Abstract
Risk stratification takes an extra level of importance in the context of geriatric surgery. Risk stratification is not only essential for predicting for perioperative morbidity and mortality, but equally important is to predict for return to baseline function. As such, successful surgery is predicated not only on survival but the ability of the patient to return to their desired level of function and independence. This chapter discusses both the traditional risk scoring systems as well as specific geriatric tools and includes a discussion on the concept of frailty.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
3.2 Introduction
Preoperative risk stratification for the elderly is extremely important and serves three functions:
-
1.
Assist in the decision to offer surgery or not
-
2.
Assist in the perioperative management of the patient
-
3.
Assist in presenting the patient with adequate information for informed consent
Of particular importance, and perhaps uniquely in the geriatric population, the decision to choose between a surgical intervention or not can be a complex process. Typically, when a patient is diagnosed with a malignancy that is resectable, surgery generally follows. However, in the geriatric population, one must consider whether the cure, i.e., surgical intervention to extend life, will compete with the patient’s expectation with regard to quality of life. If surgery can extend life but comes with a high risk of mortality and morbidity and result in a patient unlikely returning to their baseline function, then, is he or she better served by foregoing surgery and an extended but low-quality lifespan and instead choose to live a shorter lifespan but with a better quality of life? One must ask whether an otherwise high-functioning patient would desire surgery if there is a substantial risk that he or she will become bed bound or lose their independence permanently.
The second reason for the need for risk stratification is to allow for better perioperative management of the patient that chooses to undergo surgery. This allows recognition of specific physiological problems that may be better optimized preoperatively or require close postoperative monitoring. In the elderly patient, this is no simple task as a significant number of patients will present with more than one comorbidity and may be on multiple medications that will impact perioperative care. Coupled with age-related decreases in functional reserves, a thorough and holistic risk analysis can be a daunting task.
It also goes without saying that in order to provide patients with proper informed consent, the surgical risks and their likelihoods is a very important area of concern that requires adequate discussion prior to surgery. Moreover, the impact on the patient’s quality of life will need to be discussed in detail both for decision making and for the patient to make adequate plans for long-term postoperative care.
Lastly, one should also keep in mind the goals of treatment. It is certainly obvious that, if the patient has decided on surgery for treatment, the goals are to maximize the therapeutic benefit of the intervention leading to cure and to minimize perioperative morbidity and mortality. However, just as important, as alluded to previously, is for the geriatric patient to return to baseline function. In some ways, this goal is even more difficult than the others. As such, unique to geriatric surgery, is the need to document a patient’s baseline function, have a plan to return to this baseline, and measure if this occurs postoperatively.
3.3 General Risk Scoring Systems
A number of general risk scoring systems are in common use today. These are either physiological-based or organ system-specific systems that deal with perioperative morbidity and mortality.
3.3.1 ASA Physical Status Scoring System
In 1941, the American Society of Anesthetists made the first attempt by any medical specialty to risk stratify patients in the form of the ASA physical status classification system (Table 3.1). A three-person committee was tasked to develop a system to collect and tabulate anesthetic data. It is thus useful for record keeping and for statistical analyses looking at perioperative data. This widely used classification system determines risk solely on the basis of a patient’s preoperative history and is relatively easy to use.
Of note is that the ASA classification was not designed as a tool to predict postoperative morbidity or mortality. There is no attempt to quantify the risk. As such, it is a relatively crude instrument for the analysis of operative risk. However, there have been studies that have sought to validate the ASA scoring system and have shown that the ASA score does correlate with outcomes such as unplanned ICU admissions, cardiopulmonary adverse events, and prolonged hospital stay. As such, it is still widely used by anesthetists for perioperative planning.
In the context of geriatric surgery, it is important to note that age is not a criteria along with other important variables such as type of surgery, degree of weight loss, etc. As well, it is to be noted that this scoring system uses subjective measures as opposed to objective, measured indicators.
