Abstract
Multiphoton laser microscopy or tomography associated to fluorescence lifetime imaging (MPT/FLIM) is an emerging noninvasive imaging method enabling an in vivo ‘optical biopsy’. Thanks to its spatial resolution similar to that of histopathology at high power magnification (<1 μm lateral, <2 μm) and to the possible use of colour coding of the fluorescence decay time, this technique enables the morphology of the tissue to be immediately recognizable. MPT/FLIM is particularly suited to study the ageing process of the dermis, enabling an in vivo distinction between collagen fibres and the elastotic material in the extracellular matrix of the dermis. It also holds great promise for increasing diagnostic accuracy of skin tumours. Thanks to the recognition of morphologic parameters and the study of fluorescence lifetime modifications in cancer cells, basal cell carcinoma (BCC) cells can be distinguished from normal keratinocytes, enabling both a diagnosis of BCC and the identification of tumour margins. Melanin-containing cells can be identified based on the short fluorescence lifetime decay characteristics of melanin. This contributes to the recognition of melanocytes in healthy skin and benign and malignant melanocytic lesions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Multiphoton laser microscopy or tomography (MPT) associated to fluorescence lifetime imaging (FLIM) is one among the very few noninvasive imaging methods enabling an in vivo optical biopsy. Thanks to its spatial resolution similar to that of histopathology at high power magnification (<1 μm lateral, <2 μm axial) [1] and to the possible use of colour coding of the fluorescence decay time [2, 3], this technique enables the morphology of the tissue to be immediately recognizable.
MPT is an optical imaging system that excites fluorescence from the tissue through the simultaneous absorption of two or more photons of infrared light [4]. Whereas for conventional confocal fluorescence microscopy, fluorophores are excited by absorption of individual photons in the visible or ultraviolet spectrum, MPT excitation entails the simultaneous absorption of two or more photons of longer wavelength. This process requires a high intensity of excitation light and is confined to the tightly focused excitation spot. The longer wavelength infrared radiation undergoes less scattering than visible light and can thus facilitate high resolution imaging deeper into biological tissue [1, 4–13].
MPT can exploit autofluorescence of intrinsic tissue fluorophores, i.e. naturally occurring molecules that can be imaged using MPT without the need for exogenous contrast agents. Fluorophores are integral components of the molecules to which they confer the characteristic autofluorescence. They include NADH (reduced nicotinamide adenine dinucleotide), NADPH (reduced nicotinamide adenine dinucleotide phosphate), flavines, keratin, melanin, elastin, collagen, porphyrin, tryptophan, cholecalciferol and lipofuscin [1, 4–13]. After energy absorption, fluorophores can then emit energy in turn, generating a visible signal at defined and characteristic wavelengths, different from those of absorption. The quantity and the wavelength of the emitted energy depend on the chemical characteristics of the fluorophore, on its environment and particularly on the type of the surrounding molecules [14–16].
Efficient MPT excitation usually requires ultrashort femtosecond laser pulses, which are also able to produce the nonlinear effect of second harmonic generation (SHG). The SHG signal comes from periodic structures such as collagen and is characterized by an emission wavelength corresponding to half of that of the incident photon; this particular signal allows the visualization of dermal collagen bundles and their distinction from cellular components and elastin fibres [1, 5, 6]. With MPT bidimensional images are acquired which correspond to optical sectioning parallel to the tissue surface (reported to a defined xy-plane). Pictures obtained at various depths, called z-stacks, can be acquired by sequentially modifying the depth of the focal plane in the tissue, reaching levels of 200 μm measured from the departure point at the skin surface [8, 10, 13]. Grey scale images are generated, reproducing the fluorescence intensity in different tissue components (Fig. 9.1a).
