Abstract
The preoperative evaluation of the geriatric clearly presents unique challenges. Historically, risk stratification has focused on a single organ system. In the geriatric patient the combined effects of frailty, comorbidity, and disability contribute cumulatively to poor outcomes. Age, cognitive dysfunction, falls, malnutrition, and anemia are all markers for poor outcome in the geriatric patient. After completion of the geriatric workup, a complete picture of the patient’s overall health in all domains will be completed. The combined and cumulative effects of these markers provide a more powerful tool for the prediction of mortality, functional recovery, and institutionalization following surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Continuous Positive Airway Pressure
- Surgical Site Infection
- Geriatric Patient
- Advance Directive
- Frailty Index
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The elderly are the most rapidly enlarging segment of the population due to the combined effects of the “baby boom,” the population growth during the two decades after World War II, and the increase in life expectancy; this increased life span has become the burden of chronic disease and disability [1]. These trends in the aging of the population have resulted in parallel growth in the number of patients undergoing operation, with elderly patients comprising a significant percentage of the surgical workload [2]. Over 20 % of elderly patients undergoing surgery develop in-hospital complications, primarily involving the cardiovascular, neurologic, and pulmonary systems [3]. These complications significantly affect outcomes, with a substantial increase in-hospital length of stay. Over twice as many patients will be discharged to a skilled nursing facility or nursing home than those elderly patients without complications, often due to a reduced ability to perform activities of daily living. Complications result in a significant reduction in physical functioning, mental, and emotional health when compared to the general elderly population [4]. In addition, in-hospital complications result in substantially increased costs [5]. Need for operation has increased in the very elderly, with patients over the age of 80 making up a growing percentage of operative patients. These patients are more likely to undergo emergency operations with associated higher surgical risk. In this population one in five will experience complications, leading to mortality in 25 %, with comorbid illness playing a greater role in outcome than age. The increase in mortality associated with complications is even more dramatic, and thus their avoidance even more important [6, 7]. Many of these risk factors can be identified during the preoperative period, allowing the surgeon to employ strategies for their avoidance, and proper counseling of patients and families.
General Evaluation
History and Physical
Preoperative assessment of the elderly patient, similar to any patient, begins with a careful and thorough history. The history is the most expedient and sensitive method to determine the presence of comorbid conditions, and the extent to which these conditions limit the patient. The importance of this phase cannot be overstated. Pay special attention to cardiac, pulmonary, renal, and neurologic conditions, as these are most likely to impact management in the operating room and the perioperative period. In addition, preoperative interventions may help limit the impact of these comorbidities. The use of medications and supplements should be sought in detail. This allows appropriate management in both the perioperative and postoperative periods. Finally, signs and symptoms of activity-limiting cardiac and pulmonary conditions should be investigated.
The effects and extent of comorbid illness can be determined during the physical examination. Pay special attention to both cognitive and physical function in the elderly, as limitations in these areas predict postoperative complications. In the emergency situation with the obtunded or demented patient, the physical examination may be the only perioperative evaluation possible. The signs of significant cardiac, pulmonary, or hepatic dysfunction can be readily observed when present. Surgical scars can provide a basic surgical history. The stigmata of malnutrition and frailty can be easily identified.
After completing the history and physical, a general sense of the operative and perioperative risks has usually been determined; history and physical alone can determine fitness for surgery in up to 96 % of patients [8]. At this point, the remainder of the assessment will be determined by those comorbid conditions identified during the history and physical as well as the urgency of operation. The remainder of the evaluation discussed below will attempt to describe optimal evaluation of the geriatric patient. Emergency surgery rarely allows a complete assessment, but the information gleaned to this point will guide the remainder of the preoperative evaluation.
Basic Labs and Tests
The laboratory assessment and basic testing should be determined by the history of comorbid conditions, symptoms experienced by the patient, findings on physical examination, and the use of certain medications. Laboratory assessment in the healthy, asymptomatic patient has little value. The presence of abnormalities is low, and these findings rarely alter the intraoperative management of patients [9–11]. Despite these observations, numerous laboratory assessments are frequently ordered in geriatric patients. Each of these common tests will be addressed, with attention paid to their indications and implications in the geriatric patient (Table 10.1).
Medications and Supplements
General Considerations
A thorough medication history should be sought from all patients. This includes prescription medications and indication, over-the-counter medications, vitamins, and herbal supplements. Over 80 % of elder adults take at least one medication, and one-third take at least five medications. This becomes especially prevalent in those 75–85 years of age. Compounding potential adverse events related to medications, nearly half of all elders use at least one over-the-counter medication, and nearly half use some sort of dietary supplement [22]. Polypharmacy can be defined by either the absolute number of drugs taken or the use of medications without appropriate indication or the use of duplicate medications. Inappropriate prescribing may be present in half of older adults, and contributes to cognitive impairment, falls, incontinence, and impairment [23]. All unnecessary medications should be discontinued in the perioperative period.
When considering medication use in the perioperative period, consider the potential for withdrawal from the medication, potential progression of disease while the medication is not administered, and the potential for interactions with anesthetic agents. Abrupt discontinuation of medications may lead to complications from withdrawal syndromes which include selective serotonin reuptake inhibitors (SSRIs), beta-blockers, clonidine, statins, and corticosteroids. Other drugs such as tricyclic antidepressants, benzodiazepines, MAO inhibitors, and antipsychotics are generally deemed safe in the perioperative period and need not be discontinued. ACE inhibitors and angiotensin receptor blockers should be continued unless the only indication is for hypertension and this is well controlled [24]. Drug therapy may be predictive of postoperative complications, but withholding of regular medications, especially those used to treat cardiovascular disease, also increases complications. The rate of complications, especially cardiac, increases with the time the patient is off the medication. All essential medications discontinued at the time of surgery should be resumed as soon as safely possible during the postoperative period [25].
