Abstract
In both Hodgkin disease and non-Hodgkin lymphoma, imaging plays an important role for primary diagnosis and staging [1]. Except for cerebral lymphoma, whole-body MRI is of high research interest but not clinical routine in the staging algorithm of lymphoma patients. This situation could change quickly, and whole-body MRI might become a good alternative to CT [2]. Especially whole-body diffusion-weighted MRI, with a sensitivity of 90 % and a specificity of 94 %, is a good candidate for supplementing/replacing 18F-FDG PET-CT for the staging of Hodgkin disease and non-Hodgkin lymphoma [3, 4]. Alternatively, combing MR and 18F-FDG PET might further increase diagnostic accuracy and play an important role as research tool in evaluating the strengths and draw-backs of both modalities directly against each other. This might also give additional data on the view of some authors who argue that 18F-FDG PET-CT might even eliminate the need for bone marrow biopsy in the primary staging of Hodgkin disease because 18F-FDG PET-CT is highly sensitive and specific for bone marrow involvement in this disease, at 92 and 90 %, respectively [5]. Additional information using PET-MR could be specifically gained from diffusion-weighted sequences in the case of indolent lymphomas [6]. Finally due the lack of radiation exposure of MRI, compared with CT, PET/MRI may get an alternative to PET-CT especially in young patients with good prognosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Lymphoma, Lung and Other Tumors
In both Hodgkin disease and non-Hodgkin lymphoma, imaging plays an important role for primary diagnosis and staging [1]. Except for cerebral lymphoma, whole-body MRI is of high research interest but not clinical routine in the staging algorithm of lymphoma patients. This situation could change quickly, and whole-body MRI might become a good alternative to CT [2]. Especially when combining with whole-body diffusion-weighted MRI, with a its high sensitivity could improve the diagnostic accuracy for the staging of Hodgkin disease and non-Hodgkin lymphoma [3, 4]. Alternatively, combing MR and 18F-FDG PET might further increase diagnostic accuracy and play an important role as research tool in evaluating the strengths and draw-backs of both modalities directly against each other. This might also give additional data on the view of some authors who argue that 18F-FDG PET/CT might even eliminate the need for bone marrow biopsy in the primary staging of Hodgkin disease because 18F-FDG PET/CT is highly sensitive and specific for bone marrow involvement in this disease, at 92 % and 90 % respectively [5]. Additional information using PET/MR could be specifically gained from diffusion-weighted sequences in the case of indolent lymphomas [6]. Finally due the lack of radiation exposure of MRI, compared with CT, PET/MRI may get an alternative to PET/CT especially in young patients with good prognosis.
MR in general is considered to be inferior to CT for staging of lung cancer and detection of pulmonary metastases [7, 8]. However MRI, including DWI sequences, has been shown to detect 100 % of lung metastases larger than 7 mm found on CT and the presence of small metastases is often no therapeutically relevant [9, 10]. Hereby first preliminary data indicate an equivalent accuracy of PET/MR and PET/CT for lung lesions [11]. In addition, new developments like half-Fourier, single-shot, turbo spin echo sequences have substantially improved the lung-tissue contrast of MRI in the recent years [8]. With regard to local tumor infiltration into adjacent structures MRI might improve T-staging when compared to CT.
Diffuse Large B-Cell Lymphoma
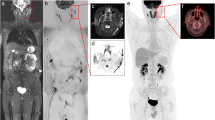
Clinical History
Thirty-eight-year-old patient with diffuse large B-cell lymphoma (originally as gastric MALT). Follow-up study acquired after two cycles of chemotherapy. Status post renal transplant at age of 19.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 369 MBq of 18F-FDG, 57 kg/157 cm patient, with 5.2 mmol/L of fasting glycemia.
MRI: Whole body atMR (T1 weighted), supine position. 3D FFE T1 weighted (eThrive) whole-body MRI.
Findings
Initial staging study prior to treatment showed multiple hypermetabolic lymph nodes in the coeliac and retroperitoneal areas. Super diaphragmatic extension showed a single positive supraclavicular lymph node. Follow-up study after two cycles of chemotherapy show complete normalization of lymph nodes metabolic activity.
Teaching Points
Although whole-body MR images may not provide similar diagnostic anatomical resolution as PET/CT, PET/MR may be a valuable alternative technique for assessment of the extent of the disease and response to chemotherapy particularly in patients with limited renal function that may be at risk of renal toxicity from CT contrast media.