On the left (a), multiphoton tomography intensity image of healthy epidermis. In (b) pseudo-colour-coded fluorescence lifetime image of the same epidermal area, where red-coloured melanocytes, characterized by a short lifetime decay time, are well distinguishable from green-coloured keratinocytes with a medium lifetime value. Pseudo-colour scale: 0–2,000 ps
1 Excitation Wavelength
By modulating the excitation wavelength, different skin structures can be selectively excited, obtaining an enhancement of their morphology. When exploring the skin, a wavelength of 760 nm is first chosen for a proper imaging of epidermal structures [8, 10, 13]. When reaching the dermo-epidermal junction, the excitation wavelength has to be increased up to 800–820 nm, for selective melanin imaging. By this wavelength, most keratinocytes progressively become invisible. On the contrary, since melanin has an absorption spectrum that decreases from the UV region to NIR, with a selective excitation wavelength of 800 nm [17–19], melanin and melanin-containing cells (melanocytes and melanin-containing keratinocytes) will appear as single cells in the basal layer showing intense fluorescence. This characteristic can be employed to recognize melanocytes and melanin granules in cell cultures (Fig. 9.2).
Multiphoton tomography intensity images. Melanin imaging and excitation wavelength. In a melanocyte cell culture, by a 720-nm excitation wavelength (a), cells and melanin granules are not recognizable; (b) at 760 nm, both melanocytes and melanin granules are clearly visible; (c, d) by increasing the excitation wavelength to 780 and 800 nm, melanin granules are enhanced, but melanocyte bodies fade (c) and are not more visible (d)
A wavelength of 800 nm is generally employed to adequately visualize the extracellular matrix of the dermis. At this wavelength, collagen fibres that generate the SHG signal are selectively excited, whereas at 760 nm, dermal autofluorescent components such as elastin are enhanced in the image.
2 Fluorescence Lifetime Imaging
Fluorescence lifetime imaging (FLIM) is based on the measurement of the decay rate of the fluorescence signal following a short pulse of excitation light [11, 15, 19]. This represents an additional technique for use in combination with MPT (MPT/FLIM), further improving the understanding of skin morphology in detail. Further discrimination between fluorophores can be gained using multispectral FLIM, which is based on the analysis of multiple emission spectral channels [20–22].
Whereas MPT conventionally relies on the assessment of the intensity of endogenous fluorescence emitted by fluorophores in the skin, FLIM provides additional information based on the contrast generated by differences in the decay rate of the fluorescence intensity, not only providing morphological information but also a quantitative assessment of metabolic changes in living tissue. Since FLIM is immune to intensity artefacts, it enables a more robust numerical description of the images than intensity imaging [2, 20–22]. Images presented in this chapter are obtained by a FLIM system, developed jointly by the Photonics Group of the Imperial College of London and JenLab GmbH (Jena, Germany), which has been incorporated into the commercially available DermaInspect® (JenLab GmbH, Jena, Germany). The distribution of fluorescence lifetimes within an image is visualized through a histogram that plots the fluorescence lifetime (x-axis) against the number of corresponding pixels occurring at that lifetime (y-axis). Pseudo-colour images are generated, where each image pixel contains information about its fluorescence decay time corresponding to a specific colour. Thus, four dimensional data sets are generated, where the tissue is not only studied according to its structure in the x-, y- or z-axis but also according to the fluorescence dynamics of its components corresponding to different states or metabolic characteristics of the tissue [2, 20–22]. Besides essential information on fluorescence decay rates, false colour coding, enhancing image contrast and providing a more user-friendly visualization method permits the immediate identification of cellular, subcellular or extracellular structures in the image. As an example, when employing a 0–2,000 scale, keratinocytes, exhibiting fluorescence decay time values around 1,000 ps, are represented in the blue-green range, whereas melanocytes, with medium to short fluorescence decay time, are coded in the yellow-red range (Fig. 9.1b) [23]. Fluorescence lifetime scale intervals may be varied according to the need for enhancing particular structures or cells belonging to a certain typology or to identify subcellular particles. Figure 9.3 shows upper melanoma layers represented by two different scales. On the left, employing a 0–2,000 colour scale, melanoma cells are coloured red, corresponding to short-lifetime values, and this permits the immediate categorization into melanin-containing cells; on the right, short-lifetime values are expanded employing a 0–400 scale, enabling the enhancement of intracellular structures.
