls remaining, one must choose between different core materials. In a fatigue study, Kovarik et al. (1992) tested glass ionomer cement (GIC), composite resin, and amalgam as a core material under crowns. It took 20,000 cycles to bring all GIC core crowns to failure. At 50,000 cycles, 80 % of composite core crowns experienced failures. As for amalgam core crowns, 30 % experienced failures at 70,000 cycles. Gateau et al. (2001) reported that two GIC-based materials used as core materials showed a higher number of defects than amalgam, suggesting that fatigue resistance of GIC-based materials may be inadequate for post and core applications. Some clinicians have used silver-reinforced GIC-based materials (known as cermets) for core buildups. As stated by Combe et al. (1999), cermet GIC materials are one of the weakest materials in terms of tensile, flexure, and modulus values, despite being similar to some resin materials in terms of compressive strength. Cermet GIC materials are not suitable for core buildup procedures in the posterior teeth.
3.4 Prognosis of Endodontically Treated Teeth
Restorative considerations put aside, endodontic therapy has been demonstrated to be a predictable procedure provided that the quality of the canal disinfection and that of the root canal obturation are good. In the absence of preoperative apical periodontitis, primary root canal therapy has shown success rates above 90 % (Marquis et al. 2006). However, when preoperative apical periodontitis was present, this number dropped to approximately 80 % (Sjogren et al. 1990; de Chevigny et al. 2008).
In their systematic review, Gillen et al. (2011) suggest that all aspect of the treatment, from the periodontal condition to the root canal therapy to the restoration, have an impact on the overall outcome. When coronal restorations are inadequate, the odds of maintaining the healed status of an apical periodontitis decrease as microbes ingress through the defective margins of the restorations.
3.4.1 Survival Rate of the Endodontically Treated Anterior Teeth
There is a belief that endodontically treated anterior teeth without crowns are not susceptible to as much fracture as posterior ones. However, a recent study on 1.4 million teeth (Salehrabi and Rotstein 2004).demonstrated that 83 % of teeth that were extracted had not received a crown, while 9.7 % of the extracted teeth had a crown and a post and 7.3 % of the extracted teeth had a crown without post. The result of this 2004 large-scale study contrasts the findings reported by Sorensen and Martinoff in 1984, where it was suggested that endodontically treated anterior teeth do not have a significantly better prognosis if they are crowned, compared if there were not (Sorensen and Martinoff 1984). Please refer to Chap. 6 for more evidence about the positive impact of fiber posts on endodontically treated anterior teeth.
3.4.2 Survival Rate of the Endodontically Treated Posterior Teeth
When endodontically treated posterior teeth are not restored with a crown, they are more likely to fracture than vital teeth (Aquilino and Caplan 2002). In another study, it was demonstrated that teeth without crowns failed after an average period of 50 months, while pulpless teeth restored with a full coverage restoration were lost after an average of 87 months following the placement of the restoration (Vire 1991). In a retrospective cohort study, it was demonstrated that endodontically treated molars that were intact, except for the endodontic access opening, were successfully restored using composite resin restorations. It is interesting to know that composite resin restorations had better clinical performance than dental amalgam restorations. On a 2-year basis, the survival of molars restored with composite resin restorations was 90 % vs. 77 % for amalgam restorations. At 5 years, the survival declined significantly for both restorative materials, to 38 % for composite resin and 17 % for dental amalgam restorations (Nagasiri and Chitmongkolsuk 2005). Similarly, a 3-year investigation found comparable success rates between endodontically treated premolars restored with only a post and direct class II composite resin and premolars restored with complete-coverage crowns (Mannocci et al. 2002).
Amalgam may be used provided all cusps adjacent to teeth with missing marginal ridges are covered and sufficient thickness of amalgam is present, as seen in Chap. 1. It has been recommended that a thickness of 4.0 mm of amalgam protects the functional cusp and 3.0 mm over the nonfunctional cusp (Liberman et al. 1987).
Once we have determined the restorability of the tooth as a unit, it is important to assess the stress that will be applied to that tooth. As we will discuss in the next section, there is scientific evidence that suggests that an endodontically treated tooth’s position in the arch as well as its future function has an impact on its survival rate. Also Chap. 6 covers the impact of placing fiber posts on the longevity and prognosis of posterior endodontically treated teeth.
