Abstract
In this chapter, a brief overview is provided of fission reactor-based epithermal neutron irradiation facilities designed for neutron capture therapy. The overview is intended to give those who are interested in establishing this type of facility some perspective and guidance concerning the desirable performance characteristics and features. Requirements for clinical BNCT are described in the Introduction together with a review of beam design studies. This is followed by a section describing two different approaches for producing an epithermal neutron beam for clinical BNCT and a description of currently available facilities. A state-of-the-art neutron beam facility is highlighted that satisfies all of the desired beam performance criteria and is capable of supporting more advanced clinical studies where higher patient throughput is needed. Existing reactor-based neutron irradiation facilities satisfy the needs currently anticipated for clinical research in BNCT while using proven and readily available technology. Some of these facilities possess many of the features of modern radiotherapy machines and employ modular designs to enable beamline modifications. This flexibility in beam delivery is needed to realize advances derived from future clinical accrual or translational research to develop improved methods for treating different tumors. Additional facilities can be constructed in the near term if needed by modifying available research reactors or by constructing small, ultrasafe reactors that are dedicated to BNCT.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
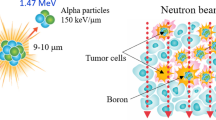
The principal objective of beam design for neutron capture therapy is to create a uniform distribution of low-energy (thermal) neutrons in the targeted treatment volume which may include a margin around the enhancing tumor as well as regions with suspected infiltrating disease. Buildup and broadening in the thermal neutron distribution are usually evident that are created as incident, higher energy neutrons slow down via elastic scattering interactions while passing through hydrogenous tissue. Tumor dose conformity is attained by thermal neutron capture in boron that is selectively targeted to the tumor and retained during irradiation. This binary strategy mitigates the need for complex tailoring of the beam spatial profile. The treatment volume can therefore be considerably larger than in conventional radiotherapy as the dose absorbed in normal tissue from the neutron beam itself is smaller than neutron capture in tumors containing boron. Neutron beams do require collimation to help avoid irradiating organs or other normal tissues peripheral to the field that may be radiosensitive or retain some of the administered boron. The adventitious dose whether from neutrons interacting with the constituents of normal tissue or boron retained in normal tissue should also be limited for critical organs both inside and outside the treatment volume. Judicious selection of the neutron beam characteristics helps to fulfill many of these aims. However, in a clinical setting, treatment planning calculations are performed to optimize tumor doses within the constraints of normal tissue dose limits by simulating various beam placements, aperture sizes, and even beam filtration options. Clinical trials in BNCT have thus far comprised mainly investigations into the safety and feasibility of this experimental modality, and the available clinical data are insufficient to fully optimize therapeutic beam delivery. Consequently, although certain neutron beam characteristics are known to be desirable, irradiation facilities must be versatile and able to adapt by making tradeoffs in beam characteristics as clinical experience is gained.
1.1 Beam Characteristics
A number of computational studies provide useful guidance on desirable characteristics for neutron beams used in BNCT [6, 9, 13, 39, 47, 53, 57–59]. More general requirements for NCT facilities have been outlined elsewhere [38], and fission reactor sources for NCT have been reviewed critically [20].
The earliest trials of BNCT employed low-energy thermal neutrons because these beams are relatively easy to create with virtually negligible unwanted fast neutron and gamma-ray contamination using a fission reactor. Thermal neutrons do not possess enough energy to penetrate deeply into tissue, and the absorbed dose profiles for the inherent, nonselective beam components therefore have maxima near the surface. These beams are therapeutically useful for superficial and relatively shallow tumors at depths of less than approximately 4 cm in tissue, depending on selectivity of the tumor boron uptake. In the earliest human clinical trials at Brookhaven (1951–1961) and at the Massachusetts Institute of Technology (1959–1961) [50], thermal neutrons were used for treatment of brain cancer, glioblastoma multiforme (GBM). Intraoperative NCT irradiations were used by Dr. W Sweet in these trials [16] because slow neutrons could not adequately penetrate to the tumor site, and this approach was subsequently continued in Japan under the leadership of Dr. H. Hatanaka [24].
Recognizing the benefit of external beam radiotherapy where deep-seated tumors (e.g., near the brain midline, approximately 8 cm deep laterally) are treated without the need to surgically reflect tissue and bone, researchers began to consider more energetic neutron beams that could achieve the desired buildup of thermal neutrons at depth in tissue. Intermediate energy or epithermal neutrons undergo moderation in tissue and produce improved thermal neutron distributions at significantly greater depths in tissue than is possible with slow neutrons. Optimizing the therapeutic parameters of beams for neutron capture therapy soon became a major subject of study in BNCT with particular emphasis on the neutron energy spectrum that is incident upon the patient.
Early studies on the effects of the incident neutron energy used Monte Carlo calculations to determine RBE-weighted depth-dose profiles along the central axis of a representative phantom and derive figures of merit collectively called advantage parameters that indicate relative performance in terms of tumor dose rate, therapeutic selectivity, and beam penetration [13]. These studies used geometrical phantoms of water or polyethylene to represent the clinical target volume and unidirectional as well as monoenergetic neutron beams or simplified energy spectra without contamination from unwanted neutrons or photons. Moreover, these optimizations were necessarily independent of other important parameters such as tumor size/location, boron uptake in tissue and tumor, beam/target size, collimation, and dose weighting factors. Indeed, increasing beam collimation as well as increasing aperture size relative to the target was found to significantly improve figures of merit by deepening penetration of the thermal neutron component [57]. Aperture size, collimation, and beam placement are also critical aspects for limiting dose to organs at risk in or near the treatment field and for minimizing patient whole-body exposure that can lead to secondary cancers or other radiation-induced injuries. As computational techniques advanced, more sophisticated multiparameter optimizations were undertaken to determine how factors such as tumor location or boron uptake influence the outcome of optimizations [6, 39]. These studies confirmed earlier results, indicating that a broad range of neutron energies from approximately 1 eV up to tens of keV are therapeutically advantageous for external beam NCT with the keV range appearing generally useful for a broad range of tumor depths and boron uptake. There does not appear to be a well-defined neutron energy range that is optimum for all therapeutic conditions envisioned. The optima are slowly varying and depend upon tumor location, size, normal tissue constraints, boron uptake, and other factors. Beams comprising a range of neutron energies are perhaps therefore most suitable for BNCT at this stage of development with flexibility incorporated into the beam delivery system to facilitate investigating new ideas derived from accrued clinical results.
