Abstract
The assessment of the cardiovascular system condition based on multiple parameters allows a more precise and accurate diagnosis of the heart and arterial tree condition. For this reason, the interest in non-invasive devices has presently increased in importance. In this work, an optical probe was tested in order to validate this technology for measuring multiple parameters such as Pulse Wave Velocity (PWV) or Augmentation Index (AIx), amongst others. The PWV measured by the optical probe was previously compared with the values obtained with the gold-standard system. Another analysis was performed in 131 young subjects to establish carotid PWV reference values as well as other hemodynamic parameters and to find correlations between these and the population characteristics. The results allowed us to conclude that this new technique is a reliable method to determine these parameters. The range of the obtained values for local PWV are in agreement with the values obtained by other studies, and significant correlations with age and smoking status were found. The AIx varied between −6.15 % and 11.46 % and exhibit a negative correlation with heart rate, and dP/dtmax shows a significant decrease with age.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The interest in non-invasive assessment of cardiovascular function has increased over the recent times, particularly around solutions able to perform multi parameter assessment for monitoring and early diagnosis of cardiovascular pathologies [1–4].
The pulse wave velocity and the parameters extracted from pulse waveform analysis (PWA) are widely used tools in the evaluation of the function of large arteries and cardiac activity, which have been shown to predict cardiovascular diseases [5].
The assessment of the cardiovascular system condition based on multi parameters allows more precise and accurate diagnosis of the heart and arterial tree condition. Risk indicators that can be assessed from the distension waveforms acquired through the hereby presented system, can be determined from the main parameters extracted from measured and analysed waveform, as well as its time characteristics and the pulse wave velocity.
The PWV is defined as the speed at which the pulse pressure propagates along the arterial tree. It is known that PWV increases with age, blood pressure (BP) and arterial stiffness [5, 6]. The reference value for regional PWV in healthy young population is 6.2 m s−1 (range of 4.7–7.6 m s−1) [6] and is usually measured from signals acquired in the femoral and carotid arteries. The time delay, or pulse transit time (PTT) between the two signals is determined through different algorithms depending on the commercial system used, while the distance (D) between the two arteries is externally measured. However, the large heterogeneity of the structure of the arterial walls at different sites constitutes an important limitation of PWV regional measurement [7]. In fact, the Expert Consensus Document in Arterial Stiffness states that the PWV increases from 4–5 m s−1 in the ascending aorta to 5–6 m s−1 in the abdominal aorta and 8–9 m s−1 in the iliac and femoral arteries [8]. A local PWV measurement technique is hence preferred.
Some studies [9] explored an ultrasound method for local PWV assessment in the carotid artery and obtained estimated PWV in the range of 4–9 m s−1. In 2008 [10] an experimental method for the local determination of PWV in the carotid artery obtained values for PWV of 3–4 m s−1.
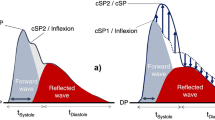
The pulse wave analysis allows the non-invasive determination of main indices of cardiovascular function: Augmentation Index (AIx), Subendocardial Viability Ratio (SEVR), Maximum Rate of Pressure Change (dP/dtmax) and Ejection Time Index (ETI). The most important points of the pulse pressure waveform are presented in Fig. 1.
Typical pressure waveform of a healthy subject and its main features used to compute the indices of cardiovascular function: pulse pressure (PP), systolic peak (SP), reflection point (RP), dicrotic notch (DN), dicrotic peak (DP), systolic duration (SD), total duration (TD) and pressure in the reflection point (Pi).
The clinical definition for the referred parameters and the mathematical expressions for their determination are summarized in Table 1.
If the backward wave arrives before the systolic peak, the AIx parameter, by definition, has a positive value due to the contribution of the increased systolic pressure. If the backward wave arrives later, it does not contribute to the increased pressure, turning the AIx value negative.