3.3.2 Goldman and Detsky Index
In an attempt to better determine and quantify risk, Goldman, in 1977, developed a risk assessment tool using nine variables to determine cardiac risk for noncardiac surgery patients (Goldman et al. 1977). Each variable is assigned a point value and a patient’s risk is determined based on the overall score (Table 3.2). The highest possible score in this system is 53. Based on this scoring scheme, patients can be classified into four distinct categories of risks (Table 3.3). His tool was derived retrospectively using a database of 1,001 patients.
This multifactorial tool certainly was a step forward from the ASA scoring system as it is an objective scale that is designed to give a predicted score. However, it only is designed to predict the possibility of a cardiovascular event and therefore will under evaluate the total mortality and morbidity risk. As well, the authors did not subsequently perform hypothesis testing after the score was developed. It is still a useful tool given the fact that cardiovascular problems are the most common comorbidity encountered in the geriatric population.
In 1986, Detsky further refined Goldman’s original system by adding newer criteria such as pulmonary edema (Detsky et al. 1986a) (Table 3.4). As well, a further attempt was made to incorporate the type of surgery that the patient was to undergo into the risk calculation. The surgical categories were major vascular surgery, orthopedic, intrathoracic/intraperitoneal, and minor surgery. This generated a pretest probability ranging from 1.6% to 13.6%. Then, a nomogram was used in conjunction with the modified multifactorial index to generate a posttest probability of a severe cardiac complication. Both the original Goldman index and Detsky index continue to be used, and web-based calculators are easily found and can be quickly used to calculate both scores and predicted risk of complications.
3.3.3 American College of Cardiology/American Heart Association Guidelines
Subsequently, the American College of Cardiology and the American Heart Association developed a joint guideline for preoperative cardiovascular evaluation for noncardiac surgery. The latest guideline was updated 2007 (Fleisher et al. 2007) and is available for download at http://content.onlinejacc.org/cgi/content/full/50/17/e159. Although the algorithm is not strictly a tool to calculate risk, it is a useful guide with respect to determining which patients may benefit or require further pre-optimization. One of the strengths of the tool is that that there is an emphasis on minimizing unnecessary procedures and tests, which would undoubtedly lead to a longer preoperative course.
3.3.4 POSSUM Scoring
Coming out of the need to develop a useful surgical audit tool to compare performance across hospitals, Copland in 1991 published a paper wherein they performed a multivariable analysis to determine independent risk factors affecting morbidity and mortality (Copeland et al. 1991). This led to the development of the Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM). The score comprises 12 preoperative and 6 intraoperative variables to predict for both mortality and morbidity (Table 3.5). Thus, a physiologic score based on the patient’s preoperative risk factors is combined with six intraoperative findings to give a more comprehensive predictor. Further analysis of this tool in the literature noted that the POSSUM score tended to overpredict mortality in low-risk patients.
Subsequently, Prytherch and colleagues developed a modification of the score known as the (Portsmuth) P-POSSUM (Prytherch et al. 1998). This score was developed in response to the short coming of overpredicting low-risk patient’s mortality and was based on the same data set used for the original POSSUM score. However, the P-POSSUM score tends to underestimate the risk in both the elderly and in emergency surgeries. Used together, the POSSUM score can be used for morbidity and the P-POSSUM is then used for mortality. Both of these scores have been validated as a tool for the use in general surgery and are widely used in the western world.
A further refinement to the POSSUM score is the Cr-POSSUM score (Table 3.6) that is specifically designed for use in colorectal surgery (Tekkis et al. 2004). Of the three, the Cr-POSSUM appears to predict mortality better than both of the above. Lastly, in 2010, Tran developed the E-POSSUM score that is further defined for use in the elderly population undergoing colorectal surgery (Tran et al. 2010). It has yet to be externally validated.
3.4 Geriatric Risk Assessment
What is of utmost importance with regard to the geriatric patient is that none of these above risk stratification systems deal with what Bernard Isaacs termed “the giants of geriatrics”: immobility, instability, incontinence, and cognitive impairment (Issacs 1997). Immobility of course is a big issue with regard to postoperative mobilization and the prevention of such conditions such as venous thromboembolism and pneumonia. Instability, of course, can lead to falls which again will cause other comorbidities such as fractures and, one of the most concerning problems, which is head trauma. Incontinence places the patient at risk of soilage and cross-contamination. And lastly, cognitive impairment is one of the biggest risks for postoperative confusion and delirium.