3.4.3 The Importance of Proximal Contacts
It has been determined that the presence of two proximal contacts had a significant positive impact on the survival rates of endodontically treated teeth (Aquilino and Caplan 2002; Caplan et al. 2002). Caplan et al. (2002) performed a retrospective study in which they reviewed charts and radiographs of 400 teeth from 280 patients. They suggested that endodontically treated teeth with less than two proximal contacts underperform the ones with two proximal contacts. To reinforce that point, a meta-analysis of 14 clinical studies also pointed out that observation. In descending order of influence, the conditions increasing the survival rate of endodontically treated teeth were as follows: (1) a crown restoration after RCT, (2) tooth having both mesial and distal proximal contacts, (3) tooth not functioning as an abutment for removable or fixed prosthesis, and (4) tooth type or specifically non-molar teeth (Balto 2011).
Another 4-year prospective study involving 759 primary root canal-treated teeth and 858 endodontically retreated teeth demonstrated that teeth with two proximal contacts had a 50 % lower risk of being lost than those with less than two proximal contacts. It was demonstrated that terminal teeth were associated with almost 96 % more tooth loss than those that were not located distal most in the arch (Ng et al. 2011). In a 10-year follow-up study, Aquilino and Caplan demonstrated that second molars had a significantly lower survival rate than any other type of teeth. The greater than fivefold decrease in the endodontically treated second molar’s survival rate could be explained by the result of increased occlusal stresses and difficult endodontic treatment due to a compromised access and restricted visibility (Aquilino and Caplan 2002).
It is well documented that the position of the endodontically treated tooth in the arch and the presence or absence of proximal contact have a significant impact on its survival rate. This could be explained by the unfavorable distribution of occlusal forces and higher non-axial stress on these teeth. Also, regardless of the chewing forces of the patient, an endodontically treated tooth is better off, in terms of stress, to oppose an acrylic tooth from a complete conventional denture than it is to oppose a single implant crown. It has more to do resiliency of the opposing prosthesis than it is about the material.
3.4.4 FPDs and RPDs
Multiple clinical studies have suggested that FPDs supported by endodontically treated abutment teeth fail more often than those supported by vital abutment teeth (Reuter and Brose 1984; Karlsson 1986; Palmqvist and Swartz 1993; Sundh and Odman 1997). Over 20 years ago, Sorensen and Martinoff (1985) reviewed over 6000 patients’ records, and based on 1273 teeth endodontically treated that served as an abutment for either an FPD or an RPD, they concluded that abutments for FPDs and RPDs that were endodontically treated had significantly higher failure rates than single crowns. Respectively, the success rate of all endodontically treated RPD abutments was 77.4 % compared with FPDs, which was 89.2 %. Interestingly, they also found that post placement was associated with significantly decreased success rate for single crown, produced no significant change for FPD abutments, and significantly improved the success of RPD abutment teeth. The nature of the study being retrospective, variables that were not recorded and may have affected that function of the RPD, and stresses on the endodontically treated teeth include the rest and retainer design, the quality of the adaptation of the extension bases, and the occlusion. Also, the span of the distal extension was not recorded, and no distinction was made between a tooth-borne and a distal extension RPD.
A more recent clinical study compared FPDs and single crowns for up to 20 years. The authors reported that the survival rate of three-unit FPDs with at least one endodontically treated abutment was comparable to FPDs on vital teeth. More failures were associated with FPDs with cantilevered units and those with more than three units (De Backer et al. 2007). Once again, when considering an endodontically treated tooth as an abutment for a prosthesis, one must accord crucial importance on the antagonist prosthesis, if any, on the periodontal condition and bony support, as well as the amount of stress bearing the abutment will be subject to. The clinician’s judgment plays an important role when, for example, he/she is confronted to a situation where a three-unit posterior FPD is retained by two endodontically treated abutments opposing a stable complete conventional denture and another situation where a nonterminal single endodontically treated and crowned posterior tooth is opposing an implant crown. The literature does not have any answer for which of the two scenarios is more favorable on the endodontically treated tooth.
3.5 Adjunct Surgical Procedures
3.5.1 Biologic Width
When carious dentin, cavitation, or existing restorations are extensive and in proximity with the root and that crown lengthening is planned, the biologic width (Fig. 1.2, Chap. 1) has to be considered. If it is violated, it may induce chronic inflammation (Gunay et al. 2000) and even lead to periodontal breakdown (Cunliffe and Grey 2008). Gargiulo et al. (1961) published one of the first studies on the issue of the dimensions of the biologic width. They averaged the length of the dentogingival junction to be 2.04 mm, the epithelial attachment to be of a mean value of 0.97 mm, and the connective tissue attachment to be of a mean value of 1.07 mm.
