Abstract
The entire benign space-occupying lesions – either extra- or intraneurally located – are described here. The list of tumors consist of schwannomas (neurinomas), neurofibromas, plexiform neurofibromas, perineurioma, nerve sheath myxoma (neurothekeoma), haemangioma, fibrolipoma, and ganglia, whereby the latter ones can occur as extraneural or intraneural manifestations. Intraneural ganglion cysts are often manifested multiply within a special nerve segment. The importance and value of modern imaging concerning this kind of focal nerve lesion has of course to be outlined. Surgical aspects with regard to each tumor type are stressed as far as experience allows. The special difficulties that plexiform neurofibromas and perineuriomas present have to be pointed out if one is to consider surgical treatment. Concerning surgery of ganglion cysts, the importance of identifying and ligating a communication to the neighbouring joint is demonstrated and reinforced by specialist literature.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
13.1 Types, Symptoms, and Diagnosis
Most types of nerve tumor are characterized by the same slowly proceeding symptoms that we consider as typical of all the other previously mentioned focal neuropathies. Therefore, it normally takes several months to find the correct diagnosis and to differentiate from alternative neuropathies. Either the patient notices a focal swelling in his extremity not on a particular day, or eventually increasing symptoms give reason for imaging examination which leads to finding a tumor.
In the following, we restrict ourselves to benign space-occupying lesions either located extra- or intraneurally for which a revised overview was recently published in literature [1]. In all of these cases, the slowly increasing space-occupying effect on nerve axons causes the typical electric-current like paresthesias, in other words, the typical Tinel sign, which characterizes all kinds of focal neuropathies with partial or complete loss of axon continuity (see Sect. 4.1). The point where these sensations are felt most strongly indicates the location of degenerating and regenerating neuronal sprouts. First, patients repeatedly notice the location of their sensation, and then they sometimes observe something like a tumor mass which is movable transverse to the nerve course. Later, it becomes more and more sensitive.
Neurological deficits occur rather late. Unfortunately, electrodiagnostic testing is of subordinate value to find the diagnosis because it cannot reveal the correct pathology (see Chap. 5). However, imaging either as high resolution ultrasound or as magnetic resonance imaging is of superior value, and it should therefore be arranged in any case (see Sects. 6.1.7 and 6.2.7).
13.2 Surgical Considerations and Prognosis
The introduction of microsurgery has extended our surgical horizons in tumor cases. Results have massively improved so that it seems increasingly difficult to justify cases where the involved nerve is completely sacrificed. As to be expected, secondary nerve repair after nerve sacrifice achieves a lower functional level than a microsurgical primary procedure with preservation of unaffected nerve fibers (Fig. 13.1).
Therefore, surgery seems mandatory in all kinds of benign histology and solitary manifestation. In most of all cases, imaging findings are sufficient to define the entity as a benign one what will facilitate to decide to operate on. The question about solitary or multiple tumor occurrences in a limb can be solved more easily by means of ultrasound because MRI is technically restricted for certain limb segments. Because most nerve tumors are revealed as solitary, they have to be assessed as easily and primarily accessible; thus we should not hesitate to apply our microsurgical experience and remove the pathology completely.
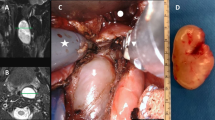
As a principle, the exposure of all kind of benign tumor first requires skin incisions large enough to identify the uninvolved nerve structure above and below the tumor. A few centimeters of the entering and exiting nerve segments should be visible, because the microsurgical procedure better starts from these healthy nerve segments. Its epineurium is longitudinally incised and perhaps partially removed so that a careful separation of fascicle groups is possible. The whole procedure is comparable to what we previously described in Sect. 7.1 as “interfascicular” neurolysis. Especially less experienced surgeons should make it a habit to start with these principles, because most of the fascicles and fascicle groups divide and disappear between the outer layers of the tumor sheath. These fibers are easier to identify and preserve when the surgeon arrives at the tumor mass with all fascicle groups in view from the beginning. They occur all over the whole tumor circumference. Under the microscope they can be carefully separated from the tumor and, sometimes, micro-scissors are needed for dissection. At the end, they remain preserved anatomically and functionally. When you finally return to the entering and exiting nerve segments, at least in cases of neurinomas, you will identify one fascicle or a small fascicle group from which the tumor originates. This small structure must be transected above and below the tumor so that you can take out the tumor and close the wound [2].
