Abstract
Urinary tract infection (UTI) is one of the most common bacterial illnesses in febrile infants younger than 60 days of age. It usually involves the upper urinary tract (pyelonephritis) and delay in therapy can lead to permanent renal damage. During early infancy, UTI is more common in boys, and uncircumcised males have the highest rates of UTI. The male-to-female ratio starts reversing by 4–6 months of age, and by 1 year of age, UTI is three times more common in girls than in boys. In febrile young infants, the diagnosis of UTI is made during sepsis evaluation as there are no specific symptoms or signs of UTI at this age. All febrile newborns <29 days of age and ill appearing 29–60 days old, undergoing sepsis evaluation (that must include urinalysis and culture), are hospitalized and treated with intravenous antibiotics until completion of sepsis work-up. Those with uncomplicated UTI are treated for 10–14 days and part of therapy can be completed with oral antibiotics as outpatient.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Urinary Tract Infection
- Renal Scarring
- Acute Pyelonephritis
- Asymptomatic Bacteriuria
- Febrile Urinary Tract Infection
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Case VignetteA 10-day-old male infant born to G1P1 mother at 35 weeks gestation (birth weight 1.93 kg) by cesarean section for non-reassuring heart tones is transferred from an outside hospital for the management of suspected sepsis. He had been inpatient at the outside facility for the management of hyperbilirubinemia and issues related with feeding. On the day of transfer, he had developed temperature instability and abdominal distension that was tender to touch. He had not been circumcised yet.
Initial laboratory evaluation revealed: hemoglobin 11.4 g/dL, WBC count 9,000, and platelet count 54,000/mm3. Serum chemistries revealed normal electrolytes and creatinine of 0.4 mg/dL. Spinal tap resulted in clear CSF under normal pressure, 14 cells/mm3 (22 % neutrophils), and normal protein and glucose levels; CSF culture remained sterile. Urinalysis revealed 2+ leukocyte esterase, negative nitrite, and 50–100 WBC and few bacterial rods per HPF. Blood culture and urine culture both grew E. coli. He was diagnosed with urosepsis and treated with IV cefepime for 21 days.
Imaging studies: Renal and bladder ultrasound revealed normal right kidney measuring 4.6 cm; left kidney measured 5.6 cm and showed moderate left hydroureteronephrosis (Fig. 9.1). Voiding cystourethrogram (VCUG) showed left grade IV VUR (Fig. 9.2). Initial 99mTc-DMSA scan revealed normal right kidney and multiple photopenic areas in the left kidney that were consistent with acute pyelonephritis (Fig. 9.3 Panel a). Four months later repeat 99mTc-DMSA scan showed persistence of photopenic areas on the left side suggesting scarring of the left kidney (Fig. 9.3 Panel b).
99mTc-DMSA scan of the patient described in the case vignette: (Panel a) at the time of admission showing multiple photopenic areas in left kidney consistent with acute pyelonephritis, and (Panel b) 4 months later there were no changes seen in the radiotracer uptake on the left side suggesting chronic renal damage (scarring). Split renal function was 72 % on right and 28 % on left side. It should however be noted that the possibility of left renal dysplasia associated with high-grade reflux on that side cannot be ruled out
Following completion of his initial antibiotic therapy, he was prescribed continuous prophylactic antibiotic therapy, initially cephalexin (10 mg/kg/dose twice daily) that was later changed to nitrofurantoin (2 mg/kg once daily), when he was 4 months old. At age 11 months, he developed another episode of urosepsis and his urine and blood culture grew Klebsiella pneumonia. The bacterium was resistant to both nitrofurantoin and sulfamethoxazole/trimethoprim. He was hospitalized and treated with intravenous ceftriaxone.
FormalPara Core Messages-
Initial episodes of urinary tract infection occur more commonly in infancy than at any other age, male newborns are at higher risk, and even more so those who are uncircumcised.
-
In young infants, fever is the only consistent symptom/sign of UTI and most of the UTIs are diagnosed during sepsis evaluation.
-
Even infants with another source of fever may still have UTI.
-
Urine specimen for culture should be obtained by either bladder catheterization or suprapubic aspiration.
-
Associated bacteremia is common but likely does not alter the outcome.
-
Total duration of therapy is 10–14 days and can be completed in part with oral antibiotics as outpatient.
-
Widespread application of prenatal ultrasonography has reduced the prevalence of previously unsuspected obstructive uropathy in infants.
-
The need to obtain VCUG and the role of prophylactic antimicrobial therapy after initial febrile UTI is being increasingly questioned, thus influencing the way we manage UTI, especially in infants older than 2 months of age.
9.1 Introduction
Urinary tract infection (UTI) is one of the most common bacterial illnesses in febrile infants younger than 60 days of age. It usually involves the upper urinary tract (pyelonephritis) and delay in therapy can lead to permanent renal damage. During early infancy, UTI is more common in boys, and uncircumcised males have the highest rates of UTI. The male-to-female ratio starts reversing by 4–6 months of age, and by 1 year of age, UTI is three times more common in girls than in boys. In febrile young infants, the diagnosis of UTI is made during sepsis evaluation as there are no specific symptoms or signs of UTI at this age. All febrile newborns <29 days of age and ill appearing 29–60 days old, undergoing sepsis evaluation (that must include urinalysis and culture), are hospitalized and treated with intravenous antibiotics until completion of sepsis work-up. Those with uncomplicated UTI are treated for 10–14 days and part of therapy can be completed with oral antibiotics as outpatient.