On the left (a), upper melanoma layers represented by a 0–2,000 ps pseudo-colour scale. Melanoma cells, displaying short lifetime values, are shown in orange and are immediately recognizable. On the right (b), a 0–400 ps scale is employed to increase the contrast inside cell components and to recognize the characteristics of the cytoplasm. Images presented in this chapter were obtained by a FLIM system, developed jointly by the Photonics Group of the Imperial College of London and JenLab GmbH (Jena, Germany), which has been incorporated into the commercially available DermaInspect® (JenLab GmbH, Jena, Germany) and were calculated using the software SPCImage (Becker & Hickl GmbH)
3 Application Fields
Cell Cultures. The MPT/FLIM technique has numerous applications in dermatology. Morphologic and metabolic characteristics of different cell types can be studied employing cell cultures, where isolated cells can be examined out of the tissue environment. Fibroblast cultures are widely used as an experimental model to study the expression of specific genes or the effect of drugs with potential chemotherapeutic activity and to check the mutagenicity and carcinogenicity of different substances. Using MPT/FLIM, a precise and rapid assessment of the morphologic and metabolic changes fibroblasts undergo after exposure to various environmental factors can be achieved without the need of cell processing and staining [24] (Fig. 9.4).
Healthy Skin and Skin Ageing. Healthy epidermis shows a homogenous distribution of cells which are divided by thin nonfluorescent intercellular spaces [7–13, 23, 25]. Since nuclei are deficient in autofluorescence signals, they appear as dark areas inside the fluorescent cytoplasm (Figs. 9.1a and 9.5). The stratum corneum shows strong keratin-based fluorescent hexagonal-shaped large flat cells. At a depth of about 20 μ from the skin surface, we find the stratum granulosum, where keratinocytes appear as large, oval cells with autofluorescence in the cytoplasm and dark nuclei. Melanin blotches inside the keratinocytes may be unique, involving a large part of the cytoplasm and sparing the nucleus, or may be organized in multiple spots, conferring a granular appearance to the keratinocyte. Sometimes the melanin blotch forms a cap over the nucleus, which is not recognizable because of the horizontal optical section of the sample. Stratum spinosum cell diameter decreases and cell density increases going more in depth towards the basal layer. At 50–100 μ from the skin surface, we find the basal layer with brightly fluorescent small polygonal keratinocytes and dark nuclei. At the dermo-epidermal junction, we find dark round/oval-shaped areas, interrupting the basal layer, corresponding to the top of the dermal papillae, where we can appreciate the presence of fibres [23].
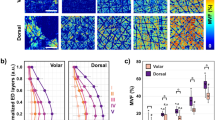
(a–c) Pseudo-colour FLIM stack of healthy epidermis. (a) Upper epidermal layers of a young subject, (b) lower epidermal layers, (c) dermo-epidermal junction and (d) upper epidermal layers in an elderly subject. In (a), keratinocytes show regular contours and intercellular distance, whereas in (d) cells present morphologic alterations and a shift of the fluorescence decay time towards higher values (blue-coloured keratinocytes)
The morphology and the metabolic states of healthy skin can be assessed in vivo, according to skin site and age. In fact, cell diameter and density vary according to epidermal cell depth and skin site [23]. In the elderly, epidermal cells show morphologic alterations, presenting irregular shape, size and intercellular distance and a decreased number at the basal layer (Fig. 9.5d). The modifications of the metabolic activities characteristic of the ageing process are reflected by variations in FLIM values, which increase at both the upper and lower layers in elderly subjects [23]. Further efforts are needed to increase knowledge on variations the epidermis undergoes according to environmental influences, for use as a reference for the study of different pathological conditions.
For the evaluation of the dermis, the excitation wavelength is switched to 800–820 nm. Two kinds of signals are generated by dermal fibres: autofluorescence signals from both collagen and elastin fibres and SHG signals from collagen fibres [6]. Separation of these signals can be accomplished by an optical filter that can be inserted into the beam path and which excludes the SHG component of the signal when exciting at up to 800–820 nm. When employing the filter eliminating the SHG signal, collagen fibres only contribute to the signal with their modest autofluorescence component, thus fading and enabling the recognition of fibres containing elastin. The latter appear as fine-curled fibres with a nonhomogeneous calibre (Fig. 9.6).