As the anatomically visible fascicular nerve pattern at different levels does not simultaneously correspond to a functional grouping, the sacrifice of the involved fascicle or fascicle group does not result in a noticeable neurological deficit. Mostly, nerve fibers from which a tumor originates have already lost their function during the growth of the tumor. The functional loss is then commonly pre-operatively compensated. It is therefore reasonable that the prognosis of most benign tumor surgery is extremely good provided the tumor addressed early enough and no other surgeon has previously tried to remove it macroscopically.
Special considerations are needed if structures of the brachial plexus, especially at trunk level, are involved. The nerve tissue differs from more peripheral nerve segments insofar as the typical inter-fascicular pattern is absent in favour of a mono- or bi-fascicular structure. We find fewer collagen fibers within plexus trunks, and a perineural layer which envelops several fascicle groups is lacking. Therefore, supra-clavicular nerve trunks have less resistance to surgical manipulation. Nevertheless, by means of all our microsurgical efforts, a complete removal of a solitary brachial plexus tumor is less difficult than perhaps expected [3].
To summarize on prognosis, the surgical principles described above can always be applied to neurinomas (schwannomas) which represent the most common nerve tumor occurrence in humans. Consequently, they have excellent prognosis, independent of their location.
Neurofibromas, however, differ insofar as the nerve structure from which they originate includes more fascicles, sometimes a whole fascicle group. Removal of such a tumor results in a slightly more functional sacrifice, but, nevertheless, its prognosis remains excellent [2].
In contrast to that, plexiform and multiple neurofibromas need quite another approach on prognosis than we would expect, taking into account the solitary tumors just mentioned [2]. The same holds true in rare cases of perineurioma, previously termed “local hypertrophic neuropathy” [4]. Both entities would theoretically need a complete nerve trunk resection and repair by grafts, but hardly any surgeon could bear responsibility for such a sacrifice.
Again, different comments on prognosis are needed in cases of intraneural multiple ganglia [5]. However, provided that microsurgical principles are kept in mind, the surgical prognosis is almost as good as for solitary neurinomas.
Special remarks on all benign nerve tumors will follow. It applies to all of these lesion types that a microsurgical step-by-step procedure remains the key to preserve the nerve function. Prognosis will then remain at a high level and independent of the availability of high-end diagnostic tools. Under magnification, the surgeon can, step by step, visualize all the details needed to decide and proceed correctly.
13.3 Special Comments on Different Tumor Types
13.3.1 Schwannomas (Neurinomas)
These tumors originate from Schwann cells of one single fascicle. Several manifestations within one nerve trunk may rarely occur, but then each time originate from another fascicle.
Imaging modalities are demonstrated in Figs. 6.10 and 6.20
Independent of the location, microsurgical removal always succeeds without any significant functional deterioration [2]. Even schwannomas of the brachial plexus in the supraclavicular area can be completely removed as described [3]. The surgeon then needs to remember that the fascicular pattern differs from nerve segments located in the periphery insofar as nerves at trunk level are mono- or bi-fascicular and with less collagen filaments inside. The challenge to microsurgical abilities is a little bit higher, but the prognosis to remove the tumor completely is excellent. A recurrence is only to be considered when fascicle involvement already starts at a very high level in the neuroforamen. These patients will need a follow up by MRI examination over the years and perhaps a second neurosurgical spine approach.
13.3.2 Neurofibromas
These tumors differ from schwannomas with regard to the histological pattern, and consequently, in some surgical aspects [2]. They are comparably encapsulated, but they originate from several fascicles or even some fascicle groups of the involved nerve trunk. Imaging modalities are shown in Fig. 6.21. At the end of the microsurgical neurolysis, not a small fascicle is found, usually several fascicles enter and exit the proximal and distal poles of the tumor. All these fibers have to be sectioned for tumor removal. Mostly, a numb skin area results, rarely a slight paresis which normally recovers within a few weeks.
Again, multiple manifestations within one or several nerve trunks are possible. They can sometimes be associated with a neurofibromatosis type I. Nevertheless, several and different surgical approaches are then necessary, because waiting deteriorates the prognosis; in association with a neurofibromatosis disease, there is a 15 % higher risk of malignant transformation so that a tumor removal would seem mandatory, particularly if its localization allows an easy approach [2].