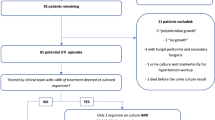
Over the last decade the management of children with a febrile UTI has become quite controversial. Conventionally, all children following an episode of UTI were investigated using renal ultrasound and voiding cystourethrogram (VCUG), aiming to identify renal anomalies, obstructive uropathy, and vesicoureteral reflux (VUR). Children with VUR of any grade were treated with prophylactic antibiotics, and surgical intervention was considered in those cases with breakthrough infections in spite of prophylactic treatment. This paradigm has been questioned in recent years by many investigators. Firstly, the widespread application of prenatal ultrasonography has clearly reduced the prevalence of previously unsuspected obstructive uropathy in infants; accordingly the yield of actionable findings revealed by renal-bladder ultrasound (RBUS) is relatively low (1–2 %) [2, 23, 25, 69]. Secondly, the most recent studies do not support the use of antimicrobial prophylaxis to prevent febrile recurrent UTI in infants without VUR or with grades I to IV VUR, thereby questioning the need for obtaining routine VCUG after the first UTI [10, 17, 37, 42, 48]. Accordingly, the American Academy of Pediatrics (AAP) recently published the newly revised guidelines on diagnosis and management of initial UTI in febrile infants and children 2–24 months of age [9]. It should be noted that the guidelines excluded infants <2 months of age, because of special considerations in this age group that may limit application of evidence derived from the studies focused on 2- to 24-month-old children. While the information in this chapter is mainly focused on infants <2 months, the material form of new AAP guidelines and other studies in older infants has been incorporated where appropriate.
9.2 Epidemiology
Initial episodes of urinary tract infection occur more commonly in infancy than at any other age [26, 66]. Infants with UTI typically present in the second week after birth, as UTI is an unusual occurrence during the first 3 days after birth [63]. In febrile infants, the reported prevalence of UTI has ranged from 4.1 to 9 % [5, 11, 47, 71]. In a recent meta-analysis of 14 articles that reported prevalence of UTI in febrile infants <24 months of age, the pooled prevalence of UTI was 7.0 % (CI: 5.5–8.4 %) [54]. The variability in prevalence is likely attributable to differences among studies in age, sex, and race of subjects; methods of urine collection; and criteria for the diagnosis of UTI. When analyzed for effects of gender and age, the meta-analysis found that prevalence rates were highest among uncircumcised male infants <3 months of age and females <12 months of age [54]. Four studies that reported UTI prevalence by race found that UTI rates were higher among white infants at 8.0 % (CI: 5.1–11.0) than among black infants 4.7 % (CI: 2.1–7.3) [54]. Among infants aged ≤2 months undergoing sepsis evaluation, the 4.6 % prevalence of UTI was fairly similar to 5.9 % in infants aged >2 months in whom UTI was suspected because there was no other source of fever. However, febrile infants with no apparent source of fever were twice (7.5 %) as likely to have UTI compared to those (3.5 %) with a possible source of fever such as otitis media [22]. Nevertheless the important lesson here is that even in infants suspected or found to have another source of fever, UTI may still coexist.
As mentioned before, in the first 6 months of life, more boys than girls present with UTIs and the incidence is greater in uncircumcised boys [68, 71]. Zorc et al. [71] reported on the clinical and demographic factors associated with UTI in febrile (≥38.0 °C) infants ≤60 days of age using a prospective multicenter cohort from eight pediatric emergency departments during consecutive bronchiolitis seasons. Overall, 9 % of the 1,025 infants were diagnosed with UTI and uncircumcised male infants had the highest rate (21 %), compared with females (5 %) and circumcised males (2.3 %). The odds ratio of UTI being associated with uncircumcised state was 10.4 (95 % CI 4.7–31.4).
9.3 Pathophysiology
UTI has multifactorial etiologies and represents an altered balance between the host and the pathogen (vide infra). As in many other diseases, biological susceptibility plays an important role in the cause of neonatal UTIs as, for instance, Lewis blood group negative children have higher incidence of UTI. Abnormal genitourinary anatomy can contribute to and complicate the clinical course of UTI. While hematogenous spread of bacteria to the urinary tract can occur, it is rare, and most UTIs start in the urinary bladder and then ascend to produce pyelonephritis. The ascent of infection to the upper tract can take place via two major mechanisms: (1) bacterial adherence properties that help them migrate upstream and (2) the presence of VUR that showers the renal pelvis with infected urine, thus allowing seeding of the renal parenchyma. If inflammation of renal parenchyma is not treated promptly, it can lead to tissue damage resulting in renal scarring.
9.3.1 Predisposing Host Factors
9.3.1.1 Vesicoureteral Reflux
The previously accepted concept that VUR is almost always the key factor in acquired renal injury secondary to a urinary tract infection is no longer accepted. This is based on the fact that less than half of the children who incur renal damage secondary to pyelonephritis have VUR; conversely, reflux itself does not cause UTI as many children with VUR diagnosed as part of evaluation of prenatally detected hydronephrosis never develop UTI. However, infants with VUR who get UTI are more likely to get pyelonephritis, and in the presence of VUR, less virulent bacteria can gain access to the upper urinary tract [34]. Furthermore, the risk of renal damage in children with high-grade VUR (grades III to V) is 4–6 times greater than the risk in those with grade I or II VUR and 8–10 times greater than the risk in those without VUR [29]. The relationship of VUR with UTI and renal damage has become more complex with the realization that some kidneys with high-grade reflux have elements of dysplasia and scarring even before any infection has been documented. In many of these cases, the parenchymal damage took place already in utero.
9.3.1.2 Innate Immunity
Despite its proximity to fecal flora, the urinary tract, with the exception of urethral meatus, is usually sterile. The precise mechanism by which the urinary tract maintains sterility is not well understood. A recent study has shown that ribonuclease 7 (RNase 7) is a novel antimicrobial peptide that is expressed in the human urinary tract and plays an important role in the innate immunity of the human uroepithelium [59]. Further studies are needed to see if alteration of this innate immunity plays a part in recurrence and severity of UTIs in certain individuals.
9.3.2 Agent Virulence
The most common bacteria infecting the urinary tract are usually Escherichia coli. The bacterial fimbriae mediate adherence to epithelial cells of the urinary tract and also cause agglutination of P-type red blood cells. Both these properties are important for bacterial virulence. The red blood cell agglutination can be blocked by sugars like mannose; therefore, mannose-resistant E. coli are more virulent than those that are mannose sensitive and predominate as pyelonephritogenic strains. Mannose resistance is mediated by P-fimbriae that recognizes specific carbohydrate receptors (Gal1–4 Gal) on the uroepithelium and can cause ascending infection in the absence of VUR [34]. K antigen is a capsular polysaccharide covering bacteria that shields them from phagocytosis and exists in greater quantities in pyelonephritogenic strains. Plos et al. [44] documented that children with UTI carry P-fimbriated E. coli in their fecal flora more often than healthy controls both at diagnosis (86 % vs. 29 %) and during infection-free intervals. The fecal carriage of P-fimbriated E. coli was also higher in children who were P-1 blood group positive (88 %) than those with P-2 blood group (40 %).