Beta-Blockers
Recent enthusiasm for the use of perioperative beta-blockade has been tempered by the findings from a large-scale study which demonstrated that despite significant reduction in cardiac events and myocardial infarction, an increase in both stroke and death in patients treated with metoprolol was observed [26]. The current recommendations for perioperative beta-blocker therapy are:
-
1.
Beta-blockers should be continued in patients undergoing surgery who are receiving beta-blockers for approved indications.
-
2.
Beta-blockers titrated to heart rate and blood pressure are indicated in patients undergoing vascular surgery with high risk due to coronary artery disease or the presence of ischemia on preoperative testing.
-
3.
Beta-blockers titrated to heart rate and blood pressure are reasonable for patients in whom cardiac disease is discovered in preoperative evaluation or who have high cardiac risk based on the presence of more than one risk factor undergoing intermediate-risk surgery [18].
Statins
Numerous studies of perioperative statin use in patients undergoing noncardiac surgery and coronary artery bypass grafting have been conducted, and the majority of these have shown that statins are beneficial in surgical patients, with reduction in mortality and myocardial infarction. Long-term mortality may also be improved by the use of statins in the perioperative setting. The current recommendations for the use of statins are:
-
1.
Statin therapy should be continued in all patients currently taking statin medications.
-
2.
Statin use is reasonable in patients undergoing vascular procedures.
-
3.
Statin use should be considered in patients undergoing intermediate-risk procedures when at least one clinical risk factor is present [18].
-
4.
Statins should be initiated as soon as possible in any patient who has an acute coronary event postoperatively.
-
5.
It is reasonable to continue use for at least 72 h in those patients receiving statins for perioperative use only [27].
Corticosteroids
Steroids should be continued when possible during the perioperative period. Withholding these drugs for 36–48 h before surgery is predictive of the need for stress dose steroids due to hypotension. When the routine dose of steroids is continued during the perioperative period, patients do not require stress doses of steroids. Stress dose steroid use is only required when patients are being treated for primary failure of the hypothalamic-pituitary-adrenal axis [28].
Supplements
The use of supplements by patients has been found in 30 % of the surgical population, and use is increasing. These same studies have found that 70 % of the patients taking these preparations failed to disclose their use during the preoperative assessment unless specifically asked. Excessive bleeding, myocardial infarction, excessive and inadequate anesthesia, or interference with needed therapeutic drugs have been documented for these supplements [29]. These supplements have various durations of effect, but the safest measure is to discontinue use 7 days prior to surgery when possible and be aware of the potential complications so they may be managed adequately [24] (Table 10.2).
Mental Status and Cognitive Function Assessment
Dementia and Cognitive Impairment
Cognitive impairment and dementia are increasingly prevalent in the elderly population. Cognitive impairment without dementia is estimated to occur in 22 % of patients age 71 or older. This prevalence is greater than that of dementia. Prominent subtypes include prodromal Alzheimer’s disease, cerebrovascular disease, stroke, and adverse effect of medication. These findings are significant, as 12 % of the patients found to have cognitive impairment will progress to dementia annually. More importantly, mortality increases from 8 % in the cognitive impairment without dementia to 11 % in the group with dementia [30]. The prevalence of dementia among persons older than 71 years is 14 %. The prevalence increases dramatically with age in this group, from 5 % in those aged 71–79 years, to 37 % in the over 90 cohort [31], and to greater than 40 % in those 100 years or older [32].
The presence of cognitive impairment dramatically increases postoperative complications and negatively influences short- and long-term outcome. Baseline cognitive impairment and dementia are strong predictors for delirium in the postoperative period [33–36], and thus increase the risk of postoperative functional decline [33] and mortality [36].
During the preoperative evaluation the presence and severity of cognitive impairment should be documented if possible. Numerous tests have been developed to screen for cognitive impairment, including the Mini-Mental State Examination (MMSE), the Memory Impairment Screen (MIS), and the Mini-Cog. These tests have shown a wide range in sensitivity and specificity, and more importantly for the acute care surgeon, the time and training required to administer ranges from 1.5 to 17 min [37]. The Mini-Cog, a brief screen that employs 3-item recall and a clock drawing task, has sensitivity and specificity of 99 and 96 % and can be administered in 3 min. This strikes the best balance between accuracy and ease of administration in the acute setting [38].
Delirium
The incidence of delirium has been reported at 5–52 % in a number of studies including a broad selection of surgical patients [39]. The usual onset is 2 days following operation and persists an average of 4 days [36]; the occurrence of delirium results in increased length of stay in the hospital [36, 40, 41]. Patients are also more likely to experience functional decline and impairment in the performance of activities of daily living [33]. This results in a higher likelihood of discharge to a skilled nursing or rehabilitation facility [36, 40]. Finally, mortality rates are increased for both in hospital [41] and the months following discharge [36, 40, 42].
With its profound impact on morbidity and mortality, identification and prediction of postoperative delirium has been the subject of numerous studies. It is hoped that with identification of patients at risk, measures may be taken to mitigate delirium and prevent its consequences.
