Abstract
Lung wedge resection through video-assisted thoracic surgery (VATS) is aimed at achieving the same goals as open surgery, but according to minimally invasive principles. Main indications for VATS wedge resection include management of pneumothorax and advanced emphysema (i.e., pneumoplasty or lung volume reduction surgery), diagnosis of interstitial lung diseases and solitary pulmonary nodules, and surgical management of pulmonary metastases. The technical details of conventional three-port VATS wedge resection are described in this chapter; however, there is general interest in innovative surgical approaches that, coupled with the implementation of locoregional anesthesia, may further reduce the invasiveness of wedge resection, rendering this procedure feasible through a single-access (uniportal) incision in a day-surgery setting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Interstitial Lung Disease
- Wedge Resection
- Solitary Pulmonary Nodule
- Pulmonary Metastasectomy
- Primary Spontaneous Pneumothorax
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Lung wedge resection through video-assisted thoracic surgery (VATS) is aimed at achieving the same goals as open surgery, but according to minimally invasive principles. Main indications for VATS wedge resection include management of pneumothorax and advanced emphysema (i.e., pneumoplasty or lung volume reduction surgery), diagnosis of interstitial lung diseases and solitary pulmonary nodules, and surgical management of pulmonary metastases. The technical details of conventional three-port VATS wedge resection are described in this chapter; however, there is general interest in innovative surgical approaches that, coupled with the implementation of locoregional anesthesia, may further reduce the invasiveness of wedge resection, rendering this procedure feasible through a single-access (uniportal) incision in a day-surgery setting.
Wedge resection is commonly referred to as a triangular excision of a peripheral portion of the pulmonary parenchyma (McKenna 2009; Rami-Porta and Tsuboi 2009). It consists of sublobar nonanatomic lung removal; therefore, a generous wedge excision may involve more than one segment. A segmentectomy, on the other hand, involves individual dissection and ligation of the segmental vessels and bronchus to an anatomically defined lung segment. However, some authors use the term atypical or nonanatomic segmentectomy when a large wedge resection without individual vessel and bronchus ligation encompasses most of an anatomic segment (see also Chap. 12).
VATS has gained popularity during the past decade as a fundamental technical innovation aimed at fulfilling, in a minimally invasive fashion, the same diagnostic and/or therapeutic purposes previously addressed only by open surgery (McKenna 2009; Sedrakyan et al. 2004). Historically, pleural diseases were the first to be approached through VATS, which soon was adopted for pulmonary indications as well (Pettiford et al. 2007). Currently accepted indications for VATS wedge resection include the surgical management of pneumothorax and end-stage emphysema, histologic characterization of interstitial lung disease, diagnosis of a solitary pulmonary nodule, and treatment of pulmonary metastases (Pettiford et al. 2007; Pfannschmidt et al. 2007; Sedrakyan et al. 2004).
Technique
From a technical standpoint, the triangular parenchymal excision consists of a simultaneous division and suturing of peripheral subsegmental arterial, venous, and bronchial branches. As a rule, one side of the wedge specimen (i.e., the base of the triangle) is represented by the pleural surface of the lung or the fissural border. The other two sides are created by the surgeon. Under general anesthesia and one-lung ventilation, the patient is prepared and draped as for a standard thoracotomy. Indeed, the thoracotomy tray must be available in the theater at all times during VATS procedures. Usually, the patient is placed in a lateral decubitus position, exposing the side of the chest with the target area already identified on preoperative imaging. To improve exposure, the distance between the ribs is increased by “breaking” the operative table at the level of the angle of the scapula of the dependent hemithorax or by hip flexion. Alternatively, an axillary roll is inserted below the scapula. Careful preoperative imaging examination and routine skin marking direct port placement relative to the target area in the lung. During conventional three-port VATS wedge resection, the trocars may be used to minimize injury to the intercostal bundles while the operative instruments are introduced, although this may sometimes impair maneuverability. To address this disadvantage, flexible trocars may be used; some surgeons do not use trocars at all apart from the videothoracoscope port, which they use only to avoid smudging the lens. For standard VATS wedge resections, both disposable and nondisposable instruments are available; the choice depends on surgeon preference and local cost containment policies (McKenna 2009). A digitalized audio–video capturing system may provide a superior quality recording and allow storage of information.