9.4 Microbiology
As in older children, the most common bacteria causing UTI in infants are Gram-negative bacteria belonging to the family Enterobacteriaceae, with E. coli being the most common pathogen. Other Gram-negative bacteria that are responsible for UTI include Klebsiella, Enterobacter, Citrobacter, Proteus, Pseudomonas, and Serratia species. Infection with Gram-positive organisms is less common and Enterococcus is the most common Gram-positive organisms isolated. Organisms such as Lactobacillus spp, micrococcus, diphtheroids, coagulase-negative staphylococci, and Corynebacterium spp are usually not considered clinically relevant isolates for otherwise healthy, 2- to 24-month-old children. The spectrum of the causative bacteria is usually similar regardless of whether or not the child has VUR [40].
9.5 Clinical Presentation
Symptoms of a febrile UTI are very nonspecific, particularly in young infants. Apart from fever, which is consistently present in infants with UTI, other nonspecific symptoms and signs such as vomiting, diarrhea, irritability, poor feeding, and jaundice, singly or in combination, may be present but cannot accurately predict the presence of UTI. Some authors recommend that UTI should always be included in the differential diagnosis of fever during the first year of life, even when a source of fever is unequivocal.
9.5.1 Focal Bacterial Nephritis
Focal bacterial nephritis also known as acute lobar nephronia affects one or more of the renal lobules and is an uncommon presentation of UTI [30, 62]. These patients may not have any pyuria. The diagnosis is suspected on imaging studies such as renal ultrasound (Fig. 9.4) and can be confirmed by computerized tomography in doubtful cases.
Renal abscess: this 3-month-old infant presented with high-grade fever of 1 day duration. Urinalysis was positive for leukocyte esterase and nitrites. Urine culture grew Citrobacter freundii (>10,000 CFU per mL); blood culture no growth. Renal ultrasound performed 2 days later revealed abscess in the superior pole of right kidney
9.6 Diagnosis
Urine culture from an appropriately collected urine specimen is the most important diagnostic test to establish the diagnosis of UTI. The results of urinalysis (dipstick and microscopic examination) are helpful but cannot substitute urine culture to document the presence of UTI. The physician managing young febrile infants must ensure that a urine specimen is obtained for both culture and urinalysis before treatment with an antimicrobial agent is initiated. The importance of this cannot be overemphasized, as a study conducted almost 20 years ago found that over half of the 1,600 pediatricians, family practitioners, and emergency medicine physicians surveyed reported that they would treat a highly febrile 4-month-old infant with an antibiotic without first obtaining a urine culture specimen [27]. It is the authors’ impression though that nowadays many more physicians, taking care of febrile infants, do obtain a urine culture before antimicrobial treatment is started.
9.6.1 Urine Collection Methods
The most common method of urine collection in older children and adults “midstream clean catch” is not practical in young infants, and bagged specimens are frequently contaminated with very high false-positive culture rates. Namely, a urine specimen obtained by urine bag is an acceptable method to rule out an infection but often an inadequate one to positively diagnose one. Therefore, and in order not to delay the start of antimicrobial treatment, bladder catheterization is the procedure of choice to collect urine for culture in febrile young infants. Less commonly, and especially in the newborn with urethral and other anatomic abnormalities of the external genitalia, suprapubic aspiration is indicated (vide infra).
9.6.1.1 Suprapubic Aspiration
Suprapubic aspiration of the bladder is the most reliable technique to identify bacteriuria that is uncontaminated by perineal flora. The technique is relatively simple and safe in young infants as urinary bladder is an abdominal organ at this age and not covered by peritoneum. The procedure should be performed in infants who have not voided in at least the hour prior to procedure and have a full bladder as assessed by palpation or percussion. One has to be very gentle during this examination as stimulation can initiate voiding. The suprapubic area is cleaned with an antiseptic solution, and a 1.5-inch, 22-gauge needle attached to a syringe is inserted perpendicular to the abdominal wall, approximately one centimeter above the pubic symphysis, and advanced under negative pressure until urine sample is obtained. The procedure can stimulate urination in many infants resulting in high failure rate. Reported success rates for obtaining urine by suprapubic aspiration have ranged from 23 to 90 % [12, 32, 45], with better results when the procedure is performed under ultrasonographic guidance [6, 19].
Despite its reported simplicity, suprapubic aspiration is associated with more pain than bladder catheterization and complications can happen [14, 31]. Minor complications such as microscopic hematuria are common, while major complications such as gross hematuria, intestinal perforation, and abdominal wall abscess are rare. As a result, suprapubic aspiration is rarely practiced outside the neonatal intensive care unit and is becoming a lost art. However, there may be no acceptable alternative to suprapubic aspiration in certain situations such as abnormalities of the external genitalia and urethra.
9.6.1.2 Bladder Catheterization
Transurethral bladder catheterization is a safe and effective method for obtaining urine samples for culture in most infants. The procedure is performed by observing all aseptic precautions. The infant is held with thighs in abducted (frog-leg) position. In uncircumcised boys the foreskin of the glans is retracted gently to permit complete visualization of the urethral meatus; the foreskin must be repositioned at the end of the procedure to prevent paraphimosis. The anterior urethra is cleansed thoroughly with povidone-iodine solution, and the penis is held perpendicular to the abdomen with the nondominant hand (which is henceforth considered contaminated) and gentle traction is applied to straighten the urethra. A 4- or 5-French catheter lubricated with sterile jelly is inserted through the urethral meatus with the dominant hand until urine returns. It is not uncommon to feel slight resistance as the catheter passes through the external bladder sphincter. This can be overcome by maintaining gentle pressure as the spasm will relax; the catheter should never be forced at this point. In female infants, the urethra may be difficult to visualize and an assistant is often needed to separate the labia majora. If the catheter is inadvertently placed in the vagina, it should be left in place to serve as a landmark for subsequent attempts.
The first few drops should be allowed to fall outside the sterile container, because they may be contaminated by bacteria in the distal urethra. Specimen contamination can occur in uncircumcised male infants and in female infants in whom the urethra is not well visualized and several attempts are required to pass the catheter.
