Abstract
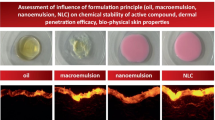
Emulsions are widely used in the cosmetic and pharmaceutical fields for the topical administration of hydrophilic and lipophilic active ingredients. There exist different types of emulsions, e.g. water-in-oil, oil-in-water, water-in-oil-in-water and oil-in-water-in-oil. Furthermore, emulsions are thermodynamically unstable and necessitate an emulsifier for the formation and stabilisation. Both, the type of emulsion and emulsifier could affect dermal and transdermal delivery, which has been reviewed in this chapter. Due to the complexity of topical emulsions and consequently the difficulty to investigate the exclusive effect of emulsifiers and emulsion type on skin absorption, as other emulsion ingredients may also contribute to interactions with the active ingredient and the skin, this chapter aimed at focusing mainly on studies with a systematic approach. For example, studies were included that investigated emulsions with the same composition and only differed in the emulsifier component or emulsion type. The review demonstrated that the type of emulsion significantly affected the dermal and transdermal delivery. In general, skin penetration of hydrophilic active ingredients was enhanced when the active was incorporated into the continuous phase of the emulsion. Furthermore, multiple o/w/o emulsions, in comparison to simple w/o emulsions, reduced the transdermal delivery of lipophilic active ingredients, whereas the dermal delivery was increased. Therefore, multiple emulsions could be useful for prolonged topical delivery. It was also demonstrated that the effect of the emulsifiers on dermal and transdermal delivery could vary, depending on the structure and physicochemical properties of the emulsifier/emulsifier system, such as the hydrophilic chain length, hydrophilic-lipophilic balance (HLB) value, emulsifier charge or solid particles vs. surfactant.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Emulsions are heterogeneous systems consisting of at least two immiscible liquid phases, in which the one liquid is dispersed as globules (dispersed phase) in the other (continuous phase). The two immiscible liquids are, in general, an oil phase and an aqueous phase. However, an emulsion can also consist of other immiscible phases, e.g. polar and nonpolar oil phases (Tadros 2009). The droplet size of macroemulsions (or conventional emulsions) is in the micrometre range and usually comprises a radius between 0.15 and 100 μm (Friberg 1990). Nanoemulsions, on the other hand, are emulsions that contain very small droplets (r <100 nm) and are also known as submicron emulsions, ultrafine emulsions or mini-emulsions (McClements 2012). However, macro- and nanoemulsions cannot be distinguished solely on the basis of the droplet size, as the physicochemical or thermodynamic properties do not clearly change when the droplet size is reduced from the micrometre to the nanometre range, and therefore no definite cut-off value for the droplet size exists. But there are other emulsion properties that can be used to differentiate between macro- and nanoemulsions. For example, nanoemulsions can become translucent or transparent and exhibit a much higher stability against creaming or sedimentation (McClements 2012).
In contrast to microemulsions, which are in a thermodynamic equilibrium and can hence form spontaneously, macro- and nanoemulsions are thermodynamically unstable and necessitate external energy for formation. Macro- and nanoemulsions are fundamentally different from microemulsions. However, there are similarities in composition, dimensions, structures and fabrication methods between micro- and nanoemulsions, e.g. both can contain droplets in a size below 100 nm and be translucent (McClements 2012). These similarities have led to confusion about the correct use of the terms in literature, and recent articles have reviewed similarities and differences between micro- and nanoemulsions in order to clarify the terminology (McClements 2012; Anton and Vandamme 2011).
This chapter focuses on macroemulsions, here referred to as emulsions, and their effect on dermal and transdermal delivery. Nano- and microemulsions as topical drug delivery systems are discussed in different chapters of this book.
2 Emulsions as Topical Delivery Systems
Emulsions are widely used in the cosmetic and pharmaceutical fields/industries for the topical administration of both hydrophilic and lipophilic active ingredients, owing to their pleasant skin sensations and their good solubilising effects on these substances (Förster and Von Rybinski 1998). The consistency of topical emulsions ranges from liquid lotions to semisolid ointments and creams (Eccleston 1997a). Since topical emulsions should be designed to feature adequate physical and chemical stability, aesthetic acceptability as well as optimal delivery characteristics, they generally are not simply two-phase formulations, but rather complex formulations (Eccleston 1997b). For example, emulsions can also contain solid particles, vesicles, liquid crystals or a third liquid (Friberg and Ma 2006). Additionally, they undergo considerable structural changes after the application onto the skin, as water and other volatile substances evaporate within a short period of time. The modified formulation structure left on the skin after evaporation of the volatile compounds is important for the topical performance of emulsions (Friberg and Ma 2006). Therefore, not only an understanding of the microstructure of the initial emulsion but also of the film that is left on the surface of the skin is important for optimisation of topical emulsions.
Despite of the complexity of emulsions, Bernardo and Saraiva (2008) presented a theoretical model for transdermal drug delivery from emulsions. The model incorporated the formulation heterogeneity and was conceived for the prediction of transdermal delivery of drugs as a function of emulsion composition. It allows the investigation of the effect of excipients on the drug activity in the two emulsion phases as well as on the drug diffusivity in the continuous phase and the influence of surfactants forming interfacial layers with different resistance on drug transfer. A simulated case study, for example, indicated that the estimated interfacial resistance by the surfactant layer may not be negligible with regard to its effect on drug delivery rates. Furthermore, the model could also be used to predict the effect of the dosing condition (e.g. applied emulsion volume) on drug absorption. Different modes of emulsion application could significantly affect drug delivery time profiles. At the same time, Grégoire et al. (2009) developed a model to predict the transport of actives into and through the skin from a cosmetic or dermatological formulation, addressing in particular simple oil-in-water emulsions. The model assumed, inter alia, that only the fraction of the active ingredient in the continuous phase of the emulsion was available for partitioning into the skin and good correlation was obtained with experimental data.
3 Emulsifiers
Since emulsions are thermodynamically unstable, emulsifiers are required for the formation and stabilisation of emulsions. Generally, an emulsifier is defined as a substance that stabilises emulsions. However, no absolute classification exists, as constituents may perform different functions, e.g. a fatty alcohol can be incorporated as an emulsifier, thickener or emollient (Eccleston 1997b).
Different types of emulsifying agents exist, e.g. ionic and nonionic surfactants, polymers and solid particles. In the absence of any emulsifiers, the emulsions tend to break down, e.g. by coalescence (fusion of droplets into larger droplets by thinning and disruption of the emulsifier layer), flocculation (aggregation of droplets without disrupting the emulsifier layer), creaming/sedimentation (gravity-induced separation) and/or Ostwald ripening (Fig. 16.1) (Tadros 2009).