13.3.3 Plexiform Neurofibromas
The term “plexiform neurofibromas” is used to describe a situation where multiple neurofibromas are localized within one circumscriptive nerve trunk segment. Each tumor has its own capsule, but all tumors can be surrounded by the nerve epineurium (see Figs. 6.11 and 9.7). Plexiform manifestations are more likely to be painful than solitary tumors. A complete removal would now need to sacrifice the whole nerve segment, and it would result in a paralysis [2]. Nerve repair as described in Chaps. 11 should theoretically follow, but patients commonly do not accept such a procedure without a guarantee that the function will return to that of the preoperative level. Patients today favour a conservative view and require a follow-up by imaging. If doing so, explicit information about the 15 % risk of malignant transformation is necessary when association with a neurofibromatosis exists [2]. These patients need strict imaging follow-up (Fig. 13.2).
When a surgeon unexpectedly comes across such a situation, he should longitudinally open the outer epineurium and stop the procedure. Such a careful decompression may diminish the patient’s radiating pain. Further action must be thoroughly discussed with the patient.
13.3.4 Perineurioma
These very rare benign peripheral nerve sheath tumors have only been included in the WHO classification system since 2000 [6]. Previously, the term “localized hypertrophic neuropathies” was used [7]. Unaware of nature of these tumors, trials of neurolysis were first reported. A complete nerve segment sacrifice with graft repair was then temporarily recommended [4]. Because of the irreversible muscle atrophy following extended waiting behavior this kind of surgery was even advised as an early procedure. But as the borderlines between tumor and healthy nerve segments could not be defined for sure – not even under high magnification – tumor resection seems to get again abandoned and neurolysis together with simultaneously clarifying the histology is preferred today [6]. Late cases, even with loss of spontaneous muscle activity in myography, should better be treated by reconstructive surgery if the type of functional loss is suitable for tendon transfer. We do not have sufficient information as to whether the tumor itself can then remain in place, because reliable long-time follow-ups are unavailable. Unfortunately, differential diagnosis by means of imaging remains challenging at present (see Sects. 6.1.7 and 6.2.7; Figs. 6.11 and 6.22).
13.3.5 Nerve Sheath Myxoma (Neurothekeoma)
A new benign entity in neuropathology consists of tumors of predominantly cutaneous or subcutaneous localization. They usually occur in the head and neck region, but also sometimes intra-spinally with relation to nerve roots [8]. Occasionally they can arise from peripheral nerves in the upper extremity. Nerve sheath myxomas are immunoreactive for S-100 protein and neuron-specific enolase. Neurothekeomas are not immunoreactive for S-100 protein, but their cells become stained after incubation with PGP9.5-antibodies. Ultra-structural observations and immunoreactions seem to confirm neuro-ectodermal origin.
We have no experience with behaviour and operability of these tumors. However, we were recently confronted with a 25-year-old patient who underwent removal of a nerve sheath myxoma in Guyon’s canal. Because he complained of severe functional deficits afterwards, hand surgeons advised an interosseous anterior nerve transfer onto the motor branch of the ulnar nerve in the palm [9]. He asked for a second opinion. As some single voluntary potentials could be derived from the adductor pollicis muscle, we warned against doing so.
13.3.6 Haemangioma
An intraneural cavernous haemangioma occurs extremely rarely, but it can be completely removed if microsurgical principles are applied as described at the beginning of this chapter [10]. A combination of neurinoma and haemangioma elements has been described, e.g. in 1978 [11], probably one of the entities termed “hybrid tumors” in 2012 [1].
13.3.7 Fibrolipoma
Fibrolipomas in the peripheral nerve are hamartomas, comparable to fibrolipomas of the intraspinal terminal myelon. They are detected in children and young adults, and they mostly involve the median nerve and its branches in the palm [12]. In about 30 % of cases they are associated with macrodactyly [13]. Patients with median nerve involvement commonly present with a carpal tunnel syndrome so that a surgeon can be unexpectedly confronted with such a tumor mass. The surgeon then should remember these rare hamartomas and should stop after carpal tunnel ligament transection. Each microsurgical trial destroys the nerve fibers such as in the myelon. The tumor has instead to remain in place for life.
Less frequently, fibrolipomatous involvement of other peripheral nerves of the upper extremity has been reported, such as in the radial nerve or the ulnar nerve (cited from [12]).
13.3.8 Ganglia
Focal neuropathies due to ganglia have the third position in terms of rate of occurrence of nerve-related tumors. They have a space-occupying effect, but they are no neoplasia. In contrary to this, they are cystic extraneural (Figs. 6.9 and 6.19) or even intraneural manifestations with hidden communication to a joint in the neighbourhood [5]. By the way, they have been well known for more than 110 years [14].