Once risk factors for delirium have been identified, those that can be corrected should (Table 10.3). In the postoperative period, numerous medications have been identified which contribute to delirium and should be avoided. These include meperidine, benzodiazepines, antihistamines, and anticholinergics. Opiates should be used with caution, but pain must be adequately controlled, as this too is a risk factor for delirium [46, 47]. Some studies have shown that preoperative geriatrics consultation has been helpful to reduce the incidence of delirium. Other small trials of prophylactic antipsychotic administration have had promising but conflicting results, and their use cannot be advocated at this time [48].
Depression
The incidence of depression in those aged 71 or greater is estimated to be over 11 %, based on the presence of major or minor depressive symptoms or current treatment for depression. Dementia and pain perception are associated with increased incidence [49]. Other risk factors for depression in the elderly are disability, new medical illness, poor overall health, and bereavement [50]. In studies of patients undergoing cardiac surgery, depression has been identified as a risk factor for mortality [51]. Preoperative depression is also associated with a longer recovery time due to delayed recovery in activities of daily living (ADL) and instrumental activities of daily living (IADL) [52]. Screening for depression may be accomplished using a variety of tools. The Patient Health Questionnaire-2 (PHQ-2) is a simple and reliable screening tool for depression in the elderly. Two questions are asked in this survey. First, “In your entire life, have you ever had a time when you felt sad, blue, depressed, or down for most of the time for at least 2 weeks?” Second, “In your entire life, have you ever had a time, lasting at least 2 weeks, when you didn’t care about the things that you usually cared about or when you didn’t enjoy the things that you usually enjoyed?” A positive response to either of these questions is suggestive of depression, with 100 % sensitivity and 77 % specificity [53]. When positive, the patient should be referred for evaluation when time and the patient’s medical condition allow.
Substance Abuse
A 2005–2006 epidemiologic study on the use of alcohol and drugs of abuse demonstrated that 60 % of adults over age 50 used alcohol in the year prior to the survey, 2.6 % used marijuana, and 0.41 % used cocaine [54]. Furthermore, at-risk and binge drinking is also prevalent in the elderly population, with 13 % of men and 8 % of women reporting at-risk drinking, and 14 % of men and 3 % of women reporting binge drinking [55]. The effects of preoperative alcohol use include increased risk of pneumonia, sepsis, surgical site infection (SSI) and wound disruption, and longer length of stay. With the exception of SSI, all of these factors are associated with increased mortality [56]. Exposure to alcohol may also increase the stress response to surgery and increase morbidity [57].
All patients should be screened for alcohol misuse. A simple tool is the CAGE questionnaire. This involves four questions, and a positive answer to one or more is suggestive of alcohol abuse (Table 10.4).
When identified, patients with at-risk alcohol history should be supplemented with folic acid and thiamine (100 mg) daily. Care protocols should include frequent assessment for withdrawal and appropriate medications or alcohol administered to avoid withdrawal in the postoperative period.
Nutritional Evaluation
Malnutrition is prevalent in the elderly and has a major impact outcome in surgery. Overall, malnutrition is present in 22.8 % of the elderly, ranging from 5.8 % in community dwelling elders to over 50 % in patients in rehabilitation. Another 46 % of elders are at risk for malnutrition [60]. In the surgical patient, malnutrition is a risk factor for multiple complications, generally related to infection and poor wound healing, and for increased length of stay [61]. During the preoperative evaluation the patient’s height and weight should be documented. In addition, serum albumin and prealbumin levels should be obtained [12, 13]. The occurrence of any significant unintentional weight loss should be sought. Risk factors for severe malnutrition and related complications include serum albumin <3.0 g/dL BMI <20 kg/m2, prealbumin <10 mg/dL, or unintentional weight loss of >10 % in 6 months [62–66]. The presence of any of these should prompt full nutritional assessment, and when possible a strategy to treat deficits in the perioperative period devised.
Cardiac Evaluation
The cardiac evaluation of the geriatric patient is an essential part of the initial assessment when time permits. Major cardiac complications occur in 2 % of patients aged 50 years or greater [15]. The incidence of adverse cardiac events increases with age [67]. Emergency operation is associated with a significantly increased risk of postoperative cardiac complications [68]. Other risk factors include high-risk procedures, history of congestive heart failure, history of ischemic heart disease, history of cerebrovascular disease, treatment with insulin, and preoperative serum Cr >2.0 mg/dL. These risk factors are additive in their prediction of cardiac events [15]. Hospital mortality is 15–25 % after perioperative myocardial infarction, and the risk of death persists for at least 6 months following operation [69]. The current ACC/AHA recommendations (Fig. 10.1) for cardiac evaluation should be followed in geriatric patients.
Approach to cardiac evaluation and care prior to noncardiac (Fleisher et al. [118]). †See Class III recommendations in Section 5.2.3. Noninvasive Stress Testing. §Noninvasive testing may be considered before surgery in specific patients with risk factors if it will change management. ‡See Table 3 for estimated MET level equivalent
Pulmonary Evaluation
Pulmonary complications occur as frequently as cardiac complications in the postoperative period. Recent studies report an incidence of 2.7–5 % of patients will experience respiratory complications after non-thoracic surgery [70–73]. Postoperative respiratory complications are associated with a higher risk of myocardial infarction, pneumonia, renal failure, thromboembolic complications, or death. The cost of pulmonary complications is greater than any other adverse events, in part due to an increased length of hospital stay [74]. During the preoperative assessment, risk factors for pulmonary complications should be identified. Risk factors may be either patient or procedure related. Table 10.5 shows identified risk factors. Preoperative spirometry is not helpful to predict postoperative complications [75].