9.6.1.3 Clean Voided Bag Specimens
While the noninvasiveness of this method of urine collection appeals to many physicians, nurses, and parents, this method should never be used for obtaining urine specimen for culture because of very high false-positive rates (vide infra). It should be noted that even if contamination from the perineal skin is minimized by cleansing, rinsing, and drying before application of the collection bag, there may be significant contamination from the vagina in girls or the prepuce in uncircumcised boys, the two groups at highest risk of UTI. Therefore, a “positive” culture result from a specimen collected in a bag cannot be used to document a UTI, and confirmation requires culture of a specimen collected through catheterization or suprapubic aspiration. Because there may be substantial delay in obtaining a second specimen, many clinicians prefer to obtain a definitive urine specimen through catheterization initially. However, if the clinician determines that the infant does not require immediate antimicrobial therapy, then often a urine collection bag affixed to the perineum can be used to collect urine specimen to rule out diagnosis of UTI by checking for leukocyte esterase and nitrites. To minimize the possibility of contamination, it is recommended that the mother checks on the bag every 10 min and that the bag is replaced by a new one every 30 min. As aforementioned, in essence a negative culture rules out a UTI whereas a positive one requires further confirmation.
9.6.2 Urinalysis
Because urine culture results are not available for at least 24 h, there is considerable interest in other urine tests that may be helpful in diagnosing those children who might have UTI thus enabling initiation of presumptive therapy. In contrast to urine specimen collected for culture, urinalysis can be performed on any specimen, including one collected from a bag applied to the perineum. However, the specimen must be fresh (<1 h after voiding with maintenance at room temperature or <4 h after voiding with refrigeration), to ensure sensitivity and specificity of the urinalysis. The tests that have received the most attention are biochemical analyses of leukocyte esterase and nitrite through a dipstick method and urine microscopic examination for white blood cells (WBCs) and bacteria.
9.6.2.1 Leukocyte Esterase
The test detects “esterase” (an enzyme released by white blood cells) and indicates presence of white blood cells in the urine (pyuria). Hoberman et al. [24] reported a sensitivity of 52.9 % in detecting the presence of ≥10 leukocytes/mm3. The specificity of this test in general is low; therefore, positive leukocyte esterase by no means confirms the diagnosis of UTI.
9.6.2.2 Nitrites
Dietary nitrates are converted to nitrites by bacteria, and positive urinary nitrite test has very high specificity (98 %) in diagnosing UTI. However, a nitrite test is not a sensitive marker of UTI in children, particularly infants, who empty their bladders frequently as conversion from nitrates to nitrites usually requires ~4 h of reaction time. Furthermore, only Gram-negative bacteria convert nitrates to nitrites; therefore, negative nitrite test results have little value in ruling out UTI [21].
9.6.2.3 Microscopic Examination
The diagnostic accuracy and the interpretation of microscopic urinalysis are influenced by the preparation of the specimen (centrifuged vs. uncentrifuged) and the method of quantifying and reporting. Stamm [61], defined pyuria as the presence of ≥10 leukocytes/mm3 in uncentrifuged urine. In young febrile children in whom urine specimen was obtained by catheterization, Hoberman et al. [24] showed that a count of <10 leukocytes/mm3 was almost invariably associated with a sterile culture, whereas a count of ≥10 leukocytes/mm3 had a sensitivity of 91 % and a low false-positive rate of 3.4 % in identifying urine culture results of ≥50,000 colony-forming units (CFUs) per ml. In urinary sediment from a centrifuged (10 mL at 2,000 rpm for 5 min) specimen, the usual threshold for significant pyuria is ≥5 WBCs per high-power field (∼25 WBCs per μL). The absence of pyuria can help differentiate true UTI from asymptomatic bacteriuria in infants with concurrent febrile infection from another source.
9.6.3 Urine Culture
“Significant” bacteriuria in urine culture has been the sole gold standard for the diagnosis of UTI. However, limitations of urine culture include uncertainty concerning the magnitude of a “significant” bacterial colony count, and inability to differentiate asymptomatic bacteriuria from infection. Urine culture results are considered positive or negative on the basis of the number of CFUs that grow on the culture medium. Definition of significant colony counts with regard to the method of collection considers that the distal urethra and periurethral area are commonly colonized by the same bacteria that may cause UTI; therefore, a low colony count may be present in a specimen obtained through voiding or catheterization even when bacteria are not present in the bladder urine. On the other hand, asymptomatic bacteriuria (≥106 bacteria/L in urine specimens obtained by suprapubic aspiration) has been reported in 0.9 and 2.5 % of female and male infants, respectively [65]. In majority of these infants, the bacteriuria is spontaneously cleared in a few months [64]. The concept that >100,000 CFUs per mL indicates a UTI was based on morning collections of urine from adult women, with comparison of specimens from women without symptoms and women considered clinically to have pyelonephritis; while the former had bacterial counts <10,000 CFUs per mL, women with pyelonephritis had ≥100,000 CFUs per mL with only 1 % of the women having bacterial counts between 10,000 and 100,000 CFUs per mL [28]. It is important to realize that definitions of positive and negative culture results are operational and not absolute. The time the urine resides in the bladder (bladder incubation time) is an important determinant of the magnitude of the colony count. Accordingly, in most instances, an appropriate threshold to consider bacteriuria “significant” in infants and children is the presence of at least 50,000 CFUs per mL of a single urinary pathogen in specimen obtained by catheterization [24]. For specimens collected by suprapubic aspiration, usually >1,000 CFU per mL of bacterial count is considered significant. As mentioned before, cultures of urine specimens collected in a bag applied to the perineum have an unacceptably high false-positive rate and are valid only when they yield negative results.
For urine culture results to be reliable, urine specimens should be processed as expeditiously as possible. If the specimen is not processed promptly, then it should be refrigerated to prevent the growth of organisms that can occur in urine at room temperature; for the same reason, specimens that require transportation to another site for processing should be transported on ice.
