Abstract
Neurilemmomas, also known as schwannomas, present as encapsulated, slow-growing, solitary, smooth-surfaced, and usually asymptomatic mass arising from Schwann cells of the nerve sheath surrounding cranial or peripheral nerves. They represent the most prevalent benign peripheral nerve sheath tumours and the occurrence in the upper extremity accounts for 12 to 19% and in the lower extremity for 13.5 to 17.5% of all cases. Schwannomas of the superficial peroneal nerve are very rare, and one can find in the literature only a few cases in the last 20 years. The smallest reported spinal giant schwannoma was of size 3 cm × 2 cm × 3 cm while the largest size reported of the same was 10 cm × 10 cm × 12 cm. We present a case report of a 54-year-old male with multiple huge ancient neurilemmomas arising from superficial peroneal nerve of 17 years’ duration. As the ultrasonography reported a hypoechoic mass in the left leg, antero-lateral muscular compartment with increased vascularity and magnetic resonance imaging (MRI) suggested large elongated lesion with multiple areas of haemorrhages; the primary diagnosis was made as vascular malformation. It was only after surgical exploration, three tumour masses were found arising from superficial peroneal nerve of sizes 15 × 6 cm, 2 × 2 cm, and 1 × 1 cm. The tumour was completely removed with meticulous dissection. Even though few fascicles of superficial peroneal nerve had to be sacrificed during excision, the patient recovered well with no neurological deficit.
Level of evidence: Level V, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Verocay first described neurilemmomas in 1910. [1] These are also known as schwannoma, neurinoma, which perineural fibroblastoma and are the most prominent benign peripheral nerve sheath tumours.[2,3,4] They come from the Schwann cells and are typically found in masses that are solitary, slow-growing, well-encapsulated, smooth-surfaced, and usually asymptomatic.[2] Typically, these tumours occur during the second to fifth decades of life, with women marginally more vulnerable than men.[5] While they constitute the most prominent tumours of the benign peripheral nerve sheath, only 1% of all cases arise in the lower limbs.[2] Exceptionally uncommon are occurrences of Schwannomas deriving directly from the superficial peroneal nerve.
Malignant transformation of neurilemmoma is rare, and the prevalence varies between 8 and 13.9%. [6] Ancient neurilemmomas are rare forms of these tumours. They are referred to as “old” because of the degenerative characteristics, such as cyst development, calcification, haemorrhage, and pronounced hyalinization obtained with increasing length. [7] We present a case study of a 54-year-old male with neurilemmoma stemming from a 17-year history of superficial peroneal nerve originally diagnosed as vascular malformation.
Case report
A 54-year-old male filed a case of swelling over the left leg side for 17 years. The swelling steadily grew in scale, initially painless later associated with occasional pain with a sudden increase in size and pain in 1 week. On clinical examination, a diffuse mass was present on the leg’s lateral aspect—smooth, firm in consistency with few areas of tenderness on palpation, and relatively immobile (Fig, 1). It was non-pulsatile without thrill and no bruit on auscultation. Distal pulsations were normal. The sensory and motor components were intact. The patient had no other co-morbidities, and his family history was non-significant. The blood investigations were within normal limits.
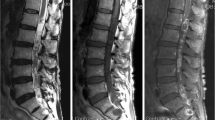
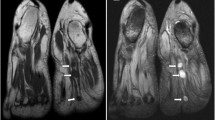
The patient underwent ultrasonography of the left leg, which showed two hypoechoic masses of size 13 × 5 × 3 cm, and 2.5 × 1.6 cm, respectively, located in the lateral intramuscular compartment. They exhibited increased vascularity and a few necrotic areas. MRI of the left leg reported multiple large elongated lesions in the lateral intramuscular compartment with haemorrhage areas, extending from the fibula’s head to the middle third of the leg and another at the lower end of the previous swelling, suggestive of vascular malformation (Figs. 2 and 3). The superficial peroneal nerve could not be delineated. Cardiovascular surgeons made a primary diagnosis of vascular malformation, and the patient was referred to the Department of Plastic & Reconstructive Surgery.
Despite the radiological diagnosis of a vascular malformation, the clinical presentation and examination findings pointed to a slow-growing, benign, possibly vascular tumour that might have had an episode of haemorrhage, causing the sudden exacerbation of symptoms.
After a thorough evaluation, the patient was planned to explore and excise the tumour mass under spinal anaesthesia. Sufficient written and informed consent has been received from the patient.
We approached the tumour through the zig-zag incision over the left leg’s lateral aspect under pneumatic tourniquet control. On exploration, three distinct masses were found in the left lateral compartment deep to the peroneus longus muscle—the largest being 15 × 6 cm and two smaller masses of 2 × 2 cm and 1 × 1 cm each at the lower end (Fig. 4). The largest mass was encapsulated, yellowish-grey, smooth to firm with few haemorrhage areas within, and peroneus longus muscle was stretched over it (Fig. 5). The mass was encompassing the superficial peroneal nerve stretched over its entire course and had few feeding vessels from the underlying muscles (Fig. 6).
Histopathology report showed yellowish-grey tissue mass along with multiple cystic areas and myxoid degeneration, suggestive of Neurilemmoma. Spindle cells with elongated nuclei were found, arranged in whorls and fascicles with Antony A and B patterns. The spindle cells surrounding the central acellular eosinophilic region of Verocay bodies and the tumour tissue also showed areas of myxoid degeneration, possibly due to its prolonged duration. There was no evidence of dysplasia (Fig. 7).
The post-operative course was uneventful. Although few fascicles of the superficial peroneal nerve had to be sacrificed, there was no neurological deficit, with sensory and motor functions found intact on follow-up (Fig. 8).