Taking into account the currently available commercial devices, a new solution based on optical technology was developed and demonstrably benefits by a non-contact and more accurate measure and multi parameter assessment ability [14].
The PWV assessment from the commercial systems consists always on a regional measurement, between two peripheral arteries as already described. With this work a local measure of PWV is proposed, where two measurements are taken at the carotid artery, simultaneously and separated by a 20 mm distance [15].
The carotid artery is the natural probing site for pulse waveform measurement, due to the heart proximity and because it is easily accessible due to its proximity to the skin surface.
The purpose of this study was to validate the optical system for PWV and PWA measurements. Firstly, it was intended to assess the values for local PWV, to establish its reference values for the carotid artery in a young and healthy population and validate the technology for hemodynamic parameters assessment from the pulse pressure waveform. The study also aimed to find correlations between hemodynamic parameters with the population characteristics such as age, gender, smoking, body mass index, blood pressure or heart rate: main characteristics described in the literature and that have significant impact in the cardiovascular system evaluation.
2 Technology
The pressure wave, generated by the contraction of the left ventricle, originates a distension wave that propagates through the aorta and other proximal elastic arterial walls. The distensibility is determined as the ratio between the variation of volume from diastole to systole and the variation of pressure that origins that distension in the arterial wall [8].
Previous studies on comparison between pressure and distension waveforms have shown that these waves can be used interchangeably for many analysis due to their similar wave contour [8, 16–18].
The proposed probes were developed to measure the arterial pulse wave profile at the carotid site and are based on the reflectance fluctuations of the skin surface during the underlying pulse wave propagation. The propagation of the pulse pressure waveform causes distension in the artery wall. This distension, known as distension wave, changes the optical reflectance angle of the wall which produces a change in the reflection characteristics of skin, causing an amplitude modulation of the light. This effect can be used to generate an optical signal that correlates with the passing pressure wave.
The illumination source is provided by local, high brightness, 635 nm monochromatic light emitting diodes (LEDs) and the light detection is performed by two photodetectors, placed at a precise distance of 20 mm apart. This guarantees the local pulse wave profile assessment at two distinct spots, providing the precise local determination of pulse transit time (PTT) and thus of the local PWV. The probe structure is enclosed in a plastic box with an ergonomic configuration, comfortable to the patient and simple to use by the operator (Fig. 2).
The plastic case contacts with the patient skin although neither the LEDs nor the photodetectors do. The electronic components remain at a fixed distance, few millimetres from the skin ensuring a totally non-contact and non-invasive local PWV assessment.
Previous bench tests had shown that the optical probe is capable of accurately measure PTT as short as 1 ms with less than 1 % of error, one can guarantee the capability of the probes in truthfully determining local PWV [19].
The comparison tests to evaluate the capability of the developed device in accurately detect the pulse waveform were carried out using an ultrasound imaging system, as source of reference data. When compared with ultrasound system, the optical sensors allow the reproduction of the arterial waveform with a much higher time resolution, adequate to feed feature extraction algorithms [14].
The signals from the photodetectors were digitized with a 16-bit resolution data acquisition system (National Instruments, USB6210®) with a sampling rate of 20 kHz and stored for offline analysis. All the algorithms were developed using Matlab® 7.8.0 (R2009a).
3 Preliminary Validation Study
In order to validate the data obtained by the developed optical system, a number of volunteers were previously submitted to a signal acquisition procedure, using simultaneously the proposed optical device and a gold-standard in the PWV assessment, a Complior Analyse® device. This preliminary study was undertaken in 14 healthy subjects (9 females, average age 23.2 ± 5.5 years).
The results showed a great consistency between the PWV obtained with the two devices. In spite of this comparison, it is worth to note that the nature of the PWV determination is different between the optical system, that is based on local assessment (carotid artery measure) and the Complior® system, which is based on a regional assessment (carotid-femoral measures).