3.4.1 Charlson Weighted Comorbidity Index
It is therefore fitting to look toward the geriatric literature to better understand risk assessment in the geriatric population. One risk assessment tool commonly used in the geriatric population is the Charlson weighted comorbidity index (Charlson et al. 1987). This tool was initially developed to assess long-term mortality in this population of patients. However, subsequently, it has been used to predict outcomes for acute medical events such as a cerebral vascular accident. Furthermore, it has been adapted for use in the surgical arena in such diverse conditions such as transplantation, mesenteric ischemia, and also perforated diverticular disease. In the realm of colorectal surgery in particular, a recent study found that a comorbidity score higher than 5 predicted for a 5 times higher risk of morbidity.
The scale itself consists of a number of comorbidities that are given a weighted value (Table 3.7). The aggregate score thus gives the clinician a tool to quantify the burden of disease. Of note is that this is primarily a geriatrician’s tool and not a surgeon’s tool.
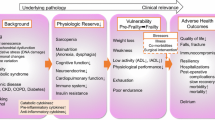
3.4.2 Frailty
A more recent and emerging concept is that of frailty. Frailty is fast becoming as recognized as another “giant” of geriatrics as the term tries to capture the overall patient’s hardiness and resilience to injury (Crome and Lally 2011). The core concepts of frailty are not in doubt, and there is consensus that frailty is a condition in which patients have impairments in multiple, interrelated systems that lead to increased vulnerability to physiological challenges and stressors. There is a loss of resiliency due to decreased functional reserves. What is interesting in regard to this concept is that it is not necessarily comorbidity based. There are patients who have multiple comorbidities and are not frail, but conversely, there are patients who have no comorbidities but are frail.
Where there is a lack of consensus is how frailty should be defined. In the literature, the most commonly cited definitions are by Fried and Rockwood. Fried’s model (Fried et al. 2001) is based on the assessment of five physical indicators: weight loss, walking speed, grip strength, physical activity, and exhaustion (Table 3.8). A finding of impairment in three or more categories meets the diagnosis of frailty. The scale has been shown to predict for falls, disability, hospital admission, and mortality. Most recently, our institution has shown that that in patients who meet the criteria for frailty, the odds ratio related to postoperative major complications was fourfold (4.083 [CI 1.433–11.638]) (Tan et al. 2011). A recent study by Makary using the Fried criteria found that it predicted for postoperative complications, length of stay, as well as discharge from hospital into a facility (Makary et al. 2010).
Some drawbacks to the Fried model are that it is difficult to apply to patients who are acutely ill and that it lacks direct measurement of mental health and psychosocial status.
Rockwood’s model proposes that the risk of becoming frail is related to the development of certain deficits. As such, as more and more deficits accumulate, the greater the risk of frailty will be. However, the model has yet to be fully accepted in the clinical setting and has not been tested in the surgical literature (Rockwood et al. 2005).
3.4.3 Baseline Function
The various standard systems noted previously reflect the typical risk stratification tools that measure the risk of mortality and perioperative complications. However, one of the biggest critiques of the state of geriatric surgery is that outcomes studies are missing the mark and that these outcome measures of morbidity and mortality, though extremely useful, do not address possibly the biggest concern of the geriatric population: what will be the quality of life after surgery? Surgeons are adept at looking into morbidity and mortality rates to best contemplate whether a surgical intervention is worthwhile and can compare it to the natural history of the disease as well as the possibility of cure based on the tumor type and surgical procedure. What is not commonly addressed both by surgeons and the literature is what is the rate of return to baseline function and, hence, quality of life after surgical intervention. There is a need to remind caregivers that health is not merely absence of disease or cancer in this case, but the state of complete physical, mental, and social well-being. As well, the affect on postoperative function can have a direct impact on survival that is separate from any tumor stage considerations.