Discussion
Neurilemmomas have a preference for the head and neck, the posterior mediastinum, and the extremities. [1, 6] They are rarely located in the leg, foot, or ankle region. Those in the upper extremity account for 12 to 19% and lower extremity for 13.5 to 17.5% in all incidents.[8] The most commonly arise between the second and fifth decade of life with a 1.6:1 ratio of female to male. An ancient neurilemmoma is a rare form of these tumours with degenerative modifications.
These are typically solitary lesions but, in unusual instances, are multiple. [6, 7] It is believed that lesions are caused by Schwann cells’ proliferation, compressing, and displacing the surrounding nerve.[9] They are slow-growing and cannot move through the nerve sheath lying on top of it, which is why they are generally clinically silent and mostly appear as an accidental discovery. [2] Tumour size and position decide symptom severity. External pressure can cause tenderness and paraesthesia. They may experience radiating leg pain, leading to a differential diagnosis of entrapment neuropathy, chronic regional pain syndrome, lumbosacral radiculopathy, diabetic neuropathy, or tarsal tunnel syndrome.[5] In the present clinical situation, the lesion manifested as a painless slow-growing swelling with recent-onset pain associated with a rapid rise in size due to intra-lesional haemorrhage inducing nerve compression.
A clear understanding of the nervous network and the peripheral nervous system helps identify treatment approaches in people with peripheral nerve disorders. [2] Identifying a patient with a potential nervous tumour usually involves history, physical examination, and imaging procedures, including computed tomography (CT), magnetic resonance imaging (MR), in particular MR neurography, which can show a peripheral nervous tumour in more detail. [2] Surgical treatment should be cautiously considered with a view to retaining its purpose. [10] We performed a complete surgical resection of the tumour with meticulous dissection while maintaining the superficial perennial nerve and associated structures, resulting in a total cure as the underlying nerve suffered minimal damage.
These benign neural sheath tumours are uncommon in the lower extremities, according to the literature. Neurilemmomas can be included in the differential diagnosis of healthy nerve tumours over the lower limb. Imaging tests, particularly magnetic resonance, are beneficial, but a detailed clinical review should be emphasized. Intraoperative observations, along with histopathological results, include a conclusive diagnosis. Total surgical resection, thus maintaining the nerve results in recurrence and recurrence, is unusual. This case study, which describes several large ancient neurilemmomas’ clinical appearance at an infrequent venue, offers useful details on these cases in the literature.
References
Rathore AS, Srivastava D, Narwal N, Shetty DC (2015) Neurilemmoma of retromolar region in the oral cavity. Case Rep Dent 2015:320830
Nascimento G, Nomi T, Marques R, Leiria J, Silva C, Periquito J (2015) Ancient Schwannoma of superficial peroneal nerve presenting as intermittent leg pain: a case report. Int J Surg Case Rep 6C:19–22
Arabi H, Bakzaza O, El Fikri A, Elktaibi A, Saidi H, El Alaoui M (2016) Compression of the peroneal nerve by a neurofibroma originating from collaterals of the peroneal nerve: a case report. J Med Case Rep 10:28
Shariq O, Radha S, Konan S (2012) Common peroneal nerve schwannoma: an unusual differential for a symptomatic knee lump. BMJ Case Rep 2012:bcr2012007346
Kuo W-H, Wu C-H, Wang T-G (2012) Sonographic detection of knee neurilemmoma: a case report and literature review. J Med Ultrasound 20(2):125–128
Patil S, Babu K, Reddy S, Bandari D, Sudhaker G, Pranavi V (2014) Schwannoma of the superficial peroneal nerve in 12-year-old female child: a case report. Open J Orthop 04:189–193
Oz TT, Aktas B, Ozkan K, Ozturan B, Kilic B, Demiroglu M (2017) A case of schwannoma of the common peroneal nerve in the knee. Orthop Rev (Pavia) 9(1):6825
Gosk J, Gutkowska O, Urban M, Wnukiewicz W, Reichert P, Ziółkowski P (2015) Results of surgical treatment of schwannomas arising from extremities. Biomed Res Int 2015:547926
Shim S-K, Myoung H (2016) Neurilemmoma in the floor of the mouth: a case report. J Korean Assoc Oral Maxillofac Surg 42(1):60–64
Budohoski KP, Guilfoyle MR, Kenyon O, Barone DG, Santarius T, Trivedi RA (2018) Microsurgical resection of a common peroneal nerve schwannoma: a 3-dimensional operative video. Oper Neurosurg 14(1):83
Author information
Authors and Affiliations
Contributions
The outline and intellectual content were described by RP and KM. The manuscript writing and literature review was done KM and SN. Final review and critical appraisal were done by RP. The approval for the final version to be published given by RP. KM is accountable for all aspects of the work. All the authors have seen and approve the final version of the manuscript for the publication.
Corresponding author
Ethics declarations
Conflict of interest
All authors Rajesh S Powar, Kiran S Mahapure, and Saipriya Natrajan declare that they have no conflict of interest.
Ethical approval
This is a case report. The Institutional Ethics Committee has confirmed that no ethical approval is required.
Informed consent
Informed consent was obtained from the patient included in the study. The Patients signed informed consent regarding publishing their data and photographs without their name and identifying details.The participant has consented to the submission of the case report to the journal.
Consent for publication
Appropriate written and informed consent was obtained from the patient for publication of the clinical data after de-identification/removing the personal details.
Additional information
Prior presentation
The case report was presented as e-poster in 78th Annual Conference of the Association of Surgeons of India, ASICON 2018, Chennai.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Powar, R.S., Mahapure, K.S. & Natrajan, S. Multiple huge ancient neurilemmomas arising from superficial peroneal nerve: a case report. Eur J Plast Surg 44, 703–707 (2021). https://doi.org/10.1007/s00238-020-01774-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01774-1