When high-risk patients are identified, several strategies may be employed for risk reduction. These include lung expansion techniques such as incentive spirometry, intermittent positive pressure breathing, continuous positive airway pressure, and chest physiotherapy [76]. Preoperative inspiratory muscle training using individualized combinations of these techniques has been shown to reduce pulmonary complications in patients with concomitant coronary artery bypass surgery [78]. With regard to the anesthetic, residual neuromuscular blockade predicts postoperative complications, and longer-acting agents such as pancuronium should be avoided [79]. When possible, nerve blocks for regional anesthesia are less likely to cause complications than general anesthetic [76]. Laparoscopic techniques may have some value in limiting pulmonary complications when compared to open techniques. Nasogastric tubes should be used selectively, as routine use is associated with increased complications. Following celiotomy, continuous positive airway pressure and the use of epidural analgesia are shown to reduce complications [74]. Of note, preoperative smoking cessation has only been shown to reduce complications when done 1–2 months prior to surgery [75, 80–82].
Functional Status Determination
The patient’s functional status should be determined during the preoperative evaluation. The ADL index involves functional independence in six areas: bathing, dressing, transferring, feeding, continence, and toileting [83]. A simple screening tool involves the following four questions: “Can you get out of bed yourself?” “Can you dress yourself?” “Can you make your own meals?” and “Can you do your own shopping?” [84]. A negative response to any question should prompt a more thorough evaluation of functional capacity, and the deficits should be documented. Other limitations should be documented, such as deficits in vision and hearing, as well as the use of assistive devices. A history of falls should be documented [12]. Physical disability can be assessed using the timed “Up & Go” test. A patient is instructed to rise from a chair, without using arms, and possibly walk 10 ft, turn, return to the chair, and sit down. A time greater than 15 s is suggestive of a high risk for falls [85, 86].
Poor functional status and impaired mobility are associated with postoperative delirium [40], surgical site infections due to methicillin-resistant Staphylococcus aureus [87], discharge to another level of care [88], and mortality [6, 83]. Preoperative functional status is also predictive of the time to postoperative recovery following abdominal surgery [52].
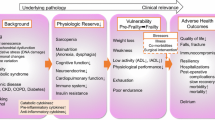
Frailty
Frailty is defined as a state of reduced physiologic reserve associated with increased susceptibility to disability [83]. Frailty manifests as age-related vulnerability to stressors secondary to this decrease in physiologic reserve and limits the maintenance of homeostasis. While similar in some ways to normal aging, it is a distinct entity [89]. Impairments associated with the frailty syndrome include sarcopenia, functional decline, neuroendocrine dysregulation, and immune impairment occurring in combination. The associated risk with the syndrome as a whole predicts poor outcomes greater than any single component, and no single component explains the entire spectrum of the manifestations. A physical phenotype was first defined in 2001; however, there is strong evidence to support additional domains to the model (Table 10.6). These include cognitive impairment, chronic diseases, and disability [90]. The overall prevalence of frailty in the United States ranges from 7 to 12 %. The prevalence increases with age, from 3.2 % in those age 65–70 years to over 25 % in the group aged 85–89 years. Frailty is more common in women across all ages [91, 92].
Confusion over the exact definition and characteristics of frailty has resulted in the development of multiple definitions and screening tools. A Frailty Index was developed using the Comprehensive Geriatric Assessment (FI-CGA), which included measurements of impairment, disability, and comorbidity, which were scored and summed as a Frailty Index [93]. Although reliable and predictive of adverse outcomes, it is time consuming and not readily applied to the acute care surgery patients. The Canadian Study of Health and Aging Frailty Index involves up to 70 deficits, which is again a powerful predictive tool, but not widely used in clinical practice [94]. Regardless of the method used to screen for frailty, it is clear that it has a significant impact on the incidence of complications, mortality, and institutionalization [88, 95]. Once identified, the presence of frailty can help the surgeon counsel patients and families appropriately and modify the interventions proposed to minimize complications. Exercise and rehabilitation may also improve functional state [96]. When combined with physical exercise, nutritional interventions have also shown an improvement in functional abilities [97].
One of the most widely used assessments tools for defining frailty is the operational definition proposed by Fried. This involves five areas of physical performance shown in Table 10.6. The presence of frailty as defined by this method was predictive of falls, worsening mobility, and disability in activities of daily living, hospitalization, and death [92]. When this same method was applied to surgical patients, frailty increased risks for postoperative complications, with an odds ratio of 2.06 in the intermediate-frail group and 2.54 in frail patients. Length of stay was increased as well. Finally, discharge to a skilled- or assisted-living facility was increased, odds ratio of 3.16 in the intermediate group and 20.48 in the patients after operation [98].
Another tool which may be more easily applied in the acute setting is the Modified Frailty Index (MFI). This index system was created by the comparing the 70-item Canadian Study on Health and Aging Frailty Index with data from the National Surgical Quality Improvement Project (NSQIP) data set. The items included are shown in Table 10.7. One point is given for each feature present, and the total, divided by the number of variables for which the patient had data, produced results from 0 to 11, increasing frailty with higher total. In patients over age 60, undergoing emergency general surgery, the score was predictive of mortality, with a tenfold increase in mortality at the extremes of age. The incidence of infections also rose as the MFI increased. The benefits of this system include rapid application through history and physical, ease of employment in the acute setting, and the lack of requirement for any specialized equipment [99].