Recurrence of Chondrosarcoma
Clinical History
Thirty-five-year-old patient with a history of surgical removal of a mixoide chondrosarcoma of the left thigh followed by radio- and chemo-therapy 2 years ago. Current study requested for investigation of recurrence of extra-articular multi-metastatic extension of the original tumor.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 369 MBq of 18F-FDG, 57 kg/157 cm patient, with 5.2 mmol/L of fasting glycemia.
MRI: Whole body atMR (T1 weighted), supine position followed by a whole body 3D FFE T1 weighted (eThrive) MRI.
Findings
Current study shows recurrence of soft tissue lesion of the left thigh with focal increase in FDG uptake with remote metastatic extension of hepermetabolic lesions in the iliac and peritoneal area of the left abdomen and pelvic area.
Teaching Points
For soft tissue tumors, high-resolution MR images can provide more adequate soft tissue differentiation and anatomical localization than CT images
Metastatic Pulmonary Cancer (NSCLC)
Clinical History
Seventy-year-old patient diagnosed with non-small cell lung cancer (NSCLC) with liver metastases. Follow-up study requested 3 months after chemotherapy.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 370 MBq of 18F-FDG.
MRI: Whole body atMR (T1 weighted), supine position. 3D FFE T1 weighted (eThrive) MRI followed by coronal high-resolution breath-hold HASTE images of the upper abdomen.
Findings
PET/MR shows left lower lobe lung cancer with metastatic mediastinal lymph node and heterogeneous tracer uptake in large lesion (7 × 9 cm) in right liver segments VI/VII corresponding to metastatic disease.
Teaching Points
For liver metastases, high-resolution breath-hold MR images can provide better definition and tissue characterization than contrast-enhanced CT images.
Esophageal Cancer with Liver Metastases
Clinical History
Sixty-year-old patient investigated for staging of a distal esophageal adenocarcinoma of the oeso-gastric junction. Status post chemotherapy.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 370 MBq of 18F-FDG.
MRI: Whole body atMR (T1 weighted), supine position. Followed by a complementary diagnostic MRI study acquired on a Siemens Espree including a T2 HASTE MRI sequences in coronal. 3D FFE T1 weighted (eThrive) sequence with contrast injection.
Findings
PET/MR shows the hypermetabolic tumor lesion of the oeso-gastric junction, and a focal metastatic lesion of the liver with high FDG uptake. Incidental finding of a benign hepatic lesion without tracer uptake, most likely an hemangioma.
Teaching Points
Combination of diagnostic MR sequences and PET images allow to better differentiate malignant from benign lesions of the liver.
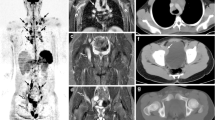
Multi-Focal Lung Tumor
Clinical History
Seventy-year-old patient with history of smoking and incidental finding of a lung tumor on chest X-ray performed for investigation of resistant cough. Histology confirmed pulmonary carcinoma (cT2a cN3 cN0, stage IIB). Study requested for staging post chemotherapy.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 370 MBq of 18F-FDG.
MRI: Whole body atMR (T1 weighted), supine position. 3D FFE T1 weighted (eThrive) MRI followed by respiratory-gated T2 weighted HASTE images acquired in coronal and axial planes.
Comparison of PET/MR (left) and PET/CT studies. Axial respiratory-gated T2 weighted HASTE images (a) fused with corresponding PET image (b), and axial CT with lung window setting (d) and soft tissue setting (e) fused with corresponding PET images (f). Both (c) and (g) show the PET images at the same level of the two studies
Findings
PET/MR shows a hypermetabolic lung lesion of the apical segment of the left lower pulmonary lobe. Identification of multiple metastatic lymph nodes with intense focal uptake of FDG in the paratracheal, hilar and subcarenal areas.
Teaching Points
While MR sequences are not optimal for examination of lung parenchyma that is best evaluated by CT, high resolution MR sequences can however provide sufficient anatomical details for identification and localization of lesions with high FDG uptake.
Brain Metastasis of Unknown Origin
Clinical History
Sixty-two-year-old patient discovered having a brain metastases in the left cerebellum on an MRI performed for investigating recurrent headaches. Current study requested for staging and identification of the original tumor. Patient also known for renal insufficiency and multiple renal cysts.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 369 MBq of 18F-FDG, 57 kg/157 cm patient, with 5.2 mmol/L of fasting glycemia.
MRI: Whole body atMR (T1 weighted), supine position. 3D FFE T1 weighted (eThrive) MRI followed by a complete diagnostic MRI study of the abdomen.