Using a non-parametric correlation analysis between the values obtained from the two systems, the Pearson correlation value is 0.819, which is a strong correlation and significant at the 0.01 level (2-tailed).
The agreement between the PWV values obtained by the Complior® and the optical probe is shown in Fig. 3 (top). The values of PWV obtained by the two systems are correlated (r2 = 0.67). The average difference between the two systems, Complior® and Optical probe, was −1.8557 m s−1with a SD of 0.5744 m s−1 as shown in a Bland-Altman plot in Fig. 2 (bottom). As one can observe in Fig. 3 (top), there is a tendency to have systematic lower values from the optical probe device than Complior®. Again, it is important to bear in mind that the values obtained using both devices correspond to different PWV determination processes (local vs. regional) and lower values are expected for PWV in the carotid (local) than the PWV in a carotid-femoral measurement (regional). This issue could explain the associated deviate of final values.
Taken together, these results allow the use of this proposed optical system as a reliable method to determine local carotid PWV.
4 Study Protocol
The central purpose of these tests is to assess the main hemodynamic parameters extractable from the pressure waveform features and pulse wave velocity, in a young and healthy population using the optical system.
The complete study database contains 131 subjects constituting a representative cohort of 18–35 year old subjects randomly sampled. The study protocol was approved by the ethical committee of the Centro Hospitalar e Universitário de Coimbra, EPE Portugal. All the subjects were volunteers and gave a written informed consent.
Measurements were performed after a rest period in a temperature-controlled environment. Each exam procedure consisted in the acquisition of a set of cardiac cycles at the carotid artery during few minutes, with the patient lying in supine position.
The assessment of the arterial blood pressure (ABP) by conventional measurement using an automated digital oscillometric sphygmomanometer (Omron Matsusaka Co., Ltd., Japan) was performed prior and after the exam for reference purposes. The diastolic and systolic pressures of arm blood pressure were used to calibrate the system.
5 Signal Processing
The stored signal data were processed offline in order to parameterize the arterial pulse waveform and to calculate the corresponding cardiovascular performance indexes. A set of dedicated pre-processing algorithms were developed to segment the data stream in single cycles, generate an average pulse and identify the corresponding remarkable points in the waveform profile. Following this stage, the signal streams underwent the full processing sequence to determine all the significant APW features and indexes along with the local PWV.
The pulse wave velocity was determined by a cross-correlation method, based on the property of the peak of the cross correlogram, from which time delays can be calculated by subtracting the peak time position from the pulse length.
The pulse wave analysis is based on differential calculus, and uses zero-crossing of the three first derivatives. The remarkable points were found by means of an iterative third-order derivative method, with which the consecutive zero-crossing of the first, second and third derivatives are used to detect inflection points that correspond to the clinically interesting features of the waveform.
An assessment of ABP by conventional measurement using a sphygmomanometer was conducted prior and after the exam for calibration purposes. Both brachial diastolic (DBP) and mean arterial pressure (MAP) values were used to calibrate the system. Studies have reported that MAP is relatively constant along the arterial tree and that DBP do not vary considerably between the carotid and brachial arteries, whereas systolic blood pressure (SBP) increases along the arterial tree [7, 20]. Thus, we made the assumption that brachial DBP and MAP are approximately the same as carotid DBP and MAP. These values were used to calibrate the carotid pressure waveform as recommended and according to the calibration method proposed by Kelly and Fitchett [8, 21, 22].
6 Results
The characteristics of the volunteers are presented in Table 2. The group consisted of 131 subjects (62 men and 69 women), normotensive and with no documented history of cardiovascular disorders or diabetes, with mean (± SD) age of 22.6 ± 5.3 years old.
The results for the parameters that were assessed by the optical probe are presented in the next sections. Data are reported as mean values (± SD) or 95 % confidence intervals, with P < 0.05 considered significant unless stated otherwise. The Shapiro-Wilk test of normality was used to assess the normality of the variables distribution. Mean differences between variables were assessed using ANOVA. The strength of the association between two variables was assessed using Pearson Correlation, for normal distributions, unless stated otherwise.