Patient Preferences, Counseling, and Advance Directives
Determination of Competency
Physicians must legally and ethically obtain informed consent from their patients before undertaking any procedure. The conditions that result in impaired decision capacity are common in the elderly patient, and the surgeon must be aware of their presence and skilled in evaluating that capacity. Conditions known to impact decision-making capacity include cognitive impairment, stroke [100], and psychiatric conditions such as schizophrenia, depression, or bipolar disorder. The general requirements for decision-making capacity are the ability to express a choice, understand pertinent information, understand the consequences of the procedure and those of foregoing treatment, and to be able to reason about these choices [101].
No single test has been shown to correlate with decision-making capacity. The Mini-Mental State Examination (MMSE) has been shown to correlate with this capacity, but without definite cutoff scores to determine capacity, although very-low (<19) and very-high (>23) scores predict absence or presence of capacity, respectively [102]. When the patient is deemed incompetent to make health-related decisions and an advance directive is not in place, the physician must seek substituted judgment, usually from a family member. Although the order may vary from state to state, the usual order is the spouse, adult children, parents, siblings, and other relatives [101].
Counseling Patients
Three things are usually taken into consideration as patients consider treatment options: treatment burden, treatment outcome, and the likelihood of the possible outcomes. When outcome is likely to be favorable, patients are typically willing to tolerate a greater treatment burden; however, this diminishes as outcomes show only marginal benefit. Quality-of-life outcomes such as prolongation of inevitable death, dependence on machinery, functional dependence, and excessive fatigue and pain are cited as important factors in patient’s decisions. Nonmedical concerns, such as becoming a burden on the family or society, also influence these decisions [103]. Preparation for death, both by the family and the patient, is valued and important to the family and patient; however, physicians tend to place less emphasis on this aspect of end-of-life care. Patients appreciate being told the expected course of their disease, the symptoms they will experience, the time course, and what can be done for them. Finally, a sense of life completion is desired by patients, and adequate, timely communication may allow this to mature [104, 105]. Achieving the last of these goals may be difficult for the acute care surgeon. Our practice, by its nature, frequently encounters patients in a situation that is a clear departure from their usual state of health. While those patients receiving palliative care are aware that they are terminally ill, the patient suffering an acute catastrophic event has not had the luxury of time for preparation.
Advance Directives and DNR Orders in the Operating Room
According to Medicare data, nearly one-third of Americans underwent surgery during the last year of their life. Further, 18 % underwent procedures in the last month of life and 8 % during the last week of life [106]. The acute care surgeon must understand issues surrounding end-of-life care, especially the application of advance directives and “do not resuscitate” orders. The application of DNR orders and advance directives in the operating room was initially met with significant resistance [107]. Prior to the 1990s, policies for handling these directives were rare, and the usual practice was to suspend the DNR order in the OR and the immediate postoperative period. Forcing patients to give up their autonomy to qualify for surgery drew criticism [108, 109]. This led to the policy of “required reconsideration,” meaning that the patient or surrogate, surgeon, and anesthesiologist must discuss and review the advance directive together. This was formalized by the American Society of Anesthesiologists (ASA) in 1993. Following this discussion, the DNR order could be formally rescinded with the patient’s informed consent; it could be left in place, specifying the patient’s goals of care; or it could be left in place with a detailed list of exactly what procedures the patient would allow [110]. The American College of Surgeons (ACS) echoed the views of the ASA. In their statement, they also stated that the automatic reversal of DNR status in the OR removed the patient from appropriate participation in the decision process and that inappropriate management in the perioperative setting might result [111].
As many as 15 % of patients with DNR orders will undergo surgery, either related to their preexisting illness or for treatment of unrelated conditions [112]. The procedures offered may be intended to either prolong life or ease suffering and improve quality of life. Many of these procedures fall within the scope of acute care surgery, and examples may include the repair of pathologic fractures, tracheostomy and feeding tube placement, treatment of bowel obstruction, vascular access, or a wide variety of others [110, 113]. A study of patients with DNR orders in place showed that the presence of the order did not affect the likelihood that patients would undergo the procedure considered. In only 18 % of the patients was the DNR order reversed. Half of the patients undergoing surgery with a DNR order in place were discharged from the hospital, and 44 % were alive 2 months following hospital discharge [113].
A Practical Approach to Working with Patients
When a patient presents for surgery with a DNR order in place, the physician must not only consider the risks and benefits of the specific procedure but also take the time to learn the values and goals of treatment for the patient. Communication is the key to resolving the complexities surrounding perioperative resuscitation. When discussions occur, the provider may learn the patient’s rationale for the DNR order. Frequently, the patient is far more concerned with the quality of life after CPR, not before. When the surgeon understands the goals and fears of the patient, a contingency plan can be developed and implemented. Looking into these concerns may show that the patient is afraid of a long stay in the ICU or of losing independence, not wanting to spend the remainder of his life in a nursing home. By learning these fears, the surgeon and care team may adjust therapy and form appropriate plans. Surrogate decision makers and the anesthesiologist should be included in these discussions [114]. The addition of the surrogate will assist in ensuring that patient’s wishes are respected, as it is not infrequent that the surrogate and the patient may not share the same goals and decisions [115]. During these discussions three options are available: rescinding the DNR order, providing limited resuscitation using a procedure-directed DNR order, and providing resuscitation with a goal-directed order.