9.6.4 Blood Culture and Spinal Tap
In comparison to older children, UTI in infants is more commonly associated with bacteremia, occurring in 4–22.7 % of cases. Presence of bacteremia is inversely related to age and is usually limited to those <6 months old, and these patients are more likely to have abnormal RBUS and VCUG [4, 13, 43]. While blood culture is routinely obtained in all infants <29 days old as a part of sepsis evaluation, it should also be obtained in older infants who appear ill at initial examination. Presence of bacteremia might require prolonged intravenous antibiotic therapy but usually there are no adverse consequences in terms of outcome. In infants <3 months of age, the risk of coexisting bacterial meningitis with UTI is very low (<1 %) but sterile pleocytosis can be seen in up to 3 % of patients [52].
9.6.5 Miscellaneous Tests
The commonly obtained laboratory tests such as WBC count, C-reactive protein, and erythrocyte sedimentation rate (ESR) have not shown high degree of accuracy in confirming the diagnosis of acute pyelonephritis in young (<2 years old) febrile children with UTI [16]. Therefore, other special tests such as urine interleukin-1β and serum procalcitonin have been investigated and have shown promising results for early detection of acute pyelonephritis but currently remain a research tool [41, 55].
9.7 Management
9.7.1 Antibiotic Therapy
The goals of treatment of acute UTI are to eradicate the acute infection, to prevent complications, and to reduce the likelihood of renal damage. All febrile infants <29 days of age who usually undergo full sepsis evaluation (complete blood count with differential, blood culture, cerebrospinal fluid analysis with culture, and urinalysis with culture) are hospitalized, and treatment is initiated with broad-spectrum intravenous antibiotics such as ampicillin along with cefotaxime. It should be noted that bacterial susceptibility to antimicrobial agents is highly variable across geographic areas; therefore, initial therapy should be guided by local sensitivity patterns [18, 70]. Once the diagnosis of UTI is confirmed, the antibiotic is changed according to the culture results and treatment is continued for 10–14 days. While in the past, all newborns used to receive intravenous antibiotics for complete duration of therapy, currently, many of them are discharged home with PO antibiotic (usually cefixime) after variable length of inpatient intravenous therapy (Personal communication with Section of Infectious Diseases, Children’s Mercy Hospital, Kansas City, MO; 2012). The majority of infants without any underlying genitourinary abnormality will become afebrile within 48–72 h of therapy [3]. The length of intravenous therapy and hospital stay is determined by the severity of illness, non-E. coli UTI (e.g., Pseudomonas), presence of bacteremia, obstructive genitourinary anomaly, abnormal kidney function, response to therapy, and questionable parental compliance.
Most experimental and clinical data support the concept that delays in the institution of appropriate treatment of pyelonephritis increase the risk of renal damage [58, 67]. For these reasons, all infants who have sustained a febrile UTI should have a urine specimen obtained at the onset of subsequent febrile illnesses, so that a UTI can be diagnosed and treated promptly.
Older infants (1–3 months old) with UTI who are well appearing at initial examination, have no history of genitourinary abnormalities or previous UTI, are not dehydrated, have no respiratory distress or concomitant acute disease, were born at term, and do not have congenital heart, lung, or metabolic disease are at very low risk of adverse events and can be treated with brief hospitalization or ambulatory intravenous antibiotics followed by oral therapy [49].
Whether given to neonates or older infants, when aminoglycosides are used, it is important to monitor their blood level and concomitant kidney function, thus avoiding or detecting in its early stage acute kidney injury that is not uncommon in this patient population.
9.7.2 Prophylactic Antibiotic Therapy
Over the last decade, the practice of using prophylactic antibiotics in patients with VUR to prevent recurrence of febrile UTIs has been challenged. A number of studies in recent years have failed to show their usefulness in children older than 24 months with VUR grades I to IV [10, 17, 37, 42, 48]. The AAP subcommittee that worked on the 2011 Clinical Practice Guidelines requested the raw data on 2- to 24-month-old infants from six researchers and their analysis on this group of 1,091 infants failed to detect any significant benefit of prophylactic antibiotics in infants with grades I–IV VUR [9]. Accordingly, both National Institute for Health and Care Excellence (NICE) [39] and current American Academy of Pediatrics (AAP) guidelines recommend that prophylactic antibiotic treatment should not be routinely used. However, these recommendations are not applicable for infants <2 months of age and those with grade V reflux. The results of the currently ongoing RIVUR (Randomized Intervention for Children with Vesicoureteral Reflux) study may put an end to this debate.
Currently, due to the high risk of UTI recurrence at a young age (vide infra), it is our practice to keep all newborns and young infants, who had a UTI, with or without the presence of VUR, on prophylaxis for 6 months. Until age 2 months, the infants receive cephalexin to be replaced then by sulfamethoxazole/trimethoprim. Due to the high rate of resistance of community E. coli to ampicillin, which in some places reaches 50 %, it is important to avoid using this drug as first-line prophylaxis [1].
9.7.3 Circumcision
Uncircumcised male infants <2 months old have one of the highest incidence of UTIs; the impact of uncircumcised state on risk of UTI decreases by 1 year of age. A meta-analysis conducted by Singh-Grewal et al. [56] that included 402,908 boys showed that circumcision was associated with a significantly reduced risk of UTI (OR = 0.13, 95 % CI 0.08–0.20, p < 0.001). Because circumcision is not a benign procedure, these authors determined that the net clinical benefit of circumcision is likely only in boys at high risk of UTI such as those with posterior urethral valves or high-grade reflux. However, this assessment was critiqued by Schoen [50], who had earlier reported that newborn circumcision not only results in a 9.1-fold decrease in incidence of UTI during the first year of life but also markedly lowers the UTI-related costs and rate of hospital admissions, thus supporting newborn circumcision as a valuable preventive health measure, particularly in the first 3 months of life [51].
9.8 Imaging Studies
9.8.1 Ultrasound
The purpose of renal-bladder ultrasound (RBUS) is to detect anatomic abnormalities that might help in the management of current UTI and/or help plan further evaluation and long-term follow-up. In addition, RBUS also provides an evaluation of the renal parenchyma and an assessment of renal size that can be used to monitor renal growth. The widespread application of prenatal ultrasonography has clearly reduced the prevalence of previously unsuspected obstructive uropathy in infants and the yield of actionable findings is relatively low (1–2 %), thereby questioning the utility of RBUS in evaluation of the infant or child with a first febrile UTI [2, 23, 25, 69]. Furthermore, in the vast majority of those found to have an abnormal finding, no intervention was required. However the above studies did not pinpoint on the neonate population, and due to the possible association of UTI at this age with a missed congenital anomaly, the practice is still to obtain an ultrasound in neonates with UTI. Images of urinary bladder should always be included so as not to miss findings such as ureterocele or diverticulum (Fig. 9.5).