Emulsifiers are required for the formation of emulsions as they form a film around the newly formed drops and consequently prevent coalescence during emulsification and storage. In addition, surfactants reduce the interfacial tension and are important for the deformation and break-up of droplets during the emulsification process (Tadros 2009). Furthermore, the properties of the interface are significant for the rate and extent of coalescence (Friberg and Ma 2006). To prevent or retard flocculation and consequently also coalescence, it is important to keep a minimum distance between the droplets to overcome the van der Waals attraction. This could be achieved, for example, by electrostatic repulsion in the presence of a surface charge (ionic surfactants or charged particles) or by steric hindrance (nonionic surfactants or polymers) (Tadros 2009). Creaming or sedimentation can be prevented or retarded by increasing the viscosity of the continuous phase, e.g. by the development of a three-dimensional network of particles or polymers (Eccleston 1997a; Aveyard et al. 2003).
Cosmetic and pharmaceutical emulsions commonly comprise of blends of emulsifiers, instead of a single emulsifying agent. Most of these mixed emulsifiers consist of ionic or nonionic surfactants, in combination with fatty amphiphiles, which may be added separately during the emulsification process, or as a pre-manufactured blend (emulsifying wax). In addition to promoting the stability of emulsions, mixed emulsifiers and emulsifying waxes have the further advantages of improving emulsification by stabilising the oil droplets during formation and by controlling the rheological properties of the emulsion (Eccleston 1997b). Another example is the simultaneous inclusion of surfactants and solid particles that could yield synergistic stabilisation of the emulsion against coalescence and creaming (Binks and Whitby 2005; Lan et al. 2007).
4 Different Types of Emulsions
Several types of emulsions can be distinguished, for instance:
-
Simple emulsions: oil-in-water (o/w) and water-in-oil (w/o)
-
Multiple emulsions: oil-in-water-in-oil (o/w/o) and water-in-oil-in-water (w/o/w)
The type of emulsion that is formed mainly depends on the property of the emulsifier, e.g. the hydrophilic-lipophilic balance (HLB) value of the surfactants. The HLB is an arbitrary scale (e.g. from 1 to 20 for nonionic surfactants), and the higher the HLB, the more hydrophilic the surfactant. According to the Bancroft rule, the phase in which the emulsifier is more soluble constitutes the continuous phase (Bancroft 1913). For example, lipophilic surfactants with a low HLB (HLB <7) tend to act as w/o emulsifiers, whilst hydrophilic surfactants with a high HLB (HLB >7) tend to form o/w emulsions. However, Harusawa et al. (1980) suggested a change to the Bancroft rule by proposing that the phase in which the surfactant forms micelles constitutes the external phase, independent of the solubility of the surfactant monomers in the oil and aqueous phases. For particle-stabilised emulsions (also known as Pickering emulsions), it was demonstrated that the wettability of the solid particles, which is determined by the contact angle, defines which type of Pickering emulsion will be formed. For example, particles with a contact angle at the oil-water interface θ ow <90° tend to form o/w emulsions, whereas particles with a contact angle θ ow >90° prefer to stabilise w/o emulsions (Fig. 16.2) (Aveyard et al. 2003).
(Upper) Position of a small spherical particle at a planar oil-water interface for a contact angle (measured through the aqueous phase) less than 90° (left), equal to 90° (centre) and greater than 90° (right). (Lower) Corresponding probable positioning of particles at a curved interface. For θ <90°, solid-stabilised o/w emulsions may form (left). For θ >90°, solid-stabilised w/o emulsions may form (right) (Reprinted from Aveyard et al. (2003), with permission from Elsevier)
5 The Effects of Emulsion Types on Dermal and Transdermal Delivery
5.1 Overview
Various studies have been performed to compare different types of emulsions (Dal Pozzo and Pastori 1996; Förster et al. 1997; Wiechers 2005). However, not only the type of emulsion was different, the formulation ingredients also varied, and their interactions with the active ingredients (e.g. solubilisation in micelles, supramolecular complex formation) may therefore have impacted on the dermal and transdermal delivery of the active ingredients (Dal Pozzo and Pastori 1996). Consequently, due to the complexity of topical emulsions, the investigation of the emulsion type effects on dermal and transdermal delivery requires a systematic approach.
A study by Lalor et al. (1995), for example, showed the effects of the incorporation of surfactants in o/w and w/o emulsions (polysorbate 60 (Tween® 60) in o/w emulsion and sorbitan sesquioleate (Arlacel® 83) in w/o emulsion) on the partitioning and permeation of three model compounds (methyl-, ethyl- and butyl-p-aminobenzoate), due to the solubilisation capabilities of the emulsifiers. It was demonstrated that the emulsifier (surfactant) and its distribution between the oil and water phase played an important role in the solubility and therefore thermodynamic activity of the permeants in the vehicle, i.e. the thermodynamic activity of the compounds in the external phase of the emulsions was found to be the driving force for permeation through the polydimethylsiloxane membranes. Polysorbate 60 (Tween® 60), the surfactant used in the o/w emulsion, was mainly available in the external aqueous phase of the emulsion, where it formed micelles and solubilised the three test permeants, methyl-, ethyl- and butyl-p-aminobenzoate, thereby reducing their thermodynamic activity and the permeability coefficient. The permeability coefficient between the o/w emulsion and its corresponding, externally isolated aqueous phase was equal, signifying the importance of the thermodynamic activity of the permeants in the external phase for promoting the permeation process. However, the solubility of the three compounds in the oil phase of the same o/w emulsion was similar to the solubility in the oil without surfactant, indicating no solubilising effect of polysorbate 60 (Tween® 60) in the oil phase of the o/w emulsion, hence resulting in similar permeability coefficients between the internal oil phase and the pure oil. Analogous results were obtained with the w/o emulsion in which the emulsifier, sorbitan sesquioleate (Arlacel® 83), was nearly entirely distributed in the oil phase of the emulsion, whereas the aqueous phase was in effect free of sorbitan sesquioleate (Arlacel® 83). This yielded no solubility increase in the internal aqueous phase and thus no reduction in permeability, when compared with water. However, the solubility of each compound increased in the oil phase, because of the formation of inverse micelles. Consequently, the permeability of the three test permeants was reduced from both the w/o emulsion and from the corresponding isolated external oil phase, when compared with the pure oil.
Several studies have been reported, involving different emulsion types with identical composition (e.g. o/w, w/o and w/o/w), hence allowing for the systematic investigation of the effect of the type of emulsion on dermal and transdermal delivery only. These study outcomes are summarised in Table 16.1.
The results in Table 16.1 demonstrate that the type of emulsion significantly influenced both skin penetration and skin permeation of the active ingredients. The effect of the type of emulsion on dermal and transdermal delivery was furthermore dependent on the dosing condition (finite non-occluded vs. infinite occluded). With finite dosing under non-occluded conditions, the physicochemical and thermodynamic properties of the formulation modified rapidly after application onto the skin, whereas at infinite dosing under occluded conditions, the thermodynamic properties did not alter significantly (Laugel et al. 1998b).