The first option is to rescind the DNR order and provide full resuscitation regardless of clinical circumstances. This avoids the question of determining what exactly constitutes resuscitation, which may prove difficult during anesthesia. In addition, it frees the treating team to act in the event of an easily reversible or iatrogenic arrest, such as an arrhythmia on induction of anesthesia. Chances for an acceptable quality of life are better during these witnessed events [116], and care may be withdrawn later if the outcome in unfavorable. Despite all of the concern for ethics, this is a viable and appropriate course of action so long as the patient is involved in the decision.
A procedure-directed DNR order may be developed by the patient and surgeon. In this type of order, patients may specify which procedures and interventions for which they will and will not give consent. This is appealing to some patients, as they prefer the control of being able to dictate exactly which procedures will and, more importantly, will not be performed. This imitates the type of orders most commonly employed on hospital wards. The patient may be presented with a list of possible interventions. Frequently included items are intubation, postoperative ventilation, CPR, defibrillation, vasoactive drugs, and placement of invasive monitoring devices. When adapting these lists and preparing for the OR environment, interventions deemed mandatory for anesthesia are discussed with the patient, as they may not be refused [111]. Despite these procedure-specific orders being clear and easily understood, they do not allow for all the clinical circumstances which may arise, or those that may be difficult to document and define preoperatively [117].
The final approach to DNR orders in the OR is to take a goal-directed approach. In this scenario, the physician is left to determine which specific procedures should be performed in the event of cardiac arrest or instability. To supplant his own judgment for that of the patient, the surgeon must know the patient’s concerns regarding resuscitation and outcome. Are they worried about pain, neurologic damage, loss of independence, or the need for further surgery and procedures? By knowing the answers to these questions, the physician is able to respond appropriately. For example, if a patient sustains an arrhythmia on induction that requires brief support with CPR, it would be administered, as outcome is likely to conform to the patient’s wishes. Conversely, if the patient experiences a massive intraoperative myocardial infarction and arrest, CPR could be withheld, also supporting the patient’s values. This approach to DNR is perhaps the most in line with preserving patient autonomy and allowing values held by the patient to be considered. The translation from theory to practice is not quite as easy. First, the surgeon and patient must understand each other, and this requires time that is not always present in emergency situations. In addition, the person responding to the arrest situation should be the same person who had the discussion with the patient. Clearly this is not the case for patients on hospital wards, but the OR, better than other places, provides for this continuity in care. When the continuity of care cannot be preserved, or when the trust required between patient and surgeon is not present, it is best to rely on a procedure-directed approach. When the goal-directed approach is taken, documentation in the medical record is essential. This will usually take the form of a descriptive narrative, detailing the conversations that have occurred and the preferences the patient has expressed for goals of care [111, 117].
References
Centers for Disease Control and Prevention (CDC). Trends in aging – United States and worldwide. MMWR Morb Mortal Wkly Rep. 2003;52(6):101–4, 106.
Etzioni DA, Liu JH, O’Connell JB, Maggard MA, Ko CY. Elderly patients in surgical workloads: a population-based analysis. Am Surg. 2003;69(11):961–5.
Leung JM, Dzankic S. Relative importance of preoperative health status versus intraoperative factors in predicting postoperative adverse outcomes in geriatric surgical patients. J Am Geriatr Soc. 2001;49(8):1080–5.
Manku K, Leung JM. Prognostic significance of postoperative in-hospital complications in elderly patients. II. Long-term quality of life. Anesth Analg. 2003;96(2):590–4, table of contents.
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell Jr DA. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199(4):531–7.
Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53(3):424–9.
Rubinfeld I, Thomas C, Berry S, et al. Octogenarian abdominal surgical emergencies: not so grim a problem with the acute care surgery model? J Trauma. 2009;67(5):983–9.
Wilson ME, WIlliams NB, Baskett PJ, Bennett JA, Skene AM. Assessment of fitness for surgical procedures and the variability of anaesthetists’ judgments. Br Med J. 1980;280(6213):509–12.
Turnbull JM, Buck C. The value of preoperative screening investigations in otherwise healthy individuals. Arch Intern Med. 1987;147(6):1101–5.
Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253(24):3576–81.
Munro J, Booth A, Nicholl J. Routine preoperative testing: a systematic review of the evidence. Health Technol Assess. 1997;1(12):i–iv; 1–62.
McGory ML, Kao KK, Shekelle PG, et al. Developing quality indicators for elderly surgical patients. Ann Surg. 2009;250(2):338–47.
Woolger JM. Preoperative testing and medication management. Clin Geriatr Med. 2008;24(4):573–83, vii.
Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function – measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9.
Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. Med Clin North Am. 2003;87(1):7–40.
Wu WC, Schifftner TL, Henderson WG, et al. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery. JAMA. 2007;297(22):2481–8.
Fleischmann KE, Beckman JA, Buller CE, et al. 2009 ACCF/AHA focused update on perioperative beta blockade. J Am Coll Cardiol. 2009;54(22):2102–28.
Liu LL, Dzankic S, Leung JM. Preoperative electrocardiogram abnormalities do not predict postoperative cardiac complications in geriatric surgical patients. J Am Geriatr Soc. 2002;50(7):1186–91.
van Klei WA, Bryson GL, Yang H, Kalkman CJ, Wells GA, Beattie WS. The value of routine preoperative electrocardiography in predicting myocardial infarction after noncardiac surgery. Ann Surg. 2007;246(2):165–70.
