Abstract
Before being analyzed by microscopical evaluation, human tissues are submitted to a series of essential treatments that fall under the designation of “preanalytical treatment.” While grossing, paraffin embedding, freezing, and tissue banking are well-defined steps in the literature, our aim is to reach a standardized definition of the time interval between surgical removal to tissue grossing and fixation (preanalytical time interval, PATI) to obtain an optimal preservation of morphological structure, nucleic acids, and proteins. In the following section, a detailed description of the technical problems connected with the PATI and with the formalin fixation step is presented. In the context of fixation, the use of fixatives alternative to formalin is reported.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction and Purpose
Histopathological analysis (i.e., microscopical examination of tissue sections leading to related interpretation and diagnosis) on formalin-fixed and paraffin-embedded (FFPE) specimens is the goal of routine diagnostic histopathology. Owing to the recent advances in molecular approaches, however, this clinical material has also become a precious source of macromolecules for genomics and proteomics studies.
Before being analyzed, human tissues are submitted to a series of essential treatments that can directly affect their use in downstream molecular applications. All such procedures fall under the designation of “preanalytical treatment.” Basically, we should consider the following steps:
-
Surgical removal of tissue
-
Grossing (in the pathology lab)
-
Fixation, to be followed by paraffin embedding, or
-
Freezing, to be followed by tissue banking
While grossing, paraffin embedding, freezing, and tissue banking are well defined in the literature, our aim is to reach a standardized definition of the time interval between surgical removal and tissue grossing and fixation, keeping in mind that the ultimate goal is to obtain an optimal preservation of morphological structure, nucleic acids, and proteins.
Preanalytical treatment of tissues is one of the most variable and debated questions in molecular analysis. Information about the time between ablation of tissues and tissue fixation or the time and the temperature of fixation procedures is hardly ever available. On the other hand, early fixation of the tissues can be considered a good possibility to standardize the tissue treatment.
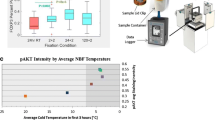
Recent studies give contradictory results about the relevance of temperature and time in the preanalytical treatment of tissues and these conditions are far from being clearly determined. The major problem is related to the hypoxic conditions of the tissues, which could occur in surgical specimens when the blood vessels are closed during the surgical treatment, even before tissue ablation. Conventionally, thirty minutes are considered the limit for a conservative treatment of the tissues [1], before fixation or freezing. However, it is difficult to accept that this time is not related to gene expression changes. Small modifications of gene expression have already been reported 5 min following the excision of the tissues [2], as a result of hypoxic conditions, but the alterations are not similar for all genes [3]. So early fixation is suggested, as it happens in small biopsies for which the clinical procedures are almost optimal. In larger surgical specimens, other variables, such as the hypoxia effect during the surgical intervention, the size of the tissues, the speed of fixative penetration, and the time for reduction of tissues to small fragments for the histological examination, have to be considered. This is still an open question that needs further studies and standardization.
The policy planned and experienced in our laboratory is that Phosphate-buffered Formalin (PBF) should be employed on tissue specimens after grossing and for a limited time (from 5 h, for relatively small specimens, up to 24 h, for large specimens). The reason for this policy is linked to observations of the uneven results of nucleic acid extraction and protein analysis of paraffin-embedded tissues (PET) fixed for long times in formalin [4, 5].The length of fixation in PBF influences the quality of RNA, which is found to be better in tissues fixed for 12–24 h, while longer fixation progressively decreases the quality of biomolecules [6, 7]. In addition, an optimal preservation of determinants predicting drug responsiveness in breast cancer is now regarded as mandatory and requires a formalin fixation not exceeding 48 h [8, 9].
Formalin fixation often starts in the surgical theater, where large specimens are immersed in PBF for transfer to the Pathology Laboratory. This procedure has drawbacks, since the degree of fixation of superficial and internal areas will be different. In addition, surgical nurses dislike handling this toxic, potentially cancerogenic fluid [10].