5.2 Hydrophilic Active Ingredients
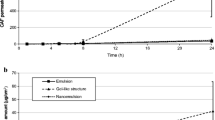
In summary, it can be concluded that the percutaneous absorption, as well as the skin penetration of hydrophilic drugs (e.g. glucose, metronidazole and lactic acid), is generally superior for o/w emulsions, compared to w/o/w and w/o emulsions (Fig. 16.3). Various suggestions were made for the differences in performance between the diverse emulsion types. For example, the higher skin uptake from o/w emulsions could have been due to a higher concentration of free hydrophilic actives in the external aqueous phase of the emulsions being directly in contact with the skin, whilst the actives were encapsulated in the internal phase of the w/o/w and w/o emulsions and as a result not readily available to the stratum corneum (Ferreira et al. 1995b; Youenang Piemi et al. 1998; Sah et al. 1998). It was hence suggested that w/o/w and w/o emulsions could be utilised for the controlled release of water-soluble actives (Sah et al. 1998). As shown by Ferreira et al. (1994, 1995b), the release of glucose and metronidazole through cellulose membranes and silicone membranes was in the following order: o/w > w/o/w > w/o. The release from the w/o/w emulsion was higher than from the w/o emulsion, due to the leakage of glucose and metronidazole into the external aqueous phase, resulting in a higher effective concentration of the hydrophilic actives in the external aqueous phase of w/o/w emulsions than in the external oil phase of w/o emulsions (Ferreira et al. 1995a, b). It should also be noted that the differences in polarity of the active ingredients further impacted on the performances of the various emulsions. So the difference between the various emulsions was more pronounced for glucose (high polarity) than for metronidazole (intermediate polarity), due to a smaller oil-water partitioning coefficient of glucose, indicating a higher concentration of glucose in the aqueous phase, when compared with metronidazole (Ferreira et al. 1995b). Furthermore, the partitioning between the oil and water phases in the emulsion was better for metronidazole, which in turn yielded a decrease in the internal release barrier and therefore a less pronounced difference in performance between the various metronidazole emulsions (Ferreira et al. 1995a).
(a) Percutaneous absorption profiles of glucose from w/o/w, o/w and w/o emulsions through hairless rat skin; typical plots of the cumulative amount of glucose as a function of time. Values are means (n = 6) (Reproduced from Ferreira et al. (1995b) with permission from Elsevier). (b) Percutaneous absorption profiles of metronidazole from w/o/w (□), o/w (▲) and w/o (○) emulsions. Values are the means (n = 5) ± SD. The SD values for the o/w emulsions are not represented for purposes of clarity (Reproduced from Ferreira et al. (1994), with permission from Elsevier)
Differences in dermal and transdermal delivery could also have occurred as a result of different partitioning coefficients between the stratum corneum and the various emulsions, e.g. a higher partitioning between the stratum corneum and external aqueous phase (for o/w and w/o/w emulsions) than between the stratum corneum and external oil phase (for w/o emulsions). In addition, the external aqueous phase may have contributed to the hydration of the stratum corneum, which in turn may have enhanced the permeability of hydrophilic compounds (Ferreira et al. 1995b). This effect could be more pronounced for an infinite, occluded dosing condition than for a finite, non-occluded dosing (Sah et al. 1998).
It is also important to consider the fate of the emulsion after application onto the skin and its effect on the delivery of the actives. Following the application onto the skin, volatile components (e.g. water) can evaporate, and therefore phase transitions, inversion, flocculation and coalescence may occur (Friberg and Langlois 1992). In addition, the drug concentration in the residual film could increase, due to water evaporation from a finite dose (Sah et al. 1998). Consequently, consideration of the evaporation of volatile components, as well as the vehicle structure of the remaining film after the evaporation of volatile components, is of importance when investigating skin penetration of actives. Ferreira et al. (1995a) investigated water evaporation from three different emulsions (o/w, w/o/w and w/o) and found that the rate thereof was higher from emulsions with an aqueous continuous phase (o/w and w/o/w) than from emulsions with an oily continuous phase (w/o) (Fig. 16.4), which may partially explain the differences in dermal and transdermal delivery. They also investigated the structure of the residual film after evaporation was completed and its effect on the lipid organisation of the stratum corneum. No differences were detected among the three emulsions (o/w, w/o/w and w/o) though. Youenang Piemi et al. (1998) reasoned in their article that the similar performances of w/o/w and w/o emulsions in the dermal and transdermal delivery of glucose could be due to a similar vehicle structure of the w/o/w and w/o emulsions after application onto the skin, because of the evaporation of the external water phase of the w/o/w emulsion.
Evaporation of water from emulsions containing (a) metronidazole and (b) glucose as a function of time. The data are expressed as percentage of water loss of the applied amount (Ferreira et al. (1995a), with permission from Elsevier)
It should be noted that most of the studies on hydrophilic compounds, as listed in Table 16.1, were performed with the same synthetic emulsifier system Hypermer™ A60 (a modified polyester)/poloxamer 407 (Synperonic™ PE/F127). However, the one study by Youenang Piemi et al. (1998) incorporated natural soybean phospholipids (lecithin, Emulmetik™ 100/300) as emulsifier in order to obtain different types of emulsions. Overall, the same trend was observed with the soybean phospholipids as with the synthetic emulsifiers. This was indicative of the importance of the nature of the continuous phase of an emulsion on the dermal and transdermal delivery of hydrophilic drugs (Youenang Piemi et al. 1998). Furthermore, the results of the various studies with hydrophilic active ingredients indicated that the type of emulsion (o/w, w/o/w, w/o) may not significantly affect the distribution of the actives between dermal and transdermal delivery, as the order of emulsions was similar for dermal and transdermal delivery (see Table 16.1).
5.3 Lipophilic Active Ingredients
As with the hydrophilic drugs, the encapsulation of the lipophilic actives (hydrocortisone and three different triterpenic derivatives) in the internal oily phase of multiple o/w/o emulsions reduced the percutaneous absorption of these lipophilic actives, compared to that of simple w/o emulsions, when applied as a finite dose. However, the uptake of the lipophilic actives into the epidermis and dermis was higher from the multiple o/w/o emulsion than from the simple w/o emulsion (Laugel et al. 1998a, b). Similarly, a release study showed that the release of hydrocortisone was slower from a multiple o/w/o emulsion than from a simple w/o emulsion, as the active needed to diffuse from the internal phase, across the aqueous phase and into the external phase (Laugel et al. 1998b). Both studies hence confirmed that multiple o/w/o emulsions could be used as prolonged, topical delivery systems for lipophilic drugs, when incorporated in the internal oily phase and applied as a finite dose. Furthermore, these multiple emulsions exhibited the advantages of reducing the transdermal delivery and therefore the systemic effects of the lipophilic drugs, whereas the dermal delivery was increased, thus showing a controlled release of the drugs to the site of action (Laugel et al. 1998b). However, it should be noted that no significant differences in transdermal delivery were observed between w/o and o/w/o emulsions, when an infinite dose of hydroquinone containing emulsions was applied onto the skin (Laugel et al. 1998b).