MPT/FLIM: pseudo-colour-coded fluorescence lifetime imaging (pseudo-colour scale 0–2,000 ps). Enhancement of elastin fibres by inserting a filter for SHG signals originating from collagen fibres. A nevus at a depth of –60 μ. (a) Collagen fibres (white arrows) appear as thick red filaments inside the dermal papillae; (b) after filtering SHG signals, elastin fibres appear as tiny blue (long-lifetime) filaments; melanocytes surround the papillae (triangle)
Skin ageing and pathological skin conditions of the dermis bring about morphological changes in the dermal collagen and elastin fibre network. During the ageing process, fibre tension and morphology and network pattern, as assessed by MPT, change [26]. Employing in vivo autofluorescence and SHG imaging, a relationship between morphological characteristics of human dermis assessed by MPT and age was demonstrated [27]. Investigating facial skin specimens from patients of different ages by MPT imaging, Lin et al. observed that in young individuals, autofluorescence and SHG signals are interspersed in the papillary dermis. Conversely, in the elderly, SHG signals can only be detected in the uppermost part of the dermis, whereas large amounts of fluorescent elastic fibres, corresponding to solar elastosis, are found in the dermis [28]. The trend of decreasing SHG signals and increasing autofluorescence signals is correlated with the histological findings of the decrease in collagen fibres and the increase in elastic fibres with increasing age.
MPT/FLIM is a procedure holding great promise for increasing diagnostic accuracy of skin tumours.
Basal Cell Carcinoma (BCC). BCC represents the most frequent skin tumour. Besides the diagnostic difficulties for superficial lesions which lack sensitive dermoscopic criteria, the identification of tumour boundaries, and consequently of the excision margins, represents practical problems in the daily dermatological routine. The use of MPT alone has already proved effective in identifying some diagnostic aspects of BCC. Investigating BCC specimens by MPT, histopathological features characteristic of BCC, such as elongated cells, nuclei polarization and peripheral palisading, can be recognized in the images [29, 30]. Lin et al. achieved a discrimination of BCC from normal dermal stroma by MPT imaging of formalin-fixed specimens of nine nodular type BCCs [31]. BCCs appeared as clumps of autofluorescent cells with large nuclei and peripheral palisading. By FLIM implementation and valuable information about time-resolved analysis of the fluorescence signal, further criteria are added for diagnostic purposes and tumour margin assessment. Using a multidimensional nonlinear laser imaging approach to visualize ex vivo samples of BCC, Cicchi et al. observed a blue-shifted fluorescence emission, a higher fluorescence response at 800 nm excitation wavelength and a slightly longer mean fluorescence lifetime in BCCs [32]. A wide-field (single photon excitation) study by Galletly et al. employing FLIM, imaged unstained excision biopsies of 25 BCCs with FLIM following excitation of autofluorescence with a 355 nm pulsed ultraviolet laser [3]. A significant reduction in mean fluorescence lifetimes between areas of BCC and those of surrounding uninvolved skin was demonstrated. Investigating BCC by MPT, Seidenari et al. identified specific descriptors, which were never observed in healthy skin but were present in all BCCs [30]. Further examination of BCC by MPT/FLIM revealed that some of these features correspond to traditional histopathological diagnostic criteria, such as aligned elongated monomorphous cells, peripheral palisading of tumour cells and typical tumour nests, whereas others, such as ‘blue cells’ and ‘phantom islands’, cannot be recognized in fixed and stained specimens (Fig. 9.7) [33]. ‘Blue cells’ correspond to basaloid cells showing fluorescence lifetime values higher than those of normal keratinocytes. The biological significance of the lifetime modifications in cancer cells is thought to be due to a shift from oxidative metabolism to glycolysis associated to variations in the amount of free and bound NADH [14]. Thus, FLIM imaging may represent a method to measure the oxidative stress and/or preferential metabolic pathway in living tissues [14]. ‘Phantom islands’ are generated by shifting the excitation wavelength to 800–820 nm. In this way, keratinocytes and BCC cells almost disappear, whereas the visualization of fibres is enhanced. Short-lifetime red (collagen) fibres tightly embrace the basaloid longer lifetime blue cell nests, corresponding to empty spaces (‘phantom islands’) (Fig. 9.7). Employing the MPT/FLIM technique, the separation between healthy skin and the tumour mass is achieved in all cases, making this technique a consistent tool for the definition of tumour margins.