As reactor-based NCT centers began to develop and implement resonance scattering filters that produce beams of epithermal neutrons, the necessary tradeoffs between beam intensity and purity from unwanted photons and neutrons rapidly became apparent. An epithermal beam intensity of 108 n cm2 s−1 results in a peak absorbed dose rate in brain of approximately 0.025 Gy min−1, and this was near the minimum feasible for beginning safety-related dose-escalation trials where peak brain doses of 8–10 Gy were specified. The kerma for epithermal neutrons in tissue is approximately 2 × 10−12 Gy cm2 [18], and restricting total beam kerma from unwanted photons as well as fast and thermal neutrons to less than 10 % of this (2 × 10−13 Gy cm2) is a desirable objective to avoid degrading therapeutic beam performance. The filtration needed to achieve this, however, significantly reduces beam intensity, and many facility designers instead found it necessary or practical to accept higher levels of contamination, recognizing that boron retained in normal tissue will also contribute to the nonselective dose. A study of measurements in 7 different clinical epithermal neutron beams found that when boron retention in normal tissue is 18 μg g−1 (as with boronated phenylalanine, BPA), further deleterious effects in beam penetration and therapeutic ratio occur only at relatively high contamination levels greater than approximately 3 × 10−12 Gy cm2. Significant degradation in the advantage parameters is, however, apparent for all but the lowest beam contamination levels when a very low amount of boron is retained in tissue, for example, less than 1 μg g−1 as with more advanced compounds currently under development [4].
1.2 Beam Monitoring and Control
Reliably and reproducibly administering the prescribed dose in external beam therapy requires a method for monitoring and integrating beam output while a radiation field is administered. In BNCT, most of the absorbed dose is derived from neutron interactions in tissue, and so a method is needed for monitoring neutrons transmitted by the beam. Uranium-lined fission counters are used in many systems [21, 41, 51] because they easily discriminate against the gamma rays inevitably contained in the beam and can be fabricated with the sensitivity necessary for sampling output in the epithermal energy range without significantly perturbing beam characteristics. Helium or boron gas-filled detectors are also a good choice for these reasons and have been used successfully at some clinical centers. These detectors are inherently sensitive to thermal neutrons, and it is therefore common practice to use a thermal neutron-absorbing shroud such as cadmium to reduce this response, which may arise from neutrons that backscatter toward the detector in either the collimator or patient. Gamma rays emitted by the beam itself sometimes comprise a nonnegligible portion of the absorbed dose in tissue, and beam monitoring systems may therefore contain either ionization chambers or Geiger-Müller detectors that are sensitive to gamma rays. In practice, since this dose component mostly derives from activation of beamline components, it is generally proportional to the neutron output of the beam, and the gamma-ray monitor is used only for informational purposes. The beam monitoring system is frequently equipped with a computer for displaying and archiving readings from the beam monitors throughout an irradiation.
The administered neutron fluence may also be monitored in situ by activation foils or wires usually comprised of gold that are inserted in the cavity remaining after surgical resection of the tumor [1, 27]. Activation foils are insensitive to gamma rays and for low neutron energies have an energy-dependent response very similar to that for neutron capture in boron. These measurements therefore accurately record the thermal neutron fluence in unresected tumor for individual patients, and this information can be used to determine absorbed dose. Since activation wires are integrating passive dosimeters, irradiations are frequently paused to remove the wire (or in some cases, the wire is remotely removed) for counting (measurement of the activation) that enables a determination of the remaining irradiation time. These measurements may also be augmented with small thermoluminescent dosimeters (TLDs) to measure the gamma-ray dose in situ. Although wires and TLDs may be affixed to the skin for monitoring external beam irradiations, this approach is most practical for intraoperative BNCT where detectors may be implanted near the tumor. Relatively long irradiations are required for this technique to ensure that there is enough time to complete the necessary measurements and determine the appropriate stopping time.
The precision and accuracy required for timing control in patient irradiations are inversely proportional to beam intensity. Irradiations using higher intensity beams are invariably shorter, and small errors in starting or stopping the irradiation become a relatively larger proportion of the administered field. As fields become increasingly short, on the order of minutes, an automated control system with safety interlocks is needed to help avoid human errors inadvertently causing a significant deviation from the planned exposure.
Various methods are used to control NCT beams, but fields are invariably based on integral beam monitor readings since beam output, although normally constant during an irradiation, is dictated by reactor operating conditions which can vary from day to day, especially at multipurpose reactors. Some research reactors such as the FiR-1 in Finland have a short beamline without much space for beam control shutters. This reactor is dedicated to BNCT research and beam output is controlled by manipulating reactor power. Beam output is not constant during the early part of these irradiations as the reactor gradually approaches full power, but this effect is taken into account by the beam monitors. Irradiations may be terminated rapidly by lowering reactor power or inserting all control rods to scram the reactor.
At facilities such as Petten and MIT, the reactor operates continuously for long period of time to service a variety of experimental needs, and it is not feasible to alter reactor power except in the case of an emergency. These facilities therefore employ a series of beamline shutters to turn the beam on and off, enabling free access to the medical room even when the reactor is at full power. Normally there is at least one beamline shutter that controls the irradiation by acting quickly enough so that the irradiation has a well-defined start and stop time.
1.3 Irradiation Facility and Patient Support
The experimental hall of most existing research reactors is enclosed by a containment building that is not easily penetrated or expanded and therefore represents a fixed boundary constraining the available space for constructing medical facilities. The epithermal beams used in NCT research require approximately 1 m of concrete shielding to keep ambient radiation levels low while the facility is in use, and this combined with space required for other experiments supported by the reactor often severely restricts the available options for NCT irradiation and patient support facilities. Design of the medical irradiation room is most important to mitigate constraints inherently imposed by the fixed beamline by providing enough space to accommodate staff and equipment as well as flexibility to orient the patient in any direction for fields on any part of the body. An area outside the therapy room to accommodate equipment for beam monitoring and control is also needed, and this space must be large enough for beam operators as well as responsible medical personnel to monitor the patient. Each of these components (including the shielding walls) must be carefully sized so as to avoid adversely impacting their functionality while meeting available space constraints. Other important facilities such as simulation setup areas or examination and observation rooms for pre- and postirradiation procedures although ideally located near the therapy room can be accommodated outside the containment building where space constraints are less severe.
Layout inside the therapy room is dictated by the fixed and usually horizontal beamline which ideally is centered in the room some distance from the entrance to avoid complications from entering and exiting traffic. A beamline about waist high above the floor is a comfortable working position for staff and is easiest for patients getting on and off the therapy table. Relatively short patient-to-aperture distances of a few cm or less are used in BNCT because these beams spread significantly in air, except at Petten where the beam is highly collimated and an air gap of 30 cm does not adversely affect beam characteristics. In the former cases, patient positioning is made easier by bringing the beam into the room through a cone-shaped collimator that affords space near the aperture to orient the patient at any angle to the beam. This is also convenient because the collimator is then readily accessible from inside the medical room so that differently sized or shaped apertures can be easily implemented. A photograph from the Harvard-MIT clinical trials is shown in Fig. 2.1 where the long protruding collimator is used to set up a lateral field irradiation with a small air gap of 3 cm.