9.8.2 Voiding Cystourethrogram
The whole premise behind detecting VUR by VCUG is to prevent UTI recurrence (and renal damage) by prophylactic antibiotics or an antireflux procedure. Recent evidence has shown that VUR is neither necessary nor sufficient for the development of renal scarring, and many cases of scarring do occur in children without VUR. Furthermore, as the role of prophylactic antimicrobial therapy in preventing febrile UTI (and renal damage) in infants with grades I to IV VUR has become controversial, current AAP Clinical Practice Guidelines do not recommend obtaining VCUG routinely after the first UTI. The committee also concluded that the proportion of infants with grade V VUR among all infants with first febrile UTI is small (1 %) and these infants will likely show the abnormality on RBUS, prompting obtaining VCUG. Most nephrologists will usually obtain VCUG if renal and bladder ultrasound reveals significant hydronephrosis, solitary kidney, renal dysplasia or scarring, abnormal ureteral or bladder anatomy, suggestion of obstructive uropathy, and in other atypical or complex clinical circumstances. At the same time it is important to note that a normal ultrasound does not rule out the presence of VUR [57]. Because of the high prevalence of VUR in siblings (27.4 %) and offsprings (35.7 %) [57], VCUG may be indicated for infants with a family history of VUR. Although high-grade (IV–V) V VUR is less common [9, 38] than low-grade (I–III) VUR, identification of the former is important as it places these infants in high-risk category who are at greater risk of UTI recurrence and renal damage (Fig. 9.2). These infants should be closely monitored and investigated for UTI when they present with febrile illness.
9.8.3 Radionuclide Scintigraphy
Technetium-labeled dimercaptosuccinic acid (99mTc-DMSA) is taken up by the cells of the straight and convoluted parts of the proximal tubules and provides functional image of proximal renal tubular mass. Areas of inflammation, or those damaged by scarring, or areas with dysplasia are seen as focal defects associated with volume loss or contraction of the renal cortex (Fig. 9.3) [35]. A 99mTc-DMSA renal scan is highly sensitive in detecting the focal hypoperfusion and edema of acute inflammation (pyelonephritis) as well as subsequent scarring of inflamed parenchymal areas and is considered a “gold standard” for diagnosing pyelonephritis. This test is helpful in neonates and infants in whom the diagnosis is unclear based on the clinical findings. The findings on nuclear scans rarely affect acute clinical management and do not predict risk of future scarring; therefore, nuclear scanning is not recommended as part of routine evaluation of infants with their first febrile UTI. However, the 99mTc-DMSA scanning is useful in research, because it ensures that all subjects in a study have confirmed pyelonephritis to start with and it permits assessment of later renal scarring as an outcome measure.
9.8.4 Magnetic Resonance Urography
Magnetic resonance urography (MRU) is a relatively new technology that offers major advantages in evaluation of genitourinary abnormalities. It integrates exquisite anatomical information with a variety of functional data and avoids ionizing radiation and iodinated contrast agents [7]. Using DMSA scan as the reference standard, a gadolinium-enhanced T1 sequence MRU was found to have 100 % sensitivity and 78 % specificity for the detection of renal scarring [8]. In addition, MRU can distinguish among acute pyelonephritis (area of compromised perfusion with interstitial edema), renal scarring (parenchymal defect), and renal dysplasia [20]. However, at this point, its cost, limited availability, and need for patient sedation limit its widespread application.
9.9 Prognosis
9.9.1 Risk of Recurrence
A retrospective study from Finland revealed that roughly one-third of boys and girls who had their first episode of UTI under 1 year of age and were not receiving prophylactic antibiotics had recurrence of UTI over a follow-up period of 3 years; in 86 % of the cases the first recurrence occurred within 6 months of the primary UTI. The study excluded children with genitourinary abnormalities and none of the boys in this study were circumcised. It also found that the recurrence-free interval was shorter and recurrent UTIs occurred more often in children with grades III–V VUR than in those with grades I–II VUR (log rank test p = 0.0005) [40].
9.9.2 Risk of Scarring and CKD
In a study conducted 25 years ago it was estimated that each episode of febrile UTI can lead to a 5 % risk of new renal scar formation and risk of scarring increases with number of recurrences [26]. It is generally believed that the risk of renal parenchymal damage from UTI as manifested by subsequent renal scarring is strongly related to age at the time of UTI, being highest in infancy and declining markedly with age [46]. Several studies have reported an increased risk of scarring with delayed and inadequate treatment [15, 36, 67]. Hoberman et al. [23] reported on renal scan findings in 309 children (1–24 months old); 61 % of the children had findings compatible with acute pyelonephritis and renal scarring was noted in 9.5 % of the 89 % children who had repeat scans. The degree of VUR was significantly associated with a higher incidence of renal scarring (p = 0.007). Similarly, Montini et al. [38], reported changes of pyelonephritis on initial DMSA scans in 54 % of 300 children ≤2 years of age with scarring developing in 15 % of cases on repeat DMSA scans. A recently published meta-analysis of 33 articles that included 4,891 children (0–18 years old) revealed that 57 % (CI: 50–64) of children with first UTI had changes consistent with acute pyelonephritis on the acute-phase DMSA renal scan and 15 % (CI: 11–18) had evidence of renal scarring on the follow-up DMSA scan, 5–24 months after an initial episode of UTI. Children with VUR were significantly more likely to develop pyelonephritis (RR, 1.5; CI, 1.1–1.9) and renal scarring (RR, 2.6; CI 1.7–3.9) compared with children with no VUR. Furthermore, children with VUR grades III or higher were more likely to develop scarring than children with lower grades of VUR (RR, 2.1; CI, 1.4–3.2) [53]. On the other hand, it has been shown that children who have a normal ultrasound at presentation continue to demonstrate intact anatomy on follow-up studies irrespective of recurrence of UTIs [33]. It is also evident that the vast majority, if not all those who in the past where diagnosed with reflux nephropathy due to infection, sustained the renal parenchymal damage already in utero. Several studies indeed showed that UTI per se is not a frequent cause of chronic renal failure in childhood [60].