Findings
PET/MR shows a focal hypermetabolic lesion of the hilum of the left lung. Standard whole-body MRI could not clearly characterize the lung lesion but complimentary PET/CT confirmed the suspicion of lung cancer. Additional high resolution MRI showed polycystic renal disease and incidental finding of an aortic dissection.
Teaching Points
For proper characterization of suspicious lung tumor, additional CT image are required. But PET/MR allows to properly stage the extent of remote metastatic lesions.
Pulmonary Adenocarcinoma
Clinical History
Sixty-eight-year-old patient following incidental finding of a right lung mass on chest X-ray for chronic cough. CT guided biopsy confirmed a pulmonary adenocarcinoma. Study requested for staging and treatment planning.
Imaging Technique
PET: Whole-body PET acquired 60 min after injection of 370 MBq of 18F-FDG.
MRI: Whole body atMR (T1 weighted), supine position. 3D FFE T1 weighted (eThrive) MRI followed by a whole body STIR acquisition.
Findings
PET/MR confirmed the presence of a hilar tumoral mass of the right lower lobe, associated with pneumonitis of the lower lobe secondary to partial obstruction of the bronchi by the tumor. Identification of multiple hypermetabolic lymph nodes of the mediastinum and subclavicular region
Teaching Points
PET images of PET/MR studies allow differentiating the extension of hypermetabolic tumor tissue from associated pneumonia with low or moderate FDG uptake.
PET/MR in Acute Lymphocytic Leukemia (ALL)
Clinical History
A 44 year old patient with a pathological fracture of the lumbar spine previously stabilized with dorsal instrumentation. Histopathology revealed ALL-infiltration in the lumbar spine.
Imaging Technique
Whole body PET/MR images acquired 112 min after iv injection 408 MBq 18F-FDG, 77 kg.
8 beds × 5 min together with whole body cor T1w TSE and cor T2w STIR. Axial T1w VIBE fat saturated after Gadolinium over the region of the thorax, abdomen and pelvis.
Coronal T1w TSE (far left) and T2w STIR (middle left) show bone marrow infiltration in the left sacral bone, the left proximal femur, right ischium and the upper thoracic spine. Metal artifacts from the dorsal instrumentation obscure this region on MR images. PET (middle right) and fused PET/MR (far right) images demonstrate high uptake of 18F-FDG in the corresponding regions. The lesion in the upper thoracic spine might be missed on MR only, however the high lesion-to-background ratio on the PET images helps identifying it
Coronal T12w STIR and T1w TSE show a pathological fracture of L4 with artifacts from dorsal instrumentation in L3 and L5 (upper row). The T1w hypointense signal in L4 and the proximal left femur indicates complete infiltration of the vertebra by lymphoblastic cells. A small lesion is also found in the right pubic bone. In addition T2w STIR demonstrates a hyperintense extraosseous strand on the left side reaching from L4 to the sacral bone. Another small extraosseous formation is present on the left side. Both PET and fused image confirm high uptake of 18F-FDG in the corresponding regions (lower row)
The extraosseous tumor growth is better depicted in PET (right) compared to an axial T1w VIBE sequence (left) after Gadolinium with fat saturation. In this sequence only a diffuse low to moderate contrast enhancement could be found, whereas the high lesion-to-background ratio in PET outlines the spread more clearly
Findings
A diffuse affection with bone marrow infiltration primarily of the lumbar and sacral spine is found in PET. MR demonstrates the extent of extra-osseous growth around the sacral bone.
Teaching Points
Combined PET/MR provides detailed information about the extent of the bone marrow infiltration. Smaller lesions might be missed by MR only but the high lesion-to-background ratio of PET facilitates their detection.
PET/MR for Biopsy Planning in NHL with Bone Infiltration
Clinical History
A 54 year old patient presents chronically elevated leucocytes and the suspicion of lymphoma. No suspicious lymph nodes were found on CT.
Imaging Technique
Whole body PET/MR images acquired 174 min after iv injection 444 MBq 18F-FDG, 95 kg.
4 beds × 4 min together with whole body cor T1w TSE and axial T2w HASTE fs. 1 bed (pelvis) a 4 min together with cor T2w STIR and axial T1w fs after Gadolinium.