When it comes to restoration margin placement, some authors have advocated the importance of maintaining a 3 mm biologic distance coronal to the osseous crest and the plaque-associated margins (Nevins and Skurow 1984). Another retrospective study indicated that 40 % of the molars developed a furcation lesion at 5 years after the crown placement if their initial margin-to-bone distance is less than 4 mm (Dibart et al. 2003).
Although it seems to be widely accepted that a minimum of 3 mm from the osseous crest to the restoration margin significantly reduced the risk of periodontal attachment loss, the clinician must always keep in mind that every patient’s dental anatomy is slightly different. Vacek et al. (1994) tested a hypothesis similar to that of Gargiulo et al.’s previous study and published a range of biologic width (Table 3.1). Adequate probing and proper diagnostic radiographs are invaluable.
When in doubt, it is typically because we are about to violate the biologic width. However, if one wishes so, a long-term provisional restoration could be a good method to test the response of the epithelial attachment prior to deciding on crown lengthening. Careful attention must be taken to have tight margins and a well-polished provisional restoration to prevent marginal leakage and/or accumulation of inflammation-inducing plaque.
3.5.2 Crown Lengthening
When the tooth presents with little structure to allow for retention and resistance on sound dentin, the clinician might need to “create” additional sound tooth structure by reverting to surgical procedure. The crown lengthening surgical procedure might need to be combined with orthodontic forced eruption (Fig. 3.6). We will not be discussing the details of orthodontic forced eruption in this chapter. The reader who is interested will find a great deal of information on the subject in other dental literature. The addition of sound tooth structure to be embraced by the future restoration allows for the occlusal forces to be distributed into the periodontium rather than on the post-core-tooth interface. However, one must keep in mind the crown-to-root ratio as the mobility of the tooth could increase and accentuate the amount of horizontal components to the occlusal stress. The inertia of the periodontal membrane to an axial load has been calculated as being 17 times as great as it is to a transverse load (Thayer 1980). Al-Hazaimeh and Gutteridge (2001) tested in vitro the effect of a ferrule preparation on the fracture resistance of ten post crowned natural central incisor teeth with a 2 mm ferrule preparation and compared it to his control group of ten without ferrule. The author suggested more attention be given to the post length than the presence of a ferrule.
In this clinical presentation, the inflammation of the gingival tissue is evident. The retainer’s margin of this FPD (9-X-11) has clearly violated the epithelial attachment. The clinician must keep in mind the gingival margin level of the contiguous teeth if crown lengthening is to be performed. Forced orthodontic extrusion, combined with crown lengthening, could be considered
The need for the future restoration to embrace sound tooth structure circumferentially in order to increase its resistance to fracture cannot solely justify the creation of a ferrule through surgical procedure. Along with the overall treatment plan, other considerations have to be taken into account during treatment planning.
In order to remain favorable, the crown-to-root ratio must remain at a maximum of 1:1. Considering that the reduced periodontium is still subjected to the same amount of load, increased mobility could result from poor planning. Also, when roots are in near proximity, it becomes difficult to remove the interdental bone without damaging the roots. This will also result in a limited crown exposure since the soft tissue cannot be repositioned apically.
The clinician must keep in mind that the further apically the preparation of the tooth, the thinner the dentinal wall is and more likely the chances of pulp exposure or of over-contouring of the restorations due to insufficient restorative space laterally. The clinician must be diligent in choosing the appropriate finish line, particularly in the lower anterior teeth (Borelli et al. 2015).
In order to maintain periodontal health and prevent the creation of a mucogingival defect, it is important that the amount of attached gingiva remains at least 2–3 mm (Fig. 3.7) (Maynard and Wilson 1979).