5.4 Stabilisation Effects of the Formulation
When investigating the dermal and transdermal delivery of active ingredients from emulsions, consideration of the stabilisation effects of a formulation on delivering degradation-sensitive active ingredients intact into and/or across the skin can prove beneficial. Schmidts et al. (2011) investigated the stabilisation effects of various emulsion systems against enzymatic degradation of topically applied oligonucleotides. They found that the enzymatic degradation of water-soluble DNAzymes, encapsulated in the inner aqueous phase of w/o/w and w/o emulsions, was significantly reduced, compared to DNAzymes, incorporated in the outer aqueous phase of a microemulsion and a submicron emulsion. The outcomes of their study suggested that w/o and w/o/w emulsions are promising formulations for effective encapsulation of DNAzymes with concurrent protection against enzymatic degradation.
6 The Effects of Various Emulsifiers on Dermal and Transdermal Delivery
6.1 Overview
As was mentioned above, various substances exist that can be utilised as emulsifiers (e.g. surfactants, polymers, solid particles), and often the stabilisation effect of emulsifiers can be attributed to more than one method. For instance, some surfactants may form a monolayer at the oil-water interface, whilst an excess thereof may also arrange in liquid crystalline structures in the aqueous phase, which could improve emulsion stability by preventing coalescence (Friberg and Solans 1986). Hydrophobically modified water-soluble polymers can stabilise o/w emulsions by adsorbing at the oil-water interface (hydrophobic part of the polymer), as well as by gelation of the aqueous continuous phase (hydrophilic part of the polymer) (Eccleston 1997a). In case of Pickering emulsions, the particles can, in addition to the adsorption at the oil-water interface, also form a three-dimensional network in the continuous phase surrounding the droplets. The resulting increased viscosity of the emulsions can reduce the rate and extent of creaming (Aveyard et al. 2003). Furthermore, the complexity of emulsions makes it more difficult to study the exclusive effect of emulsifiers on dermal and transdermal delivery, as other emulsion ingredients also contribute to interactions with the active ingredient in the vehicle, as well as with the stratum corneum. Therefore, this chapter aimed at focusing mainly on studies in which a more systematic approach to investigating the effects of emulsifiers on dermal and transdermal delivery was followed, such as using emulsions with the same oil and aqueous phases and hence reducing the influences of varying formulation ingredients on the active’s transport into and across the skin.
Montenegro et al. (2004) investigated the effects of various silicone emulsifiers using the same oil and aqueous phase ingredients for the preparation of the emulsions. The study illustrated that the type of silicone emulsifier could significantly affect the permeation of octyl methoxycinnamate (Uvinul MC 80®) across human skin, whereas the permeation of butyl methoxydibenzoylmethane (Uvinul BMBM®) was insignificantly affected. It was assumed that changes in the thermodynamic activity in the emulsion and modification of the interaction between permeant and emulsion components could account for the different effects of the emulsifiers on skin permeation. Though the inclusion of different silicone emulsifiers altered the viscosity of the emulsions and the release of the active ingredients, these factors could not be related to the modification in permeation.
Wiechers et al. (2004) suggested that the emulsifier system may influence the distribution of the active ingredient between dermal and transdermal delivery, whilst emollients may significantly affect the total skin absorption (dermal + transdermal delivery) thereof. For example, the emulsion with the emulsifier system, sorbitan stearate/sucrose cocoate (Arlatone® 2121), exhibited a higher transdermal, but lower dermal, delivery of octadecenedioic acid (Arlatone™ DIOIC DCA), in comparison with the emulsion containing steareth-2/steareth-21 (Brij® 72/721). No explanations could be given as more investigations were required to understand the influence of the emulsifier system on skin delivery.
These studies, using the same oil and aqueous phases for the emulsions, demonstrated that emulsifiers significantly affected dermal and transdermal delivery. However, the emulsifiers being compared varied in structure and physicochemical properties, making it difficult to explain their particular effects on skin penetration and permeation. The following examples focus more on studies that compare emulsifiers with particular differences (e.g. variation in hydrophilic chain length of nonionic surfactants, HLB values, emulsion droplet charge).
6.2 Effects of Hydrophilic Chain Length of Nonionic Surfactants
Oborska et al. (2004) investigated the effect of three different polyoxyethylene cetostearyl ethers of various oxyethylene chain lengths (ceteareth-12 (Eumulgin® B1), ceteareth-20 (Eumulgin® B2) and ceteareth-30 (Eumulgin® B3)) in o/w emulsions on the permeation of two flavonoids, quercetin and rutin, through a liposome model membrane. The study revealed that the permeability coefficient of both permeants decreased with increasing length of the oxyethylene chain and their effects were more pronounced for rutin, the more water-soluble flavonoid. No explanation was given. However, a similar trend was observed in a study by Dalvi and Zatz (1981), when investigating the effects of the polyoxyethylene chain length of nonionic surfactants on benzocaine flux from aqueous solutions. The reduction in benzocaine flux from non-saturated solutions with increasing polyoxyethylene chain length was explained by a higher micellar entrapment of benzocaine and therefore a lower concentration of free benzocaine giving rise to a lower driving force for permeation. Although this study was performed on aqueous solutions, the solubilisation effects of the nonionic surfactants with increasing length of the oxyethylene chain could have also occurred with quercetin and rutin in the o/w emulsions used by Oborska et al. (2004).
A study by Förster et al. (2011) tested o/w emulsions with different surfactants of the polyethylene glycol ester type, which varied in the length of the alkyl- and polyethylene glycol chains (PEG6C18:1, PEG20C12 and PEG20C18:1), for skin penetration of the lipophilic active, retinol. The results confirmed that surfactants with a short polar head group had an enhancement effect on penetration into the skin, as the penetration into the epidermis and dermis from emulsions with PEG6C18:1 was higher than from emulsions with PEG20C12 and PEG20C18:1. Confocal Raman microspectroscopy revealed that all three tested emulsions did not differ in the lateral interaction (ratio of I2880/I2850), an indicator for the lateral packing of lipids. Furthermore, the ratio I2880/I2850 for all three emulsions did not significantly differ from the ratio for untreated skin. As there was no indication of disruption of the lipid structure of the stratum corneum by any of the emulsions, the increased dermal delivery with PEG6C18:1 was linked to a change in partitioning behaviour of retinol between the skin and formulation. These results were congruent with those from studies by Oborska et al. (2004) and Dalvi and Zatz (1981), demonstrating that drug permeation was inversely related to the hydrophilic chain length of the surfactants, due to a change in solubilisation capacity of the surfactant micelles, without an apparent interaction between the surfactants and the stratum corneum lipids (Dalvi and Zatz 1981).