All statistical analyses were performed with Analytics Software Statistics 18.0.0 (SPSS, Inc, Chicago, IL).
6.1 Carotid PWV Results
In a total of 131 subjects the mean value for PWV is 3.33 ± 0.72 m s−1 (range of 2.00-5.13 m s−1). The results obtained for PWV approximated a normal distribution. Statistically negligible differences between genders were found. For females the mean of PWV is 3.31 ± 0.64 m s−1 and for males is 3.35 ± 0.81 m s−1.
It is well documented in other studies that PWV tends to increase with age [6]. Since the population under study is young we categorized it in three groups: under 20 years (22 subjects), 21–29 years (93 subjects) and over 30 years old (16 subjects).
The correlation between PWV and age is weak (0.244) but significant with a 2-tailed significance value of 0.008 (p < 0.01). The comparison of PWV mean values among the different age categories using ANOVA shown this statistically significant difference, with a significance value = 0.024 (p < 0.05). The PWV mean value (± SD) for each age category is 2.96 ± 0.52 m/s for the less than 20 years old group, 3.38 ± 0.7 m/s for the 20–29 years group and 3.58 ± 0.7 m/s for subjects above 30 years old (Fig. 4).
It was hypothesized whether there is statistically significant difference for PWV, between smoker and non-smoker subjects. The data analysis shows that smoking influences significantly the PWV.
These results show a small but significant correlation between PWV and smoking with a 2-tailed significance value of 0.016 (p < 0.05). Non-smoker subjects presented a PWV mean value (± SD) of 3.29 ± 0.72 m s−1 while smoker subjects showed a mean PWV value of 3.81 ± 0.6 m s−1, represented in Fig. 5.
The comparison of PWV mean values among these two groups using ANOVA confirms the statistically significant difference between the obtained PWV for smokers and non-smokers, with a significance value = 0.021 (p < 0.05).
The data suggests that, in spite of having a young population, smoking would significantly influence the arterial stiffness, thus leading to increased PWV. Similar findings have been reported by N. Jatoi et al., [23].
Contrary to expectations, no significant correlation between blood pressure and PWV was found. This contrasts with other studies where this correlation is verified [6, 24].
6.2 AIx Results
For the total of the subjects in study, the mean value for AIx is −6.151 ± 11.46 % (range −44.31 % to 24.26 %).
Small differences between genders were verified, as the female mean of AIx is −5.59 ± 1.36 % and the male is −6.93 ± 1.59 %. However, this difference did not reach the statistical significance threshold (P > 0.05).
Also for this parameter, as well as for PWV, statistically differences between smoker and non-smoker subjects were found. AIx is higher for smokers (−4.33 ± 4.42 %) than for non-smokers (−6.35 ± 1.04 %), this shows that for smokers the reflected wave arrives earlier in time, which is consistent with a slight higher the arterial stiffness.
The negative correlation between the AIx and the heart rate was described in other tests [4, 25] and was confirmed in this study (Fig. 6). The results of Person-Correlation test were compatible with a significant negative correlation, between heart rate (HR) and AIx at a 0.05 level (2-tailed). Nevertheless, the strength of the relationship found between these two variables is medium, since the Pearson Correlation is significant with a 2-tailed significance value of −0.226 (p < 0.05). The comparison of AIx mean values among these three groups using ANOVA confirms a statistically significant difference, with a significance value = 0.024 (p < 0.05).
The negative correlation between these two parameters is explained due to the early return of the reflected wave in systole when HR is lower, and the long period of heart contraction.
6.3 Other Hemodynamic Parameter Results
The Ejection Time Index, Subendocardial Viability Ratio and Maximum Rate of Pressure Change are other hemodynamic parameters assessed by the optical system, and the results for the population in study are shown in Table 3.