Wall and ceiling mounted lasers to illuminate the beam central axis enable using field setup practices developed for conventional radiotherapy, and this improves patient comfort by making setup easier and more efficient. Axial back pointing and beam’s eye view lasers as implemented in the MIT therapy room are also useful for confirming beam entry or exit that may be used as a reference in treatment plans. At the FiR-1 reactor in Finland, a mock-up of the beamline with a specially designed docking couch is used to pre-position the patient outside the therapy room where more space is available. Once the patient is in place, the couch may be moved into the therapy room and accurately positioned using a matching dock and coordinate settings on the couch [29].
Two-way audio communication between the control console and therapy room is important for both operational convenience and safety so that staff may easily communicate and monitor the patient during irradiations. Visual monitoring is similarly important, and this is often done via closed-circuit television. Some facilities are also equipped with a shielded window which is not susceptible to electric power failure and helps reassure the patient with a view to outside the room.
1.4 Summary
This section described epithermal neutron irradiation facilities using fission reactor sources, which together with currently approved boron delivery drugs can attain useful therapeutic effect for tumors up to approximately 9-cm depth in soft tissue. The following characteristics and capabilities are recommended for future NCT facilities to enable efficient and productive clinical studies as well as more routine clinical use where higher throughput may eventually be needed:
-
1.
High intensity to facilitate delivering radiation fields in several minutes as is normally done with conventional photon therapy. Short irradiation times also enable better temporal targeting of the beam during the optimum boron pharmacokinetic window that may be relatively brief. Additional beam intensity is invaluable for improving other beam parameters such as collimation, purity, or energy filtration that may eventually prove advantageous and which will inevitably reduce beam output. Short irradiation times also significantly improve patient comfort and reduce the need for rigid restraint to keep the patient properly positioned.
-
2.
The neutron beam purity and energy spectrum should achieve a therapeutic ratio greater than unity up to and beyond 9-cm depth using a boron delivery drug like BPA where tissue and tumor uptake is approximately 18 and 65 μg g−1, respectively.
-
3.
Well-collimated beams, with an accessible portion of the beamline near the patient, and a wide range of apertures is desirable. This will afford flexibility in treatment planning for a variety of treatment sites using multiple beam placements, in an effort to optimize tumor dose while restricting dose to sensitive organs in the field and keeping whole-body exposure acceptably low.
-
4.
A large (approximately 9 m2 or larger) shielded medical irradiation room with a long, protruding beam snout, or patient collimator, eases patient setup and enables comfortably placing beams for any envisioned tumor site. Figure 2.1 illustrates the use of a long patient collimator during a lateral brain irradiation at the MIT FCB.
-
5.
The NCT irradiation facility should be able to operate reliably with high capacity factor and, if needed, 24 h/day and 7 days/week.
-
6.
Systems for observing, monitoring, and communicating with the patient inside the medical therapy room are necessary.
-
7.
An automated beam monitoring and control system which ensures accurate dose delivery by precisely monitoring beam output with interlocks to help assure safety of both patients and staff is essential.
-
8.
A system for conveniently positioning the patient and aligning the planned irradiation fields is important.
Specific parameters based on these criteria for epithermal neutron irradiation facilities are summarized in Table 2.1. Reactor-based epithermal neutron facilities are able to meet or exceed these first-order requirements and thereby help advance clinical research in BNCT. A few facilities presently fulfill all of these criteria, and several others satisfy most except, for example, intensity or contamination. Regardless of the parameters, each facility used in clinical BNCT plays an important role by accruing valuable information that is needed to develop this modality. Clinical experience gained with the beams available today is needed to guide future designs or modifications and to help judge the relative importance of various beam parameters for sustaining or possibly improving clinical performance. Most BNCT irradiation facilities available today are suitable for this purpose, and the best are able to accommodate more advanced clinical implementations where significantly higher patient throughput is needed.
The following sections discuss two different approaches for using fission reactors as sources for epithermal neutron-based NCT. The performance of current reactor-based epithermal neutron facilities is described, illustrating how they satisfy the operational characteristics outlined above, followed by a section on a state-of-the-art epithermal irradiation facility as well as a concluding summary.
2 Approaches to Using Reactors for Epithermal Neutron NCT
In the past, neutron beam facilities for NCT have not generally been part of the original design specifications for research or test reactors. The two exceptions are the Massachusetts Institute of Technology Research Reactor (MITR) [52] and the now decommissioned Brookhaven Medical Research Reactor (BMRR) [17], both of which were commissioned in the 1950s when interest in testing the concept of BNCT initially developed. The NCT facilities at these reactors were designed specifically for thermal neutron NCT and were used in the early clinical studies during the 1950s. During the 1990s, Brookhaven [32] and MIT [46] each constructed epithermal neutron beams at these reactors that were subsequently used in more recent trials of BNCT. More recently, a new, small (30 kW) reactor specifically designed for NCT has been constructed near a hospital site in Beijing, China [19]. This is the first reactor constructed specifically for BNCT since the 1950s and may become the first modern facility suitable for hospital siting.
Research interest in BNCT grew rapidly in the 1990s, and as the feasibility of external beam irradiations became clear, a significant number of research or test reactors were modified to incorporate epithermal neutron beams. The most common approach for retrofitting these reactors is to use the reactor core directly as the source for the epithermal neutron beam [2, 7, 11, 12, 33, 35, 37 40, 46, 49 48]. Reactors ranging in power from 100 kW to several MW have been successfully converted using this approach. Examples include the low-power (250 kW) Finnish reactor FiR-1 [2], the 1 MW Washington State University Reactor [40], and the high-power (45 MW) test reactor, HFR, at Petten [42]. Small, low-power ultrasafe reactors could also be built to obtain high-performance epithermal neutron beams using designs that are specifically optimized for BNCT. These reactors would require only 100–300 kW of fission power because core neutrons could be used directly as a source for the epithermal neutron beam. Several preliminary designs have been proposed for this type of special purpose reactor [30, 31]. These special purpose NCT reactors could be expected to meet the requirements for clinical investigations of BNCT as well as more routine clinical treatments.