Melanocytic Nevi. Common nevi, which are characterized by a proliferation of typical melanocytes, in single cells or in aggregates, are benign lesions which are clinically relevant as their appearance may be very similar to malignant melanocytic lesions. By MPT/FLIM, specific descriptors, referring both to cytology and architecture, enable their diagnosis [34]. Melanin-containing keratinocytes are recognizable in FLIM images as long-lifetime cells containing short-lifetime spots or blotches (red to yellow in the 0–2,000 ps pseudo-colour scale) characterizing melanin, whereas epidermal melanocytes in the upper and the lower layers appear as tiny short-lifetime cells, which are smaller than keratinocytes presenting a well visible small nucleus and homogeneously distributed melanin (Fig. 9.8a). At the dermo-epidermal junction level, the tips of the dermal papillae, appearing as roundish structures surrounded by a regular orange boundary of melanin-containing keratinocytes and melanocytes, are visible. ‘Edged papillae’ are characterized by a well-demarcated rim of orange cells surrounding a dark space containing fibres or cells, whereas ‘non-edged papillae’ lack a well-defined boundary (Fig. 9.9). Junctional nevus cell nests appear as aggregates of short-lifetime cells rising from the periphery of the papillae (Fig. 9.9). In compound nevi, short-lifetime ‘dermal cell clusters’ are also visible (Fig. 9.8b). By MPT/FLIM a regular architecture is generally observable in benign melanocytic lesions.
On the left (a), pseudo-colour-coded fluorescence lifetime image of upper layers in a nevus, where small red-coloured melanocytes, characterized by a short-lifetime decay time, are well distinguishable from large green-coloured keratinocytes with a medium lifetime value. The pseudo-colour scale employed to represent this picture ranges from 500 to 2,000 ps. On the right (b), a dermal melanocyte cluster in a compound nevus; blue elastin fibres are visible in the dermis
Selective melanin imaging and enhancement of collagen fibres by switching the excitation wavelength from 760 (a) to 800 nm (b). A nevus at a depth –60 m. Pseudo-colour scale: 0–2,100 ps. (a) By a 760-nm excitation wavelength, dermal papillae (white dots) are surrounded by red short-lifetime cells (melanin-containing cells), forming a junctional nest (arrow), whereas keratinocytes (white triangle) appear green. (b) By an excitation wavelength of 800 nm, melanin-containing cells maintain their visibility, whereas keratinocytes disappear. Inside the papillae, collagen fibres appear as thick red (short-lifetime) filaments
Melanoma. Melanoma (MM) is a lethal cancer. Despite a high cure rate for thin melanomas, advanced melanomas have a poor prognosis. Thus, early identification of melanoma represents a crucial end point for physicians. Due to its high resolution, MPT/FLIM holds a great potential for improving MM diagnosis [19, 35].
By MPT/FLIM, keratinocytes may not be recognizable at the superficial layers of a MM. When present, they are infiltrated by atypical melanocytes [36]. When displaying images by a 0–2,000 ps fluorescence lifetime range, MM cells appear orange to red, due to their short fluorescence decay time, and this immediately enables the determination of the melanocytic nature of the lesion (Fig. 9.3a). To increase contrast for the distinction of image details, a 0–400 scale is then applied (Fig. 9.3b). At the superficial level, atypical MM cells appear as large short-lifetime cells with a nucleus with undefined contours and a nonhomogeneous cytoplasm with speckled melanin. A peripheral cytoplasmic halo is often observable due to variable lifetime values of different cell areas (Fig. 9.3). Deeper MM layers show atypical short-lifetime cells smaller in size with respect to those observable on the surface; these are pleomorphic, variable in size and irregular in shape with a nonhomogeneous distribution. At this level, atypical short-lifetime cells may form aggregates or nests and may infiltrate dermal papillae and hair follicles. When dermal papillae are recognizable, these are not usually surrounded by a rim of regularly arranged melanocytes; they are irregularly sized and shaped and are separated by interpapillary spaces of different thickness. An architectural disorder is always visible. In MM metastases, besides atypical short-lifetime cells, long-lifetime (lacking melanin) cell nests are intermingled with long-lifetime (collagen) fibres (Fig. 9.10).