It is remarkable that the mean values of SEVR and ETI stay within the range presented by other studies (Table 1) even though it is clear that they show a wide variation. For the SEVR parameter it was also verified a decrease with the heart rate (Fig. 7) with a significant variance (ANOVA, P = 0.01) and a significant Pearson correlation at 0.01 level (2-tailed).
The derived values for dP/dtmax differ substantially from the ones presented by other studies, a wider range than the expected and a smaller mean value is evident probably originated by the differences in the calibration method used. However, a relation between dP/dtmax. and gender, was found, since the Pearson Correlation is -0.408. The female subjects showed lower values for this parameter, which are represented in Fig. 8.
The dP/dtmax values decrease significantly with subjects’ age, this allows the inferring that with the increasing age the velocity of the myocardial contraction is lower, meaning that there is a decrease in the myocardial performance.
For the ETI parameter there were verified slight differences between gender, the mean vales for the females is 36.80 ± 0.72 % and for males 33.60 ± 0.85 %. This suggests that there is a shorter systole during cardiac cycle in males than in females. Also for this parameter, a significance correlation with heart rate was found since the Pearson Correlation is −0.408.
7 Conclusions
These trial tests were carried out in a large group of young and healthy subjects. This study has attempted to validate the proposed optical system as a reliable method to assess non-invasively local PWV in the carotid artery, to establish reference values of the local PWV as well as other mentioned parameters in this type of population.
Previously, this new system had also proved to be reliable in reproducing the arterial waveform with a higher resolution, adequate to feed feature extraction algorithms, when compared to an ultrasound image system that was used as a reference for comparison.
Besides of the ability of the optical system in acquiring non-invasively a carotid distension waveform with high definition, the presented optical system shows other advantages over the actual commercial devices.
One advantage of this optical approach relies on being a non-contact technique that avoids the drawback of pressure application as happens with piezoelectric transducers that could result in the distortion of the signal of interest.
Another benefit is the possibility of local PWV assessment, in a single arterial segment, avoiding coarse approximations of the distance between test points constituting an important advance in the PWV assessment.
The validation test, in which the obtained values using the optical probes were compared with those obtained with a commercial device are supported by all the previous bench test results and allowed to consider this technique as a valid method to assess PWV and analyse PWA parameters.
The range of the obtained values for local CA PWV are in agreement with the values obtained by other studies that also assessed the carotid local PWV. The expected and obtained lower values of the carotid PWV assessment when compared to those obtained with Complior® device are due to the different PWV determination processes (local vs. regional). The lack of compatibility between methods limits the inferences that can be made and thus, more studies of repeatability, comparing the local PWV obtained by the optical system with the values estimated by ultrasound data, are necessary to ensure accuracy of the proposed system.
The PWV measured by the optical probe confirmed a significant increase of PWV with age. Even though the sample consists of young subjects with a relatively narrow age distribution, this result generally agrees with those obtained in other studies.
The PWA parameters revealed the important relations between some characteristics of the population and the arterial system status. The negative correlation between the AIx and the heart rate were verified in this study, and differences between gender and smokers/non-smokers were found.
For SEVR parameter was also verified a decrease with heart rate. The dP/dtmax. analysis showed a difference with gender, with lower values for female subjects, and this parameter decreased significantly with age.
All the correlations obtained in this study showed that age contributes to the arterial stiffness as reflected in the values found for various parameters. Smokers appear to have higher arterial age, and therefore increased cardiovascular risk.
The optical system under study proved to be a good choice for determination of hemodynamic parameters in a non-invasive and non-contact assessment, which allows a better knowledge about the cardiovascular condition and management of many disease states. Further studies must compare the non-invasive measurement of distension waveform in carotid artery with the invasive profile of the pulse pressure acquired by an intra-arterial catheter in ascending aorta, in patients who have undergone cardiac catheterization.