Another approach to modifying existing reactors for epithermal NCT is to use a subcritical array of fuel called a fission converter originally proposed by Rief et al. [43] that is located outside the reactor core and driven by thermalized neutrons from the moderator. The first such facility, known as the fission converter beam (FCB), was constructed at the MITR [22, 23, 25]. A few other fission converter-based beams have been designed, one for the 3-MW BMRR [32] and another for the 2 MW McClellan Air Force Base Reactor [34]. A fission converter is particularly appropriate for higher power or multipurpose research reactors without a movable core that support a broad range of experiments. These reactors cannot accommodate frequent power changes or shutdowns that are used for beam control at some low-power facilities without integrated beamline shutters. Moreover, due to the large number of experimental stations at some reactors, it is often impractical or impossible to install a medical room near the reactor core to attain the necessary epithermal neutron flux. A fission converter could be incorporated into the initial design of a multipurpose research or test reactor to help accommodate the desired experimental facilities. Whether using a fission converter or the reactor core directly, careful consideration of the NCT facility during the initial reactor design should generally result in better and less expensive facilities than those made by retrofitting existing reactors.
3 Performance of Some Current Epithermal Neutron Irradiation Facilities
Table 2.2 summarizes parameters and figures of merit published for most epithermal neutron beams that have been used in NCT clinical trials together with pertinent details about the corresponding irradiation facilities. The figures of merit are described in detail elsewhere [14] and are good first-order indicators of beam performance. More sophisticated analyses, such as treatment plans for identical targets showing tumor isodose contours as well as dose to nearby normal tissue, are beyond the scope of this chapter. The data in Table 2.2 are taken from an experimental study comparing seven different clinical epithermal neutron beams [4] as well as published reports on the performance and features of the irradiation facilities [1, 49, 55]. Unless otherwise noted, the figures of merit (where available) are all derived using a common set of dose conversion parameters, boron concentrations, and weighting factors that are representative of brain irradiations using both BPA and an advanced compound.
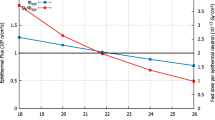
The advantage depth (AD) or useful beam penetration should exceed a minimum of 8 cm if external beam brain irradiations are contemplated. An 8–10-mm-thick filter of pure 6Li as in the case of the Studsvik and MIT beams hardens the neutron energy spectrum and provides a significant increase in AD, thereby improving dose coverage for the deepest tumors [5]. A lithium filter does, however, reduce therapeutic margin in shallow tumors and is associated with a roughly 50 % reduction in beam intensity that increases treatment time. 6Li filtration is therefore best used as an option for deeper tumors in beams with the highest intensity where the reduced output does not lead to excessively long irradiations. All of the currently available epithermal neutron beams achieve an AD of at least 8 cm with BPA, increasing significantly when parameters for an advanced compound are applied, where the most penetrating beams have an AD exceeding 11 cm.
The advantage ratio (AR) is the total tumor-to-normal-tissue dose ratio averaged from the beam entrance to the advantage depth. This varies between five and six in most beams when using BPA which indicates an average tumor dose five to six times higher than in nearby normal tissue. The advantage ratio is generally higher in beams with lower contamination, but this figure of merit depends principally on the boron uptake parameters, increasing to nearly 12 for an advanced compound in the cleanest beams.
High beam intensity is important to minimize treatment times. Short irradiations are more comfortable for the patient and more efficient for clinical staff. Shorter fields also mitigate degradation in the therapeutic advantage that may occur as the compound is washed out of tissue and tumor following administration. However, patient throughput is at present limited by the clinical resources available to BNCT rather than the duration of irradiations or the capacity and availability of suitable neutron sources. High beam intensity is nevertheless desirable for the reasons described earlier and for future development to enable larger, more comprehensive studies that rigorously evaluate the efficacy of this modality. Table 2.2 lists the incident epithermal flux intensity together with the irradiation time to reach a peak brain dose of 12.5 Gy (w) using a single field that is representative of irradiations in the brain cancer trials performed to date. Irradiation time is inversely related to the incident epithermal neutron flux although the two quantities are not directly proportional. MIT and Studsvik with the highest beam intensities can reach tolerance doses in several minutes, and this duration is comparable to fields routinely administered with other forms of radiotherapy. Irradiations at other facilities last two to six times longer than those at MIT, and these are manageable for clinical investigations but would become a limiting factor with significant increases in clinical enrollment. Irradiation times could also become substantially longer in trials using better tumor-targeting agents where the normal tissue dose rate is lower due to much lower retention of boron in normal tissue.
Neutron beam characteristics are relatively straightforward to quantify, and based on the clinical experience to date, some of the most recently constructed facilities have reached a practical optimum in terms of intensity, beam purity, and therapeutic effectiveness. The operational characteristics of these irradiation facilities are, however, equally important for implementing clinical programs and eventually incorporating new ideas derived from translational and preclinical research. Reactor-based beamlines are fixed (usually horizontal), but many designs have incorporated flexibility in terms of beam delivery and patient positioning as summarized in the bottom four rows of Table 2.2. Brain irradiations in BNCT normally apply circular beam apertures with diameters ranging from 12 to 16 cm. Variable aperture sizes are used at several facilities, and these are helpful in minimizing collateral dose and improving tumor dose conformity while restricting doses to organs at risk.
A highly collimated neutron beam also helps to minimize normal tissue dose and is associated with increased beam penetration [4] that can improve coverage for deep-seated tumors. Good collimation eases patient positioning and minimizes uncertainties associated with dose falloff from the aperture of the beam. In the FCB facility at MIT, the epithermal neutron flux decreases at a rate of approximately 0.7 % mm−1, and the routinely applied air gap of 3 cm modestly reduces intensity of the incident beam by approximately 20 % [45]. Positioning uncertainties of approximately 5 mm therefore result in up to a 3.5 % error in the administered dose which is comparable to other sources of uncertainty. An even larger air gap between the patient and beam aperture is feasible at the facility in Petten where the neutron beam has extraordinarily high collimation and intensity drops by less than 20 % over 30 cm from the beam aperture. The full width at half maxima (FWHM) of epithermal neutron profiles measured in air 30 cm from the collimator are only 10 % (or less) wider than the nominal beam aperture. Patients may therefore be positioned at this distance without adversely affecting beam targeting, and axial positioning uncertainties are negligible [42].
A beam collimator that protrudes into the medical room helps to comfortably position patients, especially in cranial irradiations where the shoulders of the patient may interfere. With the advent of relatively intense and pure epithermal neutron beams, greater consideration is now being given to operational characteristics, for example, in Finland where the facility was recently modified to make patient positioning easier [3]. A long, protruding patient collimator accessible from inside the irradiation room that can be readily adapted to accommodate apertures of different sizes or shapes affords more beam placement options and greater flexibility in treatment planning and facilitates easier patient setups for a multitude of disease sites. A medical therapy room with an area of approximately 9 m2 centered about the beam is large enough to accommodate the length of a patient for either side of a lateral brain irradiation. Some of the facilities listed in Table 2.2 are larger than this and have ample space for the patient and associated monitoring equipment. Field placement may however still be encumbered by room geometry that restricts angles relative to the beam centerline for positioning patients. An example is the medical room at JRR-4 which is spacious but long and narrowest near the beam aperture so patient positions are relatively restricted. Facilities with less than a full 180º arc for positioning patients about the beam centerline are noted in Table 2.2.