9.10 Conclusion
Many studies regarding UTI have been conducted on infants older than 30 or 60 days but there is only a paucity of such studies in the neonate. In general it seems agreeable by all that once appropriate urine sample is obtained, prompt antibiotic treatment should be provided, at least for several days by the intravenous route, and ultrasound of the urinary tract performed. Common sense should guide the need for a VCUG especially when taking into consideration the fact that only a minority of patients may benefit from long-term prophylaxis. On the other hand, a 6-month prophylaxis in all neonates recovering from acute UTI might be less invasive and more cost effective.
References
Alon U, Davidai G, Berant M et al (1987) Five-year survey of changing patterns of susceptibility of bacterial uropathogens to trimethoprim-sulfamethoxazole and other antimicrobial agents. Antimicrob Agents Chemother 31:126–128
Alon US, Ganapathy S (1999) Should renal ultrasonography be done routinely in children with first urinary tract infection? Clin Pediatr 38:21–25
Bachur R (2000) Nonresponders: prolonged fever among infants with urinary tract infections. Pediatrics 105:e59–e62
Bachur R, Caputo GL (1995) Bacteremia and meningitis among infants with urinary tract infections. Pediatr Emerg Care 11:280–284
Bauchner H, Phillip B, Dashefsky B et al (1987) Prevalence of bacteriuria in febrile children. Pediatr Infect Dis J 6:239–242
Buys H, Pead L, Hallett R et al (1994) Suprapubic aspiration under ultrasound guidance in children with fever of undiagnosed cause. Br Med J 308:690–692
Cerwinka WH, Kirsch AJ (2010) Magnetic resonance urography in pediatric urology. Curr Opin Urol 20:323–329
Chan YL, Chan KW, Yeung CK et al (1999) Potential utility of MRI in the evaluation of children at risk of renal scarring. Pediatr Radiol 29:856–862
Clinical Practice Guideline (2011) Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128:595–610
Craig J, Simpson J, Williams G (2009) Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med 361(18):1748–1759
Crain EF, Gershel JC (1990) Prevalence of urinary tract infection in febrile infants younger than 8 weeks of age. Pediatrics 86:363–367
Djojohadipringgo S, Abdul Hamid RH, Thahir S et al (1976) Bladder puncture in newborns: a bacteriological study. Paediatr Indones 16:527–534
Doré-Bergeron MJ, Gauthier M, Chevalier I et al (2009) Urinary tract infections in 1- to 3- month old infants: ambulatory treatment with intravenous antibiotics. Pediatrics 124:16–22
El-Naggar W, Yiu A, Mohamed A et al (2010) Comparison of pain during two methods of urine collection in preterm infants. Pediatrics 125:1224–1229
Fernandez-Menendez JM, Malaga S, Matesanz JL et al (2003) Risk factors in the development of early technetium-99m dimercaptosuccinic acid renal scintigraphy lesions during first urinary tract infection in children. Acta Paediatr 92:21–26
Garin EH, Olavarria F, Araya C et al (2007) Diagnostic significance of clinical and laboratory findings to localize site of urinary infection. Pediatr Nephrol 22:1002–1006
Garin EH, Olavarria F, Garcia N et al (2006) Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics 117(3):626–632
Gaspari RJ, Dickson E, Karlowsky J et al (2005) Antibiotic resistance trends in pediatric uropathogens. Int J Antimicrob Agents 26:267–271
Gochman RF, Karasic RB, Heller MB (1991) Use of portable ultrasound to assist urine collection by suprapubic aspiration. Ann Emerg Med 20:631–635
Grattan-Smith JD, Little SB, Jones RA (2008) Evaluation of reflux nephropathy, pyelonephritis and renal dysplasia. Pediatr Radiol 38:s83–s105
Hellerstein S, Alon U, Warady BA (1992) Letter. Urinary screening tests. J Pediatr Infect Dis 11:56–57
Hoberman A, Chao HP, Keller DM et al (1993) Prevalence of urinary tract infection in febrile infants. J Pediatr 123:17–23
Hoberman A, Charron M, Hickey RW et al (2003) Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med 348:195–202
Hoberman A, Winberg J, Roberts KB et al (1994) Pyuria and bacteriuria in urine specimens obtained by catheter from young children with fever. J Pediatr 124:513–519
Jahnukainen T, Honkinen O, Ruuskanen O et al (2006) Ultrasonography after the first febrile urinary tract infection in children. Eur J Pediatr 165:556–559
Jodal U (1987) The natural history of bacteriuria in childhood. Infect Dis Clin N Am 1:713–729
Jones RG, Bass JW (1993) Febrile children with no focus of infection: a survey of their management by primary care physicians. Pediatr Infect Dis J 12:179–183
Kass E (1956) Asymptomatic infections of the urinary tract. Trans Assoc Am Phys 69:56–64
Keren R (2007) Imaging and treatment strategies for children after first urinary tract infection. Curr Opin Pediatr 19:705–710
Klar A, Hurvitz H, Berkun Y et al (1996) Focal bacterial nephritis (lobar nephronia) in children. J Pediatr 128:850–853
Kozer E, Rosenbloom E, Goldman D et al (2006) Pain in infants who are younger than 2 months during suprapubic aspiration and transurethral bladder catheterization: a randomized controlled study. Pediatrics 118:e51–e56
Leong YY, Tan KW (1976) Bladder aspiration for diagnosis of urinary tract infection in infants and young children. J Singapore Paediatr Soc 18:43–47
Lowe LH, Patel MN, Gatti JM et al (2004) Utility of follow-up renal sonography in children with vesicoureteral reflux and normal initial sonogram. Pediatrics 113:548–550
Majd M, Rushton HG, Jantausch B et al (1991) Relationship among vesicoureteral reflux, P-fimbriated Escherichia coli, and acute pyelonephritis in children with febrile urinary tract infection. J Pediatr 119:578–585
Merrick MV, Uttley WS, Wild SR (1980) The detection of pyelonephritic scarring in children by radioisotope imaging. Br J Radiol 53:544–556