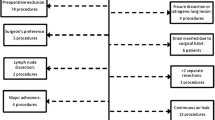
Typically, the target area of the lung to be excised represents the vertex of an ideal “baseball diamond” in which the home base corresponds to the port for the videothoracoscope (Figs. 11.1 and 11.2a). A small incision adequate for a 5- or 10-mm videothoracoscope is usually made at the level of the seventh or eighth intercostal space, on the scapular line, or immediately anterior or posterior to it, depending on the target area to be visualized (McKenna 2009). For example, wedge resection of the diaphragmatic surface of the lower lobes may impose a different positioning of the videothoracoscope. In this setting, the use of smaller ports to accommodate 5-mm 0° or 30° videothoracoscopes increasingly is being described. Furthermore, conventional three-port VATS requires the placement of two additional “operative” ports through which the grasping and stapling instruments are inserted sequentially according to an anterior–posterior approach (Fig. 11.2b) (McKenna 2009). As a rule, the most posterior incision should not be placed near the vertebral column and the most anterior one should not come anywhere close to the nipple to avoid bothersome paresthesia. If in doubt, a good method to select the ideal locations for the ports is to have the assistant probe different intercostal spaces with a needle inserted through the chest wall and monitored by the videothoracoscope. Consequently, the operating surgeon may determine the best site to avoid instrumentation interference and facilitate the performance of the procedure. This distribution of the operative incisions renders it difficult for one surgeon to perform the entire sequence of operative steps unless the patient is a child or is petite. As a rule, the operating surgeon holds the stapling instruments while two assistants visualize the field and grasp the lung trying to “accommodate” the lung parenchyma between the jaws of the endostapler. Sometimes the lung grasper can be inserted from the operator’s side to make it easier for the assistant to palpate the lung to identify a nodule to be resected. A maneuver to facilitate the wedge resection and improve hemostasis and aerostasis consists of clamping the parenchyma with two converging Roberts clamps to gently crush the lung before applying the endostapler.
While a wedge resection can be accomplished in open surgery by clamping and suturing the residual edges after removal of the wedged parenchyma, the same operation is facilitated thoracoscopically by the introduction of endoscopic staplers, which may be selected for different lengths and tissue thicknesses. For most indications, 45- or 60-mm blue cartridges are used (Fig. 11.2b). Alternatively, 45- or 60-mm green cartridges warrant air/blood tightness when fibrotic parenchyma is encountered. Once available only with straight jaws, endostaplers now offer a unique articulating feature aimed at improving jaw placement at the desired angle across the target area of the lung. Grasping instrumentation likewise has evolved, and both disposable and nondisposable devices now integrate articulating arms aimed at coordinating the thoracoscopic resection. Depending on the indication for wedge resection, multiple firings may be needed; in this case, special attention should be devoted to overlapping suture lines without leaving unstapled bridges of parenchyma. If the lung parenchyma is thin and at risk for continued air leak despite accurate cartridge selection, buttressing may be recommended. When cancer is suspected, care must be exercised in extracting the specimen through an endobag so as not to contaminate the wound (McKenna 2009). An alternative to stapling is the increasingly popular use of laser for excising pulmonary nodules, especially metastases to the lung (Fig. 11.3) (Pfannschmidt et al. 2007). In experienced hands, this approach may result in complete resections of multiple bilateral metastatic disease, including neoplastic lesions close to the hilum (Pfannschmidt et al. 2007). The laser technique for pulmonary metastasectomy is described in detail in Chap. 13.
Patient positioning and port distribution for conventional three-port VATS wedge resection. With the patient in the lateral decubitus position, the target area in the lung is placed at the vertex of an ideal “baseball diamond” configuration. Opposite the target area is the port for the videothoracoscope, and lateral are the operative ports through which the endograsper and endostapler can be inserted
Technical Variants of the Conventional VATS Wedge Resection Technique
Prompted by scattered reports that the level of invasiveness offered by conventional VATS procedures is not as limited as presumed, especially with regard to chronic pain, as well as reports of the technical pitfalls intrinsic to a thoracoscopic approach compared with open surgery (e.g., lack of palpation), several alternatives to conventional three-port VATS wedge resection have emerged in the recent literature.
In particular, single-access (uniportal) VATS wedge resection has been proposed as a completely different surgical philosophy that takes advantage of current technologic innovations, such as articulating endoscopic instruments, and awake-patient anesthesia (Rocco et al. 2010). The uniportal technique involves the sequential insertion through the same 2- to 2.5-cm long incision, together with the 5-mm 0° or 30° videothoracoscope, of articulating endograspers and endostaplers that address the target area to be resected according to a craniocaudal (i.e., sagittal, not anteroposterior) line (Fig. 11.4a, b) (Rocco et al. 2010). There are obvious similarities to the open technique, as the surgeon manipulates the lung and performs the subsequent resection the same way he or she normally would during thoracotomy. This is possible because deployment of the articulating arms of the operative instruments occurs away from the target area, thereby increasing intrathoracic maneuverability. In turn, this advantageous spatial distribution of the instruments helps avoid interference because the stems of the operative instruments are kept sideways along the single incision, taking full advantage of the laterality of the incision itself. Hence, compared with conventional three-port VATS, the uniportal approach does not impinge on multiple intercostal bundles.