Some facilities have incorporated options to control the neutron energy spectrum by adding one or more tanks to the beamline that can be filled with heavy water to moderate neutrons with low parasitic absorption [12, 49, 55]. Other groups have augmented their beamline to accommodate cassettes containing solid lithium metal which hardens the neutron energy spectrum and may be added or removed as needed [5, 12]. Reactor-based beamlines can therefore extract neutrons spanning the entire energy range of interest in BNCT from thermal up to ∼10 keV, and this may prove advantageous because no single neutron energy is optimum for tumors at all depths in tissue.
Clinical trials in BNCT have thus far been carried out exclusively with reactor-based neutron sources. This reflects the suitability and relative abundance of the aforementioned facilities that are located at research reactors around the world near large metropolitan areas with research hospitals. Several accelerator-based sources are being developed for BNCT, mainly in physics research laboratories. Research results from these programs indicate that intensities for these sources must increase by more than an order of magnitude over currently achievable levels to match the beam characteristics of existing reactor-based beams [8, 10, 15, 28, 56]. The limitations arise mainly from engineering challenges in beamline and target development, and if these problems are resolved, accelerator-based sources may become a competitive option for clinical research. Accelerator-based beamlines could be more readily transferred to a radiation oncology center than reactor-based sources.
4 A State-of-the-Art Epithermal Neutron Irradiation Facility
A state-of-the-art epithermal neutron irradiation facility was designed and constructed at MIT to meet all of the requirements for a clinical BNCT research facility with the capability for high patient throughput in support of larger clinical trials or more routine therapy. Constructed at the 6 MW MITR, the FCB provides a high-performance irradiation facility suitable for clinical studies and large animal experiments that is capable of administering irradiations to several patients a day in support of larger trials or more routine clinical implementation. A fission converter-based neutron source comprised of a subcritical array of fuel was chosen because the reactor core is fixed in the center of the surrounding reflector/moderator, making it difficult to access core neutrons directly. Figure 2.2 shows an isometric view of the FCB epithermal neutron irradiation facility [22, 23]. Also depicted in the lower left-hand corner of Fig. 2.2 are the vertical thermal neutron beamline and medical irradiation room that were included in the original design of the MITR and provide a high-quality thermal neutron beam for NCT research. The fission converter is presently configured to produce 120 kW by using 11 standard MITR-II fuel elements cooled with D2O and was designed and licensed to operate up to 250 kW. Considerable increases in neutron source strength are therefore possible in the future, which can be achieved by using an optimized converter fuel rather than MITR fuel elements or by increasing the reactor power. Details on the characteristics and performance of the epithermal neutron beam are documented elsewhere [44].
A shielded horizontal beamline 2.5 m long directs neutrons from the converter to the treatment room as shown schematically in Fig. 2.2. The beamline consists of a series of Al (81 cm), Teflon® (13 cm), and Cd (0.5 mm) neutron filter/moderators; a lead photon shield (8 cm); and a large conical collimator 1.1 m long with lead walls 15 cm thick that is followed by a final patient collimator. An experimental study of radiation damage effects has verified that the fluorine contained in Teflon® is chemically stable and the material retains adequate mechanical properties during the expected lifetime of the FCB [23]. The 0.42-m-long patient collimator is made from a mixture of lead and boron or lithium-loaded (95 % enriched in 6Li) epoxy that extends the beamline into the shielded medical therapy room. The patient collimator has provisions for inserting a cassette into the beamline that contains an 8-mm-thick lithium metal disc (also 95 % enriched in 6Li). This filter hardens the neutron beam by removing some of the lower energy neutrons and can increase the useful therapeutic beam penetration for deep-seated tumors.
The neutron beam is controlled by three in-line shutters acting independently that are installed along the length of the beamline. The first of these, starting near the reactor core, is the converter control shutter (CCS) that is a 0.5-mm layer of Cd followed by a 6.4-mm sheet of aluminum alloyed with boron of natural isotopic abundance. This shutter modulates the fission rate in the converter (and beam intensity) between 1 and 100 % by shielding the converter fuel against thermal neutrons incident from the MITR-II reflector region. Downstream from the converter fuel is a 68-cm-long tank that when filled with light water provides effective neutron attenuation. Following this is the mechanical shutter that effectively turns the beam on and off (reducing beam intensity by 2–3 orders of magnitude) within 3 s during therapy and comprises a large sliding slab to fill a section of the collimator with a 20-cm thickness of borated (100 mg cm−3 10B) high-density (ρ = 4.0 g cm−3) concrete and 20 cm of lead. The room entrance is shielded from direct beam radiation by a short hallway as well as a 0.28-m-thick steel door driven by an air motor that opens the door in 10 s.
The medical room in Fig. 2.3 is built with 1.1 m-thick walls of high-density concrete with a roof of 15 cm-thick steel beneath 55 cm of high-density concrete. The wall of the medical room nearest the FCB control console includes a large window containing layers of quartz and lead glass as well as mineral oil as shown schematically in Fig. 2.3. Inner surfaces of the walls and ceiling are lined with 2.5 cm of borated polyethylene to absorb thermal neutrons and reduce activation of the steel-reinforced concrete walls and steel ceiling. A 1 cm thick boron loaded epoxy ground reduces activation of the concrete floor.
During operation at full beam intensity, dose equivalent rates outside the medical room are a maximum of 12 μSv h−1 measured behind the rear wall opposite the beam, with no significant neutron contribution. Since the observed values are only marginally higher than the nominal background of approximately 8 μSv h−1 in the reactor hall without the converter operating, no additional access control to the experimental hall is required when the FCB is in use. Inside the medical room with all shutters closed, a dose equivalent rate of 100 μSv h−1 is apparent at the patient position (somewhat higher immediately following an irradiation) that is due entirely to photons emanating from the beamline. General area dose rates of approximately 20 μSv h−1 are observed away from the patient collimator in the medical room with the reactor at full power, and staff can therefore freely enter the room without the need to lower reactor power.
The beam centerline in the medical room is 0.42 m above the floor, and the patient collimator can be readily configured to provide aperture diameters of 80, 100, 120, and 160 mm that conveniently extend up to 0.42 m beyond the wall of the medical room. The collimator diameter tapers from 0.67 m at its base to 0.3 m near the patient, and this, combined with ample (14 m2) floor space in the medical room allows patients to be comfortably positioned for cranial irradiations in a full 180° arc around the beam centerline while lying supine on the treatment couch. A laser projection illuminates the central axis of the beam to help with patient positioning as well as optics that penetrate the wall of the collimator to provide a beam’s eye view. Prior to commencing an irradiation, the laser and optics are withdrawn and replaced with a plug that has a composition identical to the patient collimator walls.