Currently, there is a dearth of tools and knowledge as to the affect that colorectal rectal surgery has on quality of life and return to baseline function. At the minimum, any surgical unit that performs geriatric surgery should consider using a tool such as Barthel’s activities of daily living index (Table 3.9) to use as a baseline score and then follow this out postoperatively and to collect this data prospectively to better understand and quantify the impact that surgery has on baseline function. This will continue to be an ever expanding area of inquiry and concern. The aim, of course, is to be able to nurture patients back to their baseline function should they decide on surgery.
3.4.4 Comprehensive Geriatric Assessment
The above three parameters form part of a comprehensive assessment which has potential implications that are wider than surgical risk assessment alone and thus have been mentioned in other chapters in this book as well.
3.5 Conclusion
With the myriad of tools that have been developed, colorectal surgeons should become familiarized with at least one physiological scoring system and one that looks at frailty. At this time, the best tools available appear to be the Cr-POSSUM score as well as Fried’s frailty index. Using a combination of these tools will allow the clinician to better consider the appropriateness of surgery for each individual patient and also use this information to better allow the patient to give informed consent.
An increasing emphasis needs to be placed on the patient’s return to baseline function. We need to expand our definition of surgical success not only on tumor cure and absence of morbidity and mortality, but also on the patient’s ability to return to their prior level of function. For patients who are undergoing surgery, Barthel’s index should be used to document baseline function and subsequently allow for postoperative goal setting as well as quality assurance. As hinted above, having a geriatrician as an active part of the team is invaluable and the use of the Charlson index can be added.
As the geriatric population increases, the need for more colorectal surgery will also increase and more and better tools will be required to better help select which patients will benefit from surgery. The need though is for better tools to predict not just morbidity or mortality, but to also predict for quality of life and the ability of the patient to return to baseline function. A further challenge is for the development of effective tools to mitigate and/or alleviate the problem of frailty. As such, all colorectal units have an obligation to prospectively collect and routinely analyze their data to develop newer and better protocols to treat the elderly patient with colorectal cancer.
References
Saklad M (1941) Grading of Patients for Surgical Parodures. Anesthesioloygy 2(3);272–280
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78(3):355–360
Crome P, Lally F (2011) Frailty: joining the giants. Can Med Assoc J 183(8):889–890
Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR (1986a) Cardiac assessment for patients undergoing non cardiac surgery: a multifactorial clinical risk index. Arch Intern Med 146:2131–2134
Detsky A, Abrams HB, McLaughlin JR, Drucker DJ, Sasson Z, Johnston N, Scott JG, Forbath N, Hilliard JR (1986b) Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1(4):211–219
Fleisher LA et al (2007) ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 50:e159–e242
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a pheno- type. J Gerontol A Biol Sci Med Sci 56(3):M146–M156
Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, Burke DS, O’Malley TA, Goroll AH, Caplan CH, Nolan J, Carabello B, Slatter EE (1977) Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 297(16):845–850
Issacs B (1997) The challenge of geriatric medicine. Oxford University Press, Oxford
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried P (2010) Frailty as a predictor of surgical outcomes of older patients. J Am Coll Surg 39:412–423
Prytherch DR, Whitely MS, Weaver PC, Prout WG, Powell SJ (1998) POSSUM and Portsmouth POSSUM for predicting mortality. Br J Surg 85(9):1217–1220
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 173:489–495
Tan KY, Kawamura YJ, Tokomitsu A, Tang T (2011) Assessment for frailty is useful for predicting morbidity in elderly patients undergoing colorectal cancer resection whose comorbidities are already optimized. Am J Surg [Epub ahead of print]
Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, Windsor AC (2004) Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg 91(9):1174–1182
Tran BLP, du Montcel ST, Duron JJ, Levard H, Suc B, Descottes B, Desrousseaux B, Hay JM (2010) Elderly POSSUM, a dedicated score for prediction of mortality and morbidity after major colorectal surgery in older patients. Br J Surg 97(3):296–403
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Woo, E.CH., Tan, KY. (2013). Risk Stratification for Elderly Surgery. In: Tan, KY. (eds) Colorectal Cancer in the Elderly. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-29883-7_3
Download citation
DOI: https://doi.org/10.1007/978-3-642-29883-7_3
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-29882-0
Online ISBN: 978-3-642-29883-7
eBook Packages: MedicineMedicine (R0)