6.3 Effects of Emulsifier Ratios and HLB Value
As mentioned, often emulsifier combinations are used to manufacture and stabilise topical emulsions. The studies discussed next illustrate the influence that an emulsifier mixture may exhibit on dermal and transdermal delivery. These examples also include nanoemulsions, although a separate book chapter deals with nanoemulsions as skin delivery systems in more detail.
Nam et al. (2012) showed that the incorporation of a second emulsifier (Phospholipon® 90 G, mostly soybean phosphatidylcholine with max. 4.0 % lysophosphatidylcholine) with skin permeation-enhancing capabilities could increase skin absorption of the active ingredient, tocopheryl acetate. Mixtures of Phospholipon® 90 G and a polymer (poly(ethylene oxide)-block-poly(ε-caprolactone) (PEO-b-PCL)) in various ratios were used to stabilise o/w nanoemulsions being tested for their skin absorption effects. The permeation-enhancing effects of the unsaturated lipid yielded improved skin absorption of tocopheryl acetate from nanoemulsions, with increasing lipid-to-polymer ratios (Fig. 16.5). In comparison, the nanoemulsion, solely being stabilised with the polymer, PEO-b-PCL, exhibited a much lower skin penetration. It was furthermore indicated that not only the permeation-enhancing effect of the unsaturated lipid but also the smaller size of the emulsion droplets could have yielded an improved skin delivery of tocopheryl acetate.
Cumulative amount of tocopheryl acetate absorbed by the hairless guinea pig skin form nanoemulsions stabilised using a mixture of a lipid (P90G) and a polymer (PEO45-b-PCL42) as a function of the lipid-polymer ratio for 12 h (●) and 24 h (■) (Reproduced from Nam et al. (2012), with permission from Elsevier)
Another study by Cho et al. (2012) utilised a triblock copolymer (poly(ethylene oxide)-block-poly(ε-caprolactone)-block-poly(ethylene oxide) (PEO-PCL-PEO)) to co-stabilise a retinol emulsion that was primarily stabilised using polysorbate 20 (Tween® 20). Their work included an investigation of the effect of the PCL block length of the triblock copolymer on the topical delivery of retinol, and it was ascertained that the accumulation of retinol in the artificial skin was enhanced by employing the triblock copolymer, as well as by increasing the PCL block length. It was, furthermore, found that with increasing length of the PCL block, the hydrophilic-lipophilic balance (HLB) value, as well as the size of the emulsion droplets decreased. The outcomes from this study suggested that the PCL block length and HLB value are important considerations for the topical delivery of actives from emulsions being co-stabilised with a triblock copolymer.
Wu et al. (2001) found that the rate and extent of inulin permeation from water-in-oil nanoemulsions were highly dependent on the HLB values of the incorporated surfactant mixtures (different ratios of sorbitan monooleate (Span® 80) and polysorbate 80 (Tween® 80)). Surfactant mixtures with a low HLB resulted in significantly higher permeation of inulin than surfactant mixtures with a high HLB (Fig. 16.6). It was suggested that inulin, encapsulated into the aqueous phase of the w/o nanoemulsions, was mainly transported via the transfollicular route and that its transport was facilitated by nanoemulsions in which the HLB of the oil phase was compatible with the sebum environment of the hair follicle.
Correlation between permeation rate of inulin across hairy mouse skin (expressed as per cent of applied formulation per h ± SE) and HLB of surfactant mixture in nanoemulsion or micellar formulation. HLB of surfactant mixture = ((volume per cent Span® 80 in formulation × 4.3) + (volume per cent Tween® 80 in formulation × 15.0))/100 (Reprinted from Wu et al. (2001), with permission from Elsevier)
These examples illustrate that the type of emulsifier/emulsifier system, together with the ratio of the emulsifier mixture, is not only essential to the emulsification and stabilisation effects but potentially also for modifying skin penetration significantly. Moreover, the HLB value may considerably influence topical performance.
Some studies reported that the various emulsifiers and/or ratios of emulsifier mixtures also altered the droplet size and viscosity of the emulsions, which may have affected dermal and transdermal delivery. The study by Klang et al. (2011), however, revealed that neither skin permeation nor penetration was influenced by the droplet size and viscosity. Klang et al. (2011) used sucrose stearate S-970 (Ryoto® Sugar Ester) as emulsifier to formulate stable o/w emulsions by forming a hydrophilic network around the oil droplets. Through a slight modification of the manufacturing process, they were able to produce a highly viscous macroemulsion and a less viscous, fluid nanoemulsion with exactly the same composition, thus enabling the investigation of the influence of droplet size and viscosity on dermal and transdermal delivery. The macro- and nanoemulsions showed neither significant difference in flux, penetration depth nor in accumulation of the three model drugs used (curcumin, flufenamic acid, diclofenac acid) in the stratum corneum. The results regarding droplet size are congruent with the outcome of the study by Izquierdo et al. (2007), where also no correlation could be found between the droplet size and the dermal and transdermal delivery. On the contrary, Nam et al. (2012) showed that the size of the emulsion droplets could affect skin absorption. They prepared nanoemulsions with the same chemical composition but different droplet sizes by applying different pressure in the microfluid process and found that smaller droplet sizes enhanced the skin absorption of tocopheryl acetate. However, transdermal delivery was not determined in this study.
6.4 Effects of Emulsion Droplet Charge
Positively and negatively charged submicron emulsions were compared by Youenang Piemi et al. (1999) for their effects on the dermal and transdermal delivery of econazole and miconazole nitrate. The composition of the emulsions was the same and only differed in the emulsifier component giving the charge to the emulsion droplets, i.e. stearylamine in the case of positively charged emulsions and deoxycholic acid in case of negatively charged emulsions. In overall, the positively charged o/w emulsion containing stearylamine was more effective in dermal and transdermal delivery of econazole and miconazole nitrate than the negatively charged o/w emulsion containing deoxycholic acid (Fig. 16.7). It was suggested that positively charged submicron emulsion droplets could facilitate the transport of the permeants into and through the skin, most probably owing to a superior binding of the positively charged droplets to the skin, which is negatively charged at neutral pH.
Permeation profiles of econazole and miconazole nitrate incorporated in negatively (−) and positively (+) charged submicron emulsion across hairless rat skin determined by HPLC. Approximately 37 μg of drug were applied per cell with an effective diffusional area of 0.635 cm2; n = 6; mean ± S.D (Reprinted from Youenang Piemi et al. (1999), with permission from Elsevier)
Two studies by Ghouchi Eskandar et al. (2009a, 2010), investigating oil-in-water submicron emulsions, also showed the possible dependency of dermal delivery on the emulsifier charge. The skin retention of the tested lipophilic compounds, all-trans-retinol and acridine orange 10-nonyl bromide, was significantly higher for those emulsions being stabilised by the positively charged oleylamine, compared to emulsions, stabilised by the negatively charged lecithin. Two explanations were given. Firstly, the higher skin accumulation of the lipophilic compounds being released from the oleylamine-stabilised emulsions could be attributed to the electrostatic attraction between the positively charged oleylamine droplets and negatively charged skin surface. Secondly, it could also have been due to reduced skin barrier properties, as a result of the disrupting effect of oleylamine on the stratum corneum lipid organisation.