Four fission counters positioned in the periphery of the beam near the base of the patient collimator operate in pulse mode and serve as integral monitors of the neutron fluence as it is delivered to the patient. Fields are prescribed as an integral number of counts in these detectors based on a correlation with absorbed dose measurements that are used to benchmark treatment plans [26]. Signals are fed to NIM electronics, and irradiations are administered with a redundant pair of programmable logic controlled (PLC) systems that automatically terminates the irradiation when the integrated counts on any of the four beam monitors reach the prescribed target. Data from instrumentation in the FCB cooling system and beamline shutters are also fed to the PLCs, which are programmed with automated interlocks to help ensure the safety of the patient and operational staff alike. The facility is operated from the control console that includes a dedicated computer for displaying progress of an irradiation and archiving data from the PLCs. During an irradiation, the patient and his or her vital signs are monitored through the shielded viewing window and closed-circuit cameras which contain an integrated audio system for two-way communication between the medical room and control console.
Prior to commencing an irradiation, a series of safety interlocks must be satisfied before the shutters can be opened to turn the beam on. The prescribed monitor units are entered using a numeric keypad on the console. The operator commences therapy with a single pushbutton, and the PLCs issue commands to open each shutter in sequence and initiate data acquisition. It takes 2 min for all shutters to open. Monitor counts accumulate continuously on the updated display. The PLCs repeatedly interrogate all safety interlocks, check that the accumulated monitor counts are below the preset targets, and store the data to the computer in programmed intervals of 10 s. Like conventional radiotherapy machines, no other actions are required from the operator unless they need to intervene, for which there is a manual override that terminates an irradiation by closing shutters or scramming the reactor. When the accumulated counts on any one of the four beam monitors first reach the set target, the PLCs signal all shutters to close. To defend against overexposures that might be caused by some mechanical or electrical failure during shutter closure, programmed safety interlocks automatically scram the reactor if any channel exceeds 102 % of the prescribed target value [21, 54].
Controls for opening shutters are deactivated when the shield door to the medical room is open to help prevent inadvertent beam exposure of staff inside the room. The entrance to the medical room is equipped with motion sensors that stop sideways movement of the pneumatically operated 11 t shielding door if anyone is in the vicinity and pressure-sensitive strips run along its leading edge to stop the door upon any contact.
Loss of building power would automatically scram the MITR-II, but if electrical power fails only to the medical area, uninterruptible power supplies keep the PLCs, computer, and other vital instrumentation running for at least 20 min to enable an irradiation field to be completed as planned. The mechanical shutter can be rapidly closed using a hand crank located on the outside of the room, while the water shutter and CCS close automatically under the force of gravity. The shielding door can also be opened by hand in an emergency to quickly gain access to the medical room.
The fission converter concept has proven suitable for obtaining a high-purity beam of epithermal neutrons for BNCT with intensities that result in irradiation times as short as a few minutes. The relatively low power (120 kW) generated in the converter illustrates the efficiency of the fission process for producing epithermal beams and the feasibility of small reactor-based sources for dedicated use in a hospital.
Since the MITR-II is not dedicated solely to BNCT research, the FCB operates independently of other experiments and does not affect regular reactor operation. The beamline is presently optimized for brain tumor studies although it can be easily reconfigured to treat other disease sites. The operational characteristics of the facility closely match those established for conventional radiotherapy, which together with nearly optimum beam characteristics ensure that the FCB is capable of determining whether the radiobiological promise of this cellular tumor-targeting therapy can be realized in routine practice.
5 Summary
This short chapter provides some guidance for those planning to design and construct reactor-based epithermal neutron irradiation facilities for neutron capture therapy. Important performance capabilities for these facilities are presented, and different approaches for using reactors as epithermal neutron irradiation facilities are described. Reactor-based facilities that are presently available generally meet the requirements for clinical studies with more recently constructed facilities making important advances in terms of patient comfort, flexibility, and ease of use. A few of the newer facilities can support larger clinical trials with high patient throughput that is typical of more routine clinical application. Patient throughput and development of BNCT are presently not restricted by the characteristics of existing reactor-based facilities but rather by the level of resources committed to BNCT that in some programs are by necessity centered at institutes hundreds of kilometers away instead of nearby hospitals. Epithermal neutron beams designed for BNCT have been optimized based upon established clinical programs and the trial experience gathered thus far. Additional optimization or customization may become desirable as more data are accrued and a clinical rationale is developed for exploring other tumors outside the brain. Although gains from these optimizations are likely to be small compared, for example, with those derived from improved boron targeting, new facilities should nevertheless seek to incorporate flexibility into beamline designs to be able to realize the full benefit of progress in clinical research. At present, a strong basis for widespread implementation of BNCT does not exist, and it is difficult to envision a major demand for new neutron sources. New reactor-based BNCT facilities could be constructed if needed by modifying more research reactors as described in this chapter or by using currently available and well-proven technology to construct low-power ultrasafe reactors.