Extraneural manifestations have to be operated on by external “neurolysis” comparable to what we do for entrapment release. If possible, the communication to the neighboured joint should be ligated in order to avoid recurrence. Typical locations of occurrence are in the neighbourhood of the tibio-fibular joint with involvement of the common peroneal nerve, in the neighbourhood of the ankle with involvement of the tibial nerve in the tarsal tunnel, and in the neighbourhood of the elbow joint or wrist with involvement of the ulnar nerve. Rather rarely, the supraclavicular nerve is affected by single or multiple ganglia which communicate with the gleno-humeral joint. They can be punctured ultrasound guided (Fig. 13.3).
In contrast, single and multiple intraneural ganglia are a challenge for surgeons (see Figs. 6.12, 6.19, 9.19 and 9.20). Localizations of occurrence are the same as in the case of extraneural manifestations. The surgeon needs microsurgical equipment, and he has to apply all principles of “inter-fascicular neurolysis” over the whole involved nerve segment. Each cyst has to be evacuated only, and its membrane cannot be removed because it contains invisible nerve fibers. There is no argument to sacrifice the nerve at all. On the other hand, no cyst can be neglected in order to avoid persistence of the problem. The exposure therefore needs to be long enough. Nevertheless, a recurrence is sometimes possible as described in the literature because detection of the communication to the joint remains the main problem [5]. We remember a patient whose deep peroneal nerve branch was involved over the whole course. A recurrence came after a few months despite ligation of a communication to the tibio-fibular joint. He was treated by a posterior tibial tendon transfer to restore the partial foot drop described as a reconstructive alternative [15]. The multiple cysts were left in place. To summarize: intraneural ganglia need real microsurgery, cyst evacuation, ligation of the joint communication, and imaging follow-up perhaps once or twice.
References
Rodriguez FJ, Folpe AL, Giannini C, Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol. 2012;123(3):295–319.
Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg. 1994;81:362–73.
Lusk MD, Kline DG, Garcia CA. Tumors of the brachial plexus. Neurosurgery. 1987;21(4):439–53.
Gruen JP, Mitchell W, Kline DG. Resection and graft repair for localized hypertrophic neuropathy. Neurosurgery. 1998;43:78–83.
Spinner RJ, Atkinson JLD, Harper CM. Recurrent intraneural ganglion cyst of the tibial nerve. J Neurosurg. 2000;92:334–7.
Scheller C, Richter HP, Scheuerle A, Kretschmer T, König RW, Antoniadis G. Intraneural perineurinomas: a rare entity. Clinical, surgical and neuropathological details in the management of these lesions. Zentralbl Neurochir. 2008;69:134–8.
Kline DG, Hudson AR. Nerve injuries. Philadelphia: W B Sounders; 1995. p. 569–72.
Lee D, Suh YL, Han J, Kim ES. Spinal nerve sheath myxoma (neurothekeoma). Pathol Int. 2006;56(3):144–9.
Haas SC, Chung KG. Anterior interosseous nerve transfer to the motor branch of the ulnar nerve for high ulnar nerve injuries. Ann Plast Surg. 2002;49(3):285–90.
Kim JR, Seo JS, Kwon MS. Intraneural hemangioma of the median nerve. A case report. J Korean Soc Surg Hand. 2011;16(3):175–8.
Bojsen-Møller M, Spaun E. Peripheral nerve tumor composed of neurilemmoma and haemangioma elements. Acta Neurochir. 1978;40:299–305.
Toms A, Anastakis D, Bleakney RR, Marshall TJ. Lipofibromatous hamartoma of the upper extremity: a review of the radiologic findings for 15 patients. AJR Am J Roentgenol. 2006;186:805–11.
Gupta A, Geetha V, Monappa V, Bhat SS. Multiple neural fibrolipomas with macrodactyly. Indian J Dermatol. 2011;56(6):766–7.
Hardwell AS. Contributions from the Long Island Hospital Boston Harbour. Cystic tumor of median nerve: operation: restoration of function. Boston Med Surg J. 1901;144:582–3.
Penkert G, Fansa H. Peripheral nerve lesions. Berlin: Springer; 2004. p. 166–9.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Penkert, G. (2015). Nerve Tumors. In: Focal Peripheral Neuropathies. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-54780-5_13
Download citation
DOI: https://doi.org/10.1007/978-3-642-54780-5_13
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-54779-9
Online ISBN: 978-3-642-54780-5
eBook Packages: MedicineMedicine (R0)