6.5 Effects of Surfactant Association Structures
When viewing the effects of surfactants, one should not solely consider the surfactant but also the association structures that could form in emulsions. In addition to the formation of a surfactant monolayer at the oil-water interface, some surfactants, when in excess, may arrange in liquid crystalline structures in the aqueous phase, which may aid the stabilisation of emulsions (Friberg and Solans 1986) and could affect skin permeation. Only two studies are mentioned below to illustrate the effect of the emulsifier association structures on skin permeation. For more information on liquid crystalline structures, the reader is referred to a separate chapter in the book.
A study by Brinon et al. (1998) illustrated that the flux of benzophenone-4 (Uvinul® MS40) was increased by emulsions containing lamellar liquid crystals (triethanolamine stearate, sorbitan stearate/sucrose cocoate (Arlatone® 2121) and steareth-2/-21 (Brij® 72/721) in comparison to emulsions without liquid crystals (polysorbate 60 (Tween® 60), poloxamer 407 (Synperonic™ PE/F127) and acrylates/C10-30 alkyl acrylate crosspolymer (Pemulen® TR1)). The differences in permeation could be due to modified interactions between surfactants and permeant that may have influenced the interactions between the surfactants and stratum corneum. Furthermore, the partitioning between the formulation and the skin could have been altered, e.g. partitioning between the skin and the aqueous phase (emulsions without liquid crystals) and partitioning between the skin and the liquid crystal phase (emulsions with liquid crystals).
The effect of liquid crystalline structures in o/w emulsions on dermal and transdermal delivery was also investigated by Otto et al. (2010). Five o/w emulsions were tested:
-
‘Hydrosome’ emulsion, stabilised by sorbitan stearate and sucrose cocoate (Arlatone® 2121), with lamellar gel structuring of the water phase (Tadros et al. 2006)
-
‘Phosphosome EFA’ (essential fatty acid) emulsion, stabilised by linoleamidopropyl PG-dimonium chloride phosphate (Arlasilk™ Phospholipid EFA), with structuring of the water phase and lamellar liquid crystalline phases around the oil droplets
-
‘Phosphosome PTC’ (phosphatidylcholine) emulsion, stabilised by cocamidopropyl PG-dimonium chloride phosphate (Arlasilk™ Phospholipid PTC), with structuring of the water phase and lamellar liquid crystalline phases around the oil droplets
-
‘Oleosome’ emulsion, stabilised by steareth-2/steareth-21 (Brij® 72/721) incl. cetearyl alcohol (Laurex CS™) and PPG-15 stearyl ether (Arlamol™ E), with surfactant bilayers around the oil droplets (Tadros et al. 2006)
-
‘Conventional’ emulsion, stabilised by steareth-2/steareth-21 (Brij® 72/721), without liquid crystalline phases
The study revealed that the hydrosome and phosphosome emulsions, with lamellar gel structuring of the water phase, enhanced the dermal and transdermal delivery of hydroquinone and octadecenedioic acid (Arlatone™ DIOIC DCA), when compared with the conventional o/w emulsion without liquid crystalline phases and the oleosome emulsion with lamellar liquid crystalline phases around the oil droplets (Fig. 16.8a, b). The increase in skin penetration was ascribed to an improved partitioning of both permeants into the skin. However, a different pattern was observed for salicylic acid, where no differences in skin penetration occurred between the o/w emulsions with and without liquid crystalline phases (Fig. 16.8c). It was assumed that the interactions between the different emulsifiers and active ingredients varied and therefore the solubilisation capacities of the various emulsifiers and their association structures, which could have resulted in changes in the thermodynamic activity of the permeants in the emulsions.
(a) Skin permeation data on hydroquinone (HQ) expressed as total amount delivered over 8 h of skin penetration as least square means (formulation effect) ± 95 % confidence interval (CI) obtained after two-way ANOVA. Conv. conventional, Phosph. phosphosome. *Statistically significant compared with the conventional o/w emulsion (Reprinted from Otto et al. (2010), with permission from Karger). (b) Skin permeation data on octadecenedioic acid (DIOIC) expressed as total amount delivered over 24 h of skin penetration as least square means (formulation effect) ± 95 % confidence interval (CI) obtained after two-way ANOVA. Conv. conventional, Phosph. phosphosome. *Statistically significant compared with the conventional o/w emulsion (Reprinted from Otto et al. (2010), with permission from Karger). (c) Skin permeation data on salicylic acid (SA) expressed as total amount delivered over 12 h of skin penetration as least square means (formulation effect) ± 95 % confidence interval (CI) obtained after two-way ANOVA. Conv. conventional, Phosph. phosphosome. *Statistically significant compared with the conventional o/w emulsion (Reprinted from Otto et al. (2010), with permission from Karger)
6.6 Effects of Solid Particles as Emulsifiers
More recently, new topical emulsion systems have been introduced that are surfactant free and being stabilised by solid particles. These particle-stabilised emulsions are also known as Pickering emulsions. Another chapter in this book discusses Pickering emulsions as topical delivery systems; however, a few examples are mentioned below to illustrate the differences in topical performance due to different emulsifiers.
Frelichowska et al. (2009b) investigated the skin absorption of the hydrophilic active caffeine from silica particle-stabilised w/o emulsions (Pickering emulsions) and compared it to the absorption from surfactant-stabilised w/o emulsions (conventional emulsions). These emulsions had the same physicochemical properties (droplet size and viscosity), as well as chemical composition and only varied in the type of emulsifier. The study revealed that the caffeine flux was threefold higher from the Pickering emulsion than from the conventional emulsion, although the release was slower from the Pickering emulsion. The increased skin absorption could be explained by the higher adhesion of the silica particle-stabilised water droplets onto the skin surface. Furthermore, it was found that silica particles penetrated into the upper layers of the stratum corneum and it was hypothesised that caffeine was transported into the skin by means of adsorption onto the silica particles.
Another study by Frelichowska et al. (2009a), investigating oil-in-water emulsions, revealed that the total skin uptake of the lipophilic drug, all-trans-retinol, was similar for the conventional emulsion and the Pickering emulsion and no transdermal delivery was observed. However, the distribution of all-trans-retinol within the skin varied. The Pickering emulsion showed an enhanced accumulation of all-trans-retinol in the stratum corneum, whereas the conventional emulsion increased the transport through the stratum corneum into the viable epidermis and dermis. It was hypothesised that the enhanced accumulation of all-trans-retinol in the stratum corneum could be due to a lack of flexibility of the Pickering emulsion droplets.