References
Akutsu H, Yamamoto T, Matsumura A, Shibata Y, Nakai K, Yasuda S, Matsushita A, Nose T, Yamamoto K, Kumada H, Hori N, Torii Y (2000) In: 9th international symposium on neutron capture therapy. International Society for Neutron Capture Therapy, Osaka, 2000, pp 199–200
Auterinen I, Hiismäki P, Kotiluoto P, Rosenberg RJ, Salmenhara S, Seppälä T, Seren T, Tanner V, Aschan C, Kortesniemi M, Kosunen A, Lampinen J, Savolainen S, Toivonen M, Välimäki P (2001) Metamorphosis of a 35 year-old TRIGA reactor into a modern BNCT facility. In: Hawthorne MF (ed) Frontiers in neutron capture therapy, vol I. Kluwer Academic/Plenum Publishers, New York, pp 267–275
Auterinen I, Kotiluoto P, Hippeläinen E, Kortesniemi M, Seppälä T, Serén T, Mannila V, Pöyry P, Kankaanranta L, Collan J, Kouri M, Joensuu H, Savolainen S (2004) Design and construction of shoulder recesses into the beam aperture shields for improved patient positioning at the FiR1 BNCT facility. Appl Radiat Isot 61:799–803
Binns PJ, Riley KJ, Harling OK (2005) Epithermal neutron beams for clinical studies of boron neutron capture therapy: a dosimetric comparison of seven beams. Radiat Res 164:212–220
Binns PJ, Riley KJ, Ostrovsky Y, Gao W, Albritton JR, Kiger WS III, Harling OK (2007) Improved dose targeting for a clinical epithermal neutron capture beam using optional 6Li filtration. Int J Radiat Oncol Biol Phys 67:1484–1491
Bisceglie E, Colangelo P, Colonna N, Santorelli P, Variale V (2000) On the optimal energy of epithermal neutron beams for BNCT. Phys Med Biol 45:49–58
Blaumann HR, Calzetta-Larrieu O, Longhino JM, Albornoz AF (2001) NCT facility development and beam characterization at the RA-6 reactor. In: Hawthorne MF, Shelly K, Wiersema RJ (eds) Frontiers in neutron capture therapy, 1st edn. Kluwer Academic/Plenum Publishers, New York, pp 313–317
Bleuel DL, Donahue RJ, Ludewigt BA, Vujic J (1998) Designing accelerator-based epithermal neutron beams for boron neutron capture therapy. Med Phys 25:1725–1734
Brugger RM, Constantine G, Harling OK, Wheeler FJ (1990) Rapporteurs’ report. In: Harling OK, Bernard JA, Zamenhof RG (eds) Neutron beam, design, development and performance for neutron capture therapy. Plenum Press, New York, p 54
Burlon AA, Kreiner AJ (2008) A comparison between a TESQ accelerator and a reactor as a neutron sources for BNCT. Nucl Instrum Methods Phys Res B 266:763–771
Burn KW, Casalini L, Martini S, Mazzini M, Nava E, Petrovich E, Rosi G, Sarotto M, Tinti R (2004) An epithermal facility for treating brain gliomas at the TAPIRO reactor. Appl Radiat Isot 61:987–991
Capala JA, Stenstam BH, Sköld K, Munck af Rosenschöld P, Giusti V, Persson C, Wallin E, Brun A, Franzen L, Carlsson J, Salford L, Ceberg C, Persson B, Pellettieri L, Henriksson R (2003) Boron neutron capture therapy for glioblastoma multiforme: clinical studies in Sweden. J Neurooncol 62:135–144
Clement SD, Choi JR, Zamenhof RG, Harling OK (1990) Monte Carlo methods of neutron beam design for neutron capture therapy at the MITR-II. In: Harling OK, Bernard JA, Zamenhof RG (eds) Neutron beam, design, development and performance for neutron capture therapy. Plenum Press, New York, pp 51–70
Coderre JA, Makar MS, Micca PL, Nawrocky MM, Liu HB, Joel DD, Slatkin DN, Amols HI (1993) Derivations of relative biological effectiveness for the high-LET radiations produced during boron neutron capture irradiations of the 9L rat gliosarcoma in vitro and in vivo. Radiat Res 27:1121–1129
Culbertson CN, Green S, Mason AJ, Picton D, Baugh G, Hugtenburg RP, Yin Z, Scott MC, Nelson JM (2004) In-phantom characterization studies at the Birmingham accelerator-generated epithermal neutron source (BAGINS) BNCT facility. Appl Radiat Isot 61:734–738
Farr LE, Sweet WH, Robertson JS, Foster CG, Locksley HB, Sutherland DL, Mendelsohn ML, Stickley EE (1954) Neutron capture therapy with boron in the treatment of glioblastoma multiforme. Am J Roentgenol Radium Ther Nucl Med 71:279–293
Godel JB (1960) Description of facilities and mechanical components, medical research reactor (MRR) Brookhaven National laboratory, BNL-600, Brookhaven National Laboratory, Upton
Goorley JT, Kiger WS III, Zamenhof RG (2002) Reference dosimetry calculations for neutron capture therapy with comparison of analytical and voxel models. Med Phys 29:145–156
Guotu K, Ziyong, S, Feng, S (2009) The study of physics and thermal characteristics for in hospital neutron irradiator (IHNI). Appl Radiat Isot 67:S234-S7
Harling OK, Riley KJ (2003) Fission reactor neutron sources for neutron capture therapy – a critical review. J Neurooncol 62:7–17
Harling OK, Moulin SJ, Chabeuf JM, Solares GS (1995) On-line beam monitoring for neutron capture therapy at the MIT research reactor. Nucl Instrum Methods Phys Res B 101:464
Harling OK, Riley KJ, Newton TH, Wilson BA, Bernard JA, Hu LW, Fonteneau EJ, Menadier PT, Ali SJ, Sutharsan B, Kohse GE, Ostrovsky Y, Stahle PW, Binns PJ, Kiger WS III, Busse PM (2002) The fission converter based epithermal neutron irradiation facility at the Massachusetts Institute of Technology reactor. Nucl Sci Eng 140:223–240
Harling OK, Kohse GE, Riley KJ (2002) Irradiation performance of polytetrafluoroethylene (Teflon ®) in a mixed fast neutron and gamma radiation field. J Nucl Mater 304:83–85
Hatanaka H (1975) A revised boron-neutron capture therapy for malignant brain tumors. II. Interim clinical result with the patients excluding previous treatments. J Neurol 209:81–94
Kiger WS III, Sakamoto S, Harling OK (1999) Neutronic design of a fission converter-based epithermal neutron beam for neutron capture therapy. Nucl Sci Eng 131:1–22
Kiger WS III, Lu XQ, Harling OK, Riley KJ, Binns PJ, Kaplan J, Patel H, Zamenhof RG, Shibata Y, Kaplan ID, Busse PM, Palmer MR (2004) Preliminary treatment planning and dosimetry for a clinical trial of neutron capture therapy using a fission converter epithermal neutron beam. Appl Radiat Isot 61:1075–1081
Kobayashi T, Sakurai Y, Kanda K (2001) Characteristics of neutron irradiation facility and dose estimation method for neutron capture therapy at Kyoto University Research Reactor Institute. In: Current status of neutron capture therapy, IAEA Tecdoc 1223, IAEA, Vienna, 2001, pp 175–185
Kononov OE, Kononov VN, Bokhovko MV, Korobeynikov VV, Soloviev AN, Sysoev AS, Gulidov IA, Chu WT, Nigg DW (2004) Optimization of an accelerator-based epithermal neutron source for neutron capture therapy. Appl Radiat Isot 61:1009–1013
Kortesniemi M (2002) Solutions for clinical implementation of boron neutron capture therapy in Finland. Ph.D. thesis, University of Helsinki, Helsinki, ISBN 951-45-8955-6; http://ethesis.helsinki.fi, pp 54–68