4 Advantages, Disadvantages and Future Objectives of MPT/FLIM
The morphology of MPT/FLIM images, acquired with a spatial resolution similar to that of histopathology at high power magnification, is extremely coherent with that of the histopathological analysis, suggesting that this new technique, once fully developed, may replace histology [1, 10].
Intensity images are visualized during the examination process in real time. FLIM images require a further elaboration to allow the operational system to develop a diagram of the fluorescence decay time and to produce a pseudo-colour image [3, 22]. Not only does MPT/FLIM generate high resolution images providing highly informative morphologic details but it also enables the study of the kinetics of the fluorescence decline and the calculation of the mean fluorescence intensity and lifetime values for selected areas of interest such as the cytoplasm of single cells, providing numerical data for an objective assessment of physiologic and pathologic skin conditions [2–4, 22]. The subcellular spatial resolution study of tissue samples in three dimensions is made possible by the acquisition of a sequence of horizontal optical sections (stack). Moreover, the nonlinear excitation produced by the NIR radiation allows a higher visualization of the deep dermis. The potential of this technique to provide an improvement in diagnostic accuracy is especially valuable for skin tumours, where an ‘optical biopsy’ enabling a diagnosis on the basis of both architectural and cellular morphology and numerical parameters is immediately available.
Long-term studies of cutaneous affections can be performed by the repetition of the in vivo examination on the same explored skin site within short or long intervals, considering that this technique has proved noninvasive [9].
On the other hand, the MPT/FLIM technique is at present unsuitable for continuous clinical use, since it presents some drawbacks consisting in a long acquisition/elaboration time of the images and the small field of view. Thus, important goals are both to reduce the acquisition time to avoid imaging deformities caused by voluntary and involuntary movements and to implement a device enabling the imaging of skin areas, large enough to be representative of the entire lesion.
Abbreviations
- BCC:
-
Basal cell carcinoma
- FLIM:
-
Fluorescence lifetime imaging
- MM:
-
Melanoma
- MPT:
-
Multiphoton tomography
- NADH:
-
Reduced nicotinamide adenine dinucleotide
- NADPH:
-
Reduced nicotinamide adenine dinucleotide phosphate
- NIR:
-
Near infrared
- SHG:
-
Second harmonic generation
- UV:
-
Ultraviolet
References
König K, Riemann I (2003) High-resolution multiphoton tomography of human skin with subcellular spatial resolution and picoseconds time resolution. J Biomed Opt 8(3):432–439
Elson D, Requejo-Isidro J, Munro I, Reavell F, Siegel J, Suhling K, Tadrous P, Benninger R, Lanigan P, McGinty J, Talbot C, Treanor B, Webb S, Sandison A, Wallace A, Davis D, Lever J, Neil M, Phillips D, Stamp G, French P (2004) Time-domain fluorescence lifetime imaging applied to biological tissue. Photochem Photobiol Sci 3:795–801
Galletly NP, McGinty J, Dunsby C, Teixeira F, Requejo-Isidro J, Munro I, Elson DS, Neil MA, Chu AC, French PM, Stamp GW (2008) Fluorescence lifetime imaging distinguishes basal cell carcinoma from surrounding uninvolved skin. Brit J Dermatol 159:152–161
Denk W, Strickler JH, Webb WW (1990) Two-photon laser scanning fluorescence microscopy. Science 248:73–76
Kollias N, Zonios G, Stamatas GN (2002) Fluorescence spectroscopy of skin. Vib Spectrosc 28(1):17–23