We consider that in order to achieve the goal of standardizing fixation times, grossing has to be done on fresh tissues and that, in order to assure a uniform fixation, this has to be done on 3–4 mm thick tissue slices in cassettes and for strictly definite times: for a minimum of 5 h for small specimens and for an average of 24 h (maximum 48 h) for large specimens.
Among the preanalytical variables associated with tissue harvesting and processing, the most critical one is the transfer of tissues from the surgical theater to the Pathology Laboratory. In our opinion, time and conditions of transfer need to be controlled, as a prerequisite to standardize fixation.
In our hospital (a large regional and University Hospital), tissue specimens to be transferred from the surgical theaters to the grossing room in the Pathology department are not immersed in formalin any more, but instead processed under vacuum (U.V.) [11]. This alternative procedure has further advantages, as tissue banking, cell cultures, and gene expression profiling are still feasible in U.V.-preserved tissues.
Upon the specific request of the surgical theatre personnel, the U.V. policy has been adopted in the whole hospital, which is presently considered as formalin-free as small specimens are treated in prefilled vessels, while large blocks are transferred U.V. in plastic bags (formalin is used in the Pathology Laboratory, but under proper hoods).
No detrimental effect, either on the morphological patterns or on the immunohistochemical features or gene expression profiling, was observed for tissues kept U.V. at 4°C over the weekend (up to 72 h).
In conclusion, it is practicable and feasible to start standardizing the length of fixation in PBF, a first step for a complete standardization of preanalytical variables. As a result, we shall achieve a more reliable evaluation of antigenic and genetic parameters, which nowadays represents a mandatory requirement in histopathological diagnoses.
In the following section, the detailed description of the technical problems connected with the preanalytical time interval (PATI) and with the formalin fixation step is presented. In the context of fixation, the use of fixatives alternative to formalin is reported.
2 Preanalytical Time Interval (PATI)
The PATI can be divided into Interval I and Interval II.
2.1 Interval I: From the Body to the Surgical Table (Temperature 37°C or More)
This interval is also called “warm ischemia time.” It depends on:
-
Type of operation
-
Modality of intervention
-
Ability of the surgeon
Time between ligation of arteries and removal:
Time negligible for:
-
Brain
-
Breast
-
Liver
-
Lymph nodes
-
Skin
Time from a minimum of 30 min to 1 h for:
-
Stomach
-
Colon
-
Lung
-
Pancreas
-
Thyroid
Effects:
-
Tissues are kept in hypoxic conditions at 37°C for variable time.
-
Remarkable loss of RNA and antigen degradation if the time is longer than a few minutes [12, 13].
-
If elimination of blood from ablated tissue is not immediate and complete, the hemoglobin coming from rapid tissue hemolysis can inhibit the downstream RT-PCR procedure.
Additional Caveats:
-
Areas near heath cutting
-
Treatment with Lugol solution (used for detecting the presence of starch in the cells)
2.2 Interval II: From the Surgical Table to the Pathology Lab
The options can be:
-
1.
Tissues left fresh
-
2.
Tissues immersed in formalin
-
3.
Tissues preserved under vacuum
2.2.1 Tissues Left Fresh
Temperature: Room Temperature (about 20°C).
In some realities, tissues (free in a vessel or in a bag) are transferred to the grossing room. After grossing, tissue specimens can be either stored at −80°C for frozen-section histology or fixed in a fixation solution (see Sect. 2.4 and Chap. 3).
-
Time interval between the surgical table and the pathology lab: relatively short, but depends on the internal organization of the hospital.
-
Time in pathology lab before grossing: variable, from a few minutes up to several hours. Optimal: 30 min.
-
Up to 4 h in most Pathology labs, according to Grizzle [14].