Another study should be designed to evaluate the behaviour of the carotid artery in atherosclerosis. In this case the comparison between invasive data (catheter) and Ecodoppler signals will be important to prove the agreement with non-invasive signals acquired by the optical probe in this particular disease.
Although this method provides a set of parameters strongly related to pulse waveform morphology it needs a proper and extensive gold standard comparison with an invasive system.
Finally, it is worth mentioning that, in spite of its lack of maturity (meaning that many engineering aspects of the probe can still be improved), the proposed method exhibits a very high patient hit success. In fact, for 119 out of 131 patients (90 %) it took around 1 to 2 mins to start acquiring reasonable quality signals, each take lasting for 30 seconds. Although some training is required, the method is much less demanding on the operator skills as compared to ultrasound, Complior® or tonometer.
References
Willum-Hansen, T., Staessen, J.A., Torp-Pedersen, C., Rasmussen, S., Thijs, L., Ibsen, H., Jeppesen, J.: Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 113(5), 664–670 (2006)
Blacher, J., Asmar, R., Djane, S., London, G.M., Safar, M.E.: Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 33(5), 1111–1117 (1999)
Hayashi, T., Nakayama, Y., Tsumura, K.: Reflection in the arterial system. Am. J. Hypertens. 15(5), 405–409 (2002)
Weber, T., Auer, J., O’Rourke, M.F., Kvas, E., Lassnig, E., Berent, R., Eber, B.: Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation 109(2), 184–189 (2004)
Huck, C.J., Bronas, U.G., Williamson, E.B., Draheim, C.C., Duprez, D.A., Dengel, D.R.: Noninvasive measurements of arterial stiffness: repeatability and interrelationships with endothelial function and arterial morphology measures. Vasc. Health Risk Manage. 3(3), 343–349 (2007)
Vermeersch, S.J., Dynamics, B., Society, L.: Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur. Heart J. 31(19), 2338–2350 (2010)
Safar, M.E.: Arterial stiffness: a simplified overview in vascular medicine. Atherosclerosis, Large Arteries Cardiovasc. Risk 44, 1–18 (2007)
Laurent, S., Cockcroft, J., Van Bortel, L., Boutouyrie, P., Giannattasio, C., Hayoz, D., Pannier, B., Vlachopoulos, C., Wilkinson, I., Struijker-Boudier, H.: Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur. Heart J. 27(21), 2588–2605 (2006)
Rabben, S.I., Stergiopulos, N., Hellevik, L.R., Smiseth, O.A., Slørdahl, S., Urheim, S., Angelsen, B.: An ultrasound-based method for determining pulse wave velocity in superficial arteries. J. Biomech. 37(10), 1615–1622 (2004)
Sørensen, G.L., Jensen, J.B., Udesen, J., Holfort, I.K.: Pulse wave velocity in the carotid artery, vol. 1(1), pp. 1386–1389 (2008)
Siebenhofer, A., Kemp, C., Sutton, A., Williams, B.: The reproducibility of central aortic blood pressure measurements in healthy subjects using applanation tonometry and sphygmocardiography. J. Hum. Hypertens. 13(9), 625–629 (1999)
Payne, R.A., Hilling-Smith, R.C., Webb, D.J., Maxwell, S.R., Denvir, M.A.: Augmentation index assessed by applanation tonometry is elevated in Marfan Syndrome. J. Cardiothorac. Surg. 2, 43 (2007)
Istratoaie, O., Mustafa, R., Donoiu, I.: Central aortic pressure estimated by radial applanation tonometry in hypertensive pulmonary oedema. J. Hyperten. 28(p e149) (2010)
Pereira, T., Oliveira, T., Cabeleira, M., Matos, P., Pereira, H.C., Almeida, V., Borges, E., Santos, H., Pereira, T., Cardoso, J., Correia, C.: Signal analysis in a new optical pulse waveform profiler for cardiovascular applications. In: Signal and Image Processing and Applications/716: Artificial Intelligence and Soft Computing, Sipa, pp. 19–25 (2011)