Finally, the clinician must keep in mind the entire dentition and the overall treatment plan. In an esthetically driven patient, or with patient with a high smile line, the patient’s lip position could reveal a disharmony between the gingival levels and affect the esthetic outcome. In cases of passive eruption in the anterior region, the short clinical crowns sometimes accompanied by a high smile line could result in excessive gingival display. If the patient is concerned about having teeth with better proportions in the anterior sextant, surgical crown lengthening exposing more anatomical crown might be warranted (Allen 1993; McGuire 1998). In these scenarios, a diagnostic wax-up must be completed in order to provide the surgeon with a surgical stent to properly determine the position of the new restorations. Functional and esthetic crown lengthening can be combined when subgingival caries do not extend apically into the root. Also particular care must be taken due to the possible loss of the interproximal papillae. One must determine whether there is a need for resective surgery of the interdental bone or whether it should be limited to the labial aspect. In the advent that the gingival embrasures are widened, resulting in an unpleasant display, the restorative dentist might need to better contour the restorations or widen their contact area. Black triangles can develop where the distance between the interdental osseous crest and the contact point is greater than 5 mm (Tarnow et al. 1992) (Fig. 3.8).
(a) The provisional crowns on the maxillary right lateral incisor, the maxillary right central incisor (implant), the maxillary left central incisor, and the maxillary left lateral incisor were left in the mouth for approximately 6 months to allow for the papillae to creep into the gingival embrasures. (b) Ultimately, crown lengthening only on the labial aspect of the maxillary left central incisor and proper contouring of the permanent restorations created an esthetically pleasing result (Courtesy of Dr. Remi Elkattah and master ceramist Aram Torosian)
3.6 Treatment Options for Missing Teeth
When one or several teeth are deemed unrestorable or have poor prognosis, extraction is often the outcome. The patient has to be informed of the diagnosis and the rationale prior to discussing replacement options.
3.6.1 FPDs
For many years, FPDs have been considered the gold standard. They are relatively quick to fabricate and provide a reasonable and a somehow predictable result. Undeniably, their downfall is the preparation of the adjacent teeth and their difficulty to clean. It is more likely the noncompliance of the patient to perform oral hygiene under the pontic than their difficulty to clean that affects their survival rate and increases the risk of decay around the margins of the restoration. Although some cases of bone deposition under pontics have been reported, the lack of stimulation of the alveolar bone by the periodontal ligament under pontics most often results in bone loss and the need of the restorative dentist and the dental technician to fabricate bigger than normal pontic height or to mask the defect with pink porcelain.
Several authors have written on the longevity of FPDs. Salinas et al. (2004) have reported a 69 % survival rate at 15 years. Others have suggested a 50–69 % survival rate at 20 years (Budtz-Jorgensen 1996). The survival of adjacent teeth at 10 years has been reported at 92 % (Aquilino et al. 2001). A proper solution is only one that complies with evidence-based dentistry and meets the patient’s expectations. Henceforth, the patient is presented with other treatment modalities to replace an edentulous area.
3.6.2 RPDs
An RPD is a relatively inexpensive tooth replacement alternative and has the potential to replace areas where the soft tissue is deficient in volume. Unfortunately, patients sometimes report the sensation of having a “mouthful.” Also, depending on the clinical situation, removable partial dentures could represent significant torque/stress on adjacent teeth, and being partially supported by the underlying tissue, bone loss is to be expected under the load-bearing areas. The longevity of this type of prosthesis at 10 years has been reported at 50 % (Budtz-Jorgensen 1996). Aquilino et al. (2001) reported a 56 % survival rate at 10 years for the teeth adjacent to the edentulous areas.
3.6.3 Endosseous Dental Implant
Taking over FPDs as the gold standard for replacing edentulous areas, dental implant restorations help maintain bone in edentulous spaces by stimulating the bone. Although this alternative often requires a longer treatment time, involves surgical procedures, and represents an initial increased cost, the adjacent teeth remain more often than none untouched and the long-term financial investment is considerably reduced. Although dental caries are not a concern for implant restorations, new concepts of peri-implant mucositis and peri-implantitis have surfaced with the advent of implants. Wilson has reported cases of cement-induced peri-implantitis manifesting as long as 9 years after the insertion of the final cement-retained prosthesis (Wilson 2009). On the other hand, several studies have demonstrated endosseous dental implant survival rate of above 95 % on 15–20 years (Budtz-Jorgensen 1996; Salinas et al. 2004).
From a prosthetic point of view, the presence or absence of the periodontal ligament makes a significant difference in tactile sensitivity between implants and natural teeth. The mean values of an axial displacement of teeth are approximately 25–100 μm, compared with a dental implant of 3–5 μm (Schulte 1995; Kim et al. 2005). The dental implant restoration and its components are therefore subject to more stress, and the periodical evaluation of the occlusion is of utmost importance to prevent fracture or chipping of the ceramic or technical/mechanical complications of the implant restoration system. In a 10-year retrospective study assessing the rate of mechanical/technical complications and failures with implant-supported fixed dental prosthesis and single crowns, Wittneben et al. (2014) demonstrated that out of 397 fixed implant reconstructions, ceramic chipping was the most frequent complication (20.31 %) followed by occlusal screw loosening (2.57 %) and the loss of retention (2.06 %).