Miller T, Phillips S (1981) Pyelonephritis: the relationship between infection, renal scarring, and antimicrobial therapy. Kidney Int 19:654–662
Montini G, Rigon L, Zucchetta P et al (2008) Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, noninferiority trial. Pediatrics 122(5):1064–1071
Montini G, Zucchetta P, Tomasi L et al (2009) Value of imaging studies after a first febrile urinary tract infection in young children: data from Italian renal infection study I. Pediatrics 123:e239–e245
Mori R, Lakhanpaul M, Verrier-Jones K (2007) Diagnosis and management of urinary tract infection in children: summary of NICE guidance. Br Med J 335:395–397
Nuutinen M, Uhari M (2001) Recurrence and follow-up after urinary tract infection under the age of 1 year. Pediatr Nephrol 16:69–72
Pecile P, Miorin E, Romanello C et al (2004) Procalcitonin: a marker of severity of acute pyelonephritis among children. Pediatrics 114:e249–e254
Pennesi M, Travan L, Peratoner L et al (2008) Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics 121(6):e1489–e1494
Pitetti RD, Choi S (2002) Utility of blood cultures in febrile children with UTI. Am J Emerg Med 20:271–274. doi:10.1053/ajem.2002.33786
Plos K, Connell H, Jodal U et al (1995) Intestinal carriage of P fimbriated Escherichia coli and the susceptibility to urinary tract infection in young children. J Infect Dis 171:625–631
Pryles CV, Atkin MD, Morese TS et al (1959) Comparative bacteriologic study of urine obtained from children by percutaneous suprapubic aspiration of the bladder and by catheter. Pediatrics 24:983–991
Pylkkänen J, Vilska J, Koskimies O (1981) The value of level diagnosis of childhood urinary tract infection in predicting renal injury. Acta Paediatr Scand 70:879–883
Roberts KB, Charney E, Sweren RJ et al (1983) Urinary tract infection in infants with unexplained fever: a collaborative study. J Pediatr 103:864–867
Roussey-Kesler G, Gadjos V, Idres N et al (2008) Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol 179(2):674–679
Schnadower D, Kuppermann N, Macias CG et al (2010) Febrile infants with urinary tract infections at very low risk for adverse events and bacteremia. Pediatrics 126:1074–1083
Schoen EJ (2005) Circumcision for preventing urinary tract infections in boys: North American view. Arch Dis Child 90:772–773
Schoen EJ, Colby CJ, Ray GT (2000) Newborn circumcision decreases incidence and costs of urinary tract infections during the first year of life. Pediatrics 105:789–793
Shah SS, Zorc JJ, Levine DA et al (2008) Sterile cerebrospinal fluid pleocytosis in young infants with urinary tract infections. J Pediatr 153:290–292
Shaikh N, Ewing AL, Bhatnagar S et al (2010) Risk of renal scarring in children with a first urinary tract infection: a systematic review. Pediatrics 126:1084–1091
Shaikh N, Morone NE, Bost JE et al (2008) Prevalence of urinary tract infection in childhood. Pediatr Infect Dis J 27:302–308
Sheu JN, Meng-Chi C, Sun-Long C et al (2007) Urine interleukin-1β in children with acute pyelonephritis and renal scarring. Nephrology 12:487–493
Singh-Grewal D, Macdessi J, Craig J (2005) Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomized trials and observational studies. Arch Dis Child 90:853–858
Skoog SJ, Peters CA, Arant BS et al (2010) Pediatric vesicoureteral reflux guidelines panel summary report: Clinical Practice Guidelines for screening siblings of children with vesicoureteral reflux and neonates/infants with prenatal hydronephrosis. J Urol 184:1145–1151
Smellie JM, Poulton A, Prescod NP (1994) Retrospective study of children with renal scarring associated with reflux and urinary infection. Br Med J 308:1193–1196
Spencer JD, Schwaderer AL, DiRosario JD et al (2011) Ribonuclease 7 is a potent antimicrobial peptide within the human urinary tract. Kidney Int 80:174–180
Sreenarasimhaiah S, Hellerstein S (1998) Urinary tract infections per se do not cause end-stage kidney disease. Pediatr Nephrol 12:210–213
Stamm WE (1983) Measurement of pyuria and its relation to bacteriuria. Am J Med 75:53–58
Steele BT, Petrou C, DeMaria J (1990) Renal abscess in children. Urology 36:325–328
Visser VE, Hall RT (1979) Urine culture in the evaluation of suspected neonatal sepsis. J Pediatr 94:635–638
Wettergren B, Jodal U (1990) Spontaneous clearance of asymptomatic bacteriuria in infants. Acta Paediatr Scand 79:300–304
Wettergren B, Jodal U, Jonasson G (1985) Epidemiology of bacteriuria during the first year of life. Acta Paediatr Scand 74:925–933
Winberg J, Andersen HJ, Bergstrom T (1974) Epidemiology of symptomatic urinary tract infection in childhood. Acta Paediatr Scand 252(Suppl):1–20
Winter AL, Hardy BE, Alton DJ et al (1983) Acquired renal scars in children. J Urol 129:1190–1194
Wisewell TE, Hachey WE (1993) Urinary tract infections and the uncircumcised state: an update. Clin Pediatr 32:130–134
Zamir G, Sakran W, Horowitz Y et al (2004) Urinary tract infection: is there a need for routine renal ultrasonography? Arch Dis Child 89:466–468
Zhanel GG, Hisanaga TL, Laing NM et al (2005) Antibiotic resistance in outpatient urinary isolates: final results from the North American Urinary Tract Infection Collaborative Alliance (NAUTICA). Int J Antimicrob Agents 26:380–388
Zorc JJ, Levin DA, Platt SL et al (2005) Clinical and demographic factors associated with urinary tract infection in young febrile infants. Pediatrics 116:644–648
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Chadha, V., Alon, U.S. (2014). Neonatal Urinary Tract Infection. In: Chishti, A., Alam, S., Kiessling, S. (eds) Kidney and Urinary Tract Diseases in the Newborn. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-39988-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-642-39988-6_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-39987-9
Online ISBN: 978-3-642-39988-6
eBook Packages: MedicineMedicine (R0)