Dangers:
Effect of delay on:
-
Structure
-
Proteins (antigens)
-
Nucleic acids
Merits:
No Fixation (material available for fresh banking)
Drawbacks:
-
Drying of tissues (Even those left in the refrigerator)
-
Loss of antigens and RNA related to the time spent at room temperature before grossing
2.2.1.1 Fresh Tissues Immersed in Stabilization Solutions
A possible option is the use of new tissue stabilization solutions in order to specifically recover intact RNA from fresh frozen tissue specimens. One of the most commonly used reagents of this type is RNAlater (Applied Biosystems). It rapidly permeates tissues and inactivates RNases by precipitation, which eliminates the need to immediately freeze or formalin fix tissues after their removal. It is a practical solution because, after resection, the sample can be left in RNAlater solution for at least 1 week at room temperature, 8 weeks at 4°C, or indefinitely at −20°C, theoretically without compromising RNA integrity. Tissue in RNAlater can be subsequently processed as a fresh frozen sample for downstream molecular analysis. RNA purification can be performed, for example, by the standard TRIzol-based protocol (see product details at http://www.ambion.com/techlib/prot/bp_7020.pdf).
However, contrasting opinions have risen about its effective conservative properties on tissue architecture and macromolecule integrity. Some studies indicate that tissue samples stored in RNAlater and conventionally processed for histology have excellent morphology and immunohistochemical stain [15]. Others observed uneven results and decreased reactivity using different antibodies [16]. Some studies reported that results of RNA analysis in RNAlater-treated samples are comparable to those obtained in fresh frozen tissues [15, 17]. Others suggest that freezing should still be preferred over RNAlater treatment [18]. Recently, RNAlater has been compared to standard tissue fixatives [16]. RNAlater has also been tested as a pretreatment solution before alcohol-based tissue fixation, but at present the introduction of this prefixation step affects RNA quality [19].
2.2.2 Tissues Immersed in Formalin
Variables:
-
Temperature: room temperature (generally).
-
Time interval: variable from a few minutes up to days but it depends on the internal organization of the hospital.
-
Formalin: penetration is initially fast (1 mm/h), but then becomes much slower (1 cm/24 h). This is followed by fixation (slow) reaching subtotal binding plateau at 24 h [20, 21].
-
Fixation time: should be at least 6–8 h for 3 mm thick specimens [8, 22]. This is also applicable to fixation before and after grossing.
Merits:
In small blocks, formaldehyde rapidly affects structure, antigens, and nucleic acids (preservation/denaturation).
Drawbacks (in large specimens):
-
Degradation continues in deep areas (not reached by the fixative)
-
Frozen tissue banking is hampered
-
Formalin containing vessels are heavy to carry
-
Spilling of formalin may occur
-
Fumes are dispersed while grossing
-
Nurses refuse to handle this “carcinogen” in the surgical theater (without hoods)
-
Tissue is forgotten by the surgeon because it is “already safe in formalin”
2.2.3 Tissues Preserved Under Vacuum
Temperature: 0–4°C.
Time interval between the surgical table and the pathology lab: up to days.
Preservation under vacuum (U.V.) is easy to handle (inside the surgical theater). Tissues are immersed (packaged) in a plastic bag (with identification label), then into the U.V. machine (relatively small, semiprofessional). In a matter of seconds, the tissue is U.V.
The bag is left in the fridge, then transferred to the pathology lab inside a plastic container (with icing devices) [11]. After grossing, the tissue specimens can be easily processed as fresh tissues or immersed in fixation solutions (see Sect. 2.4 and Chap. 3).
Merits:
-
No more formalin in the surgical theater (except for small specimens, where prefilled tubes are employed)
-
No spilling
-
No fumes
-
No drying of tissues
-
Colors preserved
-
Lack of insulating air around tissues allows fast cooling
-
Tissues (bags) light and easy to carry
-
Structure (DNA, RNA, Antigens) preserved up to days
-
Banking (selective) allowed
Demonstration of operated tissues is convincing for students and surgeons
2.3 Consequences of PATI on Gene Expression Levels
PATI variably affects the expression profile both at the mRNA and the protein level [2]. These expression alterations represent a biological response to the detrimental effects of PATI rather than to the pathological condition.