Zipfel WR, Williams RM, Christie R, Nikitin AY, Hyman BT, Webb WW (2003) Live tissue intrinsic emission microscopy using multiphoton-excited native fluorescence and second harmonic generation. Proc Natl Acad Sci U S A 100(12):7075–7080
Riemann I, Dimitrow E, Fischer P, Reif A, Kaatz M, Elsner P, König K (2004) High resolution multiphoton tomography of human skin in vivo and in vitro. SPIE-Proc 21–28
Schenke-Layland K, Riemann I, Damour O, Stock UA, König K (2006) Two-photon microscopes and in vivo multiphoton tomographs-powerful diagnostic tools for tissue engineering and drug delivery. Adv Drug Deliv Rev 58(7):878–896
Lin SJ, Jee SH, Dong CY (2007) Multiphoton microscopy: a new paradigm in dermatological imaging. Eur J Dermatol 17(5):361–366
König K (2008) Clinical multiphoton tomography. Review. J Biophotonics 1(1):13–23
Cicchi R, Sestini S, De Giorgi V, Massi D, Lotti T, Pavone FS (2008) Nonlinear laser imaging of skin lesions. J Biophotonics 1(1):62–73
Tsai TH, Jee SH, Dong CY, Lin SJ (2009) Multiphoton microscopy in dermatological imaging. J Dermatol Sci 56(1):1–8
König K, Raphael AP, Lin L, Grice JE, Soyer HP, Breunig HG, Roberts MS, Prow TW (2011) Applications of multiphoton tomographs and femtosecond laser nanoprocessing microscopes in drug delivery research. Adv Drug Deliv Rev 63(4–5):388–404
Skala MC, Riching KM, Gendron-Fitzpatrick A, Eickhoff J, Eliceiri KW, White JG, Ramanujam N (2007) In vivo multiphoton microscopy of NADH and FAD redox states, fluorescence lifetimes, and cellular morphology in precancerous epithelia. Proc Natl Acad Sci U S A 104(49):19494–19499
Sanchez WY, Prow TW, Sanchez WH, Grice JE, Roberts MS (2010) Analysis of the metabolic deterioration of ex vivo skin from ischemic necrosis through the imaging of intracellular NAD(P)H by multiphoton tomography and fluorescence lifetime imaging microscopy. J Biomed Opt 4:046008
Palero JA, Bader AN, de Bruijn HS, Der Ploeg van den Heuvel A, Sterenborg HJ, Gerritsen HC (2011) In vivo monitoring of protein-bound and free NADH during ischemia by nonlinear spectral imaging microscopy. Biomed Opt Express 2(5):1030–1039
Teuchner K, Freyer W, Leupold D, Volkmer A, Birch DJ, Altmeyer P, Stücker M, Hoffmann K (1999) Femtosecond two-photon excited fluorescence of melanin. Photochem Photobiol 70(2):146–151
Teuchner K, Ehlert J, Freyer W et al (2000) Fluorescence studies of melanin by stepwise two-photon femtosecond laser excitation. J Fluoresc 10:275–281
Dimitrow E, Riemann I, Ehlers A, Koehler MJ, Norgauer J, Elsner P, König K, Kaatz M (2009) Spectral fluorescence lifetime detection and selective melanin imaging by multiphoton laser tomography for melanoma diagnosis. Exp Dermatol 18(6):509–515
Becker W, Bergmann A, Biskup C (2007) Multispectral fluorescence lifetime imaging by TCSPC. Microsc Res Tech 70(5):403–409
Talbot CB, Patalay R, Munro I, Warren S, Ratto F, Matteini P, Pini R, Breunig HG, König K, Chu AC, Stamp GW, Neil MA, French PM, Dunsby C (2011) Application of ultrafast gold luminescence to measuring the instrument response function for multispectral multiphoton fluorescence lifetime imaging. Opt Express 19(15):13848–13861
Patalay R, Talbot C, Alexandrov Y, Munro I, Neil MA, König K, French PM, Chu A, Stamp GW, Dunsby C (2011) Quantification of cellular autofluorescence of human skin using multiphoton tomography and fluorescence lifetime imaging in two spectral detection channels. Biomed Opt Express 2(12):3295–3308, Epub 2011 Nov 10