Dental implants could play a role in preserving remaining teeth; Priest has reported a 99.5 % survival rate of the adjacent teeth on a 10-year period (Priest 1999).
Finally, if it is the patient’s wish to do so, an edentulous space could remain so. Inevitably, this could lead to bone loss in the edentulous area and affects the survival of the adjacent teeth (Aquilino et al. 2001).
3.7 Summary
In a very concise way, here is the thought process leading to the treatment planning:
The clinician must perform a complete evaluation of the whole mouth, in tandem with the particular tooth in question, so that a clear and comprehensive treatment plan can be formulated.
-
1.
How are the current condition and the prognosis of the tooth?
-
(a)
Periodontal support
-
(b)
Quality of root canal treatment
-
(a)
-
2.
How much of sound tooth structure will remain after?
-
(a)
Caries removal
-
(b)
Root canal treatment
-
(c)
Crown preparation
-
(a)
-
3.
How much of stress will be applied to that tooth?
-
(a)
Serving as a single crown vs. abutment of FPD/RPD
-
(b)
Enduring eccentric guidance
-
(c)
Occlusal force (anterior vs. posterior tooth), bruxism/clenching
-
(a)
-
4.
After knowing the structure and stress issues, ask the following questions, while considering how much vertical space exists for core buildup.
-
(a)
Is the remaining sound tooth structure sufficient to provide a strong support to the restoration? (sub-question: Will post improve the retention of the core?)
-
(b)
Is the remaining tooth structure strong enough to resist crown/core fracture at the neck of the tooth? (sub-questions: Pocket depth? Is crown lengthening possible and worth it? Will bonded post strengthen the system?)
-
(a)
If the answers of the two questions are:
-
YES, the options are:
-
1.
Amalgam or composite core restoration (four, three, two remaining walls) (sub-question: Will composite core bonding against amalgam lower the chance for cusps split?)
-
2.
Prefabricated post (three, two remaining walls) + core buildup (sub-questions: If vital, is elective endodontic treatment worth it? Even with enough tooth walls, will addition of fiber post improve prognosis of the tooth?)
-
3.
Prefabricated post, if maxillary anterior teeth had an endodontic treatment and crown is indicated
-
1.
-
NO, the options are:
-
1.
Prefabricated post (three, two, one wall) + core buildup (sub-question: If vital, is elective endodontic treatment worth it?).
-
2.
Cast dowel and core (one wall or ferrule only or compromised ferrule) (sub-question: If vital, is elective endodontic treatment worth it?).
-
3.
Crown lengthening + cast dowel and core (sub-question: If vital, is elective endodontic treatment worth it on top of crown lengthening?).
-
4.
Extract and replace tooth with implant or FPD.
-
5.
Finally, consider overall treatment plan of full dentition, the longevity of treatment, other options that might be available (implant, FPD, RPD), cost effectiveness, what patient wants, etc.
-
1.