Evaluation of ischemia effects on differential gene expression is currently focused on the detection of genes that are up-regulated. This strategy is pursued because gene down-regulation could be incorrect due to an artifact of RNA degradation (caused, for example, by a prolonged warm ischemia time) rather than to the cell response to tissue injury.
Several studies have reported that overexpression changes are time and tissue dependent (Table 2.1). Significant changes have been found not only in hypoxia-related genes (HIF-1α, c-fos, HO-1), but also in cytoskeletal genes (i.e., CK20) and in tumor-associated antigens (i.e., CEA).
Therefore specific precautions should be taken when gene expression studies are performed on target genes that could be affected by a physiological reaction of the cell to a decrease in oxygen availability.
3 Fixation
Fixation is required for the preservation of the tissue specimens that will be submitted for histopathological examination. Currently, formalin is the most commonly used fixative in tissue processing because it ensures an optimal preservation of tissue morphology, although other fixatives are specifically used in some pathology departments in Europe (i.e., Bouin’s solution [25]).
The quality of nucleic acids obtained from formalin-fixed and paraffin-embedded (FFPE) tissues varies enormously among laboratories. In some cases, but not in all, it is possible to extract well-preserved nucleic acids even from very old paraffin blocks [26]. Several fixation-related variables can affect the recovery of macromolecules. The failure of their optimization may result in underfixation or overfixation of the tissue, with a consequent high variability of the downstream results.
Fixation effects on macromolecule recovery depend on several elements:
-
The time of fixation is not standardized. During the week, the histopathology lab procedures are quite standardized, but any variation can double the time of fixation and this fact is not usually reported anywhere. This can happen with the samples collected just before the weekend, or any holiday.
-
The speed of fixative penetration is affected by the type and thickness of tissue. There is large diversity in the size of surgical specimens. Needle biopsy specimens are small (about 1.5 mm in diameter and 20 mm in length) and fix rapidly compared to larger tissue samples, while excisional specimens are 1 cm in diameter or more [7].
-
The volume of fixative can vary widely during the handling of surgical specimens. Since the minimum formalin:tissue ratio is 10:1, the volume of fixative represents a problem for large surgical specimens, especially those weighing more than 100 g [7]. Optimally, small sections should be obtained from the fresh specimen as soon as possible and allowed to fix after dissection.
-
The effect of the type of fixative solutions on tissues is well known, especially for formalin [27] and Bouin’s solution [25]. Concerning RNA, for example, variable levels of mRNA degradation can be obtained depending on the fixative. Similarly, selective RNA component (mRNA or rRNA) degradation can be observed [28].
Several molecular methods can be used to estimate the levels of quality and quantity of macromolecules extracted from fixed tissue specimens. They are described in detail in Chap. 17.
Several alternative fixation procedures have been proposed, with the aim of improving the preservation of nucleic acids and proteins, as compared to formalin fixation [29, 30]. In general, alcohol-based fixatives such as methacarn [31] or a combination of alcoholic fixatives and microwave treatment [28, 32] reach the important goal of an improved preservation of nucleic acid integrity, face to a good compromise of morphological preservation.
4 Tissue Processing
Tissue processing is the stepwise replacement of fixative with alcohol (dehydration) followed by the clearing step, which replaces the alcohol with an organic solvent, usually xylene. This process is fundamental for paraffin embedding and is usually performed automatically. Parameters affecting this process include time, temperature, and the presence of vacuum [6]. It has already been reported that tissue processing can affect the recovery of nucleic acids from FFPE; longer tissue processing times seem to result in better quality RNA [6]. In the absence of an exhaustive dehydration process, residual water could be trapped in the tissue with the subsequent RNA hydrolysis [6].