Benati E, Bellini V, Borsari S, Dunsby C, Ferrari C, French P, Guanti M, Guardoli D, Koenig K, Pellacani G, Ponti G, Schianchi S, Talbot C, Seidenari S (2011) Quantitative evaluation of healthy epidermis by means of multiphoton microscopy and FLIM. Skin Res Technol 17:295–303
Rice WL, Kaplan DL, Georgakoudi I (2010) Two-photon microscopy for non-invasive, quantitative monitoring of stem cell differentiation. PLoS One 5(4):e10075
Seidenari S, Arginelli F, Bassoli S, Cautela J, French P, Guanti M, Guardoli D, Kӧnig K, Talbot C, Dunsby C (2012) Multiphoton laser microscopy and fluorescence lifetime imaging for the evaluation of the skin. Dermatol Res Pract 2012:810749
Koehler MJ, Preller A, Kindler N, Elsner P, König K, Bückle R, Kaatz M (2003) Intrinsic, solar and sunbed-induced skin aging measured in vivo by multiphoton laser tomography and biophysical methods. Skin Res Technol 15(3):357–363
Koehler MJ, Hahn S, Preller A, Elsner P, Ziemer M, Bauer A, König K, Bückle R, Fluhr JW, Kaatz M (2008) Morphological skin ageing criteria by multiphoton laser scanning tomography: non-invasive in vivo scoring of the dermal fibre network. Exp Dermatol 17(6):519–523
Lin SJ, Wu R Jr, Tan HY, Lo W, Lin WC, Young TH, Hsu CJ, Chen JS, Jee SH, Dong CY (2005) Evaluating cutaneous photoaging by use of multiphoton fluorescence and second-harmonic generation microscopy. Opt Lett 30(17):2275–2277
Paoli J, Smedh M, Wennberg AM, Ericson MB (2008) Multiphoton laser scanning microscopy on non-melanoma skin cancer: morphologic features for future non-invasive diagnostics. J Invest Dermatol 128(5):1248–1255
Seidenari S, Arginelli F, Bassoli S, Cautela J, Cesinaro AM, Guanti M, Guardoli D, Magnoni C, Manfredini M, Ponti G, König K (2013) Diagnosis of BCC by multiphoton laser tomography. Skin Res Technol 19(1):e297–e304
Lin SJ, Jee SH, Kuo CJ, Wu RJ, Lin WC, Chen JS, Liao YH, Hsu CJ, Tsai TF, Chen YF, Dong CY (2006) Discrimination of basal cell carcinoma from normal dermal stroma by quantitative multiphoton imaging. Opt Lett 31(18):2756–2758
Cicchi R, Massi D, Sestini S, Carli P, De Giorgi V, Lotti T, Pavone FS (2007) Multidimensional non-linear laser imaging of basal cell carcinoma. Opt Express 15(16):10135–10148
Seidenari S, Arginelli F, French P, König K, Magnoni C, Manfredini M, Ponti G, Talbot C, Dunsby C (2012) Multiphoton laser tomography and fluorescence lifetime imaging of basal cell carcinoma: morphologic features for non-invasive diagnostics. Exp Dermatol 21(11):831–836
Arginelli F, Manfredini M, Bassoli M, Dunsby C, French P, König K, Magnoni C, Ponti G, Talbot C, Seidenari S (2013) High resolution diagnosis of common nevi by multiphoton laser tomography and fluorescence lifetime imaging. Skin Res Technol 19(2):194–204
Dimitrow E, Ziemer M, Koehler MJ, Norgauer J, König K, Elsner P, Kaatz M (2009) Sensitivity and specificity of multiphoton laser tomography for in vivo and ex vivo diagnosis of malignant melanoma. J Invest Dermatol 129(7):1752–1758
Seidenari S, Arginelli F, Bassoli M, Dunsby C, French P, König K, Magnoni C, Ponti G, Talbot C. Multiphoton laser tomography and fluorescence lifetime imaging improve the diagnostic accuracy of melanoma. Submitted (in press)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Seidenari, S. (2014). Multiphoton Laser Microscopy and Fluorescence Lifetime Imaging for the Assessment of the Skin. In: Berardesca, E., Maibach, H., Wilhelm, KP. (eds) Non Invasive Diagnostic Techniques in Clinical Dermatology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-32109-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-642-32109-2_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-32108-5
Online ISBN: 978-3-642-32109-2
eBook Packages: MedicineMedicine (R0)