Correll DJ, Hepner DL, Chang C, Tsen L, Hevelone ND, Bader AM. Preoperative electrocardiograms: patient factors predictive of abnormalities. Anesthesiology. 2009;110(6):1217–22.
Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867–78.
Hanlon JT, Schmader KE, Ruby CM, Weinberger M. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatr Soc. 2001;49(2):200–9.
Whinney C. Perioperative medication management: general principles and practical applications. Cleve Clin J Med. 2009;76 Suppl 4:S126–32.
Kennedy JM, van Rij AM, Spears GF, Pettigrew RA, Tucker IG. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol. 2000;49(4):353–62.
Devereaux PJ, Yang H, Yusuf S, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839–47.
Biccard BM, Sear JW, Foex P. Statin therapy: a potentially useful peri-operative intervention in patients with cardiovascular disease. Anaesthesia. 2005;60(11):1106–14.
Marik PE, Varon J. Requirement of perioperative stress doses of corticosteroids: a systematic review of the literature. Arch Surg. 2008;143(12):1222–6.
Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA. 2001;286(2):208–16.
Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148(6):427–34.
Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1–2):125–32.
Corrada MM, Brookmeyer R, Paganini-Hill A, Berlau D, Kawas CH. Dementia incidence continues to increase with age in the oldest old: the 90+ study. Ann Neurol. 2010;67(1):114–21.
Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58(4):643–9.
Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119(2):229–36.
Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271(2):134–9.
Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249(1):173–8.
Holsinger T, Plassman BL, Stechuchak KM, Burke JR, Coffman CJ, Williams Jr JW. Screening for cognitive impairment: comparing the performance of four instruments in primary care. J Am Geriatr Soc. 2012;60(6):1027–36.
Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021–7.
Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc. 2006;54(10):1578–89.
Brouquet A, Cudennec T, Benoist S, et al. Impaired mobility, ASA status and administration of tramadol are risk factors for postoperative delirium in patients aged 75 years or more after major abdominal surgery. Ann Surg. 2010;251(4):759–65.
Ansaloni L, Catena F, Chattat R, et al. Risk factors and incidence of postoperative delirium in elderly patients after elective and emergency surgery. Br J Surg. 2010;97(2):273–80.
Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108(1):18–30.
Noimark D. Predicting the onset of delirium in the post-operative patient. Age Ageing. 2009;38(4):368–73.
Demeure MJ, Fain MJ. The elderly surgical patient and postoperative delirium. J Am Coll Surg. 2006;203(5):752–7.
Leung JM, Tsai TL, Sands LP. Brief report: preoperative frailty in older surgical patients is associated with early postoperative delirium. Anesth Analg. 2011;112(5):1199–201.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011;40(1):23–9.
Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272(19):1518–22.
Flinn DR, Diehl KM, Seyfried LS, Malani PN. Prevention, diagnosis, and management of postoperative delirium in older adults. J Am Coll Surg. 2009;209(2):261–8, quiz 294.
Steffens DC, Fisher GG, Langa KM, Potter GG, Plassman BL. Prevalence of depression among older Americans: the Aging Demographics and Memory Study. Int Psychogeriatr. 2009;21(5):879–88.
Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147–56.
Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362(9384):604–9.
Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199(5):762–72.
Li C, Friedman B, Conwell Y, Fiscella K. Validity of the Patient Health Questionnaire 2 (PHQ-2) in identifying major depression in older people. J Am Geriatr Soc. 2007;55(4):596–602.
Blazer DG, Wu LT. The epidemiology of substance use and disorders among middle aged and elderly community adults: national survey on drug use and health. Am J Geriatr Psychiatry. 2009;17(3):237–45.
Blazer DG, Wu LT. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. Am J Psychiatry. 2009;166(10):1162–9.
Nath B, Li Y, Carroll JE, Szabo G, Tseng JF, Shah SA. Alcohol exposure as a risk factor for adverse outcomes in elective surgery. J Gastrointest Surg. 2010;14(11):1732–41.
Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869–74.
Berks J, McCormick R. Screening for alcohol misuse in elderly primary care patients: a systematic literature review. Int Psychogeriatr. 2008;20(6):1090–103.
McGrath A, Crome P, Crome IB. Substance misuse in the older population. Postgrad Med J. 2005;81(954):228–31.
Kaiser MJ, Bauer JM, Ramsch C, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58(9):1734–8.
Schiesser M, Kirchhoff P, Muller MK, Schafer M, Clavien PA. The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery. 2009;145(5):519–26.
Hickson M. Malnutrition and ageing. Postgrad Med J. 2006;82(963):2–8.
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134(1):36–42.
Corti MC, Guralnik JM, Salive ME, Sorkin JD. Serum albumin level and physical disability as predictors of mortality in older persons. JAMA. 1994;272(13):1036–42.
Souba WW. Nutritional support. N Engl J Med. 1997;336(1):41–8.
Volkert D, Berner YN, Berry E, et al. ESPEN guidelines on enteral nutrition: geriatrics. Clin Nutr. 2006;25(2):330–60.
Davenport DL, Ferraris VA, Hosokawa P, Henderson WG, Khuri SF, Mentzer Jr RM. Multivariable predictors of postoperative cardiac adverse events after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;204(6):1199–210.
Kumar R, McKinney WP, Raj G, et al. Adverse cardiac events after surgery: assessing risk in a veteran population. J Gen Intern Med. 2001;16(8):507–18.