References
Huang J, Qi R, Quackenbush J, Dauway E, Lazaridis E, Yeatman T (2001) Effects of ischemia on gene expression. J Surg Res 99(2):222–227
Spruessel A, Steimann G, Jung M, Lee SA, Carr T, Fentz AK, Spangenberg J, Zornig C, Juhl HH, David KA (2004) Tissue ischemia time affects gene and protein expression patterns within minutes following surgical tumor excision. Biotechniques 36(6):1030–1037
Bray SE, Paulin FE, Fong SC, Baker L, Carey FA, Levison DA, Steele RJ, Kernohan NM (2010) Gene expression in colorectal neoplasia: modifications induced by tissue ischaemic time and tissue handling protocol. Histopathology 56(2): 240–250
Masuda N, Ohnishi T, Kawamoto S, Monden M, Okubo K (1999) Analysis of chemical modification of RNA from formalin-fixed samples and optimization of molecular biology applications for such samples. Nucleic Acids Res 27(22):4436–4443
van Maldegem F, de Wit M, Morsink F, Musler A, Weegenaar J, van Noesel CJ (2008) Effects of processing delay, formalin fixation, and immunohistochemistry on RNA recovery from formalin-fixed paraffin-embedded tissue sections. Diagn Mol Pathol 17(1):51–58
Chung JY, Braunschweig T, Williams R, Guerrero N, Hoffmann KM, Kwon M, Song YK, Libutti SK, Hewitt SM (2008) Factors in tissue handling and processing that impact RNA obtained from formalin-fixed, paraffin-embedded tissue. J Histochem Cytochem 56(11):1033–1042
Hewitt SM, Lewis FA, Cao Y, Conrad RC, Cronin M, Danenberg KD, Goralski TJ, Langmore JP, Raja RG, Williams PM, Palma JF, Warrington JA (2008) Tissue handling and specimen preparation in surgical pathology: issues concerning the recovery of nucleic acids from formalin-fixed, paraffin-embedded tissue. Arch Pathol Lab Med 132(12):1929–1935
Goldstein NS, Ferkowicz M, Odish E, Mani A, Hastah F (2003) Minimum formalin fixation time for consistent estrogen receptor immunohistochemical staining of invasive breast carcinoma. Am J Clin Pathol 120(1):86–92
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF (2007) American society of clinical oncology/college of American pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 131(1):18–43
IARC (2006) Formaldehyde, 2-butoxyethanol and 1-tert-butoxypropan-2-ol. IARC Monographs on the evaluation of carcinogenic risks to humans, vol 88
Bussolati G, Chiusa L, Cimino A, D’Armento G (2008) Tissue transfer to pathology labs: under vacuum is the safe alternative to formalin. Virchows Arch 452(2):229–231
Ohashi Y, Creek KE, Pirisi L, Kalus R, Young SR (2004) RNA degradation in human breast tissue after surgical removal: a time-course study. Exp Mol Pathol 77(2):98–103
Stanta G, Schneider C (1991) RNA extracted from paraffin-embedded human tissues is amenable to analysis by pcr amplification. Biotechniques 11(3):304, 306, 308
Grizzle WE (2001) The effect of tissue processing variables other than fixation on histochemical staining and immunohistochemical detection of antigens. J Histotechnol 24(3):213–219
Florell SR, Coffin CM, Holden JA, Zimmermann JW, Gerwels JW, Summers BK, Jones DA, Leachman SA (2001) Preservation of RNA for functional genomic studies: a multidisciplinary tumor bank protocol. Mod Pathol 14(2):116–128
Paska C, Bogi K, Szilak L, Tokes A, Szabo E, Sziller I, Rigo J Jr, Sobel G, Szabo I, Kaposi-Novak P, Kiss A, Schaff Z (2004) Effect of formalin, acetone, and RNAlater fixatives on tissue preservation and different size amplicons by real-time PCR from paraffin-embedded tissue. Diagn Mol Pathol 13(4):234–240