Coronal T1w TSE and T2w STIR show patchy bone marrow infiltration of the lumbar spine and pelvis (upper row). Note the normal interposed bone marrow between the affected areas. Coronal PET shows moderate increase tracer uptake in the lumbar spine and pelvis. Fused PET and T1w TSE demonstrate good correlation between the uptake in PET and the hypointense regions in T1w (lower row)
Axial PET and fused images show a patchy infiltration of the pelvis and sacral bone (upper row). Diffuse hyperintensity in T2w HASTE fs in MRI demonstrate the replacement of fatty marrow in the corresponding region (left, lower row). In CT no abnormalities could be detected (right, lower row). Incomplete fat suppression is related to hip prosthesis on the left side
Findings
T1w TSE and T2w STIR show a patchy bone marrow infiltration with islands of normal bone interposed between. Note the extensive artifacts from a hip prosthesis on the left side especially impairing the fat suppression.
Teaching Points
The combination of whole-body PET and MR can aid in guiding biopsy in patients with lymphoma especially in atypical cases like primary bone infiltration. The information of T1w TSE and T2w STIR delineate areas of bone infiltration against the normal bone marrow. In contrast, CT often shows no pathological finding.
Recurrent T-NHL with Bone Infiltration
Clinical History
A 60 year old patient with prior T-NHL presents with pain in the right hip. CT demonstrates diffuse osteolyses in the right acetabulum rising the suspicious of a recurrence with bone infiltration.
Imaging Technique
Whole body PET/MR images acquired 117 min after iv injection 367 MBq 18F-FDG, 78 kg.
4 beds × 5 min together with whole body coronal T1w TSE and cor T2w STIR. Whole body axial T1w flash fat saturated after Gadolinium.
Coronal T1w TSE (left) show a nodular hypointensity in the iliac crest on the right side and a diffuse bone marrow infiltration of the right acetabulum. Coronal PET demonstrate high focal uptake in the corresponding regions (middle). A good correlation between the findings in MR and PET is outlined in the fused dataset (right)
Findings
In contrast to CT T1w TSE clearly outlines the area of bone infiltration by recurrent NHL. It corresponds to an intense high uptake of 18F-FDG.
Teaching Points
The combination of PET and MRI can demonstrate the extent of bone marrow infiltration more clearly than PET/CT. Especially T1w TSE sequences outline the replacement of fatty bone marrow by malignant tissue better than CT.
Liver Metastasis of Adenocarcinoma of the Adrenal Gland
Clinical History
Thirty-five-year-old patient with adenocarcinoma of the left adrenal gland undergoing a staging examination.
Imaging Technique
Whole body PET/MR images acquired 46 min after iv injection of 359 MBq 18F-FDG, 67 kg.
4 beds × 4 min together with coronal T1w TSE and axial T2w haste fs. 1 bed (upper abdomen) a 15 min together with ax/cor T2 HASTE, ax EPI (DWI), ax T1-VIBE dynamic post i.v. Gd.
Findings
In the right liver lobe a large focal lesion that is hyperintense on T2-weighted sequence can be depicted. The lesion shows a hyperintense signal in diffusion-weighted imaging both at a low and a high b-value suggesting a restricted diffusion within a likely hypercellular lesion. There is intense focal uptake of 18F-FDG in PET. Both MRI and PET strongly indicate a liver metastasis.
Teaching Points
Diffusion-weighted MR imaging (DWI) is an important MR sequence for both detection and characterization of focal liver lesions. In malignant lesions often a restricted diffusion due to hypercellularity can be seen.
Liver Metastases of Colorectal Cancer
Clinical History
Sixty-one-year-old patient with known liver metastases of colorectal cancer and a history of partial liver resection and radiofrequency ablation.
Imaging Technique
Whole body PET/MR images acquired 46 min after iv injection of 357 MBq 18F-FDG, 73 kg.
4 beds × 4 min together with coronal T1w TSE and axial T2w HASTE fs. 1 bed (upper abdomen) a 15 min together with ax/cor T2 HASTE, ax EPI (DWI), ax T1-VIBE dynamic post i.v. Gd.
Findings
Adjacent to the ablation defect in the left liver lobe a circular enhancement can be seen in the arterial phase after i.v. administration of contrast material. Another area of focal enhancement is seen in the right liver lobe. Both regions show an intense uptake of 18F-FDG in PET and are highly suspicious of newly developed liver metastases.
Teaching Points
Dynamic contrast-enhanced MR imaging together with PET is a valuable tool in the detection of liver metastases, especially in patients with previous treatment either by surgery or focal ablative techniques like radiofrequency ablation.
Liver Metastasis of Rectal Cancer
Clinical History
Forty-six-year-old patient with rectal cancer undergoing a staging examination.