Another technique addresses the lack of palpation with conventional VATS wedge resection, especially when used for pulmonary metastases. Several authors (especially Mineo and Detterbeck) have proposed a hand-assisted VATS wedge resection aimed at coupling minimal invasiveness and maximal accuracy in detecting pulmonary nodules. From a surgical standpoint, the innovative point resides in the creation of a substernal tunnel to accommodate the surgeon’s hand, which therefore can palpate both lungs at the same time (Pfannschmidt et al. 2007).
Results of VATS Wedge Resection
In experienced hands, procedure-related mortality and major morbidity rates after VATS wedge resection are minimal (McKenna 2009). There is a substantial body of literature supporting the association of VATS for treating pneumothorax and lung resections with reduced length of hospitalization, pain, or use of pain medications compared with thoracotomy, as well as fewer recurrences of pneumothorax compared with chest drainage alone (Sedrakyan et al. 2004). Universally accepted domains for the use of VATS wedge resections include the management of pneumothorax and end-stage pulmonary emphysema through lung volume reduction surgery (LVRS), which represents the ends of a spectrum of disease severity (Waller and Oey 2009). The results of VATS wedge resection coupled with some type of pleurodesis (e.g., apical pleurectomy or talc poudrage) are uniformly satisfactory in achieving complete lung reexpansion with less than a 5 % long-term recurrence rate and less than a 3 % rate of prolonged air leaks (Sedrakyan et al. 2004). From a technical point of view, LVRS consists of a series of coordinated, sequential wedge resections of the most compromised peripheral area of the emphysematous lung aimed at increasing recruiting nonfunctional, compressed alveolar units, which are brought into contact with the parietal pleura and hence with the negative pressure of the pleural space (Waller and Oey 2009 [for more details, see Chap. 24]). Whether VATS LVRS is performed unilaterally or on both sides, 5-year survival rates in patients may exceed 75 % (Waller and Oey 2009). The VATS LVRS approach has become common practice, with a fundamental difference compared with VATS for primary spontaneous pneumothorax: the air leak phenomenon after LVRS may complicate the postoperative course and affect postoperative mortality and morbidity to the extent that buttressing of the staple lines has been recommended. Reportedly, VATS wedge resection for clinical stage I non–small cell lung cancer may portend a higher risk for local relapse due to the narrow tumor-free margins (Pettiford et al. 2007). In this setting, adjuvant radiotherapy may prove detrimental (Rineer et al. 2010). Nevertheless, patients with primary lung cancer and compromised respiratory function and/or advanced age may benefit from VATS wedge resection with or without adjunctive brachytherapy mesh (Rami-Porta and Tsuboi 2009). In addition, this procedure may be adopted in the functionally uncompromised patient for adenocarcinoma subsets formerly known as bronchoalveolar carcinoma measuring less than 2 cm in diameter or peripheral ground glass opacities, with satisfactory long-term outcome (Rami-Porta and Tsuboi 2009).
Selected Bibliography
McKenna RJ (2009) Video-assisted thoracic surgery for wedge resection, lobectomy, and pneumonectomy. In: Shields TW (ed) General thoracic surgery, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 455–462
Pettiford BL, Schuchert MJ, Santos R, Landreneau RJ (2007) Role of sublobar resection (segmentectomy and wedge resection) in the surgical management of non-small cell lung cancer. Thorac Surg Clin 172:175–190
Pfannschmidt J, Dienemann H, Hoffmann H (2007) Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg 84:324–338
Rami-Porta R, Tsuboi M (2009) Sublobar resection for lung cancer. Eur Respir J 33:426–435
Rineer J, Schreiber D, Katsoulakis E, Nabhani T, Han P, Lange C, Choi K, Rotman M (2010) Survival following sublobar resection for early-stage non-small cell lung cancer with or without adjuvant external beam radiation therapy: a population-based study. Chest 137:362–368
Rocco G, Romano V, Accardo R, Tempesta A, La Manna C, La Rocca A, Martucci N, D’Aiuto M, Polimeno E (2010) Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 89:1625–1627
Sedrakyan A, van der Meulen J, Lewsey J, Treasure T (2004) Video assisted thoracic surgery for treatment of pneumothorax and lung resections: systematic review of randomized clinical trials. BMJ 329(7473):1008
Waller D, Oey I (2009) Staged lung volume reduction surgery—rationale and experience. Thorac Surg Clin 19(2):187–192
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Rocco, G. (2015). VATS Wedge Resection. In: Dienemann, H., Hoffmann, H., Detterbeck, F. (eds) Chest Surgery. Springer Surgery Atlas Series. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-12044-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-642-12044-2_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-12043-5
Online ISBN: 978-3-642-12044-2
eBook Packages: MedicineMedicine (R0)