Liu HB (1995) Design of neutron beams for neutron capture therapy using a 300 kw slab TRIGA reactor. Nucl Technol 109:314–326
Liu HB, Brugger RM (1994) Conceptual designs of epithermal neutron beams for boron neutron capture therapy from low-power reactors. Nucl Technol 108:151–156
Liu HB, Brugger RM, Rorer DC, Tichler PR, Hu JP (1994) Design of a high-flux epithermal neutron beam using 235U fission plates at the Brookhaven Medical Research Reactor. Med Phys 21:1627–1631
Liu HB, Greenberg DD, Capala J, Wheeler FJ (1996) An improved neutron collimator for brain tumor irradiations in clinical boron neutron capture therapy. Med Phys 23:2051–2060
Liu HB, Razvi J, Rucker R, Cerbone R, Merrill M, Whittemore W, Newell D, Autry S, Richards W, Boggan J (2001) TRIGA fuel based converter assembly design for a dual-mode neutron beam system at the McClellan Nuclear Radiation Center. In: Hawthorne MF, Shelly K, Wiersema RJ (eds) Frontiers in neutron capture therapy, 1st edn. Kluwer Academic/Plenum Publishers, New York, pp 295–300
Liu YWH, Huang TT, Jiang SH, Liu HM (2004) Renovation of epithermal neutron beam for BNCT at THOR. Appl Radiat Isot 61:1039–1043
Marek M, Burian J, Rataj J, Polák J, Spurny F (1997) Reactor based epithermal neutron beam enhancement at Rež. Radiat Prot Dosimetry 70:567–570
Moss RL, Aizawa O, Beynon D, Brugger R, Constantine G, Harling O, Liu HB, Watkins P (1997) The requirements and development of neutron beams for neutron capture therapy of brain cancer. J Neurooncol 33:27–40
Moss RL, Stecher-Rasmussen F, Ravensberg K, Constantine G, Watkins P (1992) Design, construction and installation of an epithermal neutron beam for BNCT at the high flux reactor Petten. In: Allen BJ et al. (eds) Progress in Neutron Capture Therapy for Cancer. Plenum Press, New York, pp 63–66
Nievaart VA, Moss RL, Kloosterman JL, van der Hagen THJJ, van Dam H (2004) A parameter study to determine the optimal source neutron energy in boron neutron capture therapy of brain tumors. Phys Med Biol 49:4277–4292
Nigg DW, Venhuizen JR, Wemple CA, Tripard GE, Sharp S, Fox K (2004) Flux and instrumentation upgrade for the epithermal neutron beam facility at Washington State University. Appl Radiat Isot 61:993–996
Raaijmakers CPJ, Nottelman EL, Konijnenberg MBJ (1995) Dose monitoring for boron neutron capture therapy using a reactor-based epithermal neutron beam. Phys Med Biol 41:2789–2797
Raaijmakers CPJ, Konijnenberg MW, Mijnheer BJ (1997) Clinical dosimetry of an epithermal neutron beam for neutron capture therapy: dose distributions under reference conditions. Int J Radiat Oncol Biol Phys 37:941–951
Rief H, Van Heusden R, Perlini G (1993) Generating epithermal neutron beams for neutron capture therapy in TRIGA reactors. In: Soloway AH, Barth RF, Carpenter DE (eds) Advances in neutron capture therapy. Plenum Press, New York, pp 85–88
Riley KJ, Binns PJ, Harling OK (2003) Performance characteristics of the MIT fission converter based epithermal neutron beam. Phys Med Biol 48:943–958
Riley KJ, Binns PJ, Harling OK (2004) The design, construction and performance of a variable collimator for epithermal neutron capture therapy beams. Phys Med Biol 49:2015–2028
Rogus RD, Harling OK, Yanch JC (1994) Mixed field dosimetry of epithermal neutron beams for boron neutron capture therapy at the MITR-II research reactor. Med Phys 21:1611–1625
Sakamoto S, Kiger WS III, Harling OK (1999) Sensitivity studies of beam directionality, beam size and neutron spectrum for a fission converter-based epithermal neutron beam for boron neutron capture therapy. Med Phys 26:979–988
Sakurai F, Torii Y, Kishi T, Kumada H, Yamamoto K, Yokoo K, Kaieda K (2001) Medical irradiation facility at JRR-4. In: IAEA - TECDOC-1223 Current Status of Neutron Capture Therapy. International Atomic Energy Agenct, Vienna, pp 142–146
Sakurai Y, Kobayashi T (2002) The medical-irradiation characteristics for neutron capture therapy at the heavy water neutron irradiation facility of Kyoto University Research Reactor. Med Phys 29:2328–2337
Slatkin DN (1991) A history of boron neutron capture therapy of brain tumors. Brain 114:1609–1629
Tanner V, Auterinen I, Helin J, Kosunen A, Savolainen S (1999) On-line beam monitoring of the Finnish BNCT facility. Nucl Instrum Methods Phys Res A 422:101–105
Thompson TJ, Benedict M, Cantwell T, Axford RA (1956) Final hazards summary report to the Advisory Committee on reactor safeguards on a research reactor for the Massachusetts Institute of Technology. Published Cambridge, MIT [1956] located in the Institute archives, non-circulating collection 2 TK9202.M36
Wallace SA, Mathur JN, Allen BJ (1994) Treatment planning figures of merit in thermal and epithermal boron neutron capture therapy of brain tumors. Phys Med Biol 39:897–906
Wilson BA, Riley KJ, Harling OK (2000) Automatic control and monitoring of the MIT fission converter beam. In: 9th international symposium on neutron capture therapy. International Society for Neutron Capture Therapy, Osaka, 2000, pp 237
Yamamoto T, Matsumura A, Shibata Y, Nose T, Yamamoto K, Kumada H, Hori N, Torii Y, Ono K, Kobayashi T, Sakurai Y (2000) Radiobiological characterization of epithermal and mixed thermal-epithermal beams at JRR-4. In: 9th international symposium on neutron capture therapy. International Society for Neutron Capture Therapy, Osaka, 2000, pp 205–206
Yanch JC, Blue TE (2003) Accelerator-based epithermal neutron sources for boron neutron capture therapy of brain tumors. J Neurooncol 62:19–31
Yanch JC, Harling OK (1993) Dosimetric effects of beam size and collimation of epithermal neutrons for boron neutron capture therapy. Radiat Res 135:131–145
Yanch JC, Zhou XL, Brownell GL (1991) A Monte Carlo investigation of the dosimetric properties of monoenergetic neutron beams for neutron capture therapy. Radiat Res 126:1–20
Zamenhof RG, Murray BW, Brownell GL, Wellum GR, Tolpin EI (1975) Boron neutron capture therapy for the treatment of cerebral gliomas. I: theoretical evaluation of the efficacy of various neutron beams. Med Phys 2:47–60
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Harling, O.K., Riley, K.J. (2012). Fission Reactor-Based Irradiation Facilities for Neutron Capture Therapy. In: Sauerwein, W., Wittig, A., Moss, R., Nakagawa, Y. (eds) Neutron Capture Therapy. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-31334-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-642-31334-9_2
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-31333-2
Online ISBN: 978-3-642-31334-9
eBook Packages: MedicineMedicine (R0)