Imaging Technique
Whole body PET/MR images acquired 46 min after iv injection of 487 MBq 18F-FDG, 100 kg.
4 beds × 4 min together with coronal T1w TSE and axial T2w haste fs. 1 bed (upper abdomen) a 15 min together with ax/cor T2 HASTE, ax EPI (DWI), ax T1-VIBE dynamic post i.v. Gd.
In the left liver lobe a focal liver lesion is seen. It is hyperintense in DWI on both low (a) and high (b) b-value images reflecting restricted diffusion. In the portal venous phase the lesion shows peripheral enhancement (c). In addition intense focal uptake of 18F-FDG is seen (d). Both MRI and PET strongly indicate a liver metastasis
Findings
In the left liver lobe a focal lesion with restricted diffusion and peripheral enhancement is seen. There is intense focal uptake of 18F-FDG in PET. Both MRI and PET strongly indicate a liver metastasis. No additional focal lesions are seen.
Teaching Points
In patients with colorectal cancer accurate staging of liver metastases is of paramount importance as patients eligible for resection of metastases can be treated curatively. Combination of a dedicated MR protocol of the liver and 18F-FDG PET imaging is helpful regarding the detection of liver metastases.
References
Hutchings M, Barrington SF (2009) PET/CT for therapy response assessment in lymphoma. J Nucl Med 50(Suppl_1):21S–30S
Kwee TC, Van Ufford HMEQ, Beek FJ, Takahara T, Uiterwaal CS, Bierings MB et al (2009) Whole-body MRI, including diffusion-weighted imaging, for the initial staging of malignant lymphoma: comparison to computed tomography. Invest Radiol 44(10):683–690
Punwani S, Taylor SA, Bainbridge A, Prakash V, Bandula S, Vita ED et al (2010) Pediatric and adolescent lymphoma: comparison of whole-body STIR half-Fourier RARE MR imaging with an enhanced PET/CT reference for initial staging1. Radiology 255(1):182–190
Lin C, Luciani A, Itti E, El-Gnaoui T, Vignaud A, Beaussart P et al (2010) Whole-body diffusion-weighted magnetic resonance imaging with apparent diffusion coefficient mapping for staging patients with diffuse large B-cell lymphoma. Eur Radiol 20(8):2027–2038
Wu L-M, Chen F-Y, Jiang X-X, Gu H-Y, Yin Y, Xu J-R (2012) 18F-FDG PET, combined FDG-PET/CT and MRI for evaluation of bone marrow infiltration in staging of lymphoma: a systematic review and meta-analysis. Eur J Radiol 81(2):303–311
Abdulqadhr G, Molin D, Aström G, Suurküla M, Johansson L, Hagberg H et al (2011) Whole-body diffusion-weighted imaging compared with FDG-PET/CT in staging of lymphoma patients. Acta Radiol 52(2):173–180
Antoch G, Vogt FM, Freudenberg LS, Nazaradeh F, Goehde SC, Barkhausen J et al (2003) Whole-body dual-modality PET/CT and whole-body MRI for tumor staging in oncology. JAMA 290(24):3199–3206
Schmidt GP, Baur-Melnyk A, Herzog P, Schmid R, Tiling R, Schmidt M et al (2005) High-resolution whole-body magnetic resonance image tumor staging with the use of parallel imaging versus dual-modality positron emission tomography-computed tomography: experience on a 32-channel system. Invest Radiol 40(12):743–753
Liu J, Yang X, Li F, Wang X, Jiang X (2011) Preliminary study of whole-body diffusion-weighted imaging in detecting pulmonary metastatic lesions from clear cell renal cell carcinoma: comparison with CT. Acta Radiol 52(9):954–963
Lauenstein TC, Goehde SC, Herborn CU, Goyen M, Oberhoff C, Debatin JF et al (2004) Whole-body MR imaging: evaluation of patients for metastases1. Radiology 233(1):139–148
Schwenzer NF, Schraml C, Müller M, Brendle C, Sauter A, Spengler W et al (2012) Pulmonary lesion assessment: comparison of whole-body hybrid MR/PET and PET/CT imaging—pilot study. Radiology 264(2):551–558
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Eiber, M. et al. (2013). Lymphoma, Lung and other Tumors. In: Ratib, O., Schwaiger, M., Beyer, T. (eds) Atlas of PET/MR Imaging in Oncology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-31292-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-642-31292-2_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-31291-5
Online ISBN: 978-3-642-31292-2
eBook Packages: MedicineMedicine (R0)