Chowdary D, Lathrop J, Skelton J, Curtin K, Briggs T, Zhang Y, Yu J, Wang Y, Mazumder A (2006) Prognostic gene expression signatures can be measured in tissues collected in RNAlater preservative. J Mol Diagn 8(1):31–39
Wang SS, Sherman ME, Rader JS, Carreon J, Schiffman M, Baker CC (2006) Cervical tissue collection methods for RNA preservation: comparison of snap-frozen, ethanol-fixed, and RNAlater-fixation. Diagn Mol Pathol 15(3):144–148
Benchekroun M, DeGraw J, Gao J, Sun L, von Boguslawsky K, Leminen A, Andersson LC, Heiskala M (2004) Impact of fixative on recovery of mRNA from paraffin-embedded tissue. Diagn Mol Pathol 13(2):116–125
Fox CH, Johnson FB, Whiting J, Roller PP (1985) Formaldehyde fixation. J Histochem Cytochem 33(8):845–853
Helander KG (1994) Kinetic studies of formaldehyde binding in tissue. Biotech Histochem 69(3):177–179
Goldstein NS, Hewitt SM, Taylor CR, Yaziji H, Hicks DG (2007) Recommendations for improved standardization of immunohistochemistry. Appl Immunohistochem Mol Morphol 15(2):124–133
Dash A, Maine IP, Varambally S, Shen R, Chinnaiyan AM, Rubin MA (2002) Changes in differential gene expression because of warm ischemia time of radical prostatectomy specimens. Am J Pathol 161(5):1743–1748
Schlomm T, Nakel E, Lubke A, Buness A, Chun FK, Steuber T, Graefen M, Simon R, Sauter G, Poustka A, Huland H, Erbersdobler A, Sultmann H, Hellwinkel OJ (2008) Marked gene transcript level alterations occur early during radical prostatectomy. Eur Urol 53(2):333–344
Bonin S, Petrera F, Rosai J, Stanta G (2005) DNA and RNA obtained from bouin’s fixed tissues. J Clin Pathol 58(3):313–316
Iesurum A, Balbi T, Vasapollo D, Cicognani A, Ghimenton C (2006) Microwave processing and ethanol-based fixation in forensic pathology. Am J Forensic Med Pathol 27(2): 178–182
Srinivasan M, Sedmak D, Jewell S (2002) Effect of fixatives and tissue processing on the content and integrity of nucleic acids. Am J Pathol 161(6):1961–1971
Dotti I, Bonin S, Basili G, Nardon E, Balani A, Siracusano S, Zanconati F, Palmisano S, De Manzini N, Stanta G (2010) Effects of formalin, methacarn, and fineFIX fixatives on RNA preservation. Diagn Mol Pathol 19(2):112–122
Cox ML, Schray CL, Luster CN, Stewart ZS, Korytko PJ, MK KN, Paulauskis JD, Dunstan RW (2006) Assessment of fixatives, fixation, and tissue processing on morphology and RNA integrity. Exp Mol Pathol 80(2):183–191
Lykidis D, Van Noorden S, Armstrong A, Spencer-Dene B, Li J, Zhuang Z, Stamp GW (2007) Novel zinc-based fixative for high quality DNA, RNA and protein analysis. Nucleic Acids Res 35(12):e85
Puchtler H, Waldrop FS, Meloan SN, Terry MS, Conner HM (1970) Methacarn (methanol-carnoy) fixation. Practical and theoretical considerations. Histochemie 21(2):97–116
Stanta G, Mucelli SP, Petrera F, Bonin S, Bussolati G (2006) A novel fixative improves opportunities of nucleic acids and proteomic analysis in human archive’s tissues. Diagn Mol Pathol 15(2):115–123
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Daniele, L., D’Armento, G., Bussolati, G. (2011). Preanalytical Time Interval (PATI) and Fixation. In: Stanta, G. (eds) Guidelines for Molecular Analysis in Archive Tissues. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-17890-0_2
Download citation
DOI: https://doi.org/10.1007/978-3-642-17890-0_2
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-17889-4
Online ISBN: 978-3-642-17890-0
eBook Packages: MedicineMedicine (R0)