The former studies compared Pickering emulsions being stabilised solely by solid particles with conventional emulsions being stabilised solely by surfactants. However, emulsions with mixed interfacial layers, for instance, including both surfactants and solid particles, were also tested for their topical performances, as discussed next.
Silica nanoparticle coatings of lecithin- and oleylamine-stabilised oil-in-water submicron emulsions exhibited an enhanced dermal delivery of all-trans-retinol and acridine orange 10-nonyl bromide, compared to non-silica-coated emulsions (Ghouchi Eskandar et al. 2009a, 2010). As the silica nanoparticles significantly increased the emulsification efficiency, as well as the physical stability of the emulsions (Ghouchi Eskandar et al. 2007), they could be considered as emulsifiers. In both studies it was observed that the extent and the depth of penetration of lipophilic all-trans-retinol and acridine orange 10-nonyl bromide into full-thickness porcine skin were increased by nanoparticle-coated emulsions and they both were affected by the initial loading phase of the silica nanoparticles during the preparation of the emulsions (e.g. incorporation into the water phase vs. oil phase). However, the silica coating did not influence the transdermal delivery of the two compounds, which was considered negligible. It was further shown that silica nanoparticles could also penetrate the skin up to the viable epidermis and dermis, with negligible permeation across the skin. There was a correlation found between the skin accumulation and distribution of acridine orange 10-nonyl bromide and silica nanoparticles, and it was hypothesised that the transport of acridine orange 10-nonyl bromide could have been facilitated by electrostatic complexation with silica nanoparticles (Ghouchi Eskandar et al. 2010). Furthermore, the improved physical stability of silica-coated emulsions and enhanced chemical stability of all-trans-retinol (Ghouchi Eskandar et al. 2009b) are other possible mechanisms for the increased skin retention. Additionally, the formation of a thick film of silica nanoparticles and emulsion oil droplets on the skin surface could have had an occlusive effect that may have increased the hydration of the stratum corneum, which in turn could have enhanced skin penetration (Ghouchi Eskandar et al. 2009a).
7 Conclusion
This review has emphasised that different parameters/variables require consideration when deciding on an appropriate emulsion type and emulsifier system. For example, the skin uptake into the skin as well as the permeation through the skin of a hydrophilic active could be enhanced, when the active is incorporated into the continuous phase of the emulsion. Furthermore, multiple o/w/o emulsions, in comparison to simple w/o emulsions, reduced the transdermal delivery of lipophilic active ingredients, whereas the dermal delivery was increased. Therefore, multiple emulsions could be considered if prolonged topical delivery or the protection of the active ingredient against external influences (e.g. enzymatic degradation, oxidation) is desired. It was demonstrated that the effects of surfactants, as incorporated in emulsions, on dermal and transdermal delivery could vary, depending on their structure and physicochemical properties, e.g. HLB value, hydrophilic chain length of nonionic surfactants, emulsifier charge or their association structures in the emulsion. However, the emulsifier could also influence the droplet size and viscosity of emulsions, which in turn may additionally affect topical performance. Pickering emulsions, a rather new topical delivery system type, are not only interesting in terms of improving the physical stability of emulsions but also show the potential for dermal skin targeting and controlled release.
In summary, it can be concluded that the choice of the emulsifier is not only critical for the emulsification process and for the stability of the resulting emulsion but it is also important for the dermal and transdermal performance that additionally is influenced by the type of emulsion.
References
Anton N, Vandamme TF (2011) Nano-emulsions and micro-emulsions: clarifications of the critical differences. Pharm Res 28:978–985
Aveyard R, Binks BP, Clint JH (2003) Emulsions stabilised solely by colloidal particles. Adv Colloid Interf Sci 100–102:503–546
Bancroft WD (1913) The theory of emulsification. J Phys Chem 17:501–520
Bernardo FP, Saraiva PM (2008) A theoretical model for transdermal drug delivery from emulsions and its dependence upon formulation. J Pharm Sci 97:3781–3809
Binks BP, Whitby CP (2005) Nanoparticle silica-stabilized oil-in-water emulsions: improving emulsion stability. Colloids Surf A 253:105–115
Brinon L, Geiger S, Alard V, Tranchant J-F, Pouget T, Couarraze G (1998) Influence of lamellar liquid crystal structure on percutaneous diffusion of a hydrophilic tracer from emulsions. J Cosmet Sci 49:1–11
Cho HK, Cho JH, Choi S-W, Cheong IW (2012) Topical delivery of retinol emulsions co-stabilised by PEO-PCL-PEO triblock copolymers: effect of PCL block length. J Microencapsul. doi:10.3109/02652048.2012.686528
Dal Pozzo A, Pastori N (1996) Percutaneous absorption of parabens from cosmetic formulations. Int J Cosmet Sci 18:57–66
Dalvi UG, Zatz JL (1981) Effect of nonionic surfactants on penetration of dissolved benzocaine through hairless mouse skin. J Soc Cosmet Chem 32:87–94
Eccleston GM (1997a) Formulating cosmetic emulsions: – advances in understanding emulsion technology. Cosmet Toilet 112(12):65–71
Eccleston GM (1997b) Functions of mixed emulsifiers and emulsifying waxes in dermatological lotions and creams. Colloids Surf A 123–124:169–182
Ferreira LAM, Seiller M, Grossiord JL, Marty JP, Wepierre J (1994) Vehicle influence on in vitro release of metronidazole: role of w/o/w multiple emulsion. Int J Pharm 109:251–259
Ferreira LAM, Doucet J, Seiller M, Grossiord JL, Marty JP, Wepierre J (1995a) In vitro percutaneous absorption of metronidazole and glucose: comparison of o/w, w/o/w, w/o systems. Int J Pharm 121:169–179
Ferreira LAM, Seiller M, Grossiord JL, Marty JP, Wepierre J (1995b) Vehicle influence on in vitro release of glucose: w/o, w/o/w and o/w systems compared. J Control Rel 33:349–356
Förster T, Von Rybinski W (1998) Applications of emulsions. In: Binks BP (ed) Modern aspects of emulsion science. Royal Society of Chemistry, Cambridge, pp 395–426
Förster T, Jackwerth B, Pittermann W, Von Rybinski W, Schmitt M (1997) Properties of emulsions – structure and skin penetration. Cosmet Toilet 112(12):73–82