Devereaux PJ, Goldman L, Cook DJ, Gilbert K, Leslie K, Guyatt GH. Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. CMAJ. 2005;173(6):627–34.
McAlister FA, Bertsch K, Man J, Bradley J, Jacka M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med. 2005;171(5):514–7.
Johnson RG, Arozullah AM, Neumayer L, Henderson WG, Hosokawa P, Khuri SF. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;204(6):1188–98.
Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232(2):242–53.
Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–50.
Smetana GW. Postoperative pulmonary complications: an update on risk assessment and reduction. Cleve Clin J Med. 2009;76 Suppl 4:S60–5.
Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144(8):581–95.
Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med. 2006;144(8):575–80.
Arozullah AM, Khuri SF, Henderson WG, Daley J. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med. 2001;135(10):847–57.
Hulzebos EH, Helders PJ, Favie NJ, De Bie RA, Brutel de la Riviere A, Van Meeteren NL. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA. 2006;296(15):1851–7.
Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand. 1997;41(9):1095–103.
Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet. 2002;359(9301):114–7.
Thomsen T, Tonnesen H, Moller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg. 2009;96(5):451–61.
Lindstrom D, Sadr Azodi O, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg. 2008;248(5):739–45.
Robinson TN, Eiseman B, Wallace JI, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(3):449–55.
Lachs MS, Feinstein AR, Cooney Jr LM, et al. A simple procedure for general screening for functional disability in elderly patients. Ann Intern Med. 1990;112(9):699–706.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57.
Chen TY, Anderson DJ, Chopra T, Choi Y, Schmader KE, Kaye KS. Poor functional status is an independent predictor of surgical site infections due to methicillin-resistant Staphylococcus aureus in older adults. J Am Geriatr Soc. 2010;58(3):527–32.
Robinson TN, Wallace JI, Wu DS, et al. Accumulated frailty characteristics predict postoperative discharge institutionalization in the geriatric patient. J Am Coll Surg. 2011;213(1):37–42; discussion 42–4.
Fedarko NS. The biology of aging and frailty. Clin Geriatr Med. 2011;27(1):27–37.
Abellan van Kan G, Rolland Y, Houles M, Gillette-Guyonnet S, Soto M, Vellas B. The assessment of frailty in older adults. Clin Geriatr Med. 2010;26(2):275–86.
Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1–15.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Jones DM, Song X, Rockwood K. Operationalizing a frailty index from a standardized comprehensive geriatric assessment. J Am Geriatr Soc. 2004;52(11):1929–33.
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
Lee DH, Buth KJ, Martin BJ, Yip AM, Hirsch GM. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation. 2010;121(8):973–8.
Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm – issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62(7):731–7.
Clegg A, Young J. The frailty syndrome. Clin Med. 2011;11(1):72–5.
Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–8.
Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–30; discussion 1530–1.
Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–8.
Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834–40.
Karlawish JH, Casarett DJ, James BD, Xie SX, Kim SY. The ability of persons with Alzheimer disease (AD) to make a decision about taking an AD treatment. Neurology. 2005;64(9):1514–9.
Fried TR, Bradley EH. What matters to seriously ill older persons making end-of-life treatment decisions?: A qualitative study. J Palliat Med. 2003;6(2):237–44.
Steinhauser KE, Christakis NA, Clipp EC, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22(3):727–37.
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284(19):2476–82.
Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378(9800):1408–13.
Truog RD, Waisel DB. Do-not-resuscitate orders: from the ward to the operating room; from procedures to goals. Int Anesthesiol Clin. Summer 2001;39(3):53–65.
Truog RD. “Do-not-resuscitate” orders during anesthesia and surgery. Anesthesiology. 1991;74(3):606–8.
Cohen CB, Cohen PJ. Do-not-resuscitate orders in the operating room. N Engl J Med. 1991;325(26):1879–82.
Ewanchuk M, Brindley PG. Perioperative do-not-resuscitate orders – doing ‘nothing’ when ‘something’ can be done. Crit Care. 2006;10(4):219.
Truog RD, Waisel DB, Burns JP. DNR in the OR: a goal-directed approach. Anesthesiology. 1999;90(1):289–95.
Margolis JO, McGrath BJ, Kussin PS, Schwinn DA. Do not resuscitate (DNR) orders during surgery: ethical foundations for institutional policies in the United States. Anesth Analg. 1995;80(4):806–9.
Wenger NS, Greengold NL, Oye RK, et al. Patients with DNR orders in the operating room: surgery, resuscitation, and outcomes. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Clin Ethics. 1997 Fall;8(3):250–7.
Caruso LJ, Gabrielli A, Layon AJ. Perioperative do not resuscitate orders: caring for the dying in the operating room and intensive care unit. J Clin Anesth. 2002;14(6):401–4.
Coppolino M, Ackerson L. Do surrogate decision makers provide accurate consent for intensive care research? Chest. 2001;119(2):603–12.
Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA. 1988;260(14):2069–72.
Waisel DB. Perioperative do-not-resuscitate orders. Curr Opin Anaesthesiol. 2000;13(2):191–4.
Fleisher LA, et al. Correction. J Am Coll Cardiol. 2008;52:794–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Marshall, G.T., Peitzman, A.B. (2014). Operative Risk Stratification. In: Yelon, J., Luchette, F. (eds) Geriatric Trauma and Critical Care. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8501-8_10
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8501-8_10
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8500-1
Online ISBN: 978-1-4614-8501-8
eBook Packages: MedicineMedicine (R0)