Pereira, T., Oliveira, T., Cabeleira, M., Almeida, V., Borges, E., Cardoso, J., Correia, C., Pereira, H.C.: Visible and infrared optical probes for hemodynamic parameters assessment. In: 2011 IEEE SENSORS Proceedings, pp. 1796–1799, Oct 2011
Avolio, P., Van Bortel, L.M., Boutouyrie, P., Cockcroft, J.R., McEniery, C.M., Protogerou, A.D., Roman, M.J., Safar, M.E., Segers, P., Smulyan, H.: Role of pulse pressure amplification in arterial hypertension: experts’ opinion and review of the data. Hypertension 54(2), 375–383 (2009)
Kips, J., Vanmolkot, F., Mahieu, D., Vermeersch, S., Fabry, I., de Hoon, J., Van Bortel, L., Segers, P.: The use of diameter distension waveforms as an alternative for tonometric pressure to assess carotid blood pressure. Physiol. Meas. 31(4), 543–553 (2010)
Vermeersch, S.J., Rietzschel, E.R., De Buyzere, M.L., De Bacquer, D., De Backer, G., Van Bortel, L.M., Gillebert, T.C., Verdonck, P.R., Segers, P.: Determining carotid artery pressure from scaled diameter waveforms: comparison and validation of calibration techniques in 2026 subjects. Physiol. Meas. 29(11), 1267–1280 (2008)
Pereira, T., Cabeleira, M., Matos, P., Borges, E., Cardoso, J., Correia, C.: Optical methods for local pulse wave velocity assessment. In: 4th International Joint Conference on Biomedical Engineering Systems and Technologies, Rome, Italy, pp. 74–81 (2011)
Lamia, B., Chemla, D., Richard, C., Teboul, J.-L.: Clinical review: interpretation of arterial pressure wave in shock states. Crit. Care (London, England) 9(6), 601–606 (2005)
Kelly, R., Fitchett, D.: Noninvasive determination of aortic input impedance and external left ventricular power output: a validation and repeatability study of a new technique. J. Am. Coll. Cardiol. 20(4), 952–963 (1992)
Proudfoot, N.A.: The acute effects of moderate intensity exercise on vascular stiffness in children with repaired coarctation of the aorta (2009)
Jatoi, N.A., Jerrard-Dunne, P., Feely, J., Mahmud, A.: Impact of smoking and smoking cessation on arterial stiffness and aortic wave reflection in hypertension. Hypertension 49(5), 981–985 (2007)
Padilla, J.M., Berjano, E.J., Sáiz, J., Fácila, L., Díaz, P., Mercé, S., De Morelia, I.T., De Castellón, H.P., Electro, M.V.: Assessment of relationships between blood pressure pulse wave velocity and digital volume pulse. Comput. Cardiol. 33, 893–896 (2006)
Wilkinson, B., MacCallum, H., Flint, L., Cockcroft, J.R., Newby, D.E., Webb, D.J.: The influence of heart rate on augmentation index and central arterial pressure in humans. J. Physiol. 525(Pt. 1), 263–270 (2000)
Acknowledgements
The authors acknowledge the clinical collaboration from Dr. Rui Providência and Coimbra College of Health Technology, and acknowledge the support from Fundação para a Ciência e Tecnologia (FCT) for funding (SFRH/BD/79334/2011).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this paper
Cite this paper
Pereira, T. et al. (2014). Clinical Test for Validation of a New Optical Probe for Hemodynamic Parameters Assessment. In: Fernández-Chimeno, M., et al. Biomedical Engineering Systems and Technologies. BIOSTEC 2013. Communications in Computer and Information Science, vol 452. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-44485-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-662-44485-6_19
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-44484-9
Online ISBN: 978-3-662-44485-6
eBook Packages: Computer ScienceComputer Science (R0)