References
Al-Hazaimah H, Gutteridge DL (2001) An in vitro study into the effect of the ferrule preparation on the fracture resistance of crowned teeth incorporating prefabricated post and composite core restoration. Int Endod J 34:40–46
Allen EP (1993) Surgical crown lengthening for function and esthetics. Dent Clin North Am 37:163–179
Andreasen FM, Kahler B (2015) Pulpal response after acute dental injury in the permanent dentition: clinical implication – a review. J Endod 41:299–308
Aquilino S, Caplan D (2002) Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 87:256–263
Aquilino SA, Shugars DA, Bader JD, White BA (2001) Ten-year survival rates of teeth adjacent to treated and untreated posterior bounded edentulous spaces. J Prosthet Dent 85:455–460
Balto K (2011) Tooth survival after root canal treatment. Evid Based Dent 12:10–11
Borelli B, Sorrentino R, Goracci C, Amato M, Zarone F, Ferrari M (2015) Evaluating residual dentin thickness following various mandibular anterior tooth preparations for zirconia full-coverage single crowns: an in vitro analysis. Int J Periodontics Restorative Dent 35:41–47
Budtz-Jorgensen E (1996) Restoration of the partially edentulous mouth—a comparison of overdentures, removable partial dentures, fixed dental prosthesis and implant treatment. J Dent 24:237–244
Cagidiaco MC, Garcia-Godoy F, Vichi A, Grandini S, Goracci C, Ferrari M (2008) Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am J Dent 21:179–184
Caplan DJ, Kolker J, Rivera EM, Walton RE (2002) Relationship between number of proximal contacts and survival of root canal treated teeth. Int Endod J 35:193–199
Carrotte P (2004) Endodontics: Part 2 Diagnosis and treatment planning. Br Dent J 197:231–238
Combe EC, Shaglouf AM, Watts DC, Wilson NH (1999) Mechanical properties of direct core build-up materials. Dent Mater 15:158–165
Cunliffe J, Grey N (2008) Crown lengthening surgery – indications and techniques. Dent Update 25:29–35
De Backer H, Van Maele G, Decock V, Van den Berghe L (2007) Long-term survival of complete crowns, fixed partial dentures, and cantilever fixed dental prostheses with posts and cores on root canal-treated teeth. Int J Prosthodont 20:229–234
de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, Friedman S (2008) Treatment outcome in endodontics: the Toronto study–phase 4: initial treatment. J Endod 34:258–263
Dibart S, Capri D, Kachouh I, Van Dyke T, Nun ME (2003) Crown lengthening in mandibular molars: a 5-year retrospective radiographic analysis. J Periodontol 74:815–821
Dummer PMH, Hicks R, Huws D (1980) Clinical signs and symptoms in pulp disease. Int Endod J 13:27–35
Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C (2007) Post placement affects survival of endodontically treatment premolars. J Dent Res 86:729–734
Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L, Polimeni A, Goracci C (2012) A randomized controlled trial of endodontically treated and restored premolars. J Dent Res 91:72S–78S
Fonzar F, Fonzar A, Buttolo P, Worthington HV, Esposito M (2009) The prognosis of root canal therapy: a 10-year retrospective cohort study on 411 patients with 1175 endodontically treated teeth. Eur J Oral Implantol 2:201–208
Gargiulo A, Wentz F, Orban B (1961) Dimensions and relations of the dentogingival junction in humans. J Periodontol 32:261–267
Gateau P, Sabek M, Dailey B (2001) In vitro fatigue resistance of glass ionomer cements used in post-and-core applications. J Prosthet Dent 86:149–155
Gillen BM, Looney SW, Gu LS, Loushine BA, Weller RN, Loushine RJ, Pashley DH, Tay FR (2011) Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod 37:895–902
Gunay H, Seeger A, Tschernitschek H, Geurtsen W (2000) Placement of the preparation line and periodontal health: a prospective 2-year clinical study. Int J Periodontics Restorative Dent 20:171–181
Heithersay GS (1999) Invasive cervical resorption following trauma. Aust Endod J 25:79–85
Hempton TJ, Dominici JT (2010) Contemporary crown-lengthening therapy: a review. J Am Dent Assoc 141:647–655
Karlsson S (1986) A clinical evaluation of fixed bridges, 10 years following insertion. J Oral Rehabil 13:423–432
Kim Y, Oh TJ, Misch CE, Want HL (2005) Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implant Res 16:26–35
Kovarik RE, Breeding LC, Caughman WF (1992) Fatigue life of three core materials under simulated chewing conditions. J Prosthet Dent 68:584–590
Liberman R, Judes H, Cohen E, Eli I (1987) Restoration of posterior pulpless teeth: amalgam overlay versus cast gold inlay restoration. J Prosthet Dent 57:540–543
Malmgren B, Malmgren O, Andreasen JO (2006) Alveolar bone development after decoronation of ankylosed teeth. Endod Topics 14:35–40
Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TR (2002) Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restorations. J Prosthet Dent 88:297–301
Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S (2006) Treatment outcome in endodontics –the Toronto study. Phase III: Initial treatment. J Endod 32:299–306
Maynard JG Jr, Wilson RD (1979) Physiological dimensions of the periodontium significant to the restorative dentist. J Periodontol 50:170–174
McGuire MK (1998) Periodontal plastic surgery. Dent Clin North Am 42:411–465
McGuire MK, Nunn ME (1996) Prognosis versus actual outcome. III. The effectiveness of clinical parameters in accurately predicting tooth survival. J Periodontol 67:666–674
Miller PD Jr, McEntire ML, Marlow NM, Gellin RG (2014) An evidence-based scoring index to determine the periodontal prognosis on molars. J Periodontol 85:214–225
Nagasiri R, Chitmongkolsuk S (2005) Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent 93:164–170
Nevins M, Skurow HM (1984) The intracrevicular restorative margin, the biologic width, and the maintenance of the gingival margin. Int J Periodontics Restorative Dent 4:30–49
Ng YL, Mann V, Gulabivala K (2011) A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2. Tooth survival. Int Endod J 44:610–625
Ouzounian ZS, Schilder H (1991) Remaining dentin thickness after endodontic cleaning and shaping before post space preparation. Oral Health 81:13–15
Palmqvist S, Swartz B (1993) Artificial crowns and fixed partial dentures 18 to 23 years after placement. Int J Prosthodont 6:279–285
Panitvisai P, Messer HH (1995) Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 21:57–61
Pilo R, Shapenco E, Lewinstein I (2008) Residual dentin thickness in bifurcated maxillary first premolars after root canal and post space preparation with parallel-sided drills. J Prosthet Dent 99:267–273
Priest G (1999) Single-tooth implant and their role in preserving remaining teeth: a 10-year survival study. Int J Oral Maxillofac Implants 14:181–188
Ray HA, Trope M (1985) Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 28:12–18
Reuter JE, Brose MO (1984) Failures in full crown retained dental bridges. Br Dent J 157:61–63
Rivera ME, Walton RE (1994) Extensive idiopathic apical root resorption. A case report. Oral Surg Oral Med Oral Pathol 78:673–677
Salehrabi R, Rotstein I (2004) Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod 30:846–850
Salinas TJ, Block MS, Sadan A (2004) Fixed dental prosthesis or single-tooth implant restorations? Statistical considerations for sequencing and treatment. J Oral Maxillofac Surg 62:2–16
Saunders WP, Saunders EM (1990) Assessment of leakage in the restored pulp chamber of endodontically treated multi rooted teeth. Int Endod J 23:28–33
Saunders WP, Saunders EM (1994) Coronal leakage as a cause of failure in root canal therapy: a review. Endod Dent Traumatol 10:105–108
Schulte W (1995) Implants and the periodontium. Int Dent J 45:16–26
Seltzer S, Sinai I, August D (1970) Periodontal effects of root perforations before and during endodontic procedures. J Dent Res 49:109–114
Setzer FC, Kim S (2014) Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res 93:19–26
Sjogren U, Hagglund B, Sundqvist G, Wing K (1990) Factors affecting the long-term results of endodontic treatment. J Endod 16:498–504
Sorensen JA, Martinoff JT (1984) Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent 51:780–784
Sorensen JA, Martinoff JT (1985) Endodontically treated teeth as abutments. J Prosthet Dent 53:631–636
Stock CJR (1995) Patient assessment. In: Stock CJR, Gulabivala K, Walker RT, Goodman JR (eds) Endodontics, 2nd edn. Mosby-Wolfe, London, pp 43–46
Sundh B, Odman P (1997) A study of fixed prosthodontics performed at a university clinic 18 years after insertion. Int J Prosthodont 10:513–519
Tarnow DP, Magner AW, Fletcher P (1992) The effect of the distance from the contact point to the crest of bone on the presence or absence of the inter proximal dental papilla. J Periodontol 63:995–996
Thayer H (1980) Overdentures and the periodontium. Dent Clin North Am 24:369–377
Vacek JS, Gher ME, Assad DA, Richardson AC, Giambarresi LI (1994) The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent 14:154–165
Vire DE (1991) Failure of endodontically treated teeth: classification and evaluation. J Endod 17:338–342
Wilson TG Jr (2009) The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol 80:1388–1392
Wittneben JG, Buser D, Salvi GE, Burgin W, Hicklin S, Bragger U (2014) Complication and failure rates with implant-supported fixed dental prostheses and single crowns: a 10-year retrospective study. Clin Implant Dent Relat Res 16:356–364
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Badr, F., Seong, WJ., Perdigão, J. (2016). Restoring the Endodontically Treated Tooth: Treatment Planning Considerations. In: Perdigão, J. (eds) Restoration of Root Canal-Treated Teeth. Springer, Cham. https://doi.org/10.1007/978-3-319-15401-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-15401-5_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15400-8
Online ISBN: 978-3-319-15401-5
eBook Packages: MedicineMedicine (R0)