Förster M, Bolzinger MA, Ach D, Montagnac G, Briançon S (2011) Ingredients tracking of cosmetic formulations in the skin: a confocal Raman microscopy investigation. Pharm Res 28:858–872
Frelichowska J, Bolzinger M-A, Pelletier J, Valour J-P, Chevalier Y (2009a) Topical delivery of lipophilic drugs from o/w Pickering emulsions. Int J Pharm 371:56–63
Frelichowska J, Bolzinger M-A, Valour J-P, Mouaziz H, Pelletier J, Chevalier Y (2009b) Pickering w/o emulsions: drug release and topical delivery. Int J Pharm 368:7–15
Friberg SE (1990) Micelles, microemulsions, liquid crystals, and the structure of stratum corneum lipids. J Soc Cosmet Chem 41:155–171
Friberg SE, Langlois B (1992) Evaporation from emulsions. J Disp Sci Technol 13:223–243
Friberg SE, Ma Z (2006) Emulsions: factors and issues for skin care. In: Wille JJ (ed) Skin delivery systems: transdermals, dermatologicals, and cosmetic actives. Wiley-Blackwell, Ames, pp 187–209
Friberg SE, Solans C (1986) Surfactant association structures and the stability of emulsions and foams. Langmuir 2:121–126
Ghouchi Eskandar N, Simovic S, Prestidge CA (2007) Synergistic effect of silica nanoparticles and charged surfactants in the formation and stability of submicron oil-in-water emulsions. Phys Chem Chem Phys 9:6426–6434
Ghouchi Eskandar N, Simovic S, Prestidge CA (2009a) Nanoparticle coated submicron emulsions: sustained in-vitro release and improved dermal delivery of all-trans-retinol. Pharm Res 26:1764–1775
Ghouchi Eskandar N, Simovic S, Prestidge CA (2009b) Chemical stability and phase distribution of all-trans-retinol in nanoparticle-coated emulsions. Int J Pharm 376:186–194
Ghouchi Eskandar N, Simovic S, Prestidge CA (2010) Mechanistic insight into the dermal delivery from nanoparticle-coated submicron o/w emulsions. J Pharm Sci 99:890–904
Grégoire S, Ribaud C, Benech F, Meunier JR, Garrigues-Mazert A, Guy RH (2009) Prediction of chemical absorption into and through the skin from cosmetic and dermatological formulations. Br J Dermatol 160:80–91
Harusawa F, Saito T, Nakajima H, Fukushima S (1980) Partition isotherms of nonionic surfactants in the water-cyclohexane system and the type of emulsion produced. J Colloid Interface Sci 74:435–440
Izquierdo P, Wiechers JW, Escribano E, García-Celma MJ, Tadros TF, Esquena J, Dederen JC, Solans C (2007) A study on the influence of emulsion droplet size on the skin penetration of tetracaine. Skin Pharmacol Physiol 20:263–270
Klang V, Schwarz JC, Matsko N, Rezvani E, El-Hagin N, Wirth M, Valenta C (2011) Semi-solid sucrose stearate-based emulsions as dermal drug delivery systems. Pharmaceutics 3:275–306
Lalor CB, Flynn GL, Weiner N (1995) Formulation factors affecting release of drug from topical vehicles II. Effect of solubility on in vitro delivery of a series of n-alkyl p-aminobenzoates. J Pharm Sci 84:673–676
Lan Q, Yang F, Zhang S, Liu S, Xu J, Sun D (2007) Synergistic effect of silica nanoparticle and cetyltrimethyl ammonium bromide on the stabilization of o/w emulsions. Colloids Surf A 302:126–135
Laugel C, Baillet A, Ferrier D, Grossiord JL, Marty JP (1998a) Incorporation of triterpenic derivatives within an o/w/o multiple emulsion: structure and release studies. Int J Cosmet Sci 20:183–191
Laugel C, Baillet A, Youenang Piemi MP, Marty JP, Ferrier D (1998b) Oil-water-oil multiple emulsions for prolonged delivery of hydrocortisone after topical application: comparison with simple emulsions. Int J Pharm 160:109–117
McClements DJ (2012) Nanoemulsions versus microemulsions: terminology, differences, and similarities. Soft Matter 8:1719–1729
Montenegro L, Paolino D, Puglisi G (2004) Effects of silicone emulsifiers on in vitro skin permeation of sunscreens from cosmetic emulsions. J Cosmet Sci 55:509–518
Nam YS, Kim J-W, Park JY, Shim J, Lee JS, Han SH (2012) Tocopheryl acetate nanoemulsions stabilized with lipid-polymer hybrid emulsifiers for effective skin delivery. Colloids Surf B 94:51–57
Oborska A, Arct J, Mojski M, Jaremko E (2004) Influence of polyalcohols and surfactants on skin penetration of flavonoids from the emulsion. J Appl Cosmetol 22:35–42
Otto A, Wiechers JW, Kelly CL, Dederen JC, Hadgraft J, du Plessis J (2010) Effect of emulsifiers and their liquid crystalline structures in emulsions on dermal and transdermal delivery of hydroquinone, salicylic acid and octadecenedioic acid. Skin Pharmacol Physiol 23:273–282
Sah A, Mukherjee S, Wickett RR (1998) An in vitro study of the effects of formulation variables and product structure on percutaneous absorption of lactic acid. J Cosmet Sci 49:257–273
Schmidts T, Dobler D, von den Hoff S, Schlupp P, Garn H, Runkel F (2011) Protective effect of drug delivery systems against the enzymatic degradation of dermally applied DNAzyme. Int J Pharm 410:75–82
Tadros TF (2009) Emulsion science and technology: a general introduction. In: Tadros TF (ed) Emulsion science and technology. Wiley VCH, Weinheim, pp 1–56
Tadros T, Leonard S, Taelman M-C, Verboom C, Wortel V (2006) Correlating the structure and rheology of liquid crystalline phases in emulsions. Cosmet Toilet 121(5):89–94
Wiechers JW (2005) Optimizing skin delivery of active ingredients from emulsions from theory to practice. In: Rosen MR (ed) Delivery system handbook for personal care and cosmetic products. William Andrew, Norwich, pp 409–436
Wiechers JW, Kelly CL, Blease TG, Dederen JC (2004) Formulating for efficacy. Int J Cosmet Sci 26:173–182
Wu H, Ramachandran C, Weiner ND, Roessler BJ (2001) Topical transport of hydrophilic compounds using water-in-oil nanoemulsions. Int J Pharm 220:63–75
Youenang Piemi MP, De Luca M, Grossiord J-L, Seiller M, Marty J-P (1998) Transdermal delivery of glucose through hairless rat skin in vitro: effect of multiple and simple emulsions. Int J Pharm 171:207–215
Youenang Piemi MP, Korner D, Benita S, Marty J-P (1999) Positively and negatively charged submicron emulsions for enhanced topical delivery of antifungal drugs. J Control Rel 58:177–187
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Otto, A., du Plessis, J. (2015). The Effects of Emulsifiers and Emulsion Formulation Types on Dermal and Transdermal Drug Delivery. In: Dragicevic, N., Maibach, H. (eds) Percutaneous Penetration Enhancers Chemical Methods in Penetration Enhancement. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-45013-0_16
Download citation
DOI: https://doi.org/10.1007/978-3-662-45013-0_16
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-45012-3
Online ISBN: 978-3-662-45013-0
eBook Packages: